Abstract
Background:
Since the Russian full-scale invasion of Ukraine, over 10 million Ukrainians have been displaced from their homes. This has contributed to an increase in post-traumatic stress (PTS) symptoms in both refugees and internally displaced persons (IDPs). Previous research has suggested that refugees may experience higher levels of PTS due to additional stressors inherent in migration to a new country, language barriers and separation from family and social support. PTS symptoms may also be exacerbated by avoidant coping which we proposed would be more prevalent amongst refugees because of the isolating effects of migration-related stressors.
Aims:
The present study aimed to investigate the relationship between PTS symptoms, resilience and avoidant coping in refugees and IDPs. We predicted that refugees would report higher levels of PTS symptoms and use of avoidant coping strategies, and that avoidant coping would mediate the effect of resilience on PTS symptoms. We tested a moderated mediation model to examine whether this effect differed between IDPs and refugees.
Methods:
A total of 229 women (108 IDPs and 121 refugees), who were displaced after the full-scale invasion, were recruited using online platforms and volunteering centres. They completed an online questionnaire comprising measures of PTS, resilience and coping.
Results:
We found no significant differences in resilience, PTS symptoms or reported use of avoidance coping strategies between refugees and IDPs. As expected, avoidance coping mediated the negative association between resilience and PTS symptoms, but no group differences in this effect were observed.
Conclusions:
Contrary to previous research, our findings indicate that PTS symptoms may be similarly problematic for refugees and IDPs. This may be due to increased time since the invasion as many refugees may have had time to adjust. Use of avoidant coping strategies may exacerbate PTS symptoms and our study highlights the need for mental health interventions aimed at reducing PTS symptoms in Ukrainian IDPs and refugees through fostering resilience and adaptive coping strategies.
Keywords: Russia-Ukraine war, avoidance coping, post-traumatic symptoms, PTSD, resilience
Introduction
Russia launched a full-scale invasion of Ukraine on February 24th, 2022, following Russia’s annexation of the Crimean Peninsula and occupation of the Eastern regions of Ukraine. Since the invasion, Russia has occupied 18% of the country (Center for Preventive Action, 2024) and launched 10,411 successful explosions (Air Raid Alert Map of Ukraine, 2024). As a result, many Ukrainian people have fled their homes, with 3.7 million becoming internally displaced persons (IDPs) within Ukraine, and 6.5 million fleeing Ukraine to various countries around the world as refugees (United Nations High Commissioner for Refugees, 2024).
The invasion has led to reports of post-traumatic stress disorder (PTSD) in the Ukrainian population (Chudzicka-Czupała et al., 2023). PTSD is a psychiatric disorder that can occur as a result of experiencing a traumatic or distressing event (American Psychiatric Association [APA], 2023). The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; APA, 2013) classifies a traumatic event as actual or threatened severe injury, death or sexual violence, which was experienced or witnessed by an individual, or occurred to a close family member or friend. Post-traumatic stress (PTS) symptoms are categorised by: (1) intrusions (recurrent distressing memories or flashbacks), (2) avoidance of internal and external stimuli associated with the traumatic event, (3) negative alterations in cognitions and mood (inability to remember an aspect of the traumatic event, negative beliefs about oneself or the world) as well as (4) alterations in arousal and reactivity (irritable behaviour, hypervigilance; APA, 2013). Lushchak et al. (2024) suggested that 58% of the Ukrainian population meet criteria for PTSD diagnosis, with Chudzicka-Czupała et al. (2023) reporting an incidence of 73%, of which 64% were IDPs. In refugees, 62% to 73% met the cut-off point for PTSD diagnosis (Długosz, 2023; Lushchak et al., 2024).
The biggest predictor of PTSD in Ukrainians is exposure to the war. Those with higher exposure to war-related stressors are more likely to meet criteria for PTSD (Hamama-Raz et al., 2022; Karatzias et al., 2023). These stressors include, but are not limited to, hearing or seeing bombing or artillery fire; witnessing the destruction of local infrastructure; displacement; being unable to access essential healthcare or necessities like food, water, electricity or heating; living in occupied territories; being shot at by the enemy forces; and knowing someone who was physically hurt in the war or whose belongings were destroyed.
Apart from war-related trauma, other factors can also contribute to the development of PTS symptoms. As they flee their homes to seek safety, both IDPs and refugees report higher levels of anxiety associated with the duration of the trip and the number of days spent at the transit centre (Rizzi et al., 2022). Nonetheless, Ukrainian refugees are found to have significantly higher levels of stress and trauma-related symptoms than non-displaced people (Boiko et al., 2023) and IDPs (Kurapov et al., 2023), possibly due to additional post-migration stressors that refugees face during the integration process. Hynie (2017) lists socioeconomic hardship, unemployment, unstable housing conditions, language barriers, discrimination, social isolation and uncertainty about their migratory status as frequent stressors that can hinder refugees’ recovery from the traumatic experiences. For example, language acquisition plays a crucial role in refugees’ ability to adapt to a new environment in their host country (Beiser & Hou, 2001; Długosz, 2023). Poor language skills can restrict work opportunities to jobs that do not match a refugee’s skills and qualifications, and in turn led to lower psychological well-being (Bridekirk & Hynie, 2020; Mazhak et al., 2023),
Furthermore, refugees who have no social support network or have been separated from their family have more PTS symptoms (Ahmad et al., 2019; Miller et al., 2018; Schweitzer et al., 2006). Indeed, 34% of Ukrainian refugees have reported that family was an important part of coping with the stresses of war (Oviedo et al., 2022). However, only a small proportion of these reported they had contacts in the host countries, as only 12% were being assisted by friends or relatives (Oviedo et al., 2022). Due to Ukraine’s travel restrictions abroad for men of military age, many families have been separated, with only 20% of Ukrainian refugees in Krakow and 37% of refugees in Vienna living together with their spouse or partner (Kohlenberger et al., 2023). In comparison, 78% of IDPs in Ukraine have been registered as a family who live together in one household (Information and Computing Center of the Ministry of Social Policy of Ukraine [ICCMSPU], 2024). Therefore, IDPs are more likely to have a stronger social support network, retain more aspects of their previous life and, as a result, have more protective factors than refugees. Furthermore, due to Ukraine’s travel restrictions for men of the conscription age, the majority (70%) of refugees are women (Lauren & Dumont, 2023), who appear to be more susceptible to PTSD than men (Chudzicka-Czupała et al., 2023; Długosz, 2023) and women who have children under 16 years old have an elevated risk (Hamama-Raz et al., 2022).
However, while over 70% of people worldwide report having experienced at least one traumatic event in their lifetime (Benjet et al., 2016), not everyone develops PTSD (Ozer et al., 2003). Resilience has been identified as the key protective factor (Thompson et al., 2018), but there is considerable heterogeneity in how resilience is conceptualised, defined and measured (Kalisch et al., 2017). While some studies see resilience as a personality trait (Fletcher & Sarkar, 2013), more recent research has moved towards seeing it as a dynamic process that can change overtime (Snijders et al., 2018). In the present study, we adopt the following definition of resilience by the American Psychological Association (2018): the process and outcome of effectively adapting to stressful experiences through mental, emotional and behavioral adjustment to external and internal demands. Resilience is consistently found to be negatively associated with PTS in many contexts, for instance in Nepalese psychiatry hospital patients (Dhungana et al., 2022), Swiss Alpine rescuers (Mikutta et al., 2022), survivors of natural disasters (Yang & Bae, 2022) and Syrian war asylum-seekers (Maria et al., 2021). In the context of the present Ukrainian population, resilience is related to lower psycho-emotional deterioration (Kurapov et al., 2022), and fewer PTS symptoms 6-month after the full-scale invasion (Kurapov et al., 2023).
Resilience is also associated with coping strategies, the cognitive and behavioural efforts utilised to manage internal and external demands of a stressful event (Folkman & Moskowitz, 2004). Coping strategies can be categorised as emotion-focussed (managing emotional responses to stressors), problem-focussed (directly addressing the problem causing the stress) and avoidant (evading the problem and associated emotions). These have also been conceptualised as adaptive, or approach, and maladaptive, or avoidant, coping (Campos et al., 2004; Carver et al., 1989). Adaptive coping involves direct action, reappraisal, regulated emotional expression and controlled self-discipline. Conversely, maladaptive, or avoidant, coping includes dysfunctional strategies such as rumination and venting, and behaviours like withdrawal, social isolation and substance use (Campos et al., 2004). Higher levels of trauma have been reported in Ukrainians who used strategies such as giving up and taking sedatives (Długosz, 2023) and avoidant coping is associated with lower resilience in Ukrainian civilians (Kurapov et al., 2022).
Overall, evidence suggests that resilience and coping strategies can influence PTSD development in the acute aftermath of trauma. Thompson et al. (2018) found that social withdrawal, a maladaptive avoidance coping strategy, mediated the relationship between resilience and PTSD symptoms and suggested that people with lower resilience were more likely to use avoidant coping and have increased PTSD symptoms as a result. The present study tests this proposal in Ukrainian refugees and IDPs. The results have potential to inform interventions to target PTS symptoms through resilience building and fostering more adaptive coping strategies. This is important because traditional PTSD interventions such as Cognitive Behavioural Therapy, are suggested to desensitise individuals to actual dangers if a threat situation is ongoing (Ennis et al., 2021). We aimed to examine how the relationship between resilience, avoidant coping and PTS symptoms may vary between refugees and IDPs, given that refugees have been suggested to have higher levels of PTS than IDPs due to additional post-migration stressors (Kurapov et al., 2023). We proposed the following hypotheses:
IDPs will report lower post-traumatic stress symptoms than refugees.
Resilience will be negatively associated with PTS symptoms in both IDPs and refugees.
Avoidant coping strategies will mediate the relationship between resilience and PTS symptoms in both IDPs and refugees.
Migration status (refugee vs. IDP) will moderate the relationship between resilience and avoidant coping strategies.
Method
Participants
For the planned analysis, a power analysis conducted using G*Power 3.1.9.7 (Faul et al., 2009) suggested that an overall sample size of 178 was needed for a medium effect size according to Cohen’s (1988) criteria. For between-subjects analysis, a sample size of 172 participants in each group was required. We recruited women aged 18 years or older who had been displaced internally or became refugees abroad after the invasion on 24th of February, 2022. Men who are eligible for the draft are prevented from leaving Ukraine, therefore we included only women in the present study.
Data was collected between October and December 2023. Two hundred and ninety participants were recruited from adverts placed in social media groups, refugee group chats and volunteering centres in Ukraine. Sixty-one participants were excluded due to incomplete data, leaving 229 for analysis (refugees N = 121, Mage = 36.45, SD = 12.35; IDPs N = 108, Mage = 41.75, SD = 13.74). The groups significantly differed in age, t(227) = −3.06, p < .002, d = −0.04. Categorical socio-demographic data are summarised in Table 1. Comparisons were made using Chi-square tests.
Table 1.
Socio-demographic data and significance values for between group differences.
| Socio-demographic factor | Refugees | IDPs | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | p | ||
| Time since displacement (months) | <3 | 1 | 0.8 | 4 | 3.7 | .21 |
| 3–6 | 2 | 1.7 | 3 | 2.8 | ||
| 7–12 | 5 | 4.1 | 9 | 8.3 | ||
| >12 | 113 | 93.4 | 92 | 85.2 | ||
| Relationship status | Single | 26 | 21.5 | 16 | 14.8 | .06 |
| In a long-term relationship | 20 | 16.5 | 23 | 9.6 | ||
| Married | 57 | 47.1 | 47 | 43.5 | ||
| Divorced | 13 | 10.7 | 12 | 11.1 | ||
| Widowed | 0 | 0.0 | 5 | 4.6 | ||
| Other | 5 | 4.1 | 5 | 4.6 | ||
| Children | No children | 43 | 35.5 | 22 | 20.4 | .002 |
| Child under 16 years | 54 | 44.6 | 42 | 38.9 | ||
| Child over 16 years | 24 | 19.8 | 42 | 38.9 | ||
| More than one child | 0 | 0.0 | 2 | 1.9 | ||
| Separated from family | No | 5 | 4.1 | 10 | 9.3 | .18 |
| Yes | 116 | 95.9 | 98 | 90.7 | ||
| Education | Basic secondary | 0.0 | 0.0 | 1 | 0.9 | .12 |
| Complete secondary | 13 | 10.7 | 5 | 4.6 | ||
| Professional-technical/special | 25 | 20.7 | 23 | 21.3 | ||
| Bachelor’s degree | 39 | 32.2 | 30 | 27.8 | ||
| Master’s degree | 30 | 24.8 | 43 | 39.8 | ||
| PhD/Doctorate | 5 | 4.2 | 1 | 0.9 | ||
| Two or more HE diplomas | 9 | 7.4 | 5 | 4.6 | ||
| Ukraine region of origin | Dnipro | 8 | 6.6 | 3 | 2.8 | .01 |
| Donetsk | 11 | 9.1 | 20 | 18.5 | ||
| Zaporizhzhia | 52 | 43.0 | 49 | 45.4 | ||
| Kyiv | 18 | 14.9 | 7 | 6.5 | ||
| Luhansk | 3 | 2.5 | 11 | 10.2 | ||
| Lviv | 1 | 0.8 | 0 | 0.0 | ||
| Mykolayiv | 3 | 2.5 | 3 | 2.8 | ||
| Odesa | 2 | 0.8 | 2 | 1.9 | ||
| Poltava | 3 | 2.5 | 0 | 0.0 | ||
| Sumy | 7 | 5.8 | 0 | 0.0 | ||
| Kharkiv | 8 | 6.6 | 6 | 5.6 | ||
| Kherson | 2 | 1.7 | 7 | 6.5 | ||
| Khmelnytskyi | 1 | 0.8 | 0 | 0.0 | ||
| Cherkasy Chernihiv | 11 | 0.80.8 | 00 | 0.00.0 | ||
| Current living conditions | Refugee camp | 0 | 0.0 | 1 | 0.9 | <.001 |
| Host family | 14 | 11.6 | 7 | 6.5 | ||
| Shared accommodation provided by the government or other agency | 8 | 6.6 | 4 | 3.7 | ||
| Shared accommodation paid for by yourself | 6 | 5.0 | 11 | 10.2 | ||
| Private accommodation provided by the government or other agency | 64 | 52.9 | 1 | 0.9 | ||
| Private accommodation paid for by yourself | 26 | 21.5 | 69 | 63.9 | ||
| Other | 3 | 2.5 | 15 | 13.9 | ||
| Job satisfaction before displacement | No job | 21 | 17.4 | 22 | 20.4 | .76 |
| Completely dissatisfied | 1 | 0.8 | 1 | 0.9 | ||
| More or less satisfied | 26 | 21.5 | 18 | 16.7 | ||
| Quite satisfied | 47 | 38.8 | 48 | 44.4 | ||
| Very satisfied | 26 | 21.5 | 19 | 17.6 | ||
| Job satisfaction after displacement | No job | 62 | 51.2 | 55 | 50.9 | .01 |
| Completely dissatisfied | 23 | 19.0 | 6 | 5.6 | ||
| More or less satisfied | 22 | 18.2 | 24 | 22.2 | ||
| Quite satisfied | 10 | 8.3 | 20 | 18.5 | ||
| Very satisfied | 4 | 3.3 | 3 | 2.8 | ||
| Refugee country of residence | Germany | 74 | 61.2 | |||
| UK | 20 | 16.5 | ||||
| Poland | 5 | 4.1 | ||||
| Lithuania | 2. | 1.7 | ||||
| Belgium | 3 | 2.5 | ||||
| France | 3 | 2.5 | ||||
| Norway | 3 | 2.5 | ||||
| Czech Republic | 3 | 2.5 | ||||
| Austria | 1 | 0.8 | ||||
| Italy | 1 | 0.8 | ||||
| Estonia | 1 | 0.8 | ||||
| Ireland | 1 | 0.8 | ||||
| Latvia | 1 | 0.8 | ||||
| Sweden | 1 | 0.8 | ||||
| Slovakia | 1 | 0.8 | ||||
| Cyprus | 1 | 0.8 | ||||
| Refugee language proficiency | None | 30 | 24.8 | |||
| Beginner | 52 | 43 | ||||
| Intermediate | 25 | 20.7 | ||||
| Advanced | 2 | 1.7 | ||||
| Proficient/fluent | 3 | 2.5 | ||||
Significant effects indicated in bold font.
Materials and procedure
Ethical approval was obtained from the authors’ psychology ethics and integrity committee. Data was collected via an online questionnaire and participants were required to read details of the study and check a box giving informed consent before the survey would commence. The survey was administered in Ukrainian. After collecting the data in Table 1, social support was assessed with the question What is the level of your social support (i.e. people around you or who you can easily contact that are supportive)? Followed by three response options, coded 0 to 2 as below:
0. I do not have anyone to talk to
1. I have a few people I could talk to in my city of residence
2. I have lots of people I could talk to in my city of residence
Exposure to war was measured by asking To what extent did you have immediate contact with the war prior to leaving your home? Followed by three response options:
0. I did not come into contact with the war at all
1. I had indirect contact with the war (e.g. my city has been shelled; I have spent some time in a bomb shelter but have not been impacted directly; I know someone who have experienced a shelling attack or had their home and belongings destroyed, etc.)
2. I came into direct personal contact with war (e.g. I have experienced a direct shelling attack; I had my home and belongings damaged, I or someone I know have been injured, I have lost a family member or a relative, my city has been occupied, etc.)
Participants then completed the following standardised measures:
Brief Resilience Scale (BRS, Smith et al., 2008) is a 6-item self-report questionnaire used to measure the ability to recover from stressful or traumatic events. Items such as ‘I have a hard time making it through stressful events’ are responded to on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), giving a maximum score of 60. The Ukrainian version of the BRS was used (Kurapov et al., 2023). The scale showed good reliability (α = .72).
PTSD Checklist for DSM-5 (PCL-5, Blevins et al., 2015) is a 20-item self-report measure, which assesses the severity of the post-traumatic stress disorder symptoms present in the DSM-5 (APA, 2013). Items such as ‘In the past month, how much were you bothered by repeated, disturbing, and unwanted memories of the stressful experience?’ are filled out using a 5-point Likert scale (0 = not at all to 4 = extremely), obtaining a maximum score of 80. The Ukrainian version of the PCL-5 was used (Bezsheiko, 2016). The questionnaire showed high reliability in this sample (α = .92).
Brief Coping Orientation to Problems Experienced Questionnaire (Brief-COPE, Carver, 1997) is a 28-item questionnaire, measuring 14 coping strategies, which can be measured separately, or as two overarching coping styles: approach (or adaptive) and avoidant (or maladaptive; Eisenberg et al., 2012). These two subscales can be further divided into: active coping, emotional coping, use of informational support, planning, positive reframing and acceptance (for approach coping); and venting, self-blame, self-distraction, denial, substance use and behavioural disengagement (for avoidant coping). Additionally, it measures humor and religion as coping strategies that do not fall within either style. Each coping strategy subscale is comprised of 2 statements, such as ‘I’ve been turning to work or other activities to take my mind off things’, which are responded to on a 4-point Likert scale (1 = I have not been doing this at all to 4 = I have been doing this a lot). The Ukrainian version of the Brief-COPE was used (Mazhak et al., 2023). Due to the focus of the study, only the avoidant coping subscale was included in the analysis and the score computed as the mean response to relevant items. This subscale showed low, but still acceptable, reliability (α = .65), its six additional subscales reducing overall unidimensionality (Field, 2009).
Results
All data analyses were conducted using SPSS v 28.0.1.1. Descriptive statistics are presented in Table 2. Our Hypothesis 1 predicted that refugees would present higher levels of PTS symptoms. However, the only significant difference observed between groups was for exposure to war, where IDPs reported higher levels.
Table 2.
Descriptive statistics and comparison between groups.
| Variable | IDPs | Refugees | Compared | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| PTS symptoms | 34.8 | 15.7 | 37.3 | 15.5 | t(227) = 1.20, p = .23, d = .16 |
| Resilience | 2.5 | 0.7 | 2.6 | 0.6 | t(227) = 1.10, p = .28, d = .15 |
| Social support | 1.12 | 0.65 | 1.18 | 0.65 | t(227) = 0.72, p = .48, d = .10 |
| Exposure to war | 2.44 | 0.59 | 2.11 | 0.66 | t(227) = 4.28, p < .001, d = .54 |
| Avoidant coping | 26.4 | 5.5 | 26.4 | 5.1 | t(227) = 0.02, p = .99, d = .002 |
Correlations between key measures are shown in Table 3. Consistent with Hypothesis 2, PTS symptoms was negatively correlated with resilience. avoidance coping showed a positive association with PTS and a negative association with resilience in both groups. PTS symptoms was negatively associated with social support in refuges only.
Table 3.
Bivariate correlations between key variables for both groups. Refugee data above the diagonal, IDP data below diagonal.
| PTS | Resilience | Avoidance | War exposure | Social support | |
|---|---|---|---|---|---|
| PTS | – | −.40** | .46** | .16 | −.27** |
| Resilience | −.35** | – | −.18* | −.19* | .18* |
| Avoidance | .51** | −.23** | – | −.11 | −.06 |
| War exposure | .15 | .03 | .12 | – | −.11 |
| Social support | .03 | .19* | −.01 | −.04 | – |
Sig. at p = .05. **Sig. at p = .01.
Table 4 presents the results of hierarchical linear regression on PTS symptoms. The first block comprised age, education, social support, resilience, migration status (refugees coded 0 and IDPs coded 1) and exposure to war. In the second block, avoidant coping was added. Other factors shown in Table 1 were not included in the regression due to their multiple nominal categories and small numbers in many cases. Resilience presented a significant negative effect, and a significant effect of exposure to war was also observed. Migration status also presented a significant effect. Model 2 accounted for a significantly higher level of variance, ΔR2 = .19, F(1;214) = 63, p < .001, and a decreased β-value for resilience suggested a possible mediating effect of avoidant coping, as predicted.
Table 4.
Results of linear regression on PTS symptoms (full sample, N = 229).
| Model | 95% CI | Adj. R2 | ||||
|---|---|---|---|---|---|---|
| St. β | p | Lower | Upper | |||
| 1. | Age | .04 | .51 | −.10 | .20 | |
| Education | .05 | .43 | −.83 | 1.92 | ||
| Social support | −.06 | .32 | −4.50 | 1.48 | ||
| Exposure to war | .12 | .06 | −.14 | 6.13 | .15 | |
| Migration status | −.15 | .02 | −8.59 | −.70 | ||
| Resilience | −.34 | <.001 | −11.61 | −5.34 | ||
| 2. | Age | .10 | .09 | −.02 | .25 | |
| Education | .06 | .29 | −.56 | 1.86 | ||
| Social support | −.07 | .21 | −4.34 | .95 | ||
| Exposure to war | .12 | .03 | .21 | 5.75 | .33 | |
| Migration status | −.15 | .01 | −8.25 | −1.27 | ||
| Resilience | −.24 | <.001 | −8.77 | −3.09 | ||
| Avoidant coping | .44 | <.001 | .98 | 1.63 | ||
Further regression analyses by group were conducted to examine the main effect of migration status (see Table 5). In both cases the addition of avoidance coping at stage 2 significantly increased the variance in PTS symptoms explained: refugees ΔR2 = .17, F(1, 1, 114) = 32.40, p < .001; IDPs ΔR2 = .18, F(1;101) = 29.60, p < .001. Resilience showed a significant negative effect on PTS in both groups, in line with Hypothesis 2. Avoidance coping presented a positive effect in both groups. Social support presented a significant negative effect for refugees in model 1, but this was eliminated once avoidance coping was added at model 2. A positive effect was observed for exposure to war in refugees in model 2.
Table 5.
Results of linear regression by group.
| Model | Refugees (n = 121) | IDPs (n = 108) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| St. β | p | 95% CI | St. β | p | 95% CI | ||||||
| Lower | Upper | Adj. R2 | Lower | Upper | Adj. R2 | ||||||
| 1. | Age | −.04 | .63 | −.27 | .16 | .07 | .44 | −.13 | .29 | ||
| Education | .20 | .02 | .28 | 3.81 | −.08 | .37 | −3.26 | 1.23 | |||
| Social support | −.23 | .01 | −9.46 | −1.48 | .09 | .34 | −2.27 | 6.61 | |||
| Exposure to war | .11 | .18 | −1.29 | 6.70 | .21 | .14 | .15 | −1.33 | 8.61 | ||
| Resilience | −.32 | <.001 | −12.79 | −3.75 | −.36 | <.001 | −12.90 | −4.14 | .13 | ||
| 2. | Age | .10 | .09 | −.02 | .25 | .12 | .16 | −.05 | .32 | ||
| Education | .06 | .29 | −.56 | 1.86 | −.06 | .45 | −2.75 | 1.24 | |||
| Social support | −.07 | .21 | −4.34 | .95 | .07 | .43 | −2.37 | 5.53 | |||
| Exposure to war | .12 | .03 | .21 | 5.75 | .38 | .07 | .41 | −2.60 | 6.32 | ||
| Resilience | −.24 | <.001 | −8.77 | −3.09 | −.25 | .001 | −9.88 | −1.87 | |||
| Avoidant coping | .44 | <.001 | .98 | 1.63 | .45 | <.001 | .80 | 1.75 | .32 | ||
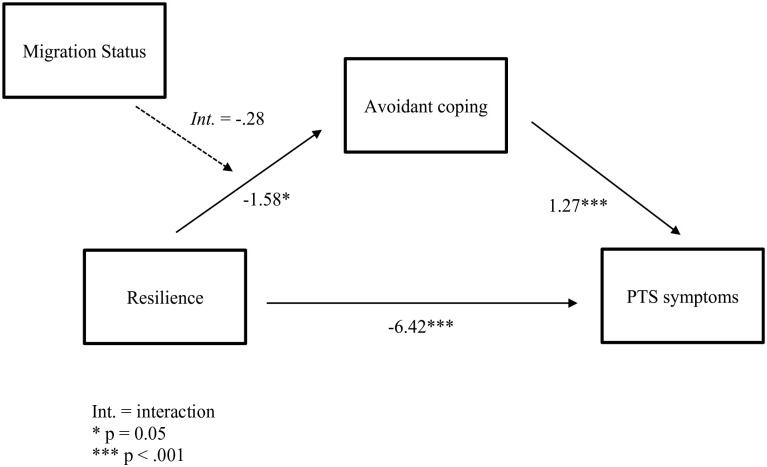
Hypothesis 3 suggested a mediating effect of avoidant coping on the relationship between resilience and PTS symptoms. Hypothesis 4 further proposed that migration status (refugees vs. IDPs) would moderate the indirect effect. We tested for moderated mediation using the PROCESS macro for SPSS, Model 7 (Hayes, 2022), controlling for exposure to war and social support. The results are shown in Figure 1.
Figure 1.
Moderated mediation model.
Note. Int. = interaction.
*p = .05. ***p < .001.
The indirect effect of resilience on PTS symptoms via avoidant coping was significant in both refugees, β = −2.02, 95% CI [−4.05, −0.30], and IDPs, β = −2.37, 95% CI [−4.35, −0.57]. This is consistent with Hypothesis 3. The moderated mediation effect of migration status however was not significant, index = −0.35, 95% CI [−2.81, 2.26], thus Hypothesis 4 is rejected.
Discussion
This was the first study to examine the effects of resilience and coping on PTS symptoms both Ukrainian refugees and IDPs. Although it was predicted that IDPs would report lower PTS symptoms than refugees, the groups did not differ significantly in this respect. However, both IDPs and refugees with higher resilience had lower PTS symptoms, as expected. A mediating effect of avoidant coping on the negative relationship between resilience and PTS symptoms was observed in both groups. However, there was no moderation effect of migration status (refugee vs. IDP) on the indirect path from resilience to PTS symptoms via avoidant coping.
Contrary to previous findings (Kurapov et al., 2023), there was no significant difference in PTS symptoms across IDPs and refugees. There are a couple of possible explanations. Firstly, in the study by Kurapov et al. (2023), the IDP sample had significantly higher resilience than refugees, whereas we found similar resilience levels in both groups. Since higher resilience is associated with fewer PTS symptoms, the differing resilience levels in the two studies could explain the variation in results. Additionally, Kurapov et al.’ (2023) study was conducted 6 months post-invasion, while the current study took place 19 months post-invasion. Over 90% of our refugee participants had been displaced for over 12 months (Table 1), and evidence suggests that refugees report better psychological well-being over time, as they adapt to new environments and learn the local language (Mazhak et al., 2023). They also build stronger social networks (Brewin et al, 2000).
As expected, we found that IDPs and refugees who had higher resilience reported lower PTS symptoms. This is consistent with previous research in other contexts (Dhungana et al., 2022; Mikutta et al., 2022; Wrenn et al., 2011) and in the Ukrainian population (Eshel et al., 2023; Kurapov et al., 2023). The relationship remained significant in both groups, even in the presence of avoidance coping and when war-related experiences, social support, age and education level were controlled for. Social support was negatively associated with PTS symptoms in refugees only. IDPs continue to share a common language and often relocate alongside family or spouses, thus facing fewer challenges in maintaining community connections (ICCMSPU, 2024). As Table 1 shows, 68% of our refugee participants reported no, or beginner level, command of their host country’s language. These findings highlight refugees’ heightened need for community-building workshops and language courses that would allow them to better integrate into the host community, build stronger social networks and attract better job opportunities that would match their qualifications.
Avoidant coping was found to mediate the relationship between resilience and PTS, consistent with previous research (Thompson et al., 2018). This finding has implications for treatment of PTS symptoms in Ukrainian population. Many PTSD interventions, such as Cognitive Therapy for PTSD (Ehlers & Clark, 2000) and trauma-focussed Cognitive Behavioral Therapy (CBT; Ennis et al., 2021) consider trauma as a one-time past event and require a safe environment for treatment. However, for people living under ongoing threat, such as frequent shelling, these interventions may reduce the healthy emotional response to threat, thus desensitising individuals to actual dangers (Cohen et al., 2011; Ennis et al., 2021). The mediating effect of avoidant coping on the relationship between resilience and PTS symptoms suggests that enhancing resilience and fostering adaptive coping strategies could reduce PTS symptoms. By promoting resilience factors, like finding meaning in life (Sood et al., 2011), nurturing positive future expectations (O’Neill et al., 2020) and boosting self-efficacy through personal strengths (Kunzler et al., 2020), individuals may adopt more adaptive coping strategies. Furthermore, adaptive coping strategies could be fostered through behavioural activation training, which counters behavioural disengagement and social withdrawal (Etherton & Farley, 2020). Problem-solving training also evokes memories of successful previous attempts at problem-solving, which increases confidence and produce positive emotions (Padmanabhanunni & Pretorius, 2023). Since no moderating effect of migration status was found, focussing on building resilience and promoting adaptive coping strategies is advocated for both Ukrainian IDPs and refugees.
The study has some limitations. Firstly, all data relied on self-reports. Due to the stigma associated with mental health in Ukraine (Quirke et al., 2021), participants might have underreported their PTS symptoms. This also presents concerns about the sampling process, and whether individuals with negative views towards mental health may have chosen not to participate. Moreover, the use of snowball sampling through social media may not fully represent the broader population, as it tends to recruit within similar networks. Additionally, certain populations are much harder to reach, such as people with more severe cases of PTS or harsher experiences of war, those who might not use social media or live in rural or occupied areas. As the study looked at Ukrainian refugees across Europe, limited responses from some countries were gathered. Future research might focus on fewer countries and consider cultural differences and local attitudes towards refugees. For example, Slovakia reports significantly more negative attitudes towards Ukrainian refugees than Estonia (Kaim et al., 2024), which can contribute to post-migration stressors and affect refugees’ mental health. It would also be beneficial to explore how proximity to conflict zones influences coping mechanisms and PTS symptoms in IDPs.
Secondly, the study was somewhat underpowered. These are hard-to-reach populations often living in difficult circumstances. Moreover, only data from women was collected, as the majority of Ukrainian refugees are female. Future research could address this by considering Ukrainian men and children who may use other coping strategies (Cholankeril et al., 2023) and possess different resilience levels (Yalcin-Siedentopf et al., 2020). Lastly, although a cross-sectional design cannot establish causation, it can offer valuable insights into the interaction between variables (Hayes, 2022). Nevertheless, a longitudinal approach would better evaluate how adaptation to a new environment, language acquisition and social integration might affect PTS symptoms, resilience and coping mechanisms over time.
In conclusion, this is the first study investigating the relationship between coping, resilience and PTS symptoms in the context of the Ukraine-Russian war. The results suggest that refugees and IDPs with lower resilience are more likely to use avoidant coping strategies, which are associated with higher PTS symptoms. As such, interventions fostering resilience and addressing maladaptive coping could be utilised to indirectly reduce PTS symptoms in Ukrainian refugees and IDPs.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alison M Bacon  https://orcid.org/0000-0003-4279-3814
https://orcid.org/0000-0003-4279-3814
References
- Ahmad F., Othman N., Lou W. (2019). Posttraumatic stress disorder, social support and coping among Afghan refugees in Canada. Community Mental Health Journal, 56(4), 597–605. 10.1007/s10597-019-00518-1 [DOI] [PubMed] [Google Scholar]
- Air Raid Alert Map of Ukraine . (2024). Air Raid Alert Map of Ukraine. Retrieved April 26, 2024, from https://alerts.in.ua/en
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596 [DOI]
- American Psychological Association. (2018). APA dictionary of psychology. https://dictionary.apa.org/resilience
- Beiser M., Hou F. (2001). Language acquisition, unemployment and depressive disorder among Southeast Asian refugees: A 10-year study. Social Science & Medicine, 53(10), 1321–1334. 10.1016/s0277-9536(00)00412-3 [DOI] [PubMed] [Google Scholar]
- Benjet C., Bromet E., Karam E. G., Kessler R. C., McLaughlin K. A., Ruscio A. M., Shahly V., Stein D. J., Petukhova M., Hill E., Alonso J., Atwoli L., Bunting B., Bruffaerts R., Caldas-de-Almeida J. M., de Girolamo G., Florescu S., Gureje O., Huang Y., Lepine J. P. (2016). The epidemiology of traumatic event exposure worldwide: Results from the world mental health survey consortium. Psychological Medicine, 46(2), 327–343. 10.1017/s0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezsheiko V. (2016). Адаптація шкали для клінічної діагностики ПТСР та опитувальника “Перелік симптомів ПТСР” для української популяції. Психосоматична Медицина та Загальна Практика, 1(1), e010108. https://uk.e-medjournal.com/index.php/psp/article/view/8 [Google Scholar]
- Blevins C. A., Weathers F. W., Davis M. T., Witte T. K., Domino J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Boiko D. I., Shyrai P. O., Mats O. V., Karpik Z. I., Rahman Md. H., Khan A. A., Alanazi A. M., Skrypnіkov A. M. (2023). Mental health and sleep disturbances among Ukrainian refugees in the context of Russian-Ukrainian war: A preliminary result from online-survey. Sleep Medicine, 113, 342–348. 10.1016/j.sleep.2023.12.004 [DOI] [PubMed] [Google Scholar]
- Brewin C. R., Andrews B., Valentine J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. 10.1037//0022-006x.68.5.748 [DOI] [PubMed] [Google Scholar]
- Bridekirk J., Hynie M. (2020). The impact of education and employment quality on self-rated mental health among Syrian refugees in Canada. Journal of Immigrant and Minority Health, 53(10). 10.1007/s10903-020-01108-0 [DOI] [PubMed] [Google Scholar]
- Campos M., lraurgui J., Páez D., Velasco C. (2004). Afrontamiento y regulación emocional de hechos estresantes. Un meta-análisis de 13 estudios [Coping and emotional regulation of stress events. A meta-analysis of 13 studies]. Boletín de Psicología, 82, 25–44. [Google Scholar]
- Carver C. S. (1997). You want to measure coping but your protocol is too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver C. S., Scheier M. F., Weintraub J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283. [DOI] [PubMed] [Google Scholar]
- Center for Preventive Action. (2024, April 24). War in Ukraine. Global Conflict Tracker; Council on Foreign Relations. https://www.cfr.org/global-conflict-tracker/conflict/conflict-ukraine [Google Scholar]
- Cholankeril R., Xiang E., Badr H. (2023). Gender differences in coping and psychological adaptation during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 20(2), 993. 10.3390/ijerph20020993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chudzicka-Czupała A., Hapon N., Chiang S.-K., Żywiołek-Szeja M., Karamushka L., Lee C. T., Grabowski D., Paliga M., Rosenblat J. D., Ho R., McIntyre R. S., Chen Y.-L. (2023). Depression, anxiety and post-traumatic stress during the 2022 Russo-Ukrainian war, a comparison between populations in Poland, Ukraine, and Taiwan. Scientific Reports, 13(1), 3602. 10.1038/s41598-023-28729-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum. [Google Scholar]
- Cohen J. A., Mannarino A. P., Iyengar S. (2011). Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine, 165, 16–21. 10.1001/archpediatrics.2010.247 [DOI] [PubMed] [Google Scholar]
- Dhungana S., Koirala R., Ojha S. P., Thapa S. B. (2022). Resilience and its association with post-traumatic stress disorder, anxiety, and depression symptoms in the aftermath of trauma: A cross-sectional study from Nepal. SSM - Mental Health, 2, 100135. 10.1016/j.ssmmh.2022.100135 [DOI] [Google Scholar]
- Długosz P. (2023). War trauma and strategies for coping with stress among Ukrainian refugees staying in Poland. Journal of Migration and Health, 8, 100196–100196. 10.1016/j.jmh.2023.100196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A., Clark D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/s0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Eisenberg S. A., Shen B. J., Schwarz E. R., Mallon S. (2012). Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. Journal of Behavioral Medicine, 35(3), 253–261. [DOI] [PubMed] [Google Scholar]
- Ennis N., Sijercic I., Monson C. M. (2021). Trauma-focused cognitive-behavioral therapies for posttraumatic stress disorder under ongoing threat: A systematic review. Clinical Psychology Review, 88, 102049. 10.1016/j.cpr.2021.102049 [DOI] [PubMed] [Google Scholar]
- Eshel Y., Kimhi S., Marciano H., Adini B. (2023). Predictors of PTSD and psychological distress symptoms of Ukraine civilians during war. Disaster Medicine and Public Health Preparedness, 12(17), e429. 10.1017/dmp.2023.69 [DOI] [PubMed] [Google Scholar]
- Etherton J. L., Farley R. (2020). Behavioral activation for PTSD: A meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 14(5), 894. 10.1037/tra0000566 [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A. G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. [DOI] [PubMed] [Google Scholar]
- Field A. P. (2009). Discovering statistics using SPSS. (3rd ed.). Sage. [Google Scholar]
- Fletcher D., Sarkar M. (2013). Psychological resilience: A review and critique of definitions, concepts and theory. European Psychologist, 18(1), 12–23. 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- Folkman S., Moskowitz J. T. (2004). Coping: pitfalls and promise. Annual Review of Psychology, 55, 745–74. 10.1146/annurev.psych.55.090902.141456 [DOI] [PubMed] [Google Scholar]
- Hamama-Raz Y., Goodwin R., Leshem E., Ben-Ezra M. (2022). Can patriotism be a protective factor for symptoms of post-traumatic stress disorder? The case of the Russia – Ukraine 2022 war. Journal of Psychiatric Research, 155, 100–103. 10.1016/j.jpsychires.2022.08.016 [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (2022). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (3rd ed.). The Guilford Press. [Google Scholar]
- Hynie M. (2017). The social determinants of refugee mental health in the post-migration context: A critical review. The Canadian Journal of Psychiatry, 63(5), 297–303. 10.1177/0706743717746666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Information and Computing Center of the Ministry of Social Policy of Ukraine. (2024). Internally displaced people analytics. https://www.ioc.gov.ua/en/dashboardVpo/
- Kaim A., Kimhi S., Siman-Tov M., Bankauskaite D., Baran M., Baran T., Cosciug A., Eshel Y., Dumbadze S., Gabashvili M., Jiglau G., Kaniasty K., Koubova A., Marciano H., Renata M., Matichescu M., Naomi S., Teperik D., Sukhashvili J., Adini B. (2024). From compassion to controversy: Unraveling the impact of societal resilience on the tapestry of attitudes towards Ukrainian refugees. International Journal of Disaster Risk Reduction, 105(15), 104326. 10.1016/j.ijdrr.2024.104326 [DOI] [Google Scholar]
- Kalisch R., Baker D. G., Basten U., Boks M. P., Bonanno G. A., Brummelman E., Chmitorz A., Fernàndez G., Fiebach C. J., Galatzer-Levy I., Geuze E., Groppa S., Helmreich I., Hendler T., Hermans E. J., Jovanovic T., Kubiak T., Lieb K., Lutz B., Müller M. B. (2017). The resilience framework as a strategy to combat stress-related disorders. Nature Human Behaviour, 1(11), 784–790. 10.1038/s41562-017-0200-8 [DOI] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Ben-Ezra M., McElroy E., Redican E., Vang M. L., Cloitre M., Ho G. W. K., Lorberg B., Martsenkovskyi D., Hyland P. (2023). War exposure, posttraumatic stress disorder, and complex posttraumatic stress disorder among parents living in Ukraine during the Russian war. Acta Psychiatrica Scandinavica, 147(3), 276–285. 10.1111/acps.13529 [DOI] [PubMed] [Google Scholar]
- Kohlenberger J., Buber-Ennser I., Pędziwiatr K., Rengs B., Setz I., Brzozowski J., Riederer B., Tarasiuk O., Pronizius E. (2023). High self-selection of Ukrainian refugees into Europe: Evidence from Kraków and Vienna. PLOS ONE, 18(12), e0279783. 10.1371/journal.pone.0279783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzler A. M., Helmreich I., Chmitorz A., König J., Binder H., Wessa M., Lieb K. (2020). Psychological interventions to foster resilience in healthcare professionals. Cochrane Database of Systematic Reviews, 7(7), cd012527. 10.1002/14651858.cd012527.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurapov A., Kalaitzaki A., Keller V., Danyliuk I., Kowatsch T. (2023). The mental health impact of the ongoing Russian-Ukrainian war 6 months after the Russian invasion of Ukraine. Frontiers in Psychiatry, 14, 1134780. 10.3389/fpsyt.2023.1134780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurapov A., Pavlenko V., Drozdov A., Bezliudna V., Reznik A., Isralowitz R. (2022). Toward an understanding of the Russian-Ukrainian war impact on university students and personnel. Journal of Loss and Trauma, 28(2), 1–8. 10.1080/15325024.2022.2084838 [DOI] [Google Scholar]
- Lauren A., Dumont J.-C. (2023, May 30). What are the integration challenges of Ukrainian refugee women? The Organization for Economic Co-Operation and Development. https://www.oecd.org/ukraine-hub/policy-responses/what-are-the-integration-challenges-of-ukrainian-refugee-women-bb17dc64/#contact-d4e1456 [Google Scholar]
- Lushchak O., Velykodna M., Bolman S., Strilbytska O., Berezovskyi V., Storey K. B. (2024). Prevalence of stress, anxiety, and symptoms of post-traumatic stress disorder among Ukrainians after the first year of Russian invasion: a nationwide cross-sectional study. The Lancet Regional Health - Europe, 36, 100773. 10.1016/j.lanepe.2023.100773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maria M., Dimitra T., Mary G., Stella K., Athanasios N., Sarafis P. (2021). Depression, resilience and post traumatic stress disorder (PTSD) in asylum-seeker war refugees. Materia Socio-Medica, 33(1), 26–29. 10.5455/msm.2021.33.26-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazhak I., Paludo A. C., Sudyn D. (2023). Self-reported health and coping strategies of Ukrainian female refugees in the Czech Republic. European Societies, 26(2), 411–437. 10.1080/14616696.2023.2203230 [DOI] [Google Scholar]
- Mikutta C., Schmid J. J., Ehlert U. (2022). Resilience and post-traumatic stress disorder in the Swiss Alpine rescue association. Frontiers in Psychiatry, 13, 780498. 10.3389/fpsyt.2022.780498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A., Hess J. M., Bybee D., Goodkind J. R. (2018). Understanding the mental health consequences of family separation for refugees: Implications for policy and practice. American Journal of Orthopsychiatry, 88(1), 26–37. 10.1037/ort0000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill E., Clarke P., Fido D., Vione K. C. (2020). The role of future time perspective, body awareness, and social connectedness in the relationship between self-efficacy and resilience. International Journal of Mental Health and Addiction, 20, 1171. 10.1007/s11469-020-00434-6 [DOI] [Google Scholar]
- Oviedo L., Seryczyńska B., Torralba J., Roszak P., Del Angel J., Vyshynska O., Muzychuk I., Churpita S. (2022). Coping and resilience strategies among Ukraine war refugees. International Journal of Environmental Research and Public Health, 19(20), 13094. 10.3390/ijerph192013094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer E. J., Best S. R., Lipsey T. L., Weiss D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Padmanabhanunni A., Pretorius T. B. (2023). Cognitive adaptation to stress and trauma: The role of self-appraised problem-solving in posttraumatic stress disorder. Chronic Stress, 7. 10.1177/24705470231189980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quirke E., Klymchuk V., Suvalo O., Bakolis I., Thornicroft G. (2021). Mental health stigma in Ukraine: Cross-sectional survey. Global Mental Health, 8, e11. 10.1017/gmh.2021.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzi D., Ciuffo G., Sandoli G., Mangiagalli M., de Angelis P., Scavuzzo G., Nych M., Landoni M., Ionio C. (2022). Running away from the war in Ukraine: The impact on mental health of internally displaced persons (IDPs) and refugees in transit in Poland. International Journal of Environmental Research and Public Health, 19(24), 16439. 10.3390/ijerph192416439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweitzer R., Melville F., Steel Z., Lacherez P. (2006). Trauma, post-migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Australian & New Zealand Journal of Psychiatry, 40(2), 179–187. 10.1080/j.1440-1614.2006.01766.x [DOI] [PubMed] [Google Scholar]
- Smith B. W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Snijders C., Pries L.-K., Sgammeglia N., Al Jowf G., Youssef N. A., de Nijs L., Guloksuz S., Rutten B. P. F. (2018). Resilience against traumatic stress: Current developments and future directions. Frontiers in Psychiatry, 9, 676. 10.3389/fpsyt.2018.00676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sood A., Prasad K., Schroeder D., Varkey P. (2011). Stress management and resilience training among department of medicine faculty: A pilot randomized clinical trial. Journal of General Internal Medicine, 26(8), 858–861. 10.1007/s11606-011-1640-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson N. J., Fiorillo D., Rothbaum B. O., Ressler K. J., Michopoulos V. (2018). Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. Journal of Affective Disorders, 225, 153–159. 10.1016/j.jad.2017.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations High Commissioner for Refugees. (2024, February). Ukraine refugee crisis: Aid, statistics and news. USA for UNHCR. https://www.unrefugees.org/emergencies/ukraine/ [Google Scholar]
- Wrenn G. L., Wingo A. P., Moore R., Pelletier T., Gutman A. R., Bradley B., Ressler K. J. (2011). The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. Journal of the National Medical Association, 103(7), 560–566. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3691279/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalcin-Siedentopf N., Pichler T., Welte A.-S., Hoertnagl C. M., Klasen C. C., Kemmler G., Siedentopf C. M., Hofer A. (2020). Sex matters: stress perception and the relevance of resilience and perceived social support in emerging adults. Archives of Women’s Mental Health, 24(3), 403–411. 10.1007/s00737-020-01076-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y.-S., Bae S.-M. (2022). Association between resilience, social support, and institutional trust and post-traumatic stress disorder after natural disasters. Archives of Psychiatric Nursing, 37, 39–44. 10.1016/j.apnu.2022.01.001 [DOI] [PubMed] [Google Scholar]