Abstract
Background:
Exposure to domestic violence by triggering repetitive distress and fear can affect neurodevelopmental and mental health in the short and long term. This, in turn, has been linked to an increased risk of substance abuse, such as alcohol abuse in adulthood.
Objective:
The present study aimed to evaluate the association between exposure to violence from the father toward the mother and alcohol abuse in Peruvian women.
Design:
Cross-sectional study
Methods:
We conducted a secondary analysis of data from the Peruvian Demographic and Family Health Survey (ENDES) of 2019. A total of 19,980 reproductive-aged women (15–49 years old) were surveyed using the Health Questionnaire during 2019. The dependent variable of the study was alcohol abuse, collected through self-report, according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria. Intimate partner violence (IPV; violence perpetrated by the father against the mother) was considered as the exposure variable. To assess the association of interest, we only considered observations with complete data and used binary logistic regression models, calculating crude odds ratios and adjusted odds ratios (aOR). For the multivariable model, we adjusted for confounding variables (age, marital status, education level, wealth index, ethnicity, residence, current smoker, depression, and IPV).
Results:
We analyzed a final sample of 9953 women. The prevalence of interparental violence and alcohol abuse was 41.3% and 1.5%, respectively. We found that interparental violence was associated with higher odds of alcohol abuse (aOR: 2.10; 95% CI: 1.03–4.28) after adjusting for age, marital status, education level, wealth level, ethnicity, area of residence, current smoking, depression, and IPV.
Conclusion:
We identified that women of reproductive age who have been exposed to interparental violence were at higher odds of experiencing alcohol abuse issues.
Keywords: alcohol abuse, domestic violence, health surveys, Peru, violence
Plain language summary
Understanding the link between witnessing parental violence and alcohol abuse in Peruvian women
Witnessing violence between parents during childhood can leave deep emotional scars. This study explores whether such experiences are related to alcohol abuse among Peruvian women in their adult years. Using data from a national health survey in Peru, the experiences of nearly 20,000 women were analyzed to determine if witnessing violence between their parents during childhood was linked to alcohol problems later in life. Responses from the 2019 Peruvian Demographic and Family Health Survey were examined, focusing on women’s reports of childhood exposure to violence between parents and current alcohol abuse, controlling for factors like age, education, and mental health. The study found that women who witnessed their parents engaging in violence were more likely to abuse alcohol as adults. About 41% of the women reported seeing such violence, and of these, a higher proportion struggled with alcohol compared to those who did not witness violence. Understanding the link between childhood experiences and adult behaviors can help develop targeted interventions to prevent alcohol abuse. This research highlights the need for support systems that help women cope with the emotional impacts of childhood trauma, potentially reducing alcohol-related problems in the future.
Introduction
Domestic violence against women is a serious public health issue. 1 In Peru, 57.7% of Peruvian women have experienced some form of violence perpetrated by their partner or husband throughout their lives. 2 Additionally, approximately 10% of women in the country report knowing at least one case of domestic violence that has resulted in the death of a neighbor, friend, or family member. 3 These figures place Peru among the countries with the highest prevalence of psychological, physical, and sexual violence against women in all of Latin America and the Caribbean (LAC).4,5
Within the context of motherhood, domestic violence also impacts children. 6 The exposure of minors to this violence can manifest in various ways, either as direct witnesses to physical or verbal aggression from the father to the mother or by witnessing the residual effects of violence, such as visible injuries and the emotional impact experienced by the mother after the aggression. 7 In high-income countries, it is estimated that up to 59.0% of reported domestic violence cases occur in households where children reside.8 –11 In addition, a statistical profile of violence against children in LAC in 2022 reveals that nearly two out of every three children between the ages of 1 and 14 in the region experience violence in their homes. 12 Unfortunately, specific data on this matter is lacking in the Peruvian context. However, it is plausible to assume that exposure to domestic violence may be equal to or even higher compared to international references due to higher overcrowding in Peruvian households compared to high-income countries. 13
Domestic violence exacerbates the vulnerability of children to develop mental health problems, and the trauma theory emerges as one of the main approaches to understanding this relationship.14,15 According to this theoretical framework, witnessing domestic violence can be traumatic for children, as it triggers emotions such as acute distress or fear. 14 Additionally, it is suggested that contextual and social factors may restrict or limit the capacity for adaptation to this traumatic event in the short, medium, and long term. 14 Following this reasoning, exposure to domestic violence and the environment in which it occurs can impact the functioning of individuals’ nervous system, which in turn may lead to the development of mental health disorders, including alcohol abuse in adulthood. 16
There are various research studies that support the validity of the trauma theory by showing an association between exposure to domestic violence and alcohol abuse in adulthood. Such associations have been observed in studies conducted in countries such as France, 17 England, 18 Thailand, 19 and the United States. 20 However, it is worth noting that, to date, this association has not been specifically explored in women residing in countries in LAC, such as Peru.
It is essential to investigate and understand how these dynamics can manifest in the cultural and social context of LAC, particularly in Peru, where social structures such as machismo prevail, which can hinder a proper adaptation to traumatic situations related to violence between parents.5,21 Furthermore, excessive alcohol consumption in Peru is approximately 22.4%, 22 and the prevalence of alcohol abuse is 5.2%. 23 In this context, the present study aimed to evaluate the association between exposure to violence from the father toward the mother and alcohol abuse in Peruvian women.
Methods
Study design
We conducted a secondary analysis of data from the Peruvian Demographic and Family Health Survey (ENDES) of 2019, which is carried out annually by the National Institute of Statistics and Informatics (INEI). The ENDES includes three questionnaires: the “Household Questionnaire,” the “Individual Questionnaire for Women,” and the “Health Questionnaire.” For the present study, we used information from the latter two questionnaires. 24
This survey has representativeness at the urban–rural, regional, and national levels. The ENDES is a multi-stage survey with a probabilistic sampling design using clusters and stratification at the departmental level, as well as urban and rural areas. The primary sampling unit consists of the selected clusters, whereas the secondary sampling unit was the selected households. Additional information on the methodology of the ENDES survey is available in the technical report. 24 The manuscript has been prepared in accordance with the STROBE guidelines.
Study population and sample
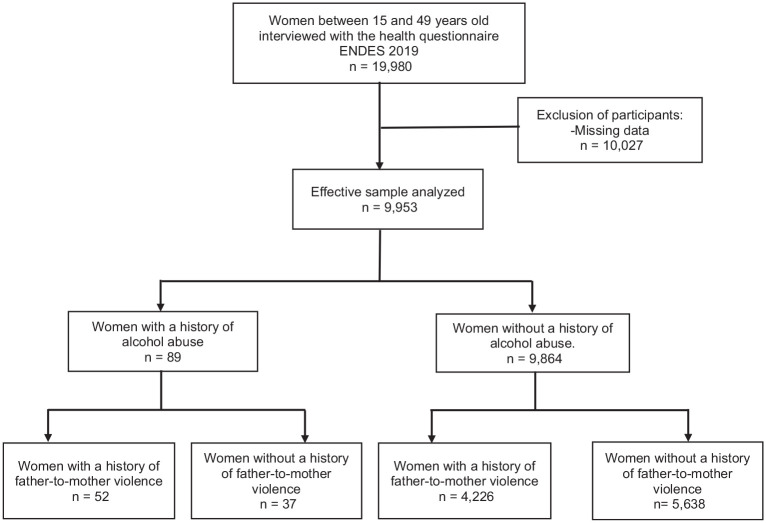
A total of 19,980 reproductive-aged women (15–49 years old) were surveyed using the Health Questionnaire during 2019. This questionnaire includes a section of questions about risk factors for non-communicable diseases, collecting information on alcohol consumption, smoking, among others. For this study, we considered women of reproductive age because the questions related to domestic violence in childhood were only asked to women. In addition, we only considered observations that had complete data on the variables of interest. The effective sample size for our study consisted of 9953 women (Figure 1). We conducted a power analysis based on the González et al. study, assuming a 13% proportion of exposed individuals with the outcome and an expected odds ratio (OR) of 2.11. 18 The power achieved with our data was 100%.
Figure 1.
Flowchart for the sample selection.
Variables
Outcome: alcohol abuse
The dependent variable of the study was alcohol abuse, collected through self-report using the health questionnaire with variables QS713, QS714, QS715, QS716, and QS717, which correspond to items from the Composite International Diagnostic Interview (CIDI 1.1) of the World Health Organization. 25 This instrument evaluates alcohol abuse according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). 26
QS713: In the last 12 months, were there times when drinking or hangovers made it difficult for you to carry out your activities or responsibilities at school, work, or home?
• QS714: In the last 12 months, were there times when alcohol consumption caused arguments or other problems with your family, friends, neighbors, or coworkers?
QS715: Did you continue drinking despite it causing problems with these people?
QS716: In the last 12 months, were there times when you were under the influence of alcohol in situations where you could have been harmed?
QS717: Have you been arrested more than once for disturbing the peace or driving under the influence of alcohol?
According to the DSM-IV criteria, a diagnosis of alcohol abuse is manifested by one or more of the following criteria within a 12-month period: (1) recurrent use of alcohol or drugs that leads to failure to fulfill major role obligations at work, school, or home; (2) recurrent use of alcohol or drugs in situations where it is physically hazardous; (3) recurrent legal problems related to alcohol or drug use; and (4) continued alcohol or drug use despite persistent or recurrent social or interpersonal problems caused or exacerbated by the substance. Alcohol abuse was defined as a positive response to at least one of the components corresponding to the diagnostic criteria.
Exposure: history of interparental violence
History of interparental violence (violence perpetrated by the father against the mother) was considered as the exposure variable for the analysis and was assessed with the following question: “Has your father ever hit your mother?,” with response options being: Yes, no, and don’t know. For the purposes of this study, the variable was defined such that those who answered affirmatively were considered as exposed.
Other variables
The following covariates of interest were selected based on previous literature27 –30: age (15–25, 26–35, 35–49 years), marital status (married or cohabiting, not married or cohabiting), education level (primary or preschool, secondary, higher), employment status (yes, no), health insurance (yes, no), geographical region (Lima Metropolitan, rest of the Coast, Sierra, Selva), residence area (urban, rural), wealth index (first quintile, second quintile, third quintile, fourth quintile, fifth quintile), ethnic origin (mestizo, quechua, black or dark-skinned, others), and daily smoking (yes, no).
Depression was defined using the Patient Health Questionnaire (PHQ-9), previously validated in the Peruvian population, 31 consisting of nine questions (QS700A, QS700B, QS700C, QS700D, QS700E, QS700F, QS700G, QS700H, QS700I), and a score greater than 10 was considered to define major depression based on the study by Kroenke et al. 32
Intimate partner violence (IPV) was considered if the woman experienced any of the following types of violence from her partner in the past 12 months: (1) verbal or psychological violence, defined as experiencing jealousy, accusations of infidelity, restrictions on friendships or family contact, control over her movements or finances, public humiliation, or threats to harm her or take their children; (2) physical violence, including pushing, shaking, throwing objects, slapping, hitting, kicking, strangling, burning, or threats with weapons; or (3) sexual violence, defined as being forced into sexual acts without consent.
It should be noted that the way of assessing violence-related issues was through a standard face-to-face interview, with privacy from other family members.
Statistical analysis
The ENDES 2019 database was downloaded and imported into Stata v.16.0 (Stata Corporation, College Station, TX, USA). All analyses were performed taking into account the complex survey design characteristics and the ENDES weighting factors using the Stata svy module.
For the descriptive analysis, as all variables were categorical, weighted absolute frequencies and proportions were calculated. For the bivariate analysis, a comparison of covariates with the history of interparental violence (exposure) and alcohol abuse (outcome) was conducted. The chi-square test with Rao–Scott correction was used for this purpose.
To assess the association of interest, binary logistic regression models were used, calculating crude odds ratios (cOR) and adjusted odds ratios (aOR). For the multivariable model, an epidemiological approach was employed, adjusting for confounding variables (age, marital status, education level, wealth index, ethnicity, residence, current smoker, depression, and IPV) described in the literature.27 –30 Additionally, a sensitivity analysis using penalized logistic regression was performed. The analyses were reported with their respective 95% confidence intervals (CI), and p-values <0.05 were considered statistically significant.
Ethics and data availability statement
This study was approved by the Ethics Committee of Universidad César Vallejo (027-UI-EM-FCS-UCV). The research involved an analysis of publicly available databases from the INEI website (https://proyectos.inei.gob.pe/microdatos/). None of the databases include personal identifiers. The collection of primary data, carried out by the INEI team, 24 required prior written consent from the participants to participate in the survey. In addition, minors under 18 were interviewed after providing verbal consent and following approval from a parent or guardian present.
Results
Baseline characteristics of the study population
The most frequent age group was 35–49 years (44.5%), with a higher proportion of women being married or living together (79.1%), having secondary education (42.5%), and being employed (75.2%). The majority of participants belonged to Metropolitan area of Lima (34.6%) and the second quintile of wealth (23.9%). Other relevant variables included experiencing depression (7.8%), not being current smokers (95.4%), and suffering from some form of IPV (57.7%) (Table 1).
Table 1.
Characteristics of the study population (n = 9,953).
| Characteristics | n | % a | 95% CI a |
|---|---|---|---|
| Age | |||
| 15–25 years | 2,005 | 13.8 | 12.7–14.9 |
| 26–35 years | 4,547 | 41.7 | 39.7–43.7 |
| 35–49 years | 3,401 | 44.5 | 42.5–46.6 |
| Current marital status | |||
| Married/cohabiting | 8,335 | 79.1 | 77.1–80.9 |
| Unmarried/non-cohabiting | 1,618 | 20.9 | 19.1–22.9 |
| Educational level of the woman | |||
| Primary or preschool | 2,326 | 21.1 | 19.7–22.6 |
| Secondary | 4,485 | 42.5 | 40.6–44.4 |
| Higher education | 3,142 | 36.4 | 34.4–38.4 |
| Employment status | |||
| Yes | 7,155 | 75.2 | 73.5–76.9 |
| No | 2,798 | 24.8 | 23.1–26.5 |
| Health insurance | |||
| Yes | 8,191 | 77.8 | 76.0–79.4 |
| No | 1,762 | 22.2 | 20.6–24.0 |
| Geographic region | |||
| Metropolitan area of Lima | 1,070 | 34.6 | 32.5–36.8 |
| Rest of the coast | 2,770 | 22.9 | 21.6–24.3 |
| Highlands | 3,496 | 26.9 | 25.3–28.4 |
| Jungle | 2,617 | 15.6 | 14.5–16.8 |
| Residence area | |||
| Urban | 6,744 | 78.0 | 76.8–79.0 |
| Rural | 3,209 | 22.0 | 21.0–23.2 |
| Wealth index | |||
| First quintile | 3,009 | 21.5 | 20.3–22.8 |
| Second quintile | 2,824 | 23.9 | 22.4–25.5 |
| Third quintile | 1,903 | 21.4 | 19.8–23.1 |
| Fourth quintile | 1,312 | 17.0 | 15.4–18.7 |
| Fifth quintile | 905 | 16.2 | 14.4–18.2 |
| Ethnic origin | |||
| Mestizo | 3,946 | 45.4 | 43.4–47.4 |
| Quechua | 3,047 | 25.5 | 23.9–27.1 |
| Black or dark-skinned | 1,015 | 10.6 | 9.5–11.8 |
| Others | 1,945 | 18.6 | 17.1–20.2 |
| Depression | |||
| No | 9,310 | 92.2 | 90.9–93.4 |
| Yes | 643 | 7.8 | 6.6–9.1 |
| Current smoker | |||
| No | 9,674 | 95.4 | 94.1–96.5 |
| Yes | 279 | 4.6 | 3.5–5.9 |
| Psychological violence by partner | |||
| No | 4,959 | 47.1 | 45.2–49.1 |
| Yes | 4,994 | 52.9 | 50.9–54.8 |
| Physical violence by partner | |||
| No | 6,996 | 69.8 | 68.1–71.5 |
| Yes | 2,957 | 30.2 | 28.5–31.9 |
| Sexual violence by partner | |||
| No | 9,310 | 91.8 | 90.5–93.0 |
| Yes | 643 | 8.2 | 7.0–9.5 |
| IPV | |||
| No | 4,427 | 42.3 | 40.3–44.2 |
| Yes | 5,526 | 57.7 | 55.8–59.7 |
| Interparental violence | |||
| No | 5,675 | 58.7 | 56.5–60.7 |
| Yes | 4,278 | 41.3 | 39.3–43.5 |
| Alcohol abuse | |||
| No | 9,864 | 98.5 | 97.6–99.1 |
| Yes | 89 | 1.5 | 0.9–2.4 |
CI: confidence interval; IPV: intimate partner violence.
Percentages weighted according to the complex sampling of the survey.
Characteristics of the study population according to the history of interparental violence
The prevalence of interparental violence was 41.3%, and it was significantly more frequent in women with higher education (62.1%; p = 0.027), those who were employed (42.9%; p = 0.010), those belonging to the second and third quintiles of wealth (46.8% and 47.8%, respectively; p < 0.001), those of Quechua ethnicity (50.9%; p < 0.001), those experiencing depression (53.8%; p < 0.001), those who were not current smokers (42.0%; p = 0.025), and those suffering from IPV (46.5%; p < 0.001) (Table 2).
Table 2.
Prevalence of interparental violence, according to the characteristics of the study population (n = 9,953).
| Characteristics | Interparental violence | p a | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % b | 95% CI b | n | % b | 95% CI b | ||
| Age | |||||||
| 15–25 years | 800 | 37.8 | 33.8–42.0 | 1,205 | 62.2 | 58.0–66.2 | 0.283 |
| 26–35 years | 2,019 | 42.5 | 39.4–45.7 | 2,528 | 57.5 | 54.3–60.6 | |
| 35–49 years | 1,459 | 41.4 | 38.1–44.7 | 1,942 | 58.6 | 55.3–61.9 | |
| Current marital status | |||||||
| Married/cohabiting | 3,562 | 41.7 | 39.4–44.0 | 4,773 | 58.3 | 56.0–60.6 | 0.525 |
| Unmarried/non-cohabiting | 716 | 40.1 | 35.7–44.6 | 902 | 59.9 | 55.4–64.3 | |
| Educational level of the woman | |||||||
| Primary or preschool | 961 | 42.4 | 38.7–46.2 | 1,365 | 57.6 | 53.8–61.3 | 0.027 |
| Secondary | 1,991 | 43.8 | 40.9–46.8 | 2,494 | 56.2 | 53.2–59.1 | |
| Higher education | 1,326 | 37.9 | 34.2–41.7 | 1,816 | 62.1 | 58.3–65.8 | |
| Employment status | |||||||
| Yes | 3,202 | 42.9 | 40.4–45.4 | 3,953 | 57.1 | 54.6–59.6 | 0.010 |
| No | 1,076 | 36.7 | 32.8–40.7 | 1,722 | 63.4 | 59.3–67.2 | |
| Health insurance | |||||||
| Yes | 3,535 | 41.0 | 38.8–43.2 | 4,656 | 59.0 | 56.8–61.2 | 0.521 |
| No | 743 | 42.6 | 38.0–47.4 | 1,019 | 57.4 | 52.6–62.0 | |
| Geographic region | |||||||
| Metropolitan area of Lima | 463 | 42.2 | 37.0–47.5 | 607 | 57.8 | 52.5–63.0 | 0.121 |
| Rest of the coast | 1,104 | 37.1 | 34.3–40.0 | 1,666 | 62.9 | 60.0–65.7 | |
| Highlands | 1,543 | 43.2 | 40.7–45.7 | 1,953 | 56.8 | 54.3–59.3 | |
| Jungle | 1,168 | 42.5 | 39.9–45.2 | 1,449 | 57.5 | 54.8–60.1 | |
| Residence area | |||||||
| Urban | 2,973 | 41.9 | 39.3–44.5 | 3,771 | 58.1 | 55.5–60.7 | 0.174 |
| Rural | 1,305 | 39.5 | 37.3–41.7 | 1,904 | 60.5 | 58.3–62.7 | |
| Wealth index | |||||||
| First quintile | 1,185 | 37.8 | 35.4–40.2 | 1,824 | 62.2 | 59.8–64.6 | <0.001 |
| Second quintile | 1,326 | 46.8 | 43.4–50.2 | 1,498 | 53.2 | 49.8–56.6 | |
| Third quintile | 889 | 47.8 | 43.3–52.4 | 1,014 | 52.2 | 47.6–56.7 | |
| Fourth quintile | 566 | 39.9 | 34.5–45.5 | 746 | 60.1 | 54.5–65.5 | |
| Fifth quintile | 312 | 31.1 | 25.4–37.3 | 593 | 69.0 | 62.7–74.6 | |
| Ethnic origin | |||||||
| Mestizo | 1,634 | 40.1 | 36.9–43.3 | 2,312 | 59.9 | 56.7–63.1 | <0.001 |
| Quechua | 1,489 | 50.9 | 47.3–54.5 | 1,558 | 49.1 | 45.5–52.7 | |
| Black or dark-skinned | 388 | 33.6 | 29.0–38.5 | 627 | 66.4 | 61.5–71.0 | |
| Others | 767 | 35.8 | 31.8–40.0 | 1,178 | 64.2 | 60.0–68.2 | |
| Depression | |||||||
| No | 3,905 | 40.3 | 38.2–42.4 | 5,405 | 59.7 | 57.6–61.8 | 0.001 |
| Yes | 373 | 53.8 | 45.5–62.0 | 270 | 46.2 | 38.0–54.5 | |
| Current smoker | |||||||
| No | 4,166 | 42.0 | 39.9–44.1 | 5,508 | 58.0 | 55.9–60.1 | 0.025 |
| Yes | 112 | 28.4 | 19.0–40.3 | 167 | 71.6 | 59.7–81.0 | |
| Psychological violence by partner | |||||||
| No | 1,832 | 36.1 | 33.2–39.1 | 3,127 | 63.9 | 60.9–66.8 | <0.001 |
| Yes | 2,446 | 46.0 | 43.1–48.9 | 2,548 | 54.0 | 51.1–56.9 | |
| Physical violence by partner | |||||||
| No | 2,629 | 35.8 | 33.4–38.3 | 4,367 | 64.2 | 61.7–66.6 | <0.001 |
| Yes | 1,649 | 54.1 | 50.4–57.7 | 1,308 | 45.9 | 42.3–49.6 | |
| Sexual violence by partner | |||||||
| No | 3,909 | 40.2 | 38.0–42.4 | 5,401 | 59.8 | 57.6–62.0 | 0.001 |
| Yes | 369 | 54.5 | 46.0–62.7 | 274 | 45.5 | 37.3–54.0 | |
| IPV | |||||||
| No | 1,544 | 34.3 | 31.3–37.5 | 2,883 | 65.7 | 62.5–68.7 | <0.001 |
| Yes | 2,734 | 46.5 | 43.8–49.2 | 2,792 | 53.5 | 50.8–56.2 | |
CI: confidence interval; IPV: intimate partner violence.
Calculated by the chi-squared test with Rao–Scott correction for complex sampling. Values with p < 0.05 are in bold.
Percentages weighted according to the complex sampling of the survey.
Characteristics of the study population according to the presence of alcohol abuse
The prevalence of alcohol abuse was 1.5%, and it was significantly more frequent in women who were not married or cohabiting (4.7%; p < 0.001), those who were employed (1.9%; p < 0.001), those who lived in urban areas (1.8%; p < 0.001), those who belonged to the fifth quintile of wealth (3.6%; p = 0.009), those who experienced depression (4.1%; p = 0.009), those who were current smokers (13.8%; p < 0.001), and those who suffered from IPV (2.2%; p < 0.001) (Table 3).
Table 3.
Prevalence of alcohol abuse according to the characteristics of the study population (n = 9,953).
| Characteristics | Alcohol abuse | p a | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % b | 95% CI b | n | % b | 95% CI b | ||
| Age | |||||||
| 15–25 years | 13 | 1.5 | 0.6–4.2 | 1,992 | 98.5 | 95.8–99.4 | 0.115 |
| 26–35 years | 50 | 2.1 | 1.0–4.3 | 4,497 | 97.9 | 95.7–99.0 | |
| 35–49 years | 26 | 0.8 | 0.5–1.4 | 3,375 | 99.2 | 98.6–99.5 | |
| Current marital status | |||||||
| Married/cohabiting | 53 | 0.6 | 0.4–0.9 | 8,282 | 99.4 | 99.1–99.6 | <0.001 |
| Unmarried/non-cohabiting | 36 | 4.7 | 2.4–9.1 | 1,582 | 95.3 | 90.9–97.6 | |
| Educational level of the woman | |||||||
| Primary or preschool | 4 | 0.3 | 0.1–1.0 | 2.322 | 99.7 | 99.0–99.9 | 0.0719 |
| Secondary | 42 | 1.4 | 0.8–2.7 | 4,443 | 98.6 | 97.3–99.2 | |
| Higher education | 43 | 2.2 | 1.0–4.4 | 3,099 | 97.9 | 95.6–99.0 | |
| Employment status | |||||||
| Yes | 79 | 1.9 | 1.1–3.1 | 7,076 | 98.1 | 96.9–98.9 | <0.001 |
| No | 10 | 0.2 | 0.2–0.4 | 2,788 | 99.8 | 99.6–99.9 | |
| Health insurance | |||||||
| Yes | 56 | 1.1 | 0.6–2.2 | 8,135 | 98.9 | 97.8–99.4 | 0.078 |
| No | 33 | 2.6 | 1.3–5.0 | 1,729 | 97.4 | 95.0–98.7 | |
| Geographic region | |||||||
| Metropolitan area of Lima | 18 | 2.2 | 1.0–5.1 | 1,052 | 97.8 | 94.9–99.0 | 0.149 |
| Rest of the coast | 23 | 1 | 0.6–1.8 | 2,747 | 99 | 98.2–99.4 | |
| Highlands | 25 | 1.2 | 0.7–2.1 | 3,471 | 98.8 | 97.9–99.3 | |
| Jungle | 23 | 0.9 | 0.5–1.7 | 2,594 | 99.1 | 98.3–99.5 | |
| Residence area | |||||||
| Urban | 83 | 1.8 | 1.1–2.9 | 6,661 | 98.2 | 97.1–98.9 | <0.001 |
| Rural | 6 | 0.3 | 0.1–0.8 | 3,203 | 99.7 | 99.2–99.9 | |
| Wealth index | |||||||
| First quintile | 3 | 0.2 | 0.0–0.9 | 3,006 | 99.8 | 99.1–99.9 | 0.009 |
| Second quintile | 21 | 0.8 | 0.5–1.4 | 2,803 | 99.2 | 98.6–99.5 | |
| Third quintile | 26 | 1.4 | 0.6–3.0 | 1,877 | 98.6 | 97.0–99.4 | |
| Fourth quintile | 23 | 2.1 | 0.9–4.9 | 1,289 | 97.9 | 95.1–99.1 | |
| Fifth quintile | 16 | 3.6 | 1.4–8.9 | 889 | 96.5 | 91.1–98.6 | |
| Ethnic origin | |||||||
| Mestizo | 44 | 1.9 | 0.9–3.8 | 3,902 | 98.1 | 96.2–99.1 | 0.437 |
| Quechua | 22 | 1.3 | 0.5–3.2 | 3,025 | 98.7 | 96.8–99.5 | |
| Black or dark-skinned | 10 | 0.7 | 0.3–1.8 | 1,005 | 99.3 | 98.2–99.7 | |
| Others | 13 | 1.1 | 0.5–2.2 | 1,932 | 98.9 | 97.8–99.5 | |
| Depression | |||||||
| No | 72 | 1.2 | 0.7–2.2 | 9,238 | 98.8 | 97.8–99.3 | 0.009 |
| Yes | 17 | 4.1 | 1.9–8.6 | 626 | 95.9 | 91.4–98.1 | |
| Current smoker | |||||||
| No | 66 | 0.9 | 0.6–1.3 | 9,608 | 99.1 | 98.7–99.4 | <0.001 |
| Yes | 23 | 13.8 | 5.3–31.3 | 256 | 86.2 | 68.7–94.7 | |
| Psychological violence by partner | |||||||
| No | 22 | 0.5 | 0.2–0.9 | 4,937 | 99.5 | 99.1–99.8 | <0.001 |
| Yes | 67 | 2.4 | 1.3–4.1 | 4,927 | 97.7 | 95.9–98.7 | |
| Physical violence by partner | |||||||
| No | 45 | 0.8 | 0.4–1.4 | 6,951 | 99.3 | 98.6–99.6 | 0.001 |
| Yes | 44 | 3.1 | 1.6–5.9 | 2,913 | 96.9 | 94.1–98.4 | |
| Sexual violence by partner | |||||||
| No | 78 | 1.4 | 0.8–2.3 | 9,232 | 98.6 | 97.7–99.2 | 0.482 |
| Yes | 11 | 2.2 | 0.7–6.9 | 632 | 97.8 | 93.1–99.3 | |
| IPV | |||||||
| No | 19 | 0.4 | 0.2–0.8 | 4,408 | 99.6 | 99.2–99.8 | <0.001 |
| Yes | 70 | 2.2 | 1.3–3.8 | 5,456 | 97.8 | 96.2–98.7 | |
| Interparental violence | |||||||
| No | 37 | 1.3 | 0.5–2.9 | 5,638 | 98.8 | 97.1–99.5 | 0.488 |
| Yes | 52 | 1.8 | 1.1–2.7 | 4,226 | 98.2 | 97.3–98.9 | |
CI: confidence interval; IPV: intimate partner violence.
Calculated using the chi-squared test with Rao–Scott correction for complex sampling. Values with p < 0.05 are in bold.
Percentages weighted according to the complex sampling of the survey.
Association between the history of interparental violence and alcohol abuse
We found that interparental violence was associated with higher odds of alcohol abuse (aOR: 2.10; 95% CI: 1.03–4.28) after adjusting for age, marital status, education level, wealth level, ethnicity, area of residence, current smoking, depression, and IPV (Table 4). Additionally, in the adjusted model using penalized logistic regression, we also found that interparental violence was associated with an increased odds of alcohol abuse (aOR: 1.73; 95% CI: 1.12–2.68) (Supplemental Table 1).
Table 4.
Logistic regression models to assess the association between a history of interparental violence and alcohol abuse, ENDES 2019.
| Characteristics | Crude model | Adjusted epidemiological model a | ||||
|---|---|---|---|---|---|---|
| cOR | 95% CI | p | aOR | 95% CI | p | |
| Interparental violence | ||||||
| No | Ref. | Ref. | ||||
| Yes | 1.41 | 0.53–3.71 | 0.490 | 2.10 | 1.03–4.28 | 0.042 |
The odds ratios and confidence intervals were calculated taking into account the complex sampling of the survey. Values with p < 0.05 are in bold. cOR: crude odds ratio; aOR: adjusted odds ratio; CI: confidence interval.
Adjusted for age, current marital status, educational level of women, wealth index, ethnicity, area of residence, current smoker, depression, and intimate partner violence.
Discussion
Main findings
In Peru, 4 out of every 10 women of reproductive age had a history of interparental violence, and nearly 2% of the total reported alcohol abuse in 2019. Furthermore, in our study, we found an association between these two variables.
Comparison with other studies
Our study revealed a high prevalence of interparental violence, which exceeds the figures reported in previous research, regardless of the socioeconomic level of the study population. Specifically, the cases of violence perpetrated by the father toward the mother in our study far exceed the rates reported in high-income countries like Spain (6.2%) 33 and the United States (13.7%). 8 When comparing with Thailand (11.6%), 19 a nation with similar middle-high income status as Peru, we observe the same trend. Likewise, when comparing our data with those from low or low-to-middle-income countries in sub-Saharan Africa, such as Angola, Ivory Coast, Burundi, Kenya, Rwanda, Tanzania, among others, our prevalence is also notably higher. 34
On the other hand, the prevalence of alcohol abuse among Peruvian women participating in our study in the past 12 months was 1.5%. This is much lower than the 12-month prevalence of alcohol abuse reported in adult women from countries such as the United States (10.4%), 35 Greece (8.5%), 36 Germany (11.0%), 37 South Africa (6.0%), 38 and Brazil (5.1%). 39 Our result only showed a relatively similar prevalence to what has been reported in adult women from Asian countries such as Lebanon (1.6%), 40 Hong Kong (0.7%), 41 and Singapore (0.3%), 42 indicating a 12-month prevalence of alcohol abuse close to 1%.
In our final analysis, after adjusting for confounding variables, we found a significant association between our variables of interest. Our results are consistent with a sub-analysis of a previous study that revealed that exposure to domestic violence by the father toward the mother is a significant risk factor for alcohol abuse in women in the United States. 20 However, in another sub-analysis of the same study, the significance of the relationship was not found after adjusting not only for sociodemographic variables but also for parental alcohol and drug problems, and comorbidities, including major depressive disorder, generalized anxiety disorder, antisocial personality disorder, exposure to adult trauma, and post-traumatic stress disorder. 20 It is important to mention that the objective of that study was to evaluate whether experiencing any type of interpersonal violence during childhood, including both physical and sexual abuse, as well as witnessing domestic violence, constitutes a risk factor for alcohol abuse in adulthood. In this sense, the results of the previously presented sub-analyses, which considered only exposure to domestic violence as an independent variable and risk factor for alcohol abuse in women, may have lacked sufficient statistical power to detect significant results, in case the relationships indeed existed.
Finally, our findings are consistent with those of other sub-analyses of research conducted in larger populations than ours, such as those carried out in France, 17 Thailand, 19 and England, 18 which also found a significant association between exposure to domestic violence and alcohol abuse. These studies included both male and female children and evaluated exposure to domestic violence perpetrated by both parents. Like our study, they included sociodemographic variables in their adjustment model, although they did not consider comorbidities such as depression and being a smoker, which were included in our study.
Interpretation of results
We employed the trauma theory to elucidate the findings of our study.14,43 Although most research focused on the trauma perspective has primarily aimed to describe how parental violence toward children during childhood is a risk factor for alcohol abuse in adulthood, 44 our results demonstrate that exposure to domestic violence can also constitute a traumatic event that increases the risk of alcohol abuse.
The trauma model provides insight into how exposure to domestic violence can lead to emotional adjustment problems at two critical moments. 14 The first moment occurs in the short term, involving immediate post-trauma reactions, such as exposure to domestic violence. 43 These reactions entail complex sensory, physiological, and cognitive experiences that can result in acute distress. 43 In children who witness domestic violence, their distress may be comparable to that experienced by children who have directly suffered violence. 45 This occurs because children may perceive a sense of threat and vulnerability in an environment that should otherwise guarantee their safety.
The second moment encompasses the course and adaptation to traumatic events over time. Trauma theory posits that these traumatic experiences and the context that facilitates their re-experiencing, such as constant exposure to domestic violence, can alter the functioning of the nervous system. 14 An altered nervous system can become hypersensitive, leading to increased reactivity even in non-threatening situations. 14 This state may give rise to maladaptive coping strategies, such as alcohol consumption, to alleviate emotional discomfort and traumatic memories, thus fostering the development of alcohol abuse in adulthood. 46
In the Peruvian context, social structures act both as facilitators for increased exposure to domestic violence and as barriers to adequate adaptation to traumatic events linked to violence.21,47 In Peru, 57.7% of women have experienced some form of violence from their partner or husband throughout their lives. 2 Additionally, approximately 10% of women report knowing at least one case of domestic violence that resulted in the death of an acquaintance. 3 These figures place Peru among the countries with the highest prevalence of psychological, physical, and sexual violence against women in LAC.4,5
Power imbalances, entrenched gender stereotypes, and economic disparities can promote the normalization of violence and hinder the efforts of victims to seek professional help. 48 As a result, one of the coping strategies adopted by these women may be alcohol abuse, used to manage emotional distress and traumatic memories. Our study encompasses one of the mechanisms that may understand alcohol abuse in Peru. The study’s findings suggest that alcohol abuse is not culturally normative in the country due to the observed low prevalence. However, further exploration is required to fully understand these patterns and their implications
Relevance in public health
We identified that violence against women, particularly in the context of motherhood, not only affects the mental and physical health of the mothers but also represents a higher odds factor for alcohol abuse in daughters exposed to such violence. The link between domestic violence and alcohol abuse underscores the need for a comprehensive approach to safeguard the health and well-being of women.
Although the prevention of violence against women and mental health care have been declared public health priorities in Peru in recent years, the responses to these issues have proven to be inadequate. 49 Specific regulations for the protection of women have been implemented in Peru, leading to the “National Program for the Prevention and Eradication of Violence against Women and Family Group Members.” This program includes services such as the 100 Helpline and Women’s Emergency Centers. 50 However, the prevalence of domestic violence against women persists at alarmingly high levels over time. Simultaneously, mental health reform has been carried out with the establishment of Community Mental Health Centers 51 for the prevention and control of addictions. Nevertheless, these initiatives face limitations due to the high demand that exceeds available resources, including infrastructure, medication supply, and trained personnel, which hinders effectiveness in alcohol abuse prevention.52,53
It is imperative that the Ministry of Health and the Ministry of Women and Vulnerable Populations in Peru intensify their collaboration to comprehensively address the impact of domestic violence on children. This involves not only providing timely care to victims and witnesses of violence but also preventing revictimization and promoting healthy coping strategies to avoid substance abuse, such as alcohol. To achieve this, it is necessary to strengthen the collaboration between Community Mental Health Centers and Women’s Emergency Centers, capitalizing on their respective strengths and specialized knowledge. In addition to interagency collaboration, it is essential to allocate adequate resources to ensure the effectiveness of mental health initiatives and violence prevention efforts. Investing in the quantity of programs alone is not enough, ensuring the quality of services and continuous training of personnel is crucial. The integration of interdisciplinary approaches and the promotion of best practices are fundamental to effectively confront these challenges.
It is important to emphasize that individual efforts are insufficient to overcome problems of such complexity. Only through strong and coordinated collaboration among all stakeholders involved will a significant impact be achieved in preventing violence and promoting mental health in the Peruvian context.
Limitations
Our study has some limitations. First, our data were based solely on physical violence by the father toward the mother, not incorporating cases of verbal or psychological violence. These types of violence are the most prevalent forms reported by women in Peru, so the actual prevalence of father’s violence toward the mother in Peru may be even higher than our results indicate. Additionally, the measurement of alcohol abuse in the ENDES is done using DSM-IV criteria and does not utilize a validated and standardized measure like the AUDIT, which could affect the accuracy in detecting cases of alcohol abuse. Second, the representativeness of the sample may be limited in certain demographic groups, such as the LGBTI community, which may not be adequately represented in the survey. This point is particularly relevant as these groups are often more exposed to violence in society. Third, we lost 23,336 participants due to missing data, which represents a significant reduction in our sample size and could introduce selection bias. This is especially concerning as the reasons for non-response could be related to factors such as the stigma associated with substance abuse, like alcohol, which might have influenced some women’s decision not to participate in the survey. Fourth, the ENDES has limitations in the information collected, as it does not assess certain variables that are associated with both exposure to domestic violence and alcohol abuse. Some of these variables include the parents’ alcohol consumption history, the presence of comorbidities such as post-traumatic stress disorder or anxiety, and the consumption of substances other than alcohol and tobacco. These omissions limit the ability to control for confounding factors and obtain more accurate results. Finally, it is important to recognize that the type of data collection method used can influence the results, and this should be noted as a limitation. The self-reporting method, in particular, can be subject to biases of memory and social desirability, which might affect the accuracy of the responses provided by participants.
Despite the noted limitations, our study stands out as a pioneer in the specific analysis of women exposed to domestic violence between parents in a LAC country. To the best of our knowledge, no previous studies have focused on this particular population. This strength allows us to gain a deeper understanding of the unique experiences and challenges these women face in the context of domestic violence.
Conclusion
We identified that women of reproductive age who have been exposed to interparental violence are at a higher odd of experiencing alcohol abuse issues.
We recommend the adoption of standardized measures, such as the AUDIT, in ENDES evaluations for a more accurate assessment of alcohol abuse and the inclusion of other forms of domestic violence, such as psychological and verbal violence. Additionally, we encourage the replication of this study in other Latin American and Caribbean nations that share similarities with the reality of Peruvian women to gain a more comprehensive and comparative understanding of the challenges and factors associated with domestic violence and alcohol abuse. This will enable the generation of more robust evidence and have an effective impact at the regional level.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057241277533 for Association between history of interparental violence and alcohol abuse among reproductive-age women: Evidence from the Peruvian Demographic and Health Survey by Carolain M Zamora-Ramírez, Brenda Caira-Chuquineyra, Daniel Fernandez-Guzman, Raisa N Martinez-Rivera, Anita P Llamo-Vilcherrez, Ricardo A Gálvez-Arévalo, Diego Urrunaga-Pastor and Carlos J Toro-Huamanchumo in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057241277533 for Association between history of interparental violence and alcohol abuse among reproductive-age women: Evidence from the Peruvian Demographic and Health Survey by Carolain M Zamora-Ramírez, Brenda Caira-Chuquineyra, Daniel Fernandez-Guzman, Raisa N Martinez-Rivera, Anita P Llamo-Vilcherrez, Ricardo A Gálvez-Arévalo, Diego Urrunaga-Pastor and Carlos J Toro-Huamanchumo in Women’s Health
Acknowledgments
None.
Footnotes
Author’s Note: Ricardo A. Gálvez-Arévalo is also affiliated to Universidad Peruana Cayetano Heredia.
ORCID iDs: Ricardo A Gálvez-Arévalo  https://orcid.org/0000-0002-1006-1523
https://orcid.org/0000-0002-1006-1523
Diego Urrunaga-Pastor  https://orcid.org/0000-0002-8339-162X
https://orcid.org/0000-0002-8339-162X
Carlos J Toro-Huamanchumo  https://orcid.org/0000-0002-4664-2856
https://orcid.org/0000-0002-4664-2856
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: This study was approved by the Ethics Committee of Universidad César Vallejo (027-UI-EM-FCS-UCV). The research involved an analysis of publicly available databases from the INEI website (https://proyectos.inei.gob.pe/microdatos/). None of the databases include personal identifiers. The collection of primary data, carried out by the INEI team, 24 required prior written consent from the participants to participate in the survey. In addition, minors under 18 were interviewed after providing verbal consent and following approval a parent or guardian present.
Consent for publication: Not applicable.
Author contribution(s): Carolain M Zamora-Ramírez: Conceptualization; Investigation; Writing – original draft
Brenda Caira-Chuquineyra: Formal analysis; Investigation; Methodology; Writing – original draft.
Daniel Fernandez-Guzman: Formal analysis; Investigation; Methodology; Writing – original draft.
Raisa N Martinez-Rivera: Investigation; Methodology; Writing – original draft.
Anita P Llamo-Vilcherrez: Investigation; Methodology; Writing – original draft.
Ricardo A Gálvez-Arévalo: Investigation; Methodology; Writing – original draft.
Diego Urrunaga-Pastor: Formal analysis; Investigation; Methodology; Writing – original draft.
Carlos J Toro-Huamanchumo: Conceptualization; Formal analysis; Investigation; Methodology; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: The data supporting the findings of this study are openly available in the INEI database at https://proyectos.inei.gob.pe/microdatos/. These datasets were derived from publicly available sources and do not include any personal identifying information.
References
- 1. World Health Organization. Violence against women [Fact Sheet] [Internet]. WHO, https://www.who.int/news-room/fact-sheets/detail/violence-against-women (2021, accessed January 2024).
- 2. Instituto Nacional de Estadística e Informática. Encuesta Demográfica y de Salud Familiar 2019 [Internet]. INEI, https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Endes2019/pdf/cap012.pdf (2019, accessed January 2024).
- 3. Mora Ruiz C. Madres e hijas maltratadas: La transmisión intergeneracional de la violencia doméstica en el Perú. Avances de Investigación. Lima, Perú: Grupo de Análisis para el Desarrollo (GRADE). 2013. [Google Scholar]
- 4. Bott S, Guedes A, Ruiz-Celis AP, et al. Intimate partner violence in the Americas: a systematic review and reanalysis of national prevalence estimates. Rev Panam Salud Publica Pan Am J Public Health 2019; 43:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pan American Health Organization and Centers for Disease Control and Prevention. Violence against women in Latin America and the Caribbean: a comparative analysis of population-based data from 12 countries. Washington, DC: PAHO, 2012. [Google Scholar]
- 6. Kelley ML, Klostermann K, Doane AN, et al. The case for examining and treating the combined effects of parental drug use and interparental violence on children in their homes. Aggress Violent Behav 2010; 15(1): 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holden GW. Children exposed to domestic violence and child abuse: terminology and taxonomy. Clin Child Fam Psychol Rev 2003; 6(3): 151–160. [DOI] [PubMed] [Google Scholar]
- 8. McDonald R, Jouriles EN, Ramisetty-Mikler S, Caetano R, Green CE. Estimating the number of American children living in partner-violent families. J Fam Psychol 2006; 20(1): 137–142. [DOI] [PubMed] [Google Scholar]
- 9. Shields M, Tonmyr L, Hovdestad WE, et al. Exposure to family violence from childhood to adulthood. BMC Public Health. 2020; 20(1): 1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Steketee M, Aussems C, Marshall IH. Exploring the impact of child maltreatment and interparental violence on violent delinquency in an international sample. J Interpers Violence 2021; 36(13–14): NP7319–NP7349. [DOI] [PubMed] [Google Scholar]
- 11. van Berkel SR, Prevoo MJL, Linting M, et al. Prevalence of child maltreatment in the Netherlands: an update and cross-time comparison. Child Abuse Negl 2020; 103: 104439. [DOI] [PubMed] [Google Scholar]
- 12. United Nations Children’s Fund. A statistical profile of violence against children in Latin America and the Caribbean. New York: UNICEF, 2022. [Google Scholar]
- 13. Meng G, Hall GB. Assessing housing quality in metropolitan Lima, Peru. J Hous Built Environ 2006; 21(4): 413–439. [Google Scholar]
- 14. Alisic E, Jongmans MJ, van Wesel F, et al. Building child trauma theory from longitudinal studies: a meta-analysis. Clin Psychol Rev 2011; 31(5): 736–747. [DOI] [PubMed] [Google Scholar]
- 15. Fergusson DM, Horwood LJ. Exposure to interparental violence in childhood and psychosocial adjustment in young adulthood. Child Abuse Negl 1998; 22(5): 339–357. [DOI] [PubMed] [Google Scholar]
- 16. Moustafa AA, Parkes D, Fitzgerald L, et al. The relationship between childhood trauma, early-life stress, and alcohol and drug use, abuse, and addiction: an integrative review. Curr Psychol 2021; 40(2): 579–584. [Google Scholar]
- 17. Roustit C, Renahy E, Guernec G, et al. Exposure to interparental violence and psychosocial maladjustment in the adult life course: advocacy for early prevention. J Epidemiol Community Health 2009; 63(7): 563–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. González RA, Kallis C, Ullrich S, et al. Childhood maltreatment and violence: mediation through psychiatric morbidity. Child Abuse Negl 2016; 52: 70–84. [DOI] [PubMed] [Google Scholar]
- 19. Jirapramukpitak T, Harpham T, Prince M. Family violence and its ‘adversity package’: a community survey of family violence and adverse mental outcomes among young people. Soc Psychiatry Psychiatr Epidemiol 2011; 46(9): 825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Meyers JL, Sartor CE, Werner KB, et al. Childhood interpersonal violence and adult alcohol, cannabis, and tobacco use disorders: variation by race/ethnicity? Psychol Med 2018; 48(9): 1540–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Glass J, Owen J. Latino fathers: The relationship among machismo, acculturation, ethnic identity, and paternal involvement. Psychol Men Masculinity 2010; 11(4): 251–261. [Google Scholar]
- 22. Hernández-Vásquez A, Chacón-Torrico H, Vargas-Fernández R, et al. Gender differences in the factors associated with alcohol binge drinking: a population-based analysis in a Latin American Country. Int J Environ Res Public Health 2022; 19(9): 4931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Caira-Chuquineyra B, Fernandez-Guzman D, Quispe-Vicuña C, et al. Factors associated with alcohol abuse in the Peruvian population: analysis of a national health survey 2019. J Public Health (Oxf) 2023; 45(2): e204–e214. [DOI] [PubMed] [Google Scholar]
- 24. Instituto Nacional de Estadística e Informática. Encuesta Demografica y de Salud Familiar 2019—Ficha Técnica [Internet]. INEI, https://proyectos.inei.gob.pe/endes/2019/documentos_2019/FICHA_TECNICA_ENDES%202019.pdf (2019, accessed January 2024).
- 25. Cottler LB, Robins LN, Grant BF, et al. The CIDI-core substance abuse and dependence questions: cross-cultural and nosological issues. The WHO/ADAMHA Field Trial. Br J Psychiatry 1991; 159: 653–658. [DOI] [PubMed] [Google Scholar]
- 26. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: APA, 1994. [Google Scholar]
- 27. Brisibe S, Ordinioha B, Dienye PO. Intersection between alcohol abuse and intimate partner’s violence in a rural Ijaw community in Bayelsa State, South-South Nigeria. J Interpers Violence 2012; 27(3): 513–522. [DOI] [PubMed] [Google Scholar]
- 28. Catalá-Miñana A, Lila M, Oliver A, et al. Contextual factors related to alcohol abuse among intimate partner violence offenders. Subst Use Misuse 2017; 52(3): 294–302. [DOI] [PubMed] [Google Scholar]
- 29. La Flair LN, Bradshaw CP, Storr CL, et al. Intimate partner violence and patterns of alcohol abuse and dependence criteria among women: a latent class analysis. J Stud Alcohol Drugs 2012; 73(3): 351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Watson-Singleton NN, Florez IA, Clunie AM, et al. Psychosocial mediators between intimate partner violence and alcohol abuse in low-income African American women. Violence Against Women 2020; 26(9): 915–934. [DOI] [PubMed] [Google Scholar]
- 31. Calderón M, Gálvez-Buccollini JA, Cueva G, et al. [Validation of the Peruvian version of the PHQ-9 for diagnosing depression]. Rev Peru Med Exp Salud Publica 2012; 29(4): 578–579. [DOI] [PubMed] [Google Scholar]
- 32. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ibabe I, Arnoso A, Elgorriaga E. Child-to-parent violence as an intervening variable in the relationship between inter-parental violence exposure and dating violence. Int J Environ Res Public Health 2020; 17(5): 1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Aboagye RG, Seidu AA, Asare BYA, et al. Exposure to interparental violence and justification of intimate partner violence among women in sexual unions in sub-Saharan Africa. Arch Public Health 2021; 79(1): 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 Alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry 2015; 72(8): 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bellos S, Petrikis P, Malliori M, et al. Prevalence of alcohol use disorders and their association with sociodemographic determinants and depression/anxiety disorders in a representative sample of the Greek general population. Psychiatry J 2020; 2020: 4841050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Adler J, Rissmann A, Kropf S, et al. Estimated prevalence of harmful alcohol consumption in pregnant and nonpregnant women in saxony-anhalt (NorthEast Germany) using biomarkers. Alcohol Clin Exp Res 2021; 45(4): 819–827. [DOI] [PubMed] [Google Scholar]
- 38. Andersson LMC, Twum-Antwi A, Staland-Nyman C, et al. Prevalence and socioeconomic characteristics of alcohol disorders among men and women in the Eastern Cape Province, South Africa. Health Soc Care Community 2018; 26(1): e143–e153. [DOI] [PubMed] [Google Scholar]
- 39. Wiener CD, Moreira FP, Zago A, et al. Mood disorder, anxiety, and suicide risk among subjects with alcohol abuse and/or dependence: a population-based study. Braz J Psychiatry 2018; 40(1): 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yazbek JC, Haddad R, Bou Khalil R, et al. Prevalence and correlates of alcohol abuse and dependence in Lebanon: results from the Lebanese Epidemiologic Survey on Alcohol (LESA). J Addict Dis 2014; 33(3): 221–233. [DOI] [PubMed] [Google Scholar]
- 41. Kim JH, Lee S, Chow J, et al. Prevalence and the factors associated with binge drinking, alcohol abuse, and alcohol dependence: a population-based study of Chinese adults in Hong Kong. Alcohol Alcohol 2008; 43(3): 360–370. [DOI] [PubMed] [Google Scholar]
- 42. Goh CMJ, Asharani PV, Abdin E, et al. Gender differences in alcohol use: a nationwide study in a multiethnic population. Int J Ment Health Addict 2024; 22: 1161–1175. [Google Scholar]
- 43. Pynoos RS, Steinberg AM, Piacentini JC. A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biol Psychiatry 1999; 46(11): 1542–1554. [DOI] [PubMed] [Google Scholar]
- 44. Walsh K, Latzman NE, Latzman RD. Pathway from child sexual and physical abuse to risky sex among emerging adults: the role of trauma-related intrusions and alcohol problems. J Adolesc Health 2014; 54(4): 442–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abbassi A, Aslinia SD. Family violence, trauma and social learning theory. J Prof Couns Pract Theory Res 2010; 38(1): 16–27. [Google Scholar]
- 46. Covington SS. Women and addiction: a trauma-informed approach. J Psychoactive Drugs 2008;Suppl 5: 377–385. [DOI] [PubMed] [Google Scholar]
- 47. Chon DS. Contributing factors for high homicide rate in Latin America: a critical test of Neapolitan’s regional subculture of violence thesis. J Fam Violence 2011; 26(4): 299–307. [Google Scholar]
- 48. Flake DF, Forste R. Fighting families: family characteristics associated with domestic violence in five Latin American countries. J Fam Violence 2006; 21(1): 19–29. [Google Scholar]
- 49. Boesten J. Pushing back the boundaries: social policy, domestic violence and women’s organisations in Peru. J Lat Am Stud 2006; 38(2): 355–378. [Google Scholar]
- 50. Ministerio de la Mujer y Poblaciones Vulnerables. Reportar casos de violencia contra las mujeres e integrantes del grupo familiar [Internet]. MIMP, https://www.gob.pe/479-reportar-casos-de-violencia-contra-las-mujeres-e-integrantes-del-grupo-familiar (2023, accessed January 2024).
- 51. Ministerio de Salud. Conocer los Centros de Salud Mental Comunitaria en el Perú [Internet]. MINSA, https://www.gob.pe/10942-conocer-los-centros-de-salud-mental-comunitaria-en-el-peru (2023).
- 52. Castillo-Martell H, Aguirre-Castañeda H, Carbone-Campoverde F, et al. Análisis del funcionamiento y rol de los Grupos de Acogimiento en la atención de la salud mental comunitaria. Lima, Perú, 2019. Rev Neuropsiquiatr 2021; 84(4): 269–279. [Google Scholar]
- 53. Castillo-Martell H, Cutipé-Cárdenas Y. Implementación, resultados iniciales y sostenibilidad de la reforma de servicios de salud mental en el Perú, 2013–2018. Rev Peru Med Exp Salud Publica 2019; 36(2): 326–333. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057241277533 for Association between history of interparental violence and alcohol abuse among reproductive-age women: Evidence from the Peruvian Demographic and Health Survey by Carolain M Zamora-Ramírez, Brenda Caira-Chuquineyra, Daniel Fernandez-Guzman, Raisa N Martinez-Rivera, Anita P Llamo-Vilcherrez, Ricardo A Gálvez-Arévalo, Diego Urrunaga-Pastor and Carlos J Toro-Huamanchumo in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057241277533 for Association between history of interparental violence and alcohol abuse among reproductive-age women: Evidence from the Peruvian Demographic and Health Survey by Carolain M Zamora-Ramírez, Brenda Caira-Chuquineyra, Daniel Fernandez-Guzman, Raisa N Martinez-Rivera, Anita P Llamo-Vilcherrez, Ricardo A Gálvez-Arévalo, Diego Urrunaga-Pastor and Carlos J Toro-Huamanchumo in Women’s Health