Abstract
Post-traumatic stress disorder (PTSD) is common in patients with chronic pain, adversely affects chronic pain outcomes, and is associated with opioid use and adverse opioid outcomes. Social support is a robust predictor of PTSD incidence and course as well as chronic pain outcome. We determined whether the association between PTSD and persistent opioid use was modified by emotional support in a cohort of patients receiving opioids for non-cancer pain. Eligible participants were ≥ 18 and had completed a new period of prescription opioid use lasting 30–90 days. Bivariate associations between cohort characteristics and each key variable was assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Interaction between PTSD and emotional support was assessed by a priori stratification on low vs. high emotional support. Participants (n=808) were 53.6 (SD±11.6) years of age, 69.8% female, 69.6% white and 26.4% African-American. Overall, 17.2% had probable PTSD. High emotional support was significantly (p<.0001) more common among those without probable PTSD. Prescription opioid use at 6-month follow-up was significantly (p=.0368) more common among patients with versus without probable PTSD. In fully adjusted models, PTSD was no longer associated with opioid use at 6-month follow-up among participants with high emotional support. Among those with lower emotional support, PTSD was significantly associated with opioid use at 6-month follow-up in unadjusted (OR=2.40; 95%CI: 1.24–4.64) and adjusted models (OR=2.39; 95%CI:1.14–4.99). Results point to the hypothesis that improvement of emotional support in vulnerable patients with chronic pain and PTSD may help reduce sustained opioid use.
Keywords: pain, opioid, psychiatry, cohort, epidemiology
INTRODUCTION
Consistent evidence has demonstrated that comorbid posttraumatic stress disorder (PTSD) and non-cancer pain are common.[14] Meta-analyses revealed that 20% of persons with chronic widespread pain have PTSD,[48] and over 50% of veterans with chronic pain have PTSD.[14] This PTSD-pain comorbidity may lead to patients with PTSD receiving more prescription opioids compared to those without PTSD. Existing evidence suggests patients with vs. without PTSD are significantly more likely to receive higher opioid doses, progress to long-term opioid therapy (LTOT), obtain early refills, receive two or more opioid prescriptions at the same time, and have increased rates for opioid misuse and use disorder.[4; 18; 38; 42; 43]
One potential contributing factor to the high rate of prescription opioid use in PTSD is lack of social support, which is among the most robust predictors of developing and maintaining PTSD.[17] Positive social support is associated with reduced PTSD severity[8] and enhanced recovery from PTSD.[12] Social support may also modify or reduce the effects of PTSD on chronic pain and opioid use.
Perceived positive social support is associated with less persistent pain after injury,[34] and lack of social support is a perceived barrier to chronic pain self-management.[3] In a systematic review, Che and colleagues[9] found that social support may reduce pain-related stress by altering appraisals to reduce the perception of threat associated with pain. Because social support facilitates pain self-management, those with PTSD and high social support may require less prescription opioids than those with PTSD and low social support. While there is evidence that having social support enables treatment seeking for opioid dependence,[26] the impact of positive social support on prescription opioid use patterns is less clear.[50] However, spending more time on average with other people, an indicator of greater social support, was related to less prescribed opioid use in daily life in patients with chronic pain.[6] In this study, we focus on emotional support, that aspect of social support with the strongest relationship to chronic pain outcomes.[15] Emotional support is that form of social support that helps patients manage negative emotions and symptoms.
The present study was designed to measure the association between PTSD and the following prescription opioid outcomes at 6-month follow-up: 1) continued opioid use, 2) likelihood of high dose opioid use and 3) daily prescription opioid use. Second, we determined if emotional support moderates the association between PTSD and each opioid outcome.
METHODS
Details about the Pathways study protocol have been previously published.[40][45] In brief, the Pathways study is a prospective cohort study with assessments at baseline, 6- and 12-month follow-up. The Pathways study was designed to determine 1) the mental health consequences of long-term, frequent, higher dose prescription opioid use, 2) the types of mental illness and comorbidity patterns most strongly associated with problem opioid use, including persistent, long-term use, and 3) the moderators of the associations in goals 1 and 2. The present report uses baseline and 6-month follow-up data. The 12-month data were not available at the time of this analyses.
Patients were recruited from two healthcare systems, Saint Louis University’s academic medical practice, St. Louis, Missouri and Henry Ford Health, Detroit, Michigan. Both health care systems offer comprehensive inpatient and outpatient care, ranging from primary care to psychiatry, surgery, emergency care, etc. Eligible patients were 18 and older, had an electronic health record (EHR) indicating no current cancer related pain (confirmed via survey question), and all had started a new period of prescription opioid use with sufficient prescriptions to allow for 30 to 90 days of opioid use at baseline. We sampled patients with 30 to 90-day baseline opioid use to enrich the sample with participants likely to engage in long-term opioid use. We defined a new period of opioid use as having no opioid prescription in the past 3 months. Prescriptions could be from any provider type and all opioid mediations prescribed for pain were included. The condition for which opioids were prescribed could have changed during 6-month follow-up. The algorithm used to search the EHR was run weekly to identify likely eligible patients. Eligibility was confirmed via screening questions to ensure this was a new period of prescription opioid use and that the patient was not receiving opioids for cancer-related pain.
Eligible patients were then mailed a study packet which contained instructions on how to participate, informed consent documents and a respondent booklet to facilitate survey completion. To keep participant responses contemporary with their new period of prescription opioid use, participants had to complete the survey within 5 weeks after mailing study packets. Those who did not participate on their own initiative were contacted by research assistants via telephone. A maximum of 10 recruitment phone calls at 2 day intervals. Informed consent was obtained and documented in the REDCap survey instrument. To participate, patients had to release their EHR data for the 12 months prior to baseline and for the 12 months of follow-up. Those who did not consent to EHR release were exited from the interview. Participants either completed the survey in REDCap or completed the survey with a study interviewer who entered answers into REDCap. Baseline enrollment began 11/2019 and ended 11/2022 with 1,047 participants enrolled. Of the 1,047 enrolled, 852 completed the 6-month follow-up survey resulting in an 81.4% retention rate. The current study uses baseline and 6-month follow-up data from the 808 participants with complete data on all measures. Sensitivity analyses included data with imputed values. Figure 1 contains a flow-chart illustrating how we derived the eligible sample.All study procedures were reviewed and approved by the Saint Louis University and Henry Ford Health IRBs.
Figure 1.
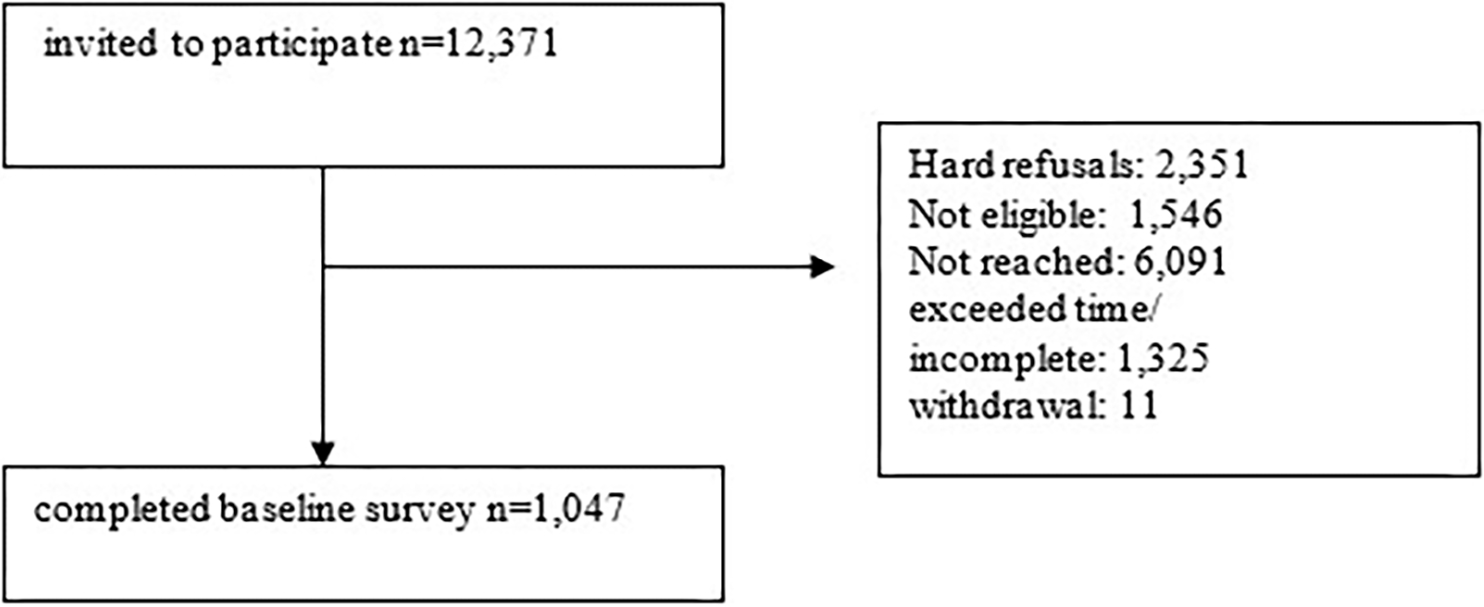
Eligible Sample
Outcomes:
The baseline and 6-month follow-up survey queried the type, dose and frequency of prescription opioid use. Participants were asked to report the name of their prescription opioid (e.g. codeine, dihydrocodeine, fentanyl, etc.) that was prescribed in the last 90 days. Participants reported the number of days per week that they used an opioid. The morphine milligram equivalent dose (MME) per day was computed using Centers for Disease Control and Prevention dose calculators[35]. Opioid outcomes at 6-month follow-up were: 1) persistent opioid use which was defined as any prescription opioid used at 6-month follow-up; 2) frequency of opioid use categorized as daily vs. less than daily and 3) daily MME dichotomized as < 50 MME per day vs. ≥50 MME per day.
Primary exposure:
PTSD was screened for at baseline using the Primary Care-PTSD-5 (PC-PTSD-5).[49] [27]Probable PTSD is defined by a PC-PTSD-5 score ≥3.
Potential effect modifier:
Emotional support was measured with the PROMIS SF v2.0–Emotional Support 4a scale.[1] Higher scores indicate more available emotional support. The emotional support scale was scored as “high” if the T-scaled score, based on the published reference population, was ≥50.
Covariates:
We modeled covariates that were measured at baseline. These included age, race, gender and highest educational attainment. The latter was categorized as no college, some college, and college graduate or higher. There is evidence that opioid prescribing increased via tele-health following onset of the COVID pandemic.[16; 36] Therefore, we controlled for the calendar year of baseline data collection to account for the waxing and waning of the pandemic over the course of the Pathways study.
Pain severity, pain related interference and number of pain sites were measured with the Brief Pain Inventory[11; 23]. Pain severity was measured with 4-items: worst in last 30 days, least in last 30 days, pain on average, and current pain. Pain severity was the mean of these items on a scale from ‘0=no pain’ to ‘10=pain as bad as you can imagine’. High pain severity was a mean score of 7 or above. Pain severity and pain interference thresholds were selected so that the distribution of high pain severity and interference scores were in the top 25th to 30th percentile. Seven pain interference questions assessed whether pain interfered with general activity, mood, walking ability, normal work, relationships, sleep, and enjoyment of life in the last 30 days. The pain interference score was the mean of these 7-items on a scale of ‘0=does not interfere’ to ‘10=completely interferes’. High pain interference was defined as a score of ≥8. The number of pain locations was obtained by asking participants if they had pain in 17 distinct body locations (e.g., lower back, arms, foot etc.).
We defined lifetime smoking as ever smoking 100 or more cigarettes.[25] We then controlled for baseline smoking status defined as current smoker vs. past/never. We used a computerized version of the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA-II)[5] to obtain lifetime DSM-IV substance use disorder diagnoses which included cannabis, stimulants/cocaine or heroin. Primary analyses did not include opioid use disorder (OUD) because we anticipated OUD to mask associations between PTSD, emotional support and opioid use outcomes. Instead, we conducted sensitivity analyses by recomputing all models with lifetime OUD diagnosis as part of the SUD variable to determine if the associations between PTSD and opioid outcomes could be detected when including OUD as part of the lifetime SUD variable.
Analytic Approach
The first step was to present univariate measures of distribution for selected cohort characteristics. For continuous characteristics, this includes the cohort mean and standard deviation (SD). For categorical characteristics, this includes percent and count in each category. Bivariate associations were computed between cohort characteristics and the primary exposure (PTSD) and then also with emotional support. Bivariate association between cohort characteristics and each key variable was assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Logistic regression models were used to assess the association between PTSD and each outcome, both before and after adjusting for relevant covariates. Interaction between PTSD and emotional support was assessed by inclusion of an interaction term in the logistic model and also by comparison of a priori stratified logistic regression results for patients with low vs. high emotional support. Alpha of 0.05 was used for all statistical tests. SAS v9.4 (Cary, NC) was used for all analyses.
Some values were missing, therefore we evaluated the robustness of our findings by conducting analyses after imputing missing values. The imputation model was compatible with the main outcome analysis model, so it included all analytic variables and the interaction of PTSD and emotional support. Auxiliary variables included depression, anxiety, and pain conditions (arthritis, back pain, muscle pain, fibromyalgia, neuropathy, chronic pain, and headache) present at baseline.
RESULTS
Baseline enrollment began 11/2019 and ended 11/2023 with 1,047 participants enrolled. Of the 1,047 enrolled, 852 completed the 6-month follow-up survey resulting in an 81.4% retention rate. As shown in the appendix, e-table 1, smokers were slightly more prevalent in the whole Pathways cohort compared to the 808 participants eligible for the present study (26.8% vs. 23.6%, p=0.0425). The average age was slightly but significantly younger in the whole cohort compared to the analytic sample (52.7±11.9 vs. 53.6±11.6). The distribution of other study variables did not significantly differ between the whole cohort and analytic sample, see e-table 1.
The most common opioid prescribed was hydrocodone (47.5%), followed by tramadol (37.5%), oxycodone (32.2%), codeine (9.9%) and morphine (2.2%). The cumulative percent of other types of prescribed opioid medications was < 10%. To protect confidentiality related to cell sizes <10, we do not report the percent prescribed these other opioid medications.
Cohort characteristics are shown in Table 1. Participants were an average of 53.6 (SD±11.6) years of age, 69.8% were female, 69.6% were white and 26.4% were African-American. Overall, 17.2% had probable PTSD. Probable PTSD was associated with younger age (p<.0001) and female gender (p=.0003). High pain interference (p<.0001) and high pain severity (p=.0002) were significantly more prevalent among those with probable PTSD and significantly more pain sites (p<.0001) were reported by those with as compared to without probable PTSD. Lifetime DSM-IV criteria SUD, with and without OUD included, were significantly (p=.0003) more prevalent in respondents with probable PTSD as was current smoking (p=.0039). Low emotional support was significantly (p<.0001) more common among those with probable PTSD. Prescription opioid use at 6-month follow-up was significantly (p=.0368) more common among patients with versus without probable PTSD. Race, educational attainment, year of data collection and opioid dose and frequency of use at 6-month follow-up were not significantly associated with probable PTSD.
Table 1.
Summary of participant characteristics by PTSD status (n=808)
| Overall (n=808) | PTSD (n=139) | No PTSD (n=669) | |||
|---|---|---|---|---|---|
| Characteristic | Category | % (n) | % (n) | % (n) | p-value |
| Age | Mean (SD) | 53.6 (11.6) | 49.7 (12.8) | 54.5 (11.2) | <.0001 |
| Race | White | 69.6% (562) | 65.5% (91) | 70.4% (471) | 0.2304 |
| Black | 26.4% (213) | 28.1% (39) | 26.0% (174) | ||
| Other | 4.1% (33) | 6.5% (9) | 3.6% (24) | ||
| Gender | Man | 30.2% (244) | 17.3% (24) | 32.9% (220) | 0.0003 |
| Woman | 69.8% (564) | 82.7% (115) | 67.1% (449) | ||
| Education | 1. No College | 28.7% (232) | 30.2% (42) | 28.4% (190) | 0.1599 |
| 2. Some College | 47% (380) | 51.8% (72) | 46.0% (308) | ||
| 3. Bachelor or higher | 24.3% (196) | 18.0% (25) | 25.6% (171) | ||
| Marital Status | Married/Living with Partner | 50.3% (406) | 36.7% (51) | 53.1% (355) | 0.0047 |
| Widow/Divorced/Separated | 30.5% (246) | 36.7% (51) | 29.2% (195) | ||
| Never Married | 18.2% (147) | 25.2% (35) | 16.7% (112) | ||
| Missing | 1.1% (9) | 1.4% (2) | 1.1% (7) | ||
| High Pain Interference | Yes | 34.2% (276) | 55.4% (77) | 29.7% (199) | <.0001 |
| Pain interference (mean, SD) | 6.6 (2.2) | 7.7 (1.9) | 6.4 (2.2) | ||
| High Pain Severity | Yes | 30% (242) | 43.2% (60) | 27.2% (182) | 0.0002 |
| Pain severity (mean, SD) | 5.9 (1.8) | 6.5 (1.8) | 5.8 (1.8) | ||
| # Pain Sites | Mean (SD) | 6.1 (3.7) | 7.9 (3.8) | 5.8 (3.6) | <.0001 |
| Year of Baseline Survey | 2020 | 18.7% (151) | 19.4% (27) | 18.5% (124) | 0.8603 |
| 2021 | 44.7% (361) | 43.9% (61) | 44.8% (300) | ||
| 2022 | 30.2% (244) | 28.8% (40) | 30.5% (204) | ||
| 2023 | 6.4% (52) | 7.9% (11) | 6.1% (41) | ||
| Lifetime Substance Use Disorder (excluding Opioids) | Yes | 9.2% (74) | 17.3% (24) | 7.5% (50) | 0.0003 |
| Lifetime SUD including OUD | 10.0% (81) | 19.4% (27) | 8.1% (54) | <.0001 | |
| Smoker | Yes | 23.6% (191) | 33.1% (46) | 21.7% (145) | 0.0039 |
| High Emotional Support | Yes | 69.1% (558) | 51.8% (72) | 72.6% (486) | <.0001 |
| Opioid at 6-month follow-up | Yes | 65.0% (525) | 72.7% (101) | 63.4% (424) | 0.0368 |
| Among Opioid Users at 6-month follow-up: | |||||
| Daily Opioid at 6-month follow-up | Yes | 54.4% (274) | 56.7% (55) | 53.8% (219) | 0.6073 |
| MME>50 at 6-month follow-up | Yes | 9.5% (44) | 10.8% (9) | 9.2% (35) | 0.6511 |
As shown in Table 2, participants with high pain interference were significantly more likely to have low emotional support compared to high emotional support (42.4% vs. 30.5%, p=0.0009). The mean number of pain sites was significantly greater among those with low emotional support compared to high emotional support (7.0±3.9 vs. 5.7±3.5). Persons with probable PTSD were more than twice as likely to have low emotional support as compared to high emotional support (26.8% vs. 12.9%, p<0.0001). Lifetime SUD, with (p=0.0118) and without OUD (p=0.0325), was also significantly more prevalent among participants with low emotional support.
Table 2.
Summary of characteristics by High vs. Not High Emotional Support (n=808)
| High ES (n=558) | Low ES (n=250) | |||
|---|---|---|---|---|
| Characteristic | Category | % (n) | % (n) | p-value |
| Age | Mean (SD) | 53.9 (11.6) | 53.1 (11.7) | 0.3361 |
| Race | White | 69.7% (389) | 69.2% (173) | 0.9535 |
| Black | 26.3% (147) | 26.4% (66) | ||
| Other | 3.9% (22) | 4.4% (11) | ||
| Gender | Man | 31% (173) | 28.4% (71) | 0.4562 |
| Woman | 69% (385) | 71.6% (179) | ||
| Education | 1. No College | 30.1% (168) | 25.6% (64) | 0.3042 |
| 2. Some College | 45.3% (253) | 50.8% (127) | ||
| 3. Bachelor or higher | 24.6% (137) | 23.6% (59) | ||
| Marital Status | Married/Living with Partner | 55.9% (312) | 37.6% (94) | <.0001 |
| Widow/Divorced/Separated | 26.2% (146) | 40.0% (100) | ||
| Never Married | 16.7% (93) | 21.6% (54) | ||
| Missing | 1.3% (7) | 0.8% (2) | ||
| High Pain Interference | Yes | 30.5% (170) | 42.4% (106) | 0.0009 |
| Pain interference (mean, SD) | 6.4 (2.2) | 7.1 (2.2) | <.0001 | |
| High Pain Severity | Yes | 28.1% (157) | 34% (85) | 0.0925 |
| Pain severity (mean, SD) | 5.8 (1.8) | 6.1 (1.8) | <.0001 | |
| # Pain Sites | Mean (SD) | 5.7 (3.5) | 7.0 (3.9) | <.0001 |
| Year of Baseline Survey | 2020 | 19% (106) | 18% (45) | 0.8209 |
| 2021 | 43.7% (244) | 46.8% (117) | ||
| 2022 | 31% (173) | 28.4% (71) | ||
| 2023 | 6.3% (35) | 6.8% (17) | ||
| Lifetime Substance Use Disorder (excluding Opioid Use Disorder) | Yes | 7.7% (43) | 12.4% (31) | 0.0325 |
| Lifetime SUD including Opioid Use Disorder | 8.2% (46) | 14% (35) | 0.0118 | |
| Smoker | Yes | 21.9% (122) | 27.6% (69) | 0.0761 |
| PTSD | Yes | 12.9% (72) | 26.8% (67) | <.0001 |
| Opioid use at 6-month follow-up | Yes | 64.5% (360) | 66% (165) | 0.6828 |
| Among Opioid Users at 6-month follow-up: | ||||
| Daily Opioid at 6 month Follow-up | Yes | 50.9% (178) | 62.3% (96) | 0.0177 |
| MME>50 at 6-month follow-up | Yes | 9.6% (30) | 9.4% (14) | 0.9485 |
As shown in Table 3, prior to adjusting for covariates, probable PTSD was significantly associated with a 54% increased odds (OR=1.54; 95%CI:1.02–2.30) of continued opioid use at 6-month follow-up. After adjusting for all covariates, this association was attenuated and no longer statistically significant (OR=1.33; 95%CI:0.86–2.04). The interaction of PTSD with emotional support on opioid use at 6-month follow-up was not statistically significant (p=.075 for unadjusted; p=.065 for adjusted models). However, the relationship between PTSD and opioid use was quite different when stratified by emotional support. Among those with high emotional support, PTSD was no longer associated with opioid use at 6-month follow-up. In contrast, among those with lower emotional support, PTSD was significantly associated with opioid use at 6-month follow-up in unadjusted (OR=2.40; 95%CI: 1.24–4.64) and adjusted models (OR=2.39; 95%CI:1.14–4.99).
Table 3.
Effect of PTSD at baseline on any prescription opioid use at 6-month follow-up
| Unadjusted | Fully Adjusted | Fully Adjusted with imputation for missing values | |
|---|---|---|---|
| Non-stratified | 1.54 (1.02–2.30) | 1.33 (0.86–2.04) | 1.26 (0.82–1.93) |
| High ES | 1.12 (0.66–1.88) | 0.92 (0.53–1.60) | 0.93 (0.53–1.62) |
| Not High ES | 2.40 (1.24–4.64) | 2.39 (1.14–4.99) | 2.09 (1.04–4.19) |
| p-value for interaction | 0.0747 | 0.0652 | 0.0683 |
Among participants who were still using opioids at 6-month follow-up, PTSD was not significantly associated with odds of being a daily vs. not daily prescription opioid user (Table 4). There was no significant interaction and PTSD was not significantly associated with daily vs. not daily opioid use in both the high and low emotional support strata.
Table 4.
Effect of PTSD at baseline on daily opioid among prescription opioid users at 6-month follow-up
| Unadjusted | Fully Adjusted | Fully Adjusted with imputation for missing values | |
|---|---|---|---|
| Non-stratified | 1.12 (0.72–1.76) | 0.79 (0.48–1.31) | 0.77 (0.46–1.29) |
| High ES | 1.06 (0.58–1.94) | 0.83 (0.42–1.62) | 0.81 (0.40–1.63) |
| Not High ES | 0.93 (0.46–1.87) | 0.65 (0.27–1.57) | 0.62 (0.25–1.53) |
| p-value for interaction | 0.7895 | 0.5246 | 0.6622 |
As shown in Table 5, PTSD was not significantly associated with odds of receiving ≥50 MME per day at 6-month follow-up. This association did not change in those with high and low emotional support.
Table 5.
Effect of PTSD at baseline on MME > 50 among prescription opioid users at 6-month follow-up
| Unadjusted | Fully Adjusted | Fully Adjusted with imputation for missing values | |
|---|---|---|---|
| Non-stratified | 1.20 (0.55–2.59) | 1.07 (0.46–2.47) | 1.05 (0.43–2.58) |
| High ES | 2.03 (0.77–5.36) | 1.63 (0.58–4.59) | 1.81 (0.60–5.46) |
| Not High ES | 0.58 (0.16–2.20) | 0.68 (0.15–3.12) | 0.46 (0.10–2.14) |
| p-value for interaction | 0.1367 | 0.1499 | 0.0724 |
Results of sensitivity analyses treating lifetime OUD as a component of lifetime SUD had minimal impact on results. Among those with lower social support, we observed PTSD was associated with 2.5 times greater odds of remaining a prescription opioid user at 6-month follow-up (OR=2.50; 95%CI:1.20–5.22).
Results from fully adjusted models using imputed data for missingness revealed no meaningful differences in point estimates, statistical significance or conclusions as compared to fully adjusted models without imputation (see Tables 3–5, far right columns).
DISCUSSION
Participants with non-cancer pain and probable PTSD at baseline had a significantly increased odds of remaining prescription opioid users at 6-month follow-up in unadjusted models. The odds of continued prescription opioid use at 6-months was attenuated and no longer significant among those with PTSD and high emotional support. PTSD among those with low emotional support was associated with more than a 2-fold increased likelihood of opioid use at 6-month follow-up. This association was independent of lifetime SUD and OUD. There were no statistically significant relationships between baseline PTSD and daily opioid use and daily dose at follow-up among those using opioids.
In bivariate analyses, PTSD was associated with: younger age, female gender, high pain interference, high pain intensity, more pain sites, lifetime substance abuse, smoking, and lower emotional support. These are similar to associations noted in previous studies of patients with chronic pain.[1; 24] Studies have consistently reported a higher prevalence of PTSD in patients with chronic pain who were prescribed opioids and that this PTSD was associated with increased risk for opioid misuse and OUD in patients with chronic pain.[28]
In bivariate analyses, lower emotional support was associated with: high pain interference, more pain sites, lifetime SUD, probable PSTD, and daily opioid use at follow-up. In previous reviews, social support has been found to be a psychosocial factor consistently associated with chronic pain outcomes.[21] Experimental pain studies have shown that receiving emotional support during a pain task not only reduces autonomic reactivity, but also reduces pain intensity and unpleasantness ratings and raises pain threshold.[37] Previous studies have found that patients with chronic pain were more likely to receive long-term opioid therapy if they came from socially disadvantaged neighborhoods.[10] In addition to Area Deprivation Index, opioid use was also associated with PROMIS depression, anxiety, and pain interference scores, but PTSD was not assessed.
Our study adds to this past work with its prospective design and its ability to study how PTSD and emotional support interact to predict long-term opioid use. Probable baseline PTSD predicted sustained opioid use 6 months later. High emotional support attenuated this effect, but lower emotional support did not. The results thus provide new information concerning the relationship between three important variables in chronic pain care: PTSD, emotional support and sustained opioid use.
The protective effect of social support on the development of PTSD after a traumatic event is supported by a robust body of research. A meta-analysis demonstrated that social support was the second strongest predictor of PTSD risk, after peritraumatic dissociation.[32] Perceived emotional support appears to be more important than social network size. Among low-income women who suffered both childhood abuse and adult sexual assault, social support had a large protective effect on PTSD severity.[41] In other studies, negative reactions from one’s social network and dissatisfaction with support predicted both the onset and severity of PTSD six months later.[2] Low social support is associated with avoidant coping which predicts a more prolonged course of PTSD.[47]
Interpersonal trauma may be a particularly potent cause of PTSD because it disrupts, as Judith Herman has noted, the interpersonal bonds of trust that connect the person to their community.[19] Epidemiological studies have consistently reported higher rates of PTSD for traumas that arise from intentional human action, including rape, combat exposure, as well as childhood neglect and abuse. In Israel, survivors of terror attacks developed PSTD at twice the rate of survivors of motor vehicle accidents.[46] Interpersonal violence carries more life threat than an accident and has a stronger relationship with PTSD.[32] Chronic pain and opioid use are usually understood as the consequence of physical events like tissue damage. But the current study suggests that psychological and social trauma may also be important in understanding the course of chronic pain and long-term opioid use.
We found high emotional support significantly attenuated the effect of probable PTSD at baseline on the use of opioids 6 months later in stratified analyses. The ability of opioids to reduce separation distress in chicks was first demonstrated in 1978 by Panskepp and colleagues.[33] Recent studies confirm that opioids may function as anxiolytics in patients with PTSD.[44] Although oxytocin and arginine vasopressin are more well-known hormonal modulators of human social behavior, Oxford evolutionary psychologist Robin Dunbar has argued in his Brain Opioid Theory of Social Attachment that the most important human social bonds are supported by endogenous opioids.[13] This theory is supported by his research demonstrating that: pain tolerance predicts human social network size,[22] adult attachment style is associated with cerebral mu-opioid receptor availability,[30] social touch modulates endogenous mu-opioid system activity,[31] blocking mu-opioid receptors inhibits social bonding in rituals,[7] and social laughter triggers endogenous opioid release.[29] Thus, people who have experienced interpersonal trauma may be prone to engage in persistent opioid use to reduce their distress.
Our study suggests that emotional support may attenuate this effect of emotional and social injury, reflected in probable PTSD, on opioid use. Patients with chronic pain and PTSD who have high emotional support may not need opioids to reduce their distress so they do not demonstrate persistent opioid use. This may be important as traditional sources of social support such as churches and synagogues have seen declining attendance in recent years. Because PTSD was only assessed with a screener at baseline and the interaction of PTSD and social support was not significant concerning opioid use at 6 months, we must consider these results as preliminary and in need of further confirmation. While prescription opioid use at 6-month follow-up was more common among patients with probable PTSD at baseline, race, educational attainment, opioid dose and frequency of opioid use at 6-month follow-up were not significantly associated with probable PTSD at baseline.
Our study may have practical clinical implications. Patients with chronic pain and PTSD are already recognized as high risk for persistent opioid use, opioid misuse and OUD. Our study provides preliminary evidence that improving emotional support in these patients may help mitigate these opioid risks. There is some evidence that emotional support provided by groups may play an important role in opioid tapering.[39] A basic insight from the care of patients with SUDs is applicable here. As substance use becomes more frequent and intense, social relationships often deteriorate. If problematic substance use is to be reduced, social relationships need to be strengthened. Patients may benefit from relying less on substances to relieve bad feelings and more on relationships.[20]
Limitations:
Our results should be interpreted in the context of several limitations. First, we did not obtain a PTSD diagnosis and findings apply to those with probable PTSD. Second, we measured one domain of social support and it is possible that results may differ by the number of persons in participants’ social network. Third, and as mentioned in the Results section above, the difference in magnitude of effect suggests effect modification by emotional support level but the p-values for the interaction terms were not statistically significant. Additional analyses in a larger sample may shed further light on this relationship. We are not able to establish the temporal associations nor able to draw causal relationships between PTSD, emotional support and opioid outcomes. We lacked measures on non-prescribed opioids. It is possible that some participants were using opioids from other sources and there is the potential that those who did not continue prescription opioids at 6-month follow-up may have switched to non-medical opioid use. Potential bias may be present if patients who did not participate because they would not share their medical record systematically differed from those who did. However, our descriptive study of baseline characteristics[45] indicated that participants differed from non-participants on only a few variables. Participants compared to non-participants were younger, more often female and had a higher prevalence of arthritis and muscle pain compared to non-participants. Those who suffer more severe PTSD may have been less likely to participate in the 6-month follow-up, however, only small differences in the distribution of smoking status and average age were observed between the full cohort and the analytic sample. This study was also conducted during the COVID-19 epidemic when opioid prescribing increased, possibly limiting the generalizability of our findings. Last, the study was conducted in two large Midwestern Healthcare systems and findings may not apply to other geographic regions.
In conclusion, our study found that probable PTSD at baseline was associated with persistent opioid use over 6 months in a sample of patients with chronic pain starting opioid therapy. This effect of PTSD on opioid use was significantly attenuated in patients reporting high levels of emotional support, but not in those reporting low levels of emotional support. This finding is theoretically important because it may clarify the role of emotional support in the experience of chronic pain and the use of long-term opioid therapy. This finding is practically significant because it may suggest that improvement of emotional support in vulnerable patients with chronic pain and PTSD may help reduce sustained opioid use and possibly other adverse opioid outcomes.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported by National Institute on Drug Abuse grant R01DA043811
The authors thank study participants for their time and effort. The authors thank the many student research assistants who contributed to recruiting participants and conducting phone surveys.
Footnotes
Conflict of Interest: All authors report no conflicts of interest relevant to this research study
Data availability:
interested persons should contact the corresponding author
REFERENCES
- [1].Afari N, Ahumada SM, Wright LJ, Mostoufi S, Golnari G, Reis V, Cuneo JG. Psychological trauma and functional somatic syndromes: a systematic review and meta-analysis. Psychosom Med 2014;76(1):2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Andrews B, Brewin CR, Rose S. Gender, social support, and PTSD in victims of violent crime. J Trauma Stress 2003;16(4):421–427. [DOI] [PubMed] [Google Scholar]
- [3].Bair MJ, Matthias MS, Nyland KA, Huffman MA, Stubbs DL, Kroenke K, Damush TM. Barriers and facilitators to chronic pain self-management: a qualitative study of primary care patients with comorbid musculoskeletal pain and depression. Pain Med 2009;10(7):1280–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bilevicius E, Sommer JL, Asmundson GJG, El-Gabalawy R. Posttraumatic stress disorder and chronic pain are associated with opioid use disorder: Results from a 2012–2013 American nationally representative survey. Drug Alcohol Depend 2018;188:119–125. [DOI] [PubMed] [Google Scholar]
- [5].Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Reich T, Schmidt I, Schnuckit MA. A new, semistructured psychiatric interview for use in genetic-linkage studies - A report on the reliability of the Ssaga. Journal of Studies on Alcohol 1994;55:149–158. [DOI] [PubMed] [Google Scholar]
- [6].Carpenter RW AS, Meshesha LZ. The Role of Environmental Context and Physical Activity in Prescribed Opioid Use and Pain in Daily Life among Patients With Chronic Low Back Pain. Ann Behav Med 2023;57(7):541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Charles SJ, Farias M, van Mulukom V, Saraswati A, Dein S, Watts F, Dunbar RIM. Blocking mu-opioid receptors inhibits social bonding in rituals. Biol Lett 2020;16(10):20200485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Charuvastra A, Cloitre M. Social bonds and posttraumatic stress disorder. Annu Rev Psychol 2008;59:301–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Che X, Cash R, Ng SK, Fitzgerald P, Fitzgibbon BM. A Systematic Review of the Processes Underlying the Main and the Buffering Effect of Social Support on the Experience of Pain. The Clinical journal of pain 2018;34(11):1061–1076. [DOI] [PubMed] [Google Scholar]
- [10].Cheng AL, Brady BK, Bradley EC, Calfee RP, Klesges LM, Colditz GA, Prather H. Opioid use and social disadvantage in patients with chronic musculoskeletal pain. PM R 2022;14(3):309–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cleeland CS. The Brief Pain Inventory User Guide Houston, TX: University of Texas M.D. Anderson Cancer Center, 1991. [Google Scholar]
- [12].Dai W, Chen L, Tan H, Wang J, Lai Z, Kaminga AC, Li Y, Liu A. Association between social support and recovery from post-traumatic stress disorder after flood: a 13–14 year follow-up study in Hunan, China. BMC Public Health 2016;16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dunbar RI. Bridging the bonding gap: the transition from primates to humans. Philos Trans R Soc Lond B Biol Sci 2012;367(1597):1837–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fishbain DA, Pulikal A, Lewis JE, Gao J. Chronic Pain Types Differ in Their Reported Prevalence of Post -Traumatic Stress Disorder (PTSD) and There Is Consistent Evidence That Chronic Pain Is Associated with PTSD: An Evidence-Based Structured Systematic Review. Pain Med 2017;18(4):711–735. [DOI] [PubMed] [Google Scholar]
- [15].Franqueiro AR YJ, Crago MA, Curiel M, Wilson JM. . The Interconnection Between Social Support and Emotional Distress Among Individuals with Chronic Pain: A Narrative Review. Psychol Res Behav Manag 2023;16:4389–4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gilmer G JN, Koscumb S, Marroquin OC, Sowa G. . A Retrospective Analysis of Clinical Utilization Between Patients Who Used Telemedicine and Office Visits in Outpatient Physical Medicine and Rehabilitation Clinics During the COVID-19 Pandemic. Am J Phys Med Rehabil 2023;102(1):34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Guay S, Billette V, Marchand A. Exploring the links between posttraumatic stress disorder and social support: processes and potential research avenues. J Trauma Stress 2006;19(3):327–338. [DOI] [PubMed] [Google Scholar]
- [18].Hassan AN, Le Foll B, Imtiaz S, Rehm J. The effect of post-traumatic stress disorder on the risk of developing prescription opioid use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. Drug Alcohol Depend 2017;179:260–266. [DOI] [PubMed] [Google Scholar]
- [19].Herman J. Trauma and Recovery. New York, NY: Basic Books. 2015. [Google Scholar]
- [20].Islam MF, Guerrero M, Nguyen RL, Porcaro A, Cummings C, Stevens E, Kang A, Jason LA. The Importance of Social Support in Recovery Populations: Toward a Multilevel Understanding. Alcohol Treat Q 2023;41(2):222–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch Phys Med Rehabil 2011;92(1):146–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Johnson KV, Dunbar RI. Pain tolerance predicts human social network size. Sci Rep 2016;6:25267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. The Clinical journal of pain 2004;20(5):309–318. [DOI] [PubMed] [Google Scholar]
- [24].Kind S, Otis JD. The Interaction Between Chronic Pain and PTSD. Curr Pain Headache Rep 2019;23(12):91. [DOI] [PubMed] [Google Scholar]
- [25].Klemperer EM HJ, Callas PW, West JC, Villanti AC. Tobacco and Nicotine Use Among US Adult “Never Smokers” in Wave 4 (2016–2018) of the Population Assessment of Tobacco and Health Study. Nicotine Tob Res 2021;23(7):1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kumar N, Oles W, Howell BA, Janmohamed K, Lee ST, Funaro MC, O’Connor PG, Alexander M. The role of social network support in treatment outcomes for medication for opioid use disorder: A systematic review. J Subst Abuse Treat 2021;127:108367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Langford DJ, Theodore BR, Balsiger D, Tran C, Doorenbos AZ, Tauben DJ, Sullivan MD. Number and Type of Post-Traumatic Stress Disorder Symptom Domains Are Associated With Patient-Reported Outcomes in Patients With Chronic Pain. J Pain 2018;19(5):506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lopez-Martinez AE, Reyes-Perez A, Serrano-Ibanez ER, Esteve R, Ramirez-Maestre C. Chronic pain, posttraumatic stress disorder, and opioid intake: A systematic review. World J Clin Cases 2019;7(24):4254–4269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Manninen S, Tuominen L, Dunbar RI, Karjalainen T, Hirvonen J, Arponen E, Hari R, Jaaskelainen IP, Sams M, Nummenmaa L. Social Laughter Triggers Endogenous Opioid Release in Humans. J Neurosci 2017;37(25):6125–6131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Nummenmaa L, Manninen S, Tuominen L, Hirvonen J, Kalliokoski KK, Nuutila P, Jaaskelainen IP, Hari R, Dunbar RI, Sams M. Adult attachment style is associated with cerebral mu-opioid receptor availability in humans. Hum Brain Mapp 2015;36(9):3621–3628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Nummenmaa L, Tuominen L, Dunbar R, Hirvonen J, Manninen S, Arponen E, Machin A, Hari R, Jaaskelainen IP, Sams M. Social touch modulates endogenous mu-opioid system activity in humans. Neuroimage 2016;138:242–247. [DOI] [PubMed] [Google Scholar]
- [32].Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 2003;129(1):52–73. [DOI] [PubMed] [Google Scholar]
- [33].Panksepp J, Vilberg T, Bean NJ, Coy DH, Kastin AJ. Reduction of distress vocalization in chicks by opiate-like peptides. Brain Res Bull 1978;3(6):663–667. [DOI] [PubMed] [Google Scholar]
- [34].Prang KH, Berecki-Gisolf J, Newnam S. Recovery from musculoskeletal injury: the role of social support following a transport accident. Health Qual Life Outcomes 2015;13:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Prevention CfDCa. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022, Vol. 2023. https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm#T1_down US Government, 2022. p. TABLE. Morphine milligram equivalent doses for commonly prescribed opioids for pain management. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Rikin S PH, Zhang C, Khalid L, Groeger J, Deng Y, Starrels JL. Changes in Outpatient Opioid Prescribing During the COVID-19 Pandemic: An Interrupted Time Series Analysis. J Prim Care Community Health 2022;13:21501319221076926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Roberts MH, Klatzkin RR, Mechlin B. Social Support Attenuates Physiological Stress Responses and Experimental Pain Sensitivity to Cold Pressor Pain. Ann Behav Med 2015;49(4):557–569. [DOI] [PubMed] [Google Scholar]
- [38].Saadoun M, Bauer MR, Adams RS, Highland KB, Larson MJ. Opioid and Nonpharmacologic Treatments Among Soldiers With Chronic Pain and Posttraumatic Stress Disorder. Psychiatr Serv 2021;72(3):264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Sandhu HK, Booth K, Furlan AD, Shaw J, Carnes D, Taylor SJC, Abraham C, Alleyne S, Balasubramanian S, Betteley L, Haywood KL, Iglesias-Urrutia CP, Krishnan S, Lall R, Manca A, Mistry D, Newton S, Noyes J, Nichols V, Padfield E, Rahman A, Seers K, Tang NKY, Tysall C, Eldabe S, Underwood M. Reducing Opioid Use for Chronic Pain With a Group-Based Intervention: A Randomized Clinical Trial. JAMA 2023;329(20):1745–1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Scherrer JF AB, Autio K, Debar L, Lustman PJ, Miller-Matero LR, Salas J, Secrest S, Sullivan MD, Wilson L, Skiold-Hanlin S. The Prescription Opioids and Depression Pathways Cohort Study. J Psychiatr Brain Sci 2020;5:e200009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. J Trauma Stress 2006;19(6):825–836. [DOI] [PubMed] [Google Scholar]
- [42].Schwartz AC, Bradley R, Penza KM, Sexton M, Jay D, Haggard PJ, Garlow SJ, Ressler KJ. Pain medication use among patients with posttraumatic stress disorder. Psychosomatics 2006;47(2):136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Seal KH, Shi Y, Cohen G, Cohen BE, Maguen S, Krebs EE, Neylan TC. Association of mental health disorders with prescription opioids and high-risk opioid use in US Veterans of Iraq and Afghanistan. JAMA 2012;307:940–947. [DOI] [PubMed] [Google Scholar]
- [44].Seal KH, Shi Y, Cohen G, Cohen BE, Maguen S, Krebs EE, Neylan TC. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA 2012;307(9):940–947. [DOI] [PubMed] [Google Scholar]
- [45].Secrest SM-ML, Chrusciel T, Salas J, Sullivan MD, Zabel C, Lustman P, Ahmedani B, Carpenter RW, Scherrer JF. . Baseline Characteristics From a New Longitudinal Cohort of Patients With Noncancer Pain and Chronic Opioid Use in the United States. . J Pain 2023;S1526-5900(23)00595-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Shalev AY, Freedman S. PTSD following terrorist attacks: a prospective evaluation. The American journal of psychiatry 2005;162(6):1188–1191. [DOI] [PubMed] [Google Scholar]
- [47].Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA 2002;288(10):1235–1244. [DOI] [PubMed] [Google Scholar]
- [48].Siqveland J, Hussain A, Lindstrom JC, Ruud T, Hauff E. Prevalence of Posttraumatic Stress Disorder in Persons with Chronic Pain: A Meta-analysis. Front Psychiatry 2017;8:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].van Dam D ET, Vedel E, Emmelkamp PM. Validation of the Primary Care Posttraumatic Stress Disorder screening questionnaire (PC-PTSD) in civilian substance use disorder patients. . J Subst Abuse Treat 2010;39(2):105–113. [DOI] [PubMed] [Google Scholar]
- [50].Zajacova A, Grol-Prokopczyk H, Limani M, Schwarz C, Gilron I. Prevalence and correlates of prescription opioid use among US adults, 2019–2020. PLoS One 2023;18(3):e0282536. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
interested persons should contact the corresponding author


