Abstract
Introduction and importance
Frontal bone osteomyelitis associated with a subperiosteal abscess is known as Pott's puffy tumor. Pott puffy tumor (PPT) is a rare entity that mainly affects children and adolescents. It is less common in adults, accounting for 30 % of cases, and predominates in men. The therapeutic management of Pott's puffy tumor is an emergency and is based on a combination of antibiotic therapy and surgical treatment to prevent the emergence of intracranial complications and reduce morbidity and mortality.
Case presentation
We report the case of a 29-year-old female patient, who consulted our ENT (ear, nose, and throat) department for a post-traumatic periorbital swelling. CT scan confirmed osteomyelitis of the frontal bone and subperiosteal abscess. The patient underwent a combined surgical drainage with antibiotics. The aim is to describe an effective management of this clinical case.
Clinical discussion
This condition presents as a subperiosteal/subgaleal abscess creating a frontal swelling, with osteomyelitis of the frontal bone most often secondary to frontal sinusitis. The most feared complications are intracranial, which can be life-threatening. Imaging is the key to positive diagnosis, as the evolution and prognosis of TPP depend on rapid management. A CT scan of the head is the examination of choice to confirm the diagnosis. Antibiotic therapy should be started as soon as possible, it is usually administered by intravenous injection. Surgical management may be limited to percutaneous drainage by needle or transnasal endoscopy or trephination, sometimes including trimming of the subperiosteal/subgaleal abscess. In the case of intracranial complications, a craniotomy may be necessary.
Conclusion
The Pott's puffy tumor is little-known complication, usually secondary to untreated or poorly treated sinusitis. As a result of this poor understanding, the condition can lead to complications, especially intracranial ones, which increase morbidity and mortality.
Keywords: Pott puffy tumor; Case report; Surgery; ENT (ear, nose, and throat); Neurology
Highlights
-
•
Pott puffy tumor is a condition featuring osteomyelitis of the frontal bone together with a subperiosteal abscess.
-
•
The condition usually results from acute or chronic frontal sinusitis, which can lead to infection of the frontal bone.
-
•
The clinical presentation of TPP is non-specific, and varies with the severity of the infection.
-
•
The therapeutic management of Pott's puffy tumor is an emergency and is based on a combination of antibiotic therapy and surgical intervention
1. Introduction
Pott's puffy tumor (PPT) represents an unusual yet critical condition in which the forehead appears as a swelling from a subperiosteal abscess associated with osteomyelitis of the frontal bone. The condition frequently occurs as a complication of frontal sinusitis or trauma. Symptoms include fever, headache, nasal discharge and signs of increased intracranial pressure. It was first described by Percival Pott in the 18th century [1,2].
It progresses to life-threatening intracranial extension. Physicians must be extremely reactive when faced with a clinical picture suggestive of a PPT [3].
In this context, we present the case with the aim of describing a successful management of patient who had suffered head trauma, presented with right pansinusitis, and who developed a PPT with intracranial complications.
This case report has been reported in line with the SCARE criteria [17].
2. Case report
We report the case of a 29-years-old male patient who consulted us in our ENT and cervico-facial surgery department for a cranio-facial pain and a right periorbital swelling. The patient is a chronic smoker.
The history of illness dates back to 1 day after head trauma, with the appearance of dizziness, headache, rhinorrhea, fever and a right periorbital swelling. On physical examination, the patient was in good general condition, with Glasgow Consciousness Scale 15/15. No signs of neurological deficit were noted. On facial examination, we note a periorbital tumefaction that is red, tender and retractable on palpation, suggesting an inflammatory response (Fig. 1).
Fig. 1.
Patient image showing the right orbital tumefaction.
On rhinoscopy we noted a serous rhinorrhea with an inflammatory appearance of pituitary mucosa.
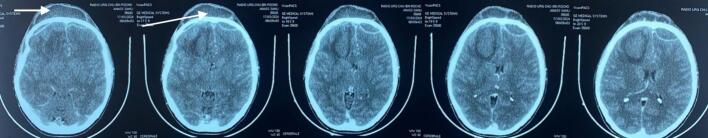
The patient then underwent a combined craniofacial CT scan showing an appearance of right pansinusitis complicated by a Pott Puffy tumor, a bilateral frontal empyemas and a right frontal parenchymal collection that looks inflammatory (Fig. 3, Fig. 2, Fig. 4).
Fig. 3.
CT scan showing a periosteal collection and frontal osteomyelitis.
Fig. 2.
CT scan showing the right pansinusitis.
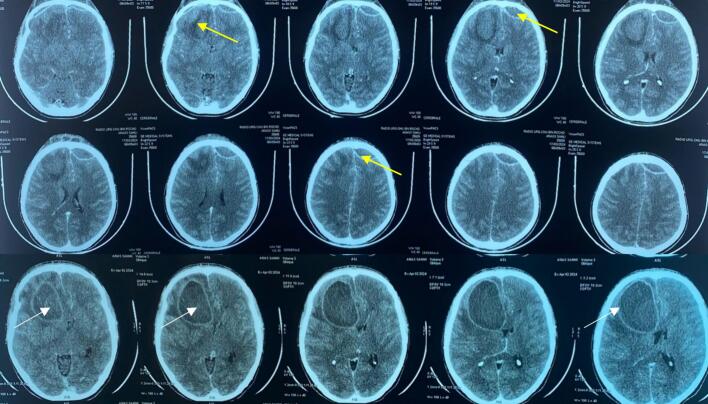
Fig. 4.
CT scan showing a bilateral frontal empyemas (yellow arrow) and a right frontal parenchymal collection (white arrow).
Medical treatment with intravenous antibiotics (Amoxicillin and Clavulanic Acid+ metronidazole) and analgesics was started immediately after the CT scan. The dosage of Amoxicillin and Clavulanic Acid was 1gx3/day. The dosage of metronidazole was 7,5 mg/kg administrated each 8 h. Antibiotics were administered intravenously for the first two weeks and per os for the last two weeks. To be noted that the patient is resistant to 3rd generation cephalosporins.
A team of ENT (ear, nose, and throat) surgeons, neurosurgeons and radiologists then decided on surgical management via a combined external and endoscopic endonasal approach. The surgery was performed on the third day following the patient's consultation. The operative procedure consisted of external drainage of the cerebral empyema and subperiosteal collection, plus endoscopic drainage of the right pansinusitis combining a middle meatotomy, anterior and posterior ethmoidectomy, sphenoidotomy and drainage of frontal sinus (Draf I).
As with all endonasal surgeries, the challenges to be taken into account in the perioperative phase were to consider any anatomical variation that could lead to a lesion of the papyraceous lamina and damage to the eyeball, or a lesion of the roof of the nasal cavity that could result in an osteomeningeal breach. Fortunately, the patient had no anatomical variations.
In terms of postoperative evolution, the patient had a positive clinical outcome, with disappearance of the right orbital swelling, rhinorrhea and facial pain in the first week post-surgery (Fig. 5).
Fig. 5.
Disappearance of the right orbital swelling.
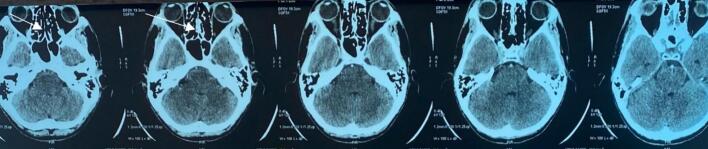
At three weeks post-op, a follow-up craniofacial CT scan showed a disappearance of paranasal sinus filling (Fig. 6), a clear regression of the subperiosteal collection, of frontal empyema and right frontal parenchymal formation (Fig. 7).
Fig. 6.
Disappearance of paranasal sinus filling.
Fig. 7.
A clear regression of the subperiosteal collection, of frontal empyema and right frontal parenchymal formation.
3. Discussion
Pott puffy tumor (PPT) is a rare but very serious complication of frontal sinusitis and more rarely in mastoiditis, featuring osteomyelitis of the frontal bone together with a subperiosteal abscess. First described by Sir Percival Pott in 1768, it was initially associated with head trauma, but is today mainly related to untreated or inadequately treated sinus infections [1,2].
The condition usually results from acute or chronic frontal sinusitis, which can lead to infection of the frontal bone. It is sometimes referred to as rhinoceros' syndrome (in reference to the forehead swelling it causes). Typical pathogens are bacteria such as staphylococcus aureus, non-enterococcal streptococci and oral anaerobes. Infection can spread by direct extension through the diploid veins, which communicate with the dural venous sinuses, leading to the formation of septic emboli. Another means of germ dissemination described is direct contamination, which can occur during superinfected open head trauma or frontal sinusitis involving the posterior wall of the frontal sinus [2,3].
Subperiosteal or subgaleal abscesses may spread to the intraorbital, interseptal or intracranial regions. Intracranial complications account for 60 % to 85 % of adult cases, and almost 100 % in children. These may include subdural or epidural empyema, frontal brain abscess in particular, but also cavernous sinus thrombosis, cortical venous thrombosis and acute meningitis [5].
PPT can also occur after chronic renal failure, cranial surgery or diabetes. It is most common in young patients, around the age of 10, and more frequently in boys. It is less common in adults, accounting for 30 % of cases [3,4].
For some authors, an erythematous, paste-like swelling of the forehead associated with fever should be considered pathognomonic for PPT [1].
But, in general, the clinical presentation of TPP is non-specific, and varies with the severity of the infection. Signs include a sensitive forehead swelling, headache, inconstant fever and purulent nasal secretions [6].
Other symptoms are related to intracranial complications (nausea, vomiting, photophobia, cranial nerve damage, convulsions, consciousness disorders) or extracranial complications (periorbital edema, skin fistulas, diplopia, exophthalmos) [7].
Diagnosis is made on the basis of emergency imaging, as the prognosis of TPP depend on rapid management. Cerebral CT with contrast injection is the examination of choice to confirm the diagnosis. It shows frontal sinusitis, osteomyelitis in the form of bone erosion, subperiosteal abscesses and extensions, notably intracranial. Magnetic resonance imaging (MRI) of the brain with contrast may represent the ideal examination if it is available and possible in an emergency, as it better studies soft tissues and intracranial complications.
However, several authors state that they believe that CT without contrast injection is largely sufficient to decide and not to delay management, especially in the emergency setting, all the more so if the patient presents neurological disorders and there are signs of intracranial hypertension [8,9].
The therapeutic management of Pott's puffy tumor is an emergency and is based on a combination of antibiotic therapy and surgical intervention. Surgical drainage and prolonged antibiotic therapy enable complete recovery in 62.5 % of cases, with mortality estimated at 12 % and neurological consequences between 12 and 40 % [14].
Several authors recommend that the ideal combination would be based on penicillin, 3rd generation cephalosporins and metronidazole. Antibiotics must be started as soon as possible after the diagnosis is first made. It is usually administered intravenously. It should be broad-spectrum, targeting the majority of germs; it is then adapted to the specific germ identified by bacteriological examination. Antibiotics should last from 4 to 8 weeks [[13], [14], [15]].
Gentamicin beads for the treatment of osteomyelitis are well known to orthopedic surgeons. Numerous reports published in orthopedic journals have described its efficacy [15].
The surgical approach is varied and may require a multidisciplinary approach involving neurosurgeons, ophthalmologists and otorhinolaryngologists.
Returning to literature, we find that it may be limited to percutaneous needle aspiration or transnasal drainage by endoscopy or trephination, sometimes including trimming of the subperiosteal/subgaleal abscess. A craniotomy may be necessary in the case of intracranial complications. Combined endoscopic and percutaneous endonasal surgery may be necessary in some cases [[10], [11], [12]].
The evolution and prognosis of PPT depend on the rapidity and quality of management. The prognosis remains favorable if management is adequate. However, neurological complications, in particular, can be functionally or even life-threatening if management is delayed [16].
4. Conclusion
Pott's puffy tumor, while rare, is a significant medical emergency that necessitates prompt recognition and intervention to prevent potentially life-threatening complications. The most common causes of PPT include sinonasal infections, particularly acute or chronic frontal sinusitis, and trauma to the forehead. Successful management requires a collaborative effort among different specialties, including neurosurgery, ENT, and radiology. According to many authors, the most effective treatment is surgery with sinus drainage and cerebral abscess drainage, combined obviously with medical treatment with antibiotics, which should be started as soon as possible.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval was provided by the authors institution.
Funding
None.
Guarantor
Saout Arrih Badr.
Research registration number
N/a.
CRediT authorship contribution statement
Saout Arrih Badr: Study concept and writing the paper
Loudghiri Myriam: Study concept and correction of the paper
Oukessou Youssef: Study concept and correction of the paper
Rouadi Sami: Study concept and correction of the paper
Abada Reda: Study concept and correction of the paper
Mahtar Mohamed: Study concept and correction of the paper.
Declaration of conflicts of interest
None.
Acknowledgement
Labib Oussama, Department of Otolaryngology, Head and Neck surgery. Ibn Rochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University. Casablanca, Morocco.
Roubal Mohamed, Department of Otolaryngology, Head and Neck surgery. Ibn Rochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University. Casablanca, Morocco.
References
- 1.ur Rehman Ayub, Muhammad Muhammad Noor, Moallam Fadi Adnan. Pott puffy tumor, a rare complication of sinusitis. Ann saudi Med. Jan-Feb 2013;33(1):79–80. doi: 10.5144/0256-4947.2012.26.5.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller Brandon. A 60-year-old man with forehead swelling. Cleve. Clin. J. Med. Feb 2016;83(2):95–96. doi: 10.3949/ccjm.83a.15011. [DOI] [PubMed] [Google Scholar]
- 3.Apostolakos D., Tang J. Image diagnosis: Pott’s puffy tumor. Perm. J. 2016;20(3):155–157. doi: 10.7812/TPP/15-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ciobanu Adela Magdalena, Rosca Tatiana, Vladescu Camelia Teodora, Tihoan Cecilia, Popa Mihaela Camelia, Boer Monica Claudia, et al. Frontal epidural empyema (Pott’s puffy tumor) associated with Mycoplasma and depression. Romanian J. Morphol. Embryol. 2014;55(3 suppl):1203–1207. [PubMed] [Google Scholar]
- 5.Perić A., Milojević M., Ivetić D. A Pott’s puffy tumor associated with epidural-cutaneous fistula and epidural abscess: case report. Balkan Med. J. May 5 2017;34(3):284–287. doi: 10.4274/balkanmedj.2016.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joo M.J., Schapira K.E. Pott’s puffy tumor: a potentially deadly complication of sinusitis. Cureus. 2019;11(12) doi: 10.7759/cureus.6351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hasan I, Smith SF, Hammond-Kenny A. Potts puffy tumour: a rare but important diagnosis. J Surg Case Rep. 2019 Apr 3;2019(4):rjz099. [DOI] [PMC free article] [PubMed]
- 8.Sharma P., Sharma S., Gupta N., Kochar P., Kumar Y. Pott puffy tumor. Proc. (Baylor Univ. Med. Cent.) 2017;30(2):179–181. doi: 10.1080/08998280.2017.11929575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tatsumi Satomi, Ri Min, Higashi Naoyuki, Wakayama Nozomu, Matsune Shoji, Tosa Mamiko. Pott’s puffy tumor in an adult. A case report and review of literature. J. Nippon Med. Sch. 2016;83(5):211–214. doi: 10.1272/jnms.83.211. [DOI] [PubMed] [Google Scholar]
- 10.El-Silimy O. Combined endonasal and percutaneous endoscopic approach to Pott’s puffy tumour. Rhinology. 1996;34:119–122. [PubMed] [Google Scholar]
- 11.Holder J., Corbin D., Marquez S., Clarke H., Walcott J., Thomas R. Pott’s puffy tumour and subdural empyema following frontal sinusitis. West Indian Med. J. 1991;40:33–36. [PubMed] [Google Scholar]
- 12.Lund V. The complications of sinusitis. In: Mackay IS, Bull TR, Kerr AG, eds. Scott Brown's Otolaryngology 5th edn. London: Butterworths, 4/13/8.
- 13.Wells R.G., Sty J.R., Landers A.D. Radiological evaluation of Pott puffy tumor. JAMA. Mar 14 1986;255(10):1331–1333. doi: 10.1001/jama.1986.03370100125030. [DOI] [PubMed] [Google Scholar]
- 14.Image Diagnosis: Pott Puffy Tumor Diane Apostolakos, MD, MS; Ian Tang, MD Perm J 2016 Summer;20(3):15–157. [DOI] [PMC free article] [PubMed]
- 15.Schein C.S., Black J.R. Implanted gentamicin beads in the treatment of osteomyelitis. A case report. J Amer Pod Med Ass. 1987;77:53–56. doi: 10.7547/87507315-77-10-563. [DOI] [PubMed] [Google Scholar]
- 16.Potts P. 1760. Observations on the Nature and Consequences of Wounds and Contusions of the Head, etc; pp. 38–58. (London) [Google Scholar]
- 17.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]