Abstract
Background:
Surgical treatment of insertional Achilles tendinopathy (IAT) historically consists of Achilles tendon debridement with reattachment and excision of the posterosuperior calcaneal prominence with or without a gastrocnemius recession. Zadek osteotomy (ZO) is an alternative to an open midline splitting approach. The purpose of this study was to analyze patient-reported outcomes and complications after percutaneously performed ZO with minimum 2 years’ follow-up.
Methods:
One hundred eight cases treated with percutaneous ZO with a minimum 2-year follow-up were retrospectively reviewed. Postoperative complications and patient satisfaction were evaluated. Foot Function Index (FFI) and visual analog scale (VAS) scores were recorded at preoperative and follow-up appointments to measure patients’ functional outcomes and pain, respectively.
Results:
Mean follow-up was 41.2 months (range, 24-65). Mean age was 51.8 years (range, 28-81). The mean FFI score improved from 56.1 (range, 47-88) to 11.0 (range, 7-59) postoperatively (P < .001). The mean VAS score improved from 7.7 (range, 5-10) to 0.4 (range, 0-7) postoperatively (P < .001). The overall complication rate was 3.8% (n = 4). Of 104 cases, 98.1% of patients said they were satisfied with their procedure (n = 102) when asked if they were satisfied with their ZO and recovery.
Conclusion:
We found the percutaneous ZO to be a safe and effective intervention for treatment of IAT. At a minimum of 2-year follow-up, this intervention is associated with minimal complications, improved function, reduced pain, and a high rate of patient satisfaction.
Keywords: Haglund deformity, insertional Achilles tendinopathy, minimally invasive surgery, Zadek osteotomy
Graphical Abstract.
This is a visual representation of the abstract.
Level of Evidence: Level IV, retrospective cohort study.
Introduction
Insertional Achilles tendinopathy (IAT) is a common source of pain in the posterior heel. IAT often presents in conjunction with Haglund deformity, a posterosuperior calcaneal prominence contributing to Achilles tendon compression and worsened tendinopathy.6,42 Several treatment options have been described, yet the ideal treatment for IAT remains controversial. First-line treatment for IAT includes conservative therapies such as anti-inflammatory medications, activity limitation, physical therapy, and shoe wear modification.4,30,42,47 Pulsed ultrasound and eccentric loading therapy have demonstrated some success in this patient population.24,40 However, these nonoperative strategies fail in 20% to 40% of cases, and surgical intervention is considered. 28 Historically, surgical treatment of IAT consists of Achilles tendon debridement with reattachment as well as excision of the posterosuperior calcaneal prominence with or without gastrocnemius recession.3,13,28,37 Although this intervention has demonstrated positive outcomes, there is a prolonged recovery and return to full activity following open Achilles debridement. 28
When compared to minimally invasive surgery, open Achilles procedures have an increased risk of wound complication and infection, which can negatively affect patient recovery.7,8,17,25,31,34,48 These complications commonly include impaired wound healing, sural nerve injury, wound tenderness, shoe wear irritation, infection, pain, prolonged recovery time, and skin sensitivity. Leitze et al 25 demonstrated a decrease in infection (3 vs 12%), nerve (10 vs 18%), and wound (7% vs 18%) complications following endoscopic retrocalcaneal decompression. Gutteck et al 17 reported no wound complications with percutaneous calcaneal osteotomy, a significant improvement in direct comparison to the 15.5% associated with open calcaneal osteotomies. Similarly, Nordio et al 31 observed no wound complications following percutaneous Zadek Osteotomy, whereas a wound complication rate of 10.9% has been cited in the open procedure. 15
The Zadek osteotomy (ZO) is an alternative surgical procedure to Achilles tendon debridement for management of IAT. Zadek originally described the procedure in 1939 as a treatment for achillobursitis; indications for ZO have since been expanded to include IAT.15,22,46,51 Through this osteotomy, the posterosuperior calcaneal tuberosity is rotated anteriorly, decreasing impingement on and mechanical irritation of the Achilles tendon insertion. The osteotomy moves the Achilles tendon insertion proximal to simultaneously decrease the tension of the Achilles at its insertion and increase ankle dorsiflexion, without disrupting the natural fibers of the tendon.1,21,31,44 A mean improvement of 7.27 degrees (54% improvement) ankle dorsiflexion has been observed after ZO. 46
Initial studies demonstrated favorable outcomes with ZO; however, they were performed with a large, lateral incision and commonly cited complications including wound dehiscence, infection, and sural nerve injury.7,13-15,22,26,44,46,51 Over the last decade, many have begun to reinvestigate this technique.44-46 Recent studies have shown improved functional outcomes and low complication rates with the percutaneous ZO approach, although limited data exist on the percutaneous technique.1,7,9,31,35
Nordio et al 31 recently reported significant improvements in visual analog scale (VAS) and Foot Function Index (FFI) scores and a high rate of patient satisfaction following percutaneous ZO. Notably, this study had a small sample size (n = 26) and minimum follow-up of only 6 months. To our knowledge, no study has evaluated minimum 2-year outcomes of percutaneous ZO with a larger sample size. The purpose of this study was to analyze outcomes of the percutaneous ZO for IAT with a minimum 2-year follow-up. We hypothesized that this approach would show improved patient pain and functional outcomes with low complication and revision rates.
Methods
Following IRB approval, a retrospective review of prospectively collected data from 2 separate institutions was performed for patients who underwent percutaneous ZO between October 2017 and July 2021. Record review was performed by fellowship-trained orthopaedic foot and ankle surgeons. Current Procedural Terminology code 28300 was used. Data were stored on a secure OneDrive for further analysis. All identifying patient information was absent throughout the analysis process.
All patients who presented with symptoms consistent with IAT or Haglund deformity, or both, had failed an appropriate (3- to 6-month) course of nonoperative management, and had no history of Achilles surgery were considered candidates for percutaneous Zadek osteotomy.
A percutaneous ZO was performed by the senior authors on all patients who met inclusion criteria. The senior authors are board-certified, fellowship-trained orthopaedic foot and ankle surgeons with extensive percutaneous foot and ankle surgery experience. All cases had a minimum 2-year follow-up. The authors did not routinely measure X/Y ratio on radiographs to determine candidates for percutaneous ZO intervention, nor were magnetic resonance images routinely obtained unless there was evidence of Achilles midsubstance tendinitis/tendinosis on examination.
Indications for surgery included patients who presented with insertional Achilles tendinopathy symptoms, with or without Achilles insertional intratendinous calcifications, that failed nonoperative treatment, and who would normally be a candidate for open Achilles insertional debridement and repair.
Contraindications of the percutaneous Zadek osteotomy were similar to those of traditional open insertional debridement, which include but are not limited to active infection, poor vascularity, smoking, and diabetes with an HbA1c above 7.5. We excluded from this study population those patients who presented for revision cases of open Achilles reconstruction treated with the percutaneous ZO.
Patient sex, age, and pertinent comorbidities were recorded. Postoperative complications and patient satisfaction following intervention were evaluated by survey. FFI scores were collected pre- and postoperatively to measure function. On the FFI, patients are surveyed on 23 items across subscales of pain, disability, and activity limitation. Higher scores are associated with higher degrees of limitation. Many previous studies have used the FFI total and subscale scores to measure outcomes following interventions for IAT.2,8,31,34 VAS scores were collected to measure pain. Patients were surveyed on pain frequency and intensity. The VAS provides a quantitative measurement of pain; higher scores are associated with an increased level of pain. Both scoring systems were obtained at all postoperative appointments and stored on the electronic medical record. Satisfaction was similarly surveyed at postoperative follow-ups. Initial postoperative visits were at 2 weeks, 6 weeks, 12 weeks, 6 months, 12 months, and then yearly thereafter. Preoperative and final follow-up scores were used for paired statistical analysis. All patients who completed the follow-up were asked if they were satisfied with their ZO and recovery, which was simply a yes or no question.
Surgical Technique
The percutaneous ZO procedure was performed through a 5-mm incision. 21 Patients received a lower extremity popliteal and adductor canal or saphenous nerve block. The procedure was performed under IV propofol sedation or general anesthesia. No tourniquet was used for the procedure. The patient was positioned in the lateral decubitus position with the operative leg off of the end of the bed resting on the mini-C-arm with a small 3-towel bump (Figure 1). The nonoperative leg was flexed out of the field and taped to the bed.
Figure 1.

Position of the leg in the lateral position on the mini-C-arm to perform the Zadek osteotomy. 21
A wire was used to mark out the ~10-mm dorsal closing wedge osteotomy on the lateral calcaneus with use of lateral fluoroscopy. 31 The safe zone over the calcaneal tuberosity, as defined by Talusan et al, 43 was identified under fluoroscopic imaging. A small 5-mm lateral calcaneal incision was made at the apex of the Zadek osteotomy, ~5-8 mm from the plantar cortex just anterior to the plantar fascia origin at the calcaneal tuberosity. A blunt straight hemostat was used to spread down to bone. Next, a 3 × 30-mm Shannon burr (Novastep, Englewood Cliffs, NJ) with a 4:1 reducer set at 6000 rpm was advanced into the lateral calcaneus at the apex of the osteotomy; position was confirmed on lateral fluoroscopy. Copious refrigerated (37 °F) normal saline via bulb syringe was used to cool the burr at all times so as to prevent skin and bone thermal injury. 36 Burring was also paused every 3-4 seconds to allow the burr to cool and clean the cutting flutes if necessary. Optionally, Kirschner wires may be placed as a guide for the burr to prevent the surgeon from straying from the desired osteotomy trajectory as described by Kaplan et al 21 (Figure 2A and B).
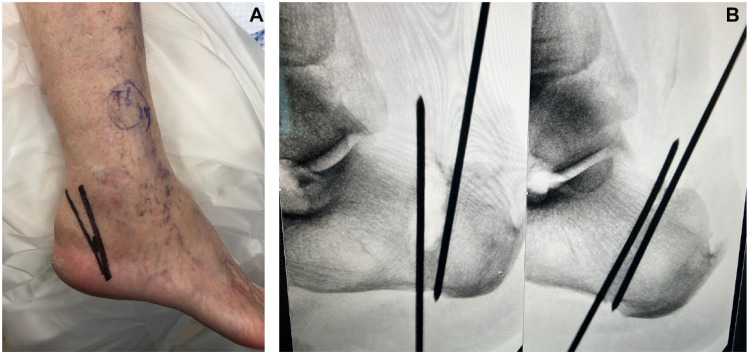
Figure 2.
(A) Clinical and (B) fluoroscopic visualization of K-wire placement and cut guide for percutaneous Zadek osteotomy as described by Kaplan et al. 21
Once the first limb of the osteotomy was completed, the Shannon burr was run to shave a dorsal 10-mm wedge (Figure 3A and B). Alternatively, the Shannon burr could be run to create a separate trajectory for the second limb of the osteotomy, and then the intervening remaining bone could be removed with a pituitary rongeur or hemostat. In the event the patient had a true Haglund deformity, the osteotomy wedge could be moved posteriorly to remove the Haglund deformity as part of the dorsal wedge resection. The osteotomy was then reduced with maximal ankle dorsiflexion. Two vertically stacked guidewires were placed with fluoroscopic guidance across the osteotomy from the posterior calcaneal tuberosity into the subchondral bone of the posterior facet. Two 7.0-mm headless compression screws were advanced across the osteotomy with the ankle kept in maximal dorsiflexion. The dorsal screw was placed first to compress the osteotomy. The second screw was placed plantar to protect the plantar hinge (Figure 4). Implant position was confirmed on lateral and Harris axial fluoroscopic views of the calcaneus. Incisions were irrigated with normal saline and closed with 2-0 nylon sutures (Figure 5). A soft dressing was placed. The ankle and foot were immobilized in a short (midcalf) controlled ankle movement boot (CAM). All patients were discharged on the same day of surgery.
Figure 3.
Schematic drawing of cut technique using quadrants in the (A) sagittal and (B) axial plane as described by Kaplan et al. 21
Figure 4.

Final fluoroscopic imaging, demonstrating placement of 2 headless cannulated compression screws, perpendicular to the percutaneous Zadek osteotomy as described by Kaplan et al. 21
Figure 5.

Clinical visualization of final closure following Zadek osteotomy.
Postoperative Management
At the initial 2-week postoperative visit, sutures were removed, and patients were allowed full weightbearing in a CAM boot. Patients were given a prescription for physical therapy to start 2 weeks postoperatively for gait training, range of motion exercises, Achilles strengthening, and soft tissue modalities. Patients who underwent right-sided ZO were not allowed to drive for 6 weeks following surgery. At 6 weeks postoperatively, patients were transitioned out of the CAM boot into supportive sneakers as tolerated. Thereafter, follow-up visits included weightbearing lateral foot radiographs and clinical evaluation at 3 months, 6 months, 12 months, and 2 years after surgery. Return to low-impact activities was allowed at 6 weeks postoperatively and high-impact activities were allowed at 3 months postoperatively as tolerated. Patients were counseled to expect heel soreness/pain for 6 weeks to 3 months postoperatively.
Statistical Analysis
Outcome measures (FFI and VAS scores) were compared between preoperative and last follow-up appointments (minimum 2 years) to evaluate clinical function and pain.11,39,40 Changes in pain, disability, activity limitation, and total FFI were analyzed using 2-tailed, paired t test whereby P <.05 was considered significant. Preoperative and postoperative VAS pain scores were similarly analyzed. Patients who were lost to follow-up before 2 years postoperatively were excluded from all analysis. IBM SPSS Statistics 28 (IBM, Armonk, NY) software was used for analyses.
Results
A total of 108 cases in 108 patients were identified as receiving a percutaneous ZO within the study time frame. There were 4 patients (2 male, 2 female) who were lost to follow-up and thereby excluded from the remainder of the analysis in accordance with per-protocol evaluation, leaving 104 patients for evaluation. The remaining 104 patients had a mean follow-up of 41.2 months (range, 24-65 months). Patients included 37 males (35.6%) and 67 females (64.4%) with a mean age of 51.8 years (range, 28-81 years) (Table 1).
Table 1.
Summary of Study Population Demographic Information. a
| Characteristic | Value |
|---|---|
| Follow-up duration, mo | 41.2 ± 13.1 (24-65) |
| Age, y | 51.8 ± 11.2 (28-81) |
| Sex | |
| Male | 37 (35.6) |
| Female | 67 (64.4) |
| Diabetes | 8 (7.7) |
| Rheumatoid arthritis | 1 (1.0) |
| Psoriatic arthritis | 1 (1.0) |
| Lupus | 1 (1.0) |
Continuous data are reported as mean ± SD (range). Categorical data are reported as total (percentage of study population).
Following intervention, mean pain, disability, activity limitation, and total FFI scores were significantly improved at final follow-up (P < .001). FFI pain scores improved from 21.3 (range, 14-42) to 3.2 (range, 2-22) (P < .001). FFI disability scores improved from 16.9 (range, 12-34) to 4.2 (range, 2-21) (P < .001). FFI activity limitation scores improved from 17.7 (range, 8-22) to 3.7 (range, 1-16) (P < .001). Mean VAS score also significantly improved from preoperative to final follow-up appointment; VAS scores improved from 7.7 (range, 5-10) to 0.4 (range, 0-7) (P < .001) (Figure 6). Cohen d effect size was >2 for each comparison, indicating a very strong treatment effect. In addition, 103 of 104 patients (99.0%) demonstrated an improvement in VAS score above the minimal clinically important difference (MCID) (Table 2). 5
Figure 6.

FFI and VAS outcome scores relative to follow-up duration.
Table 2.
Functional and Subjective Pain Pre- and Postoperative Scores as Evaluated by FFI and VAS, Respectively. a
| Preoperative Mean | Postoperative Mean | P Value | Effect Size | |
|---|---|---|---|---|
| FFI total | 56.1 ± 5.9 (47-88) | 11.0 ± 5.1 (7-59) | <.001 | 5.925 |
| FFI pain | 21.3 ± 4.0 (14-42) | 3.2 ± 2.1 (2-22) | <.001 | 4.278 |
| FFI disability | 16.9 ± 3.8 (12-34) | 4.2 ± 2.1 (2-21) | <.001 | 3.148 |
| FFI activity limitation | 17.7 ± 2.6 (8-22) | 3.7 ± 1.7 (1-16) | <.001 | 4.665 |
| VAS | 7.7 ± 1.3 (5-10) | 0.4 ± 0.9 (0-7) | <.001 | 4.713 |
Scores are reported as mean ± SD (range).
The overall complication rate was 3.8% (n = 4). Painful hardware was present in 1.9% of cases (n = 2), which required subsequent removal. Nonunion at the osteotomy site was present in 1.0% of cases (n = 1), which required a revision procedure. This was diagnosed early at 2 months post-ZO owing to displacement of the osteotomy. Partial plantar fascia tear was noted in 1.0% of cases (n = 1) and occurred at 7 months postoperatively while the patient was exercising. Symptoms resolved with conservative management. It is unlikely that this was directly related to the percutaneous ZO given the isolated and late occurrence in this series. There were no significant wound complications or deep infection in this case series. Of 104 cases, 98.1% of patients were satisfied with their procedure on survey (n = 102). Of the 2 patients who reported dissatisfaction, 1 reported their dissatisfaction was secondary to their nonunion and necessary revision. The other patient had comorbid lupus but no surgical complications or explanation for dissatisfaction. No patients reported recurrence of their initial symptoms.
Discussion
This study demonstrated a significant improvement in pain and functional outcomes with minimal complications and a high rate of patient satisfaction following percutaneous ZO intervention. In a population of 104 patients, significant improvement in FFI and VAS scores was observed after ZO. A Cohen d analysis revealed an effect size >2 for each paired analysis, indicating that the statistical changes following ZO were very strong. A low rate of complications (3.8%) and a high rate of satisfaction (98.1%) was observed. To our knowledge, the current study appears to be the first to assess surgical outcomes of percutaneous ZO for IAT with a minimum 2-year follow-up.
The percutaneous ZO is a unique intervention in that it addresses Achilles pathology, without the need for direct detachment and reattachment of the tendon. During the ZO procedure, a dorsal-based wedge is removed from the calcaneus. The calcaneus is shortened and rotated anteriorly; the Achilles insertion is moved anterior and superior to its original position. This modification simultaneously relieves pressure at the posterosuperior prominence and retrocalcaneal bursitis (if present), while relieving tension and strain on the Achilles tendon at its insertion. This is accomplished without ever disrupting the Achilles tendon itself.
Avoiding disruption of the natural Achilles tendon may allow for a shorter recovery period compared to Achilles tendon debridement. Indications for percutaneous ZO include patients who present with chronic IAT with or without intratendinous calcification (with or without Haglund deformity). 12 For patients who require intervention for IAT, yet have an increased risk of wound complications, the percutaneous ZO may be a preferred intervention compared to open procedures, but more research is needed in this area.
Many studies have demonstrated an improvement in outcomes and reduction of complications with the ZO.13,15,23,26,27,29,44,46 However, data remain limited in comparison to other interventions for IAT. Although Achilles tendon debridement procedures for IAT have good patient outcomes, they often lead to a prolonged recovery and wound complications.20,49 The posterior midline splitting approach with open Haglund resection is a common intervention for this pathology. Both procedures have been found to lead to an improvement of FFI and/or VAS score to a similar degree as seen with ZO (P < .001).7,18 However, commonly reported wound complications associated with debridement procedures include hypesthesia of the surgical scar, skin necrosis, superficial wound infection, and hematoma. Complications also can include superficial infection, delayed healing, and hypertrophy or numbness of the surgical scar.20,33,49 Wound complications as such not only affect length of recovery but also patient outcomes. Watson et al 49 report a significantly lower satisfaction rate and increased pain in patients receiving debridement for IAT. Overall, complications associated with debridement of IAT range from 4.7% to 41.0% in the literature.20,49,50 Success of Achilles insertional debridement and reattachment is dependent on the calcific tendinopathy present at the insertion and the severity of tendinosis and, therefore, is highly variable.
Numerous studies have shown favorable outcomes following ZO in treatment for IAT.13,15,23,26,27,29,44,46 In a retrospective study, Ge et al 13 found that the open ZO provided improved long-term function and symptom remission in comparison to posterosuperior prominence resection for Haglund syndrome. However, their study demonstrated increased recovery time following open ZO due to more extensive surgical dissection; patients did not achieve remission of surgery-related pain until 1 year postoperation. 13 Like all open procedures in the retrocalcaneal space, complications with superficial wound infections and sural nerve–related paresthesia have been reported after open ZO. 27 Prospective studies have reported overall complication rates up to 10.7% with open ZO intervention.15,27 Meanwhile, percutaneous foot and ankle surgery has gained popularity because of a widely observed reduction in postoperative healing time, complication rate, and need for reintervention.8,10,11,16,25,31,32,34,39,41,48 Many minimally invasive interventions have demonstrated improved functional outcomes, faster return to activity, and increased patient satisfaction in comparison to similar but open procedures.7,8,25,31,34,48
The percutaneous ZO has previously been associated with improved surgical outcomes and patient satisfaction in comparison to the open procedures for treatment of IAT.9,38 In direct comparison to open Haglund resection, Choi and Suh found that the percutaneous ZO approach achieved earlier clinical improvement. 7 Although this study included an average follow-up of 20.3 months, only 10 patients receiving percutaneous ZO and 12 patients receiving an open procedure were analyzed. The present study affirms trends reported by Choi and Suh; however, the present study has an extended mean follow-up time (41.2 months) and a much larger patient cohort (N = 104).
Nordio et al 31 found percutaneous ZO to correlate with improved VAS pain scores, improved functional outcomes, and shorter recovery in comparison to open ZO. They reported zero wound complications and a short recovery; complete pain resolution was observed at a mean of 12 weeks postoperatively. Two complications were described (7.7%): 1 nonunion and 1 patient with symptomatic hardware. However, this study included only 26 patients and a minimum follow-up of 6 months. These factors limit the assessment of longer-term outcomes such as potential recurrence of symptoms as patients return to full activity, or overall patient satisfaction.
The strengths of this study include the large sample size and higher follow-up duration compared with prior studies. To our knowledge, this is the largest study performed on the percutaneous ZO in the literature. Furthermore, this study used validated measurements to assess patient outcomes.
However, the study has notable limitations. The retrospective nature of this study comes with inherent limitations including (1) some lack of precision with selection clarity and (2) no open Achilles insertional debridement control group. Although FFI is a validated and widely used measurement, it has been found unable to differentiate between postoperative function relative to baseline activity level (ie, athletes vs sedentary). It was originally developed for low-functioning rheumatoid arthritic patients and has low “ceiling effect” measurement issues—meaning it cannot differentiate between average and much greater than average function. 19
To advance our understanding of this technique and better advise practice guidelines, further studies are necessary. Investigation of surgical time, bleeding, postoperative pain, cost of surgery, complications, and patient outcomes between the percutaneous ZO and the open Achilles procedure are needed, and most importantly a randomized controlled trial comparing complications and outcomes to usual current treatment is warranted. Additionally, the authors are further investigating ideal candidates for Zadek osteotomy based on clinical, radiographic, and advanced imaging studies. Currently, as stated earlier, the senior authors use the same indications for ZO as they would for an open Achilles debridement. However, further research is needed to identify the ideal candidates for ZO.
Conclusion
We found percutaneous ZO to be a safe and effective intervention for treatment of IAT. With a minimum 2-year follow-up, our study found a significant improvement in FFI and VAS scores, a low recurrence rate, and a high rate of patient satisfaction. Surgeons may consider percutaneous ZO as a first-line surgical option for the treatment of insertional Achilles tendinopathy.
Supplemental Material
Supplemental material, sj-pdf-1-fai-10.1177_10711007241252803 for Outcomes After Percutaneous Zadek Osteotomy for Insertional Achilles Tendinopathy by SarahRose Hall, Oliver N. Schipper, Jonathan R. M. Kaplan, A. Holly Johnson, Tyler A. Gonzalez and Ettore Vulcano in Foot & Ankle International
Footnotes
Ethical Approval: Ethical approval for this study was obtained from Institutional Review Board at Mount Sinai Medical Center [FWA00000176].
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Oliver N. Schiper, MD reports royalties or licenses and consulting fees from Treasce Medical Concepts, Vilex, Exactech, and Enovis. Jonathan R. M. Kaplan, MD, reports royalties or licenses and consulting fees from Artelon, Edge Surgical, Exactech, Surgebright, and Enovis. A. Holly Johnson, MD, reports royalties or licenses from Novastep and Treace Medical Concepts. Tyler A. Gonzalez, MD, MBA, reports royalties or licenses and consulting fees from Treace Medical Concepts, Surgical Fusion Technologies, Vilex; consulting fees from Stryker, Surgebright, and Enovis. Ettore Vulcano, MD, reports royalties or licenses and consulting fees from Novastep, Vilex, and Treace Medical Concepts. Disclosure forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: SarahRose Hall, BA,  https://orcid.org/0000-0002-4026-3118
https://orcid.org/0000-0002-4026-3118
Oliver N. Schipper, MD,  https://orcid.org/0000-0003-1248-640X
https://orcid.org/0000-0003-1248-640X
Jonathan R. M. Kaplan, MD,  https://orcid.org/0000-0002-0821-7939
https://orcid.org/0000-0002-0821-7939
Tyler A. Gonzalez, MD, MBA,  https://orcid.org/0000-0002-3210-8097
https://orcid.org/0000-0002-3210-8097
Supplemental Material: A supplemental video for this article is available online.
References
- 1. Black AT, So E, Combs A, Logan D. The Zadek osteotomy for surgical management of insertional Achilles tendinopathy: a systematic review. Foot Ankle Spec. 2023;16(4):437-445. doi: 10.1177/19386400231162411 [DOI] [PubMed] [Google Scholar]
- 2. Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561-570. doi: 10.1016/0895-4356(91)90220-4 [DOI] [PubMed] [Google Scholar]
- 3. Carmont MR, Maffulli N. Management of insertional Achilles tendinopathy through a Cincinnati incision. BMC Musculoskelet Disord. 2007;8:82. doi: 10.1186/1471-2474-8-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cengiz B, Karaoglu S. Clinical results of the Keck and Kelly wedge osteotomy approach in Haglund’s deformity: minimum 3-year follow-up. Foot Ankle Surg. 2022;28(2):269-275. doi: 10.1016/J.FAS.2021.10.006 [DOI] [PubMed] [Google Scholar]
- 5. Challoumas D, Zouvani A, Creavin K, et al. Determining minimal important differences for patient-reported outcome measures in shoulder, lateral elbow, patellar and Achilles tendinopathies using distribution-based methods. BMC Musculoskelet Disord. 2023;24(1):158. doi: 10.1186/s12891-023-06261-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chimenti RL, Cychosz CC, Hall MM, Phisitkul P. Current concepts review update: insertional Achilles tendinopathy. Foot Ankle Int. 2017;38(10):1160-1169. doi: 10.1177/1071100717723127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Choi JY, Suh JS. A novel technique of minimally invasive calcaneal osteotomy for intractable insertional Achilles tendinopathy associated with Haglund deformity. Foot Ankle Surg. 2022;28(5):578-583. doi: 10.1016/j.fas.2021.06.002 [DOI] [PubMed] [Google Scholar]
- 8. Cusumano A, Martinelli N, Bianchi A, Bertelli A, Marangon A, Sansone V. Transtendinous approach calcaneoplasty versus endoscopic calcaneoplasty for Haglund’s disease. Int Orthop. 2021;45(1):225-231. doi: 10.1007/S00264-020-04761-0/TABLES/2 [DOI] [PubMed] [Google Scholar]
- 9. deMeireles AJ, Guzman JZ, Nordio A, Chan J, Okewunmi J, Vulcano E. Complications after percutaneous osteotomies of the calcaneus. Foot Ankle Orthop. 2022;7(3):24730114221119731. doi: 10.1177/24730114221119731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ebben BJ, Buckley SE, Hewitt MA, Moon DK, Metzl JA, Hunt KJ. Outcomes in open and endoscopic treatment for Haglund’s syndrome and insertional Achilles tendinopathy. Foot Ankle Orthop. 2022;7(4): 2473011421S00652. doi: 10.1177/2473011421S00652 [DOI] [Google Scholar]
- 11. Fathi Mahmoud H, Feisal W, Samir Fahmy F. Satisfactory functional outcome and significant correlation with the length of Haglund’s deformity after endoscopic calcaneoplasty: a minimum 4-year follow-up study. Adv Orthop. 2022;2022:7889684. doi: 10.1155/2022/7889684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferranti S, Migliorini F, Liuni FM, et al. Outcomes of percutaneous calcaneoplasty for insertional Achilles tendon problems. Foot Ankle Int. 2021;42(10):1287-1293. doi: 10.1177/10711007211004963 [DOI] [PubMed] [Google Scholar]
- 13. Ge Z, Ma L, Tang H, et al. Comparison of dorsal closing wedge calcaneal osteotomy versus posterosuperior prominence resection for the treatment of Haglund syndrome. J Orthop Surg Res. 2020;15(1):168. doi: 10.1186/s13018-020-01687-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Georgiannos D, Kitridis D, Bisbinas I. Dorsal closing wedge calcaneal osteotomy for the treatment of insertional Achilles tendinopathy: a technical tip to optimize its results and reduce complications. Foot Ankle Surg. 2018;24(2):115-118. doi: 10.1016/J.FAS.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 15. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2016;38(4):381-387. doi: 10.1177/1071100716681139 [DOI] [PubMed] [Google Scholar]
- 16. Güler Y, Birinci M, Hakyemez ÖS, et al. Achilles tendon-splitting approach and double-row suture anchor repair for Haglund syndrome. Foot Ankle Surg. 2021;27(4):421-426. doi: 10.1016/J.FAS.2020.05.009 [DOI] [PubMed] [Google Scholar]
- 17. Gutteck N, Zeh A, Wohlrab D, Delank KS. Comparative results of percutaneous calcaneal osteotomy in correction of hindfoot deformities. Foot Ankle Int. 2019;40(3):276-281. doi: 10.1177/1071100718809449 [DOI] [PubMed] [Google Scholar]
- 18. Hörterer H, Oppelt S, Böcker W, et al. Patient-reported outcomes of surgically treated insertional Achilles tendinopathy. Foot Ankle Int. 2021;42(12):1565-1569. doi: 10.1177/10711007211023060 [DOI] [PubMed] [Google Scholar]
- 19. Hung M, Nickisch F, Beals TC, Greene T, Clegg DO, Saltzman CL. New paradigm for patient-reported outcomes assessment in foot & ankle research: computerized adaptive testing. Foot Ankle Int. 2012;33(8):621-626. doi: 10.3113/FAI.2012.0621 [DOI] [PubMed] [Google Scholar]
- 20. Irwin TA. Current concepts review: insertional Achilles tendinopathy. Foot Ankle Int. 2010;31(10):933-939. doi: 10.3113/FAI.2010.0933 [DOI] [PubMed] [Google Scholar]
- 21. Kaplan J, Hall S, Schipper O, Vulcano E, Jackson B, Gonzalez T. Percutaneous Zadek osteotomy for insertional Achilles tendinopathy and Haglund’s deformity: a technique tip. Foot Ankle Int. 2023;44(9):931-935. [DOI] [PubMed] [Google Scholar]
- 22. Keck S, Kelly P. Bursitis of the posterior part of the heel: evaluation of surgical treatment of eighteen patients. J Bone Joint Surg. 1965;47(2):267-273. [PubMed] [Google Scholar]
- 23. Kelsall NK, Chapman AW, Sangar A, Farrar MJ, Taylor HP. Zadek’s calcaneal osteotomy for insertional Achilles pathology. Orthop Proc. 2014;96-B(suppl 2):19. doi: 10.1302/1358-992X.96BSUPP_2.BOFAS2013-019 [DOI] [Google Scholar]
- 24. Ko VMC, He X, Fu SC, Yung PSH, Ling SKK. Clinical effectiveness of pulsed electromagnetic field therapy as an adjunct treatment to eccentric exercise for Achilles tendinopathy: a randomised controlled trial. Trials. 2023;24(1):1-10. doi: 10.1186/S13063-023-07434-6/TABLES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Leitze Z, Sella EJ, Aversa JM. Endoscopic decompression of the retrocalcaneal space. J Bone Joint Surg Am. 2003;85(8):1488-1496. doi: 10.2106/00004623-200308000-00009 [DOI] [PubMed] [Google Scholar]
- 26. López-Capdevila L, Santamaria Fumas A, Dominguez Sevilla A, et al. Dorsal wedge calcaneal osteotomy as surgical treatment for insertional Achilles tendinopathy. Rev Esp Cir Ortop Traumatol (Engl Ed). 2020;64(1):22-27. doi: 10.1016/J.RECOT.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 27. Maffulli N, D’Addona A, Gougoulias N, Oliva F, Maffulli GD. Dorsally based closing wedge osteotomy of the calcaneus for insertional Achilles tendinopathy. Orthop J Sports Med. 2020;8(3). doi: 10.1177/2325967120907985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Maffulli N, Saxena A, Wagner E, Torre G. Achilles insertional tendinopathy: state of the art. J ISAKOS. 2019;4(1):48-57. doi: 10.1136/JISAKOS-2017-000144 [DOI] [Google Scholar]
- 29. Mazura M, Goldman T, Stanislav P, Kachlik D, Hromadka R. Calcaneal osteotomy due to insertional calcaneal tendinopathy: preoperative planning. J Orthop Surg Res. 2022;17(1):1-5. doi: 10.1186/S13018-022-03359-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Myerson CL, Shimozono Y, Kennedy JG. Haglund’s deformity and chronic Achilles tendonitis. Oper Tech Orthop. 2018;28(2):104-109. doi: 10.1053/J.OTO.2018.02.006 [DOI] [Google Scholar]
- 31. Nordio A, Chan JJ, Guzman JZ, Hasija R, Vulcano E. Percutaneous Zadek osteotomy for the treatment of insertional Achilles tendinopathy. Foot Ankle Surg. 2020;26(7):818-821. doi: 10.1016/J.FAS.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 32. Ortmann FW, McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2016;28(2):149-153. doi: 10.3113/FAI.2007.0149 [DOI] [PubMed] [Google Scholar]
- 33. Paavola M, Orava S, Leppilahti J, Kannus P, Järvinen M. Chronic Achilles tendon overuse injury: complications after surgical treatment an analysis of 432 consecutive patients. Am J Sports Med. 2000;28(1):77-82. [DOI] [PubMed] [Google Scholar]
- 34. Pi Y, Hu Y, Guo Q, et al. Open versus endoscopic osteotomy of posterosuperior calcaneal tuberosity for Haglund syndrome: a retrospective cohort study. Orthop J Sports Med. 2021;9(4):23259671211001055. doi: 10.1177/23259671211001055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Poutoglidou F, Drummond I, Patel A, Malagelada F, Jeyaseelan L, Parker L. Clinical outcomes and complications of the Zadek calcaneal osteotomy in insertional Achilles tendinopathy: a systematic review and meta-analysis. Foot Ankle Surg. 2023;29(4):298-305. doi: 10.1016/J.FAS.2023.04.007 [DOI] [PubMed] [Google Scholar]
- 36. Reddy SC, Schipper ON, Li J. The effect of chilled vs room-temperature irrigation on thermal energy dissipation during minimally invasive calcaneal osteotomy of cadaver specimens. Foot Ankle Orthop. 2022;7(4):24730114221136548. doi: 10.1177/24730114221136548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ricci AG, Stewart M, Thompson D, Watson BC, Ashmyan R. The central-splitting approach for Achilles insertional tendinopathy and Haglund deformity. JBJS Essent Surg Tech. 2020;10(1):e0035. doi: 10.2106/JBJS.ST.19.00035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Roche AJ, Calder JDF. Achilles tendinopathy: a review of the current concepts of treatment. Bone Joint J. 2013;95-B(10):1299-1307. doi: 10.1302/0301-620X.95B10.31881 [DOI] [PubMed] [Google Scholar]
- 39. Sammarco GJ, Taylor AL. Operative management of Haglund’s deformity in the nonathlete: a retrospective study. Foot Ankle Int. 1998;19(11):724-729. doi: 10.1177/107110079801901102 [DOI] [PubMed] [Google Scholar]
- 40. Saxena A, Ramdath S, O’Halloran P, Gerdesmeyer L, Gollwitzer H. Extra-corporeal pulsed-activated therapy (“EPAT” sound wave) for Achilles tendinopathy: a prospective study. J Foot Ankle Surg. 2011;50(3):315-319. doi: 10.1053/j.jfas.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 41. Scholten PE, van Dijk CN. Endoscopic calcaneoplasty. Foot Ankle Clin. 2006;11(2):439-446. doi: 10.1016/J.FCL.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 42. Strasser NL, Farina KA. Haglund’s syndrome and insertional Achilles tendinopathy. Oper Tech Sports Med. 2021;29(3):150850. doi: 10.1016/j.otsm.2021.150850 [DOI] [Google Scholar]
- 43. Talusan PG, Cata E, Tan EW, Parks BG, Guyton GP. Safe zone for neural structures in medial displacement calcaneal osteotomy: a cadaveric and radiographic investigation. Foot Ankle Int. 2015;36(12):1493-1498. doi: 10.1177/1071100715595696 [DOI] [PubMed] [Google Scholar]
- 44. Tourne Y, Baray AL, Barthelemy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: clinical results and a radiographic analysis to explain its efficacy. Foot Ankle Surg. 2022;28(1):79-87. doi: 10.1016/J.FAS.2021.02.001 [DOI] [PubMed] [Google Scholar]
- 45. Tourné Y, Baray AL, Barthélémy R, Moroney P. Contribution of a new radiologic calcaneal measurement to the treatment decision tree in Haglund syndrome. Orthop Traumatol Surg Res. 2018;104(8):1215-1219. doi: 10.1016/J.OTSR.2018.08.014 [DOI] [PubMed] [Google Scholar]
- 46. Tourné Y, Francony F, Barthélémy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: its effects on the dorsiflexion of the ankle and correlations to clinical and functional scores. Foot Ankle Surg. 2022;28(6):789-794. doi: 10.1016/J.FAS.2021.11.001 [DOI] [PubMed] [Google Scholar]
- 47. Vaishya R, Agarwal AK, Azizi AT, et al. Haglund’s syndrome: a commonly seen mysterious condition. Cureus. 2016;8(10):e820. doi: 10.7759/CUREUS.820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang CL, Chen PY, Yang KC, Wu HC, Wang CC. Ultrasound-guided minimally invasive surgical resection of retrocalcaneal bursitis: a preliminary comparison with traditional open surgery. J Foot Ankle Surg. 2019;58(5):855-860. doi: 10.1053/J.JFAS.2018.12.023 [DOI] [PubMed] [Google Scholar]
- 49. Watson AD, Anderson RB, Davis WH. Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional Achilles tendinosis with calcific spur. Foot Ankle Int. 2000;21(8):638-642. doi: 10.1177/107110070002100802 [DOI] [PubMed] [Google Scholar]
- 50. Yontar NS, Aslan L, Can A, Öğüt T. Mid-term results of open debridement and reattachment surgery for insertional Achilles tendinopathy: a retrospective clinical study. Acta Orthop Traumatol Turc. 2020;54(6):567. doi: 10.5152/J.AOTT.2020.18426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zadek I. An operation for the cure of achillobursitis. Am J Surg. 1939;43(2):542-546. doi: 10.1016/S0002-9610(39)90877-9 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fai-10.1177_10711007241252803 for Outcomes After Percutaneous Zadek Osteotomy for Insertional Achilles Tendinopathy by SarahRose Hall, Oliver N. Schipper, Jonathan R. M. Kaplan, A. Holly Johnson, Tyler A. Gonzalez and Ettore Vulcano in Foot & Ankle International