Abstract
Objective
Learning from adverse outcomes in health and social care is critical to advancing a culture of patient safety and reducing the likelihood of future preventable harm to service users. This review aims to present an overview of all clinical claims finalised in one calendar year involving publicly funded health and social care providers in Ireland.
Design
This is a retrospective observational study. The Clinical Risk Unit (CRU) of the State Claims Agency identified all service-user clinical claims finalised between 1 January 2017 and 31 December 2017 from Ireland’s National Incident Management System (n=713). Claims that had incurred financial damages were considered for further analysis (n=356). 202 claims underwent an in-depth qualitative review. Of these, 57 related to maternity and gynaecology, 64 to surgery, 46 to medicine, 20 to community health and social care and 15 related to children’s healthcare.
Results
The services of surgery and medicine ranked first and second, respectively, in terms of a number of claims. Claims in maternity services, despite ranking third in terms of claims numbers, resulted in the highest claims costs. Catastrophic injuries in babies resulting in cerebral palsy or other brain injury accounted for the majority of this cost.
Diagnostic errors and inadequate or substandard communication, either with service users and/or interprofessional communication with colleagues, emerged as common issues across all clinical areas analysed. Quantitative analysis of contributory factors demonstrated that the complexity and seriousness of the service user’s condition was a significant contributory factor in the occurrence of incidents leading to claims.
Conclusion
This national report identifies common issues resulting in claims. Targeting these issues could mitigate patient safety risks and reduce the cost of claims.
Keywords: Incident reporting; Adverse events, epidemiology and detection; Healthcare quality improvement; Medical error, measurement/epidemiology; Diagnostic errors
WHAT IS ALREADY KNOWN ON THIS TOPIC
Previous studies in Ireland and elsewhere have described medical negligence claims numbers, costs and patterns by specialty. However, this study provides an analysis of clinical claims across all specialties, providing a whole system view of claims at a particular point in time.
WHAT THIS STUDY ADDS
This study contributes learning from the unique perspective of the indemnifier of a national publicly funded health and social care service about the common factors contributing to the occurrence of clinical claims across all services, and highlights deficits in relation to communication, patient/service user monitoring, therapeutic interventions and diagnostic tests.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
While not all adverse events are preventable, this study contributes to a culture of learning when things go wrong. The learnings from this study have been shared widely with senior clinicians, executives and risk managers in Ireland’s Health Service Executive, the organisation tasked with providing public health services in Ireland.
Introduction
Learning from adverse outcomes in health and social care is critical to advancing a culture of patient safety and reducing the likelihood of future harm to service users. In Ireland, the State indemnifies publicly funded health and social services for claims alleging medical negligence, resulting from personal injury, during the provision of professional medical services.
The State Claims Agency (SCA) manages these claims. It also has a risk management function, advising and assisting these services in seeking to prevent future incidents. Under the National Treasury Management Agency (Amendment) 2000 Act, health and social care services are required to report service user incidents to the SCA on the National Incident Management System (NIMS), which the SCA hosts and governs jointly with Ireland’s Health Service Executive (HSE). The SCA is, therefore, in a unique position, as it has access to national data on clinical incidents, in addition to data on claims managed by the SCA on behalf of health and social care services. This national oversight of claims enables the SCA to undertake a comprehensive end-to-end analysis of claims data.
Published clinical claims data often describes claims in relation to a particular service, specialty or claims category or provides high-level aggregate analysis. By contrast, the aim of this study was to present a descriptive analysis of the portfolio of clinical claims being managed by the SCA, the indemnifier of publicly funded health and social care services in Ireland, at a particular point of time (2017). This snapshot included an analysis of the patterns of litigation and common themes resulting in litigation. It describes claims by service, associated costs and an analysis of issues resulting in those claims. Moreover, it provides an aggregate analysis of contributory factors (CFs). This wider perspective helps identify issues common to all services resulting in claims.
Methods
Data selection
Claims within the scope of the study included all service user-related clinical claims finalised during the period 1 January 2017 to 31 December 2017 inclusive (n=713). All analysis used data available on NIMS. Only those claims that had incurred damages were considered for further analysis (n=356).
All claims with paid damages equal to or greater than €150 000 (n=89) were analysed in-depth and for those with paid damages less than €150 000 (n=267), a sample of 114 claims was selected. Purposeful sampling was employed to ensure the inclusion of hospitals or services with small numbers of claims.
An agreed claim analysis template was used for data synthesis and standardisation of the claims selected (online supplemental file 1). Following initial manual review and exclusion of claims deemed to be outside of the scope of the study, 202 claims were selected for in-depth analysis.
No patients or members of the public were involved in the study concept, design or data analysis.
Data Categorisation
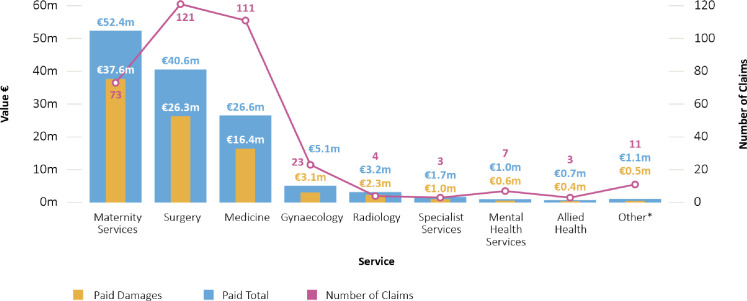
Categories of service under which claims were made are presented in figure 1, ranked by paid total. These are the categories as listed on NIMS. For psychological injury claims (eg, where a claim for psychological injury is taken by a bereaved family member(s)), the analysis focused on the clinical event giving rise to the psychological injury claim, rather than the psychological injury claim itself.
Figure 1. Claims with damages paid listed by service and cost. Paid damages: Payments awarded to the plaintiff including special and general damage payments. Paid total: The total accumulated paid cost of a claim over its lifetime and may include payments made over a number of years. Figures with regard to damages, legal costs and expert costs may be reflected in this total. *Other refers to seven service categories where the paid total for each category was less than €500 000.
Data analysis
Claims analysis was undertaken by clinical risk advisors (CRAs) in the Clinical Risk Unit (CRU) of the SCA. A standardised tool is available that provides a comprehensive framework for incident investigations and analysis, namely ‘The London Protocol’1 which was amended to reflect the information that was available to the CRU.
The Yorkshire Contributory Factors Framework (YCFF) was used to inform CF analysis. The YCFF is an evidence-based tool for patient safety reviews, primarily developed for acute hospital settings.2 The CFs reviewed were aggregated under five key domains: (1) service user factors, (2) task and technology factors, (3) individual (staff) factors, (4) team factors and (5) work environmental factors. The presence of each CF was assessed as ‘yes’, ‘maybe’ and ‘no’ or ‘unknown’ in relation to each claim. For the purposes of quantitative analysis, ‘yes’ was given a score of 2, ‘maybe’ was given a score of 1 and ‘no’ or ‘unknown’ was given a score of 0. This provided a cumulative score for each CF which was ranked in order of prominence.
All analyses used data available on NIMS. Rounding is kept to the nearest single whole number for percentages and the nearest first decimal place for monetary values. The severity rating is aligned with the HSE Risk Impact Table as outlined in the HSE Incident Management Framework (online supplemental file 2).3 All graphs and tables were generated through Tableau (V.2018.3). Analysis was subject to an internal quality assurance process whereby statistics and figures were double-checked by a second CRA.
Results
High level review of claims (n=356)
Claims where damages were paid most frequently occurred in the services of surgery, medicine and maternity, which between them accounted for 86% (305 of 356) of the claims where payments were made (figure 1). Of the 356 claims that resulted in a payment, 121 (34%) related to surgery, 111 (31%) related to medicine and 96 (27%) related to maternity and gynaecology services.
Although maternity services ranked third in terms of a number of claims where a payment was made, the total payments made in relation to maternity service claims was €52.4 million; this represented 40% of the total payments (€132.3 million) made in relation to claims finalised in 2017 and exceeded the payments made in any other clinical area. The subservices of ‘delivery’, ‘antenatal’ and ‘postnatal’ featured in the top 10 subservices by number of claims (table 1).
Table 1. Top 10 services and subservices by number of claims and associated paid total.
| Number of claims | Service | Subservice | Paid total |
| 50 | Medicine | Emergency medicine | €9, 393, 710 |
| 47 | Maternity | Delivery | €46, 602, 161 |
| 42 | Medicine | General medicine | €11, 614, 223 |
| 35 | Surgery | Orthopaedic surgery | €9, 782, 771 |
| 33 | Surgery | General surgery | €7, 074, 171 |
| 22 | Gynaecology | General | €5, 047, 011 |
| 14 | Maternity | Antenatal | €3, 005, 343 |
| 12 | Maternity | Postnatal | €2, 790, 836 |
| 10 | Surgery | Gastrointestinal | €1, 403, 998 |
| 10 | Surgery | Neurosurgery | €14, 967, 298 |
The top 10 subservices accounting for claims by number are presented below.
In the service of medicine, the highest number of claims arose in the subservices of emergency medicine and general medicine, and in the clinical area of surgery, the highest number of claims arose in the subservices of orthopaedic surgery and general surgery. 333 (94%) claims related to incidents that occurred in a hospital setting, with only 23 (6%) occurring in a community setting.
Detailed review of claims (n=202)
What went wrong?
Clinical claims frequently arose due to diagnostic error (delayed, missed or misdiagnosis) often leading to delayed or incorrect treatment, or as a result of a range of adverse outcomes related to treatment or therapeutic intervention, including complications of surgery, retention of foreign objects, medication errors or delayed treatment interventions. Claims also arose in relation to delivery (table 2).
Table 2. Examples of claims related to diagnostic error and therapeutic interventions.
| Examples of claims related to diagnostic error | Examples of claims related to therapeutic interventions |
|
|
Factors contributing to the occurrence of claims
-
Inadequate or substandard communication with service users, for example, substandard/omitted consent, failure to consent for known complications of a procedure and failure to engage in open disclosure.
Substandard consent featured in 20/64 (31%) of surgical claims analysed.
-
Inadequate or substandard interprofessional communication—between colleagues or within and between multidisciplinary teams and services, for example, unsigned, illegible or absent entries in the healthcare record, inadequate communication between teams and services when transferring care.
Substandard clinical documentation featured in 13/20 (65%) claims occurring within community health and social care.
Failure to adequately monitor a service user or recognise a deteriorating service user, for example, failure to act on abnormal findings (eg, cardiotocography (CTG)) or to escalate to a senior decision-maker as appropriate, inadequate risk assessments undertaken, failure to take account of relevant medical history.
Inadequacies related to the diagnostic process, for example, delay/failure in performing diagnostic tests and/or investigations, failure to follow-up on diagnostic tests, ordering the incorrect diagnostic tests.
Inadequacies related to treatment, interventions and procedures, for example, delay in initiating treatment, inappropriate deviation from good practice/clinical guidelines, substandard treatment due to inadequate training or familiarity with a technique.
Inadequate staffing and resources to meet demand.
Lack of availability of diagnostic equipment.
Equipment failure due to inadequate maintenance.
In addition to a qualitative analysis of the factors contributing to claims, a scoring system for CFs was used (see the ‘Methods’ section). Table 3 presents the aggregate CF ranking for all 202 claims that were subject to in-depth analysis.
Table 3. The aggregate contributory factor (CF) ranking across all 202 claims subject to in-depth analysis.
| CFs (listed in descending order of CF score) | CF score | Position |
| Service user factors—condition (complexity and seriousness) | 192 | 1 |
| Task and technology factors—task design and clarity of structure | 167 | 2 |
| Individual (staff) factors—knowledge and skills | 162 | 3 |
| Individual (staff) factors—competence | 146 | 4 |
| Team factors—written communication | 142 | 5 |
| Team factors—verbal communication | 115 | 6 |
| Task and technology factors—availability and use of protocols | 106 | 7 |
| Team factors—supervision and seeking help | 85 | 8 |
| Service user factors—language and communication | 72 | 9 |
| Task and technology factors—availability and accuracy of test results | 63 | 10 |
| Team factors—team structure (congruence, consistency, leadership, etc) | 62 | 11 |
| Work environmental factors—design, availability and maintenance of equipment | 45 | 12 |
| Work environmental factors—workload and shift patterns | 40 | 13 |
Discussion
Main findings and international comparison
This review provides a snapshot at a particular point in time at the national level of the number, costs and types of clinical claims managed by the SCA. The pattern of claims, with claims most frequently occurring in hospitals and in the clinical areas of surgery, medicine and maternity services, was in keeping with previous SCA analysis.4
The payments made for claims in maternity services exceeded the payments made in any other clinical service. This is because most catastrophic brain injury/cerebral palsy claims arise in this service, and they are usually associated with high levels of damages. This is similar to the UK experience, where obstetrics accounted for 64% of the value of total clinical negligence claims managed by National Health Service (NHS) Resolution, despite accounting for only 13% of the number of claims.5 Additionally, in a UK 10-year maternity review conducted between 2000 and 2010, the categories contributing to the largest value of obstetric-related claims related to cerebral palsy and CTG interpretation.6 This serves to emphasise the importance of initiatives to mitigate risks in labour and the risks of perinatal causes of morbidity and mortality. In Ireland, the National Neonatal Encephalopathy Action Group (NNEAG) was established in 2019 as a formal partnership arrangement between the HSE’s National Women and Infants Health Programme, the Irish Department of Health and the SCA to deal with issues of joint concern around the incidence of neonatal encephalopathy in Irish maternity units and hospitals. The purpose of NNEAG is to identify and mitigate against factors that are known to contribute to avoidable neonatal encephalopathy and improve the quality of care within Irish maternity services.
The costs of claims associated with neurosurgery were disproportionately high, with 10 of 121 surgical claims analysed accounting for 43% of the paid damages for this service, reflecting the fact that adverse events which arise in this subservice may result in catastrophic injuries.
Of the 356 claims where payments were made, 333 (94%) occurred in hospital settings, which most likely reflects the complexity of care being delivered in these locations. However, claims also arise in community settings, which emphasises the need for risk management in all health and social care settings.
This review also examined the issues contributing to the occurrence of the incidents that resulted in claims. The issues identified were not new, reflecting the recurrence of common themes. Inadequate or substandard communication with service users or with colleagues, emerged as a common issue across all clinical areas analysed. Poor communication is a predisposing factor for complaints and litigation and can strongly influence whether an incident becomes a claim.7 This includes not only the information relayed to a service user but also the manner in which the information is communicated.8 Although all procedures carry the risk of complications, claims may also arise if the plaintiff alleges they were not made aware of the potential complication(s), or if there is insufficient documented evidence of consent.
In a US-based benchmarking report in 2015, after analysis of more than 23 000 medical malpractice claims between 2009 and 2013, a third of cases could be directly linked to communication breakdown.9 Malpractice cases involving a communication breakdown closed with an indemnity payment more frequently than other cases, and those payments were above the overall average.
Well-known and structured communication tools such as ISBAR/ISBAR3 (Identify, Situation, Background, Assessment and Recommendation/Read back/Risk) are used internationally for both escalation to senior healthcare professionals and clinical handover. These have been integrated into National Clinical Effectiveness Committee (NCEC) guidelines in recognition of the need to improve and standardise communication in health and social care.10,15 Huddles are also recommended in several NCEC guidelines, and recently published literature demonstrates how they can improve communication and enable a supportive safety culture.16 17
In this review, delayed diagnosis, missed diagnosis and misdiagnosis were common adverse outcomes which resulted in claims. Process failures which resulted in these outcomes included delay/failure in performing diagnostic tests or investigations, failure to follow-up on diagnostic tests and ordering the incorrect diagnostic test.
The failure to adequately monitor and/or recognise a deteriorating service user was observed in a number of the clinical areas analysed in this study. Examples included inadequate clinical observations, inadequate risk assessments, inadequate monitoring of the complications associated with treatments, substandard interpretation/misinterpretation of fetal heart rate monitoring and inadequate assessment of the environment in those at risk of self-harm.
In a benchmarking report on malpractice risks in the diagnostic process from the USA, an investigation of 2685 diagnosis-related cases found that 29% involved testing failures and 46% involved follow-up failures.18 Of note, diagnostic tests were not performed, were performed incorrectly, specimens were lost and/or the review, communication or follow-up of the result did not occur or was delayed.
In a recently published review by NHS Resolution of emergency medicine claims the same theme of diagnostic errors arose, including missed signs of deterioration, failure to investigate and missed, incorrect and delayed diagnosis.19
In this study, claims also arose when those undertaking a procedure did not have the required knowledge and skills or failed to adhere to good practice/clinical guidelines.
When analysed quantitively, the complexity and seriousness of the service user’s condition emerged as a prominent CF. Service users with multiple morbidities and complex histories frequently require higher levels of multidisciplinary team involvement, with inputs from multiple teams and clinical services. It is likely that if communication within and between teams and services is suboptimal, the risks for these service users are likely to increase.
Advice for health and social care staff
The SCA disseminates learning derived from claims analysis to health and social care professionals through a variety of mechanisms, including direct engagement with health and social care providers at national and local levels, training and education, newsletters, webinars and other events. The learnings from this study were shared widely with senior clinicians, executives and risk managers in Ireland’s HSE, the organisation tasked with running all public health services in Ireland. Learning was also, and continues to be, shared through educational events and resources. Some of the key advice for health and social care professionals derived from this review included:
Consider enhancing communication skills through training.
Consider using methodologies to enhance communication within and between multidisciplinary teams, such as ISBAR/ISBAR3 and huddles.
Pay particular attention to written and verbal communication when care is being transferred, such as during the handover of care, during the transfer of care between services and at discharge.
Pay particular attention to the consent process and adhere to local guidance (eg, HSE consent policy). Record all discussions regarding the risks, benefits and alternative of treatments and interventions.
Take particular care with documentation. Clear and comprehensive documentation significantly enhances the chances of being able to successfully defend a claim.
Those undertaking diagnostic or therapeutic procedures should have the knowledge/skills and competency suitable to the task. Avoid working outside scope of practice where possible.
Junior staff should be supervised appropriately and empowered to call for assistance when necessary.
Be aware of good practice/clinical guidelines. Good cause should be demonstrated and documented if deviating from widely accepted national/international guidelines
Those ordering tests should follow up on the result and ensure that the appropriate action is undertaken.
Have a heightened awareness of risk when dealing with service users with complex medical and/or psychosocial conditions.
In a timely manner, always remember to report incidents to support a culture of learning from adverse events.
Strengths and limitations
This review presents an analysis of claims from the perspective of the indemnifier. The SCA perspective draws on a wide range of information (including information available on the NIMS database) related to the management of a claim, which can add complementary and valuable insights into the safety issues of service users. The SCA’s perspective is also a legal perspective, with an emphasis on the examination of breach of duty of care and causation.
Many published reports on clinical claims concentrate on the financial aspects of claims, or on particular specialties or claims categories. This review presents data on a broad range of specialties, and, in addition to presenting financial data, provides insights on the clinical failures which result in claims.
While the data presented in this review are unique and give a national view, there remain inherent biases in the analysis of closed claims. Claims generally relate to service user safety issues of a more serious nature. Analysis can also be subjective in nature and is unavoidably retrospective. However, in this report, a systematic approach was designed to mitigate bias where possible. Two internationally recognised incident analysis tools, The London Protocol and the Yorkshire Contributory Framework, were leveraged to create a claims analysis template which standardised data collection.1 2 In addition, a scoring system was employed to determine the most frequently identified CFs. Commonalities in terms of what went wrong and why it went wrong emerged and are presented below. While difficult to compare internationally, where evidence exists on claims analysis, similar themes and dominant issues emerge.9
It is worth noting that the majority of claims finalised in 2017 arose from incidents which occurred between 2009 and 2014 inclusive. Similarly, the majority of claims finalised in 2017 arose from claims which were created (or initiated) between 2011 and 2015. This demonstrates the lag between incident occurrence and claim initiation, and also the lag between claim initiation and claim finalisation. This raises two points of note. First, some of the shortcomings in care identified in this analysis may predate the introduction of policies, procedures and processes to address them. Secondly, a long interval between claim initiation and claim resolution is acknowledged by the SCA as unsatisfactory and often distressing for both plaintiffs and defendants. A preaction protocol in clinical negligence cases, designed to accelerate the process of claim resolution, as provided for in the Legal Services Regulation Act 2015 should, when introduced, assist in addressing this issue.
Conclusions
This report is the first national report in Ireland to provide an in-depth analysis of clinical claims. As noted by the Irish National Adverse Events Studies, not all adverse events are preventable and most health and social care in Ireland is delivered safely.20 21 For those that are preventable, it is to be hoped that a culture of learning when things go wrong will reduce this risk.
In-depth thematic claims analysis at the national level results in valuable learning for health and social care providers. The SCA also has mechanisms to feedback to individual hospitals and care locations on their own claims. Claims analysis is just one way in which the SCA fulfils its clinical risk management function. Other complementary activities include the analysis of patient safety incidents reported on NIMS and the sharing of analysis and advice in relation to those. All activities are designed to share lessons learnt with health and social care providers in order to enhance patient safety.
supplementary material
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Karen A Power, Email: karen.power@ntma.ie.
Irene O'Byrne Maguire, Email: iobyrnemaguire@ntma.ie.
Noelle Byrne, Email: noelle.byrne@ntma.ie.
Deirdre Walsh, Email: deirdre.walsh@ntma.ie.
Karen Robinson, Email: karen.robinson@ntma.ie.
Mark McCullagh, Email: mark.mccullagh@ntma.ie.
Yvonne Fallon, Email: yvonne.fallon@ntma.ie.
Mary Godfrey, Email: marygodfrey@rcsi.ie.
Ann Duffy, Email: ann.duffy@vhi.ie.
Claire O'Regan, Email: claire.oregan@hse.ie.
Mairead Twohig, Email: Mairead.twohig@hse.ie.
Cathal O'Keeffe, Email: cathal.okeeffe@ntma.ie.
Data availability statement
No data are available.
References
- 1.Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998;316:1154–7. doi: 10.1136/bmj.316.7138.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawton R, McEachan RRC, Giles SJ, et al. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf. 2012;21:369–80. doi: 10.1136/bmjqs-2011-000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health Service Executive . Incident management framework. Dublin: Health Service Executive; 2020. [Google Scholar]
- 4.State Claims Agency . National clinical incidents, claims and costs report. Lessons learned, a five year review: 2010-2014. Dublin: National Treasury Management Agency; 2017. [Google Scholar]
- 5.NHS Resolution . NHS resolution annual report and accounts. 2023. [Google Scholar]
- 6.NHS Litigation Authority . Ten years of maternity claims. An analysis of NHS Litigation Authority Data. 2012. [Google Scholar]
- 7.Dinwoodie M. Why patients sue… and how to try and avoid it. Medical Protection Society Casebook Ireland. 2014;22:10–1. [Google Scholar]
- 8.Travaline JM, Ruchinskas R, D’Alonzo GE. Patient-physician communication: why and how. J Am Osteopath Assoc. 2005;105:13–8. [PubMed] [Google Scholar]
- 9.CRICO Strategies . Malpractice risks in communication failures. Annual benchmarking report. Boston: CRICO Strategies; 2015. [Google Scholar]
- 10.Department of Health . Communication (clinical handover) in maternity services. National clinical guideline no.5. Dublin: Department of Health; 2014. [Google Scholar]
- 11.Department of Health . Sepsis management. National clinical guideline no. 6. Dublin: Department of Health; 2014. [Google Scholar]
- 12.Department of Health . Communication (clinical handover) in acute and children’s hospital services. National clinical guideline no.11. Dublin: Department of Health; 2015. [Google Scholar]
- 13.Dutta N, Tweedie J, Peake L, et al. Improving teams in healthcare resource 3: team communication. UK: Royal College of Physicians; 2017. [Google Scholar]
- 14.Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care. 2009;18:137–40. doi: 10.1136/qshc.2007.025247. [DOI] [PubMed] [Google Scholar]
- 15.Müller M, Jürgens J, Redaèlli M, et al. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018;8:e022202. doi: 10.1136/bmjopen-2018-022202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castaldi M, Kaban JM, Petersen M, et al. Implementing Daily Leadership Safety Huddles in a Public Hospital: Bridging the Gap. Qual Manag Health Care. 2019;28:108–13. doi: 10.1097/QMH.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 17.Melton L, Lengerich A, Collins M, et al. Evaluation of Huddles: A Multisite Study. Health Care Manag (Frederick) 2017;36:282–7. doi: 10.1097/HCM.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 18.CRICO Strategies . Malpractice risks in the diagnostic process. Annual benchmarking report. Boston: CRICO Strategies; 2014. [Google Scholar]
- 19.NHS Resolution . Clinical negligence claims in emergency departments in England. Report 1 of 3: high value and fatality related claims. 2022. [Google Scholar]
- 20.Connolly W, Rafter N, Conroy RM, et al. The Irish National Adverse Event Study-2 (INAES-2): longitudinal trends in adverse event rates in the Irish healthcare system. BMJ Qual Saf. 2021;30:547–58. doi: 10.1136/bmjqs-2020-011122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rafter N, Hickey A, Conroy RM, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals-a retrospective record review study. BMJ Qual Saf. 2017;26:111–9. doi: 10.1136/bmjqs-2015-004828. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available.