Abstract
BACKGROUND:
Heterogeneity in trauma center designation and injury volume offer possible explanations for inconsistencies in pediatric trauma center designation’s association with lower mortality among children. We hypothesized that rigorous trauma center verification, regardless of volume, would be associated with lower firearm injury-associated mortality in children.
STUDY DESIGN:
This retrospective cohort study leveraged the California Office of Statewide Health Planning and Development patient discharge data. Data from children aged 0 to 14 years in California from 2005 to 2018 directly transported with firearm injuries were analyzed. American College of Surgeons (ACS) trauma center verification level was the primary predictor of in-hospital mortality. Centers’ annual firearm injury volume data were analyzed as a mediator of the association between center verification level and in-hospital mortality. Two mixed-effects multivariable logistic regressions modeled in-hospital mortality and the estimated association with center verification while adjusting for patient demographic and clinical characteristics. One model included the center’s firearm injury volume and one did not.
RESULTS:
The cohort included 2,409 children with a mortality rate of 8.6% (n = 206). Adjusted odds of mortality were lower for children at adult level I (adjusted odds ratio [aOR] 0.38, 95% CI 0.19 to 0.80), pediatric (aOR 0.17, 95% CI 0.05 to 0.61), and dual (aOR 0.48, 95% CI 0.25 to 0.93) trauma centers compared to nontrauma/level III/IV centers. Firearm injury volume did not mediate the association between ACS trauma center verification and mortality (aOR/10 patient increase in volume 1.01, 95% CI 0.99 to 1.03).
CONCLUSIONS:
Trauma center verification level, regardless of firearm injury volume, was associated with lower firearm injury-associated mortality, suggesting that the ACS verification process is contributing to achieving optimal outcomes.
Firearm injuries are the leading cause of death among children.1 The pediatric firearm injury case fatality rate has been increasing in California.2,3 Timely access to pediatric trauma care has been associated with lower mortality among injured children.4,5 Where an injured child should be cared for has been debated given the few and sparse distribution of American College of Surgeons (ACS) verified pediatric trauma centers.6–8 Trauma center characteristics best structured to provide pediatric trauma care have been poorly defined.9–11 The finding of pediatric trauma center designation’s association with lower mortality has been inconsistent.12–14
The heterogeneity in trauma center designation criteria may explain the conflicting results. ACS verification promotes rigor and uniformity in standards of care among participating trauma centers. ACS verification of adult trauma centers has been ongoing since 1980, and since 2006 for pediatric trauma centers. Many California Local Emergency Medical Services Agencies (LEMSAs) have required ACS verification for level I and II designation since before 2017. Most LEMSAs required ACS site visits as part of trauma center designation even if verification was not obtained. The 2017 California Statewide Trauma System Planning Recommendations of the California State Trauma Advisory Committee emphasized that LEMSAs should “explore ACS verification” of level I, II, and III trauma centers. These robust recommendations and considerable population make California the ideal state to study the association between ACS trauma center verification and firearm injury-associated mortality among children.
Large variation in trauma center injury volume has been another explanation for the inconsistency observed in pediatric trauma center designation’s association with lower mortality. Trauma center volume of complex injuries commonly requiring operative management, like firearm injuries, could mediate the association between ACS trauma center verification and mortality. Adult trauma center firearm injury volume has been associated with lower mortality in adult patients and among severely injured children compared to low-volume trauma centers.15,16 Yet, there is a literature gap of whether centers’ firearm injury volume mediates the relationship between ACS trauma centers’ verification level and mortality after firearm injury in children.
The objective of this study was to determine whether firearm injury volume mediates the relationship between ACS trauma center verification level and in-hospital mortality after firearm injury in children. The first aim was to determine whether ACS trauma center verification level was associated with in-hospital mortality after firearm injury in California between 2005 and 2018. The second aim was to determine whether firearm injury volume mediated the relationship between ACS trauma center verification level and in-hospital mortality. We hypothesized that ACS trauma center verification, regardless of trauma center volume, would be associated with lower firearm injury-associated mortality in children.
METHODS
Study design and data sources
This was a retrospective observational cohort study of children who presented to a California licensed acute care hospital after firearm injury from 2005 to 2018. The time period of 2005 to 2018 was chosen to capture all emergency department encounters because data collection from the emergency department started only in 2005. Data sources included the Office of Statewide Health Planning and Development (OSHPD) Patient Discharge Data (PDD), Emergency Department Data (ED), and the California Department of Health Care Access and Information Hospital Annual Utilization data. The PDD and ED included all inpatient and emergency department encounters of injured patients. The Hospital Annual Utilization data contained hospital licensing information, patient demographics, discharges and births, and information on services provided for all nonfederal hospitals licensed in California. Hospital characteristics were obtained from the Hospital Annual Utilization dataset for the years 2005 to 2018 to correspond with those available from the PDD and ED. Study was approved by the University Institutional Review Board study number STU00211123. This study followed Strengthening Reporting of Observational Studies in Epidemiology reporting guidelines.17
Study population
This study included children ages 0 to 14 years who presented to an acute care hospital between 2005 and 2018 after firearm injury. A pediatric patient was defined as 14 years or younger by the California Emergency Medical Services Authority.18 ICD-9 or −10 external cause of injury or morbidity codes for firearm injury were used to identify patients (Supplemental Digital Content 1, http://links.lww.com/JACS/A290). Duplicates were identified using hospital ID, date of birth, and date of encounter to create a unique identifier and subsequently removed. Patient encounters were excluded when transferred to another acute care hospital (ED) or transferred from acute care hospital (PDD). These exclusions were applied to limit bias from retriage on mortality.
Primary predictor of interest
The primary predictor of interest was acute care hospital ACS trauma center verification level. ACS trauma center verification levels were linked to all acute care hospital centers in the PDD and ED based on the California Emergency Medical Services Authority.19 Where possible, the dates of verification were confirmed using health system websites. Trauma centers’ verification levels were associated with encounters by date. The LEMSAs designations were largely concordant with the ACS verifications. The exceptions were 2 adult level II centers and 2 pediatric level II centers that were verified through the ACS, but not designated through the California LEMSAs. These centers were categorized by their ACS-verified level for this study.
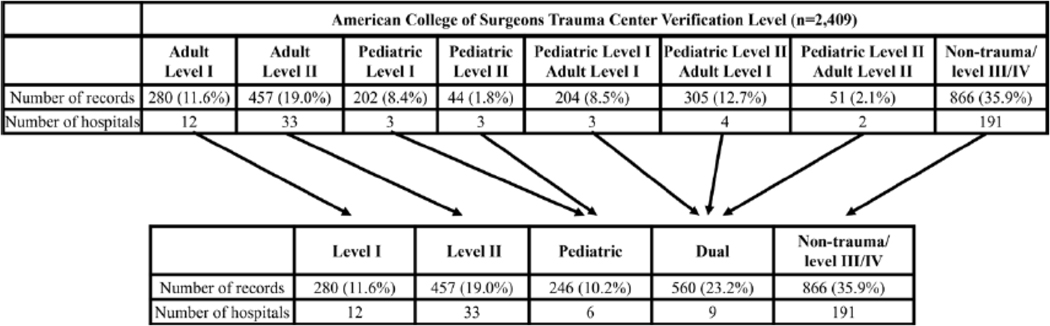
Trauma center verification levels were grouped together because of the low numbers of trauma centers with each of the potential ACS verification levels (Fig. 1). The after groups were created: adult level I, adult level II, pediatric level I and II, dual pediatric and adult level I/II and pediatric level I/II, and nontrauma/level III/IV. This was done a priori based on study team consensus and informed by knowledge of the California trauma system.18 Adult as well as pediatric trauma center level I verification requires the presence of surgical and nonsurgical specialists and a trauma research program/residency. In adult level I trauma centers, one of the after criteria must also be met: a minimum of 1,200 trauma program hospital admissions, a minimum of 240 trauma patients per year whose Injury Severity Score is greater than 15, an average of 35 trauma patients (with an Injury Severity Score greater than 15) per trauma program surgeon per year. Adult level I and adult level II centers were not combined due to the differences in volume and severity criteria. No volume and severity criteria distinguishing pediatric level I and II centers exist. Therefore, these levels were collapsed. ACS-verified non-trauma/level III/IV were used as the reference group given that the largest proportion of the cohort presented to these centers.
Figure 1.
Primary triage destination after firearm injury in California, 2005 to 2018, and groupings for study analysis. ED, Emergency Department Data; OSHPD, Office of Statewide Health Planning and Development; PDD, Patient Discharge Data.
Mediator of interest
Centers’ annual hospital adult and pediatric firearm injury volume (referred herein as annual total firearm injury volume) was considered as a mediator given that, after traumatic injury, children treated at high-volume adult trauma centers have been reported to have improved outcomes compared with low-volume trauma centers.15 Annual total firearm injury volume was defined by using the per hospital number of encounters included in the PDD and ED with an external cause of injury or morbidity code for firearm injury.
Covariable definitions
Patient age at the time of the encounter was categorized by OSHPD as less than 1 year, 1 to 4 years, 5 to 9 years, and 10 to 14 years. Given the low counts, less than 1 year and 1 to 4 years were combined as 0 to 4 years for analysis. Sex was categorized as male or female. Categories of normalized racial and ethnic groups were White, Black, Hispanic, Asian/Pacific Islander, Native American/Eskimo/Aleut, and Other. Asian/Pacific Islander and Native American/Eskimo/Aleut were included with Other due to low counts. The resulting categories for analysis were White non-Hispanic, Black non-Hispanic, Hispanic, and Other/unknown. Intent was determined using the R package icdpicr by using patient encounter ICD-9-CM or ICD-10-CM trauma codes.20 Categories of intent included self-inflicted, assault, unintentional, and undetermined. New Injury Severity Score (NISS) was also determined using icdpicr.20 The NISS was used given evidence that it best predicts mortality in penetrating trauma patients.20,21 NISS was treated as a continuous variable for analysis. However, NISS was dichotomized to create a binary variable to identify those that had severe injury, defined as a NISS greater than 15, for subgroup analysis.22 Abbreviated Injury Scale body regions head and neck, face, chest, abdomen, and extremities were also determined using icdpicr.20 A binary variable for each body region was created that indicated presence or absence of injury in that region. Hospital annual pediatric discharges of all ages less than 18 years was abstracted from the Hospital Annual Utilization dataset and included as a continuous measure of overall pediatric volume.
Outcomes of interest
The primary outcome was in-hospital mortality. This was considered an important outcome because mortality after penetrating injury has been documented as more common in children than in adults.23 Additionally, firearm injury has become the leading cause of mortality among children.1 A binary variable for in-hospital mortality was derived from the disposition variable in the PDD and ED.
Statistical analysis
Demographic and clinical characteristics were summarized by ACS trauma center verification level as defined earlier. Categorical data were described using counts and percentages. Continuous data were described using medians with interquartile ranges. Comparisons of demographic and clinical characteristics were performed using adjusted chi-square and t-tests that accounted for hospital-level clustering.24
Collinearity was evaluated before modeling for hospital variables because it is common for acute care hospitals that are high volume to seek ACS trauma center verification. We tested for collinearity between hospitals’ trauma center verification levels, annual total firearm injury volumes, and annual pediatric discharges. All hospital variables had variance inflation factors less than 2.5, meaning that variance of each variable remained <150% greater than what variance would be if there were no collinearity. A variance inflation factor of less than 2.5 is considered a conservative value.25,26
A mixed-effects multivariable logistic regression model was fit to evaluate the association between in-hospital mortality and ACS trauma center verification level after adjusting for age, sex, race and ethnicity, intent, NISS, body region, and annual pediatric discharges. Random intercepts were estimated and fit for each hospital. The mixed-effects multivariable logistic regression was rerun after introducing annual total firearm injury volume to test for mediation of the association between ACS trauma center verification level and in-hospital mortality.
A subgroup analysis was performed to evaluate the association between in-hospital mortality and ACS trauma center verification level in patients who were severely injured with NISS greater than 15. This group was selected a priori for a subgroup analysis because evidence indicates that pediatric patients with severe injury, in particular, have improved outcomes based on the ACS trauma center verification level.9,11,27,28 The same univariate and multivariable analyses were conducted with the same covariates as the full cohort described earlier.
A second subgroup analysis was performed to evaluate the association between mortality and ACS trauma center verification level in the youngest children (age less than 5 years). This analysis was also planned a priori because younger children have been shown to be the most likely to experience lower mortality when treated at a pediatric trauma center.11 The same univariate and multivariable analyses were conducted with the same covariates as the full cohort excluding age.
Only complete encounters with all predictor, mediator, covariates, and outcome were used for analysis. The most frequently missing encounter information was valid OSHPD identification number (n = 14, 0.58%), sex (n = 8, 0.33%), and ICD 9/10 codes (n = 4, 0.16%). We excluded 25 records with missing encounter information. A p value of <0.05 was used to define statistical significance. All tests were 2-sided. Statistical analyses were done using Stata v17.0 (StataCorp LLC, College Station, TX).
RESULTS
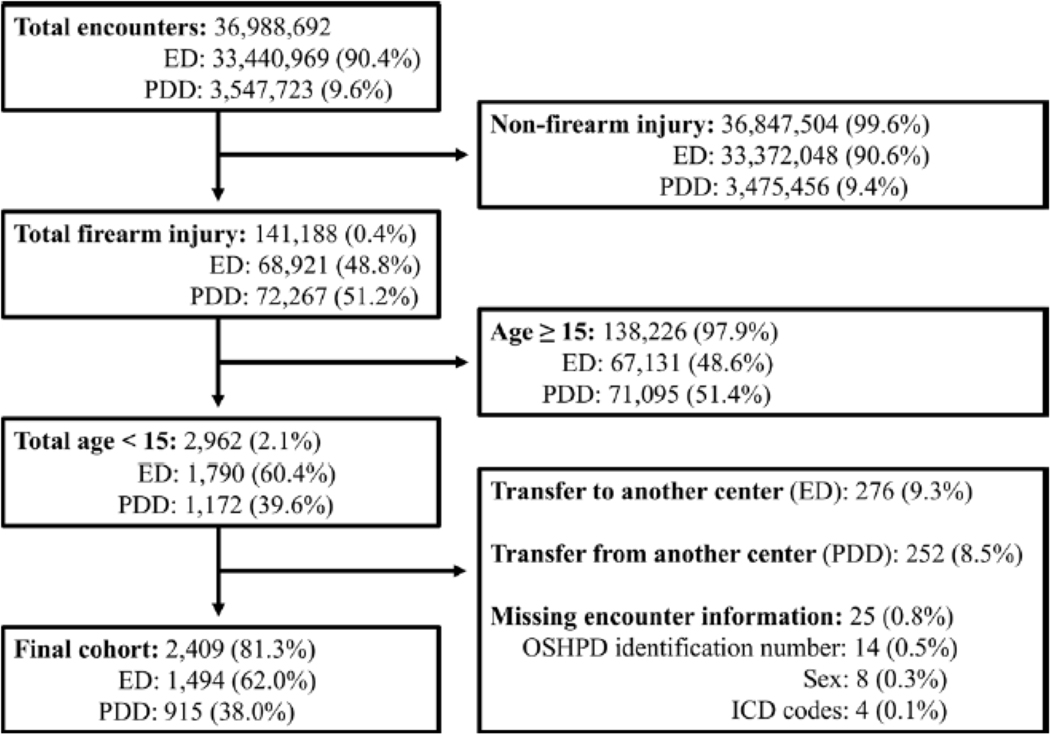
Encounters of 2,409 children aged 0 to 14 years who presented to an acute care hospital after firearm injury in California between 2005 and 2018 were included (Fig. 2). Of these, 1,494 (62.0%) were evaluated only in the emergency department, and 915 (38.0%) were admitted as inpatients.
Figure 2.
Final study cohort of children less than 15 years of age who presented to California trauma center after firearm injury between 2005 and 2018. Total encounters included all injured patients in the California Office of Statewide Health Planning and Development patient discharge data (PDD) and emergency department data (ED) datasets. Percentages for totals are derived using the previous group total as the denominator. ED and PDD percentages were derived using the total in that group as the denominator.
The pediatric firearm injury encounters were primarily of children ages 10 to 14 (n = 1,805, 74.9%; Table 1). Most injuries were due to assault (n = 1,299, 53.9%) with a median NISS of 2 (interquartile range 1 to 9). The most common body region was extremity injury (n = 812, 33.7%). The largest proportion of pediatric firearm injury encounters presented to a nontrauma/level III/IV center (n = 866, 35.9%). Of pediatric firearm injury encounters that presented to an ACS-verified level I or II trauma center, the highest proportion was taken to a dual adult and pediatric trauma center (n = 560, 23.2%). The lowest proportion of pediatric firearm injury encounters presented to ACS-verified pediatric trauma centers (n = 246, 10.2%). The median center annual total firearm injury volume was 94 (interquartile range 22 to 303). Center annual total firearm injury volumes were highest at ACS-verified dual trauma centers (median 305, interquartile range 160 to 436).
Table 1.
Demographic and Clinical Characteristics of Children and the Centers They Presented to by American College of Surgeons Trauma Center Verification Level after Firearm Injury in California, 2005–2018
| Variable | Total N = 2,409 | Adult level I n = 280 | Adult level II n = 457 | Pediatric n = 246 | Dual n = 560 | Nontrauma/level III/IV n = 866 |
|---|---|---|---|---|---|---|
| Annual total firearm injury, median (IQR) | 94 (22–303) | 265 (128–356) | 169 (72–449) | 22 (9–26) | 305 (160–436) | 22 (8–72) |
| Annual pediatric firearm injury, median (IQR) | 5 (2–11) | 7 (5–10) | 3 (2–8) | 13 (6–16) | 12 (7–17) | 2 (1–3) |
| Age, n (%) | ||||||
| 0–4 y | 253 (10.5) | 29 (11.6) | 58 (22.9) | 36 (14.2) | 61 (24.1) | 69 (27.3) |
| 5–9y | 351 (14.6) | 35 (10.0) | 41 (11.7) | 54 (15.4) | 87 (25.0) | 134 (38.2) |
| 10–14 y | 1,805 (74.9) | 216 (12.0) | 358 (19.8) | 156 (8.6) | 412 (22.8) | 663 (36.7) |
| Sex, n (%) | ||||||
| Male | 1,817 (75.4) | 213 (11.7) | 379 (20.9) | 159 (8.8) | 498 (21.9) | 668 (36.8) |
| Female | 592 (24.6) | 67 (11.3) | 78 (13.2) | 87 (14.7) | 162 (27.4) | 198 (33.5) |
| Race and ethnicity, n (%) | ||||||
| White non-Hispanic | 324 (13.5) | 41 (12.7) | 57 (17.6) | 10 (3.1) | 47 (14.5) | 169 (52.2) |
| Black non-Hispanic | 615 (25.5) | 74 (12.0) | 117 (19.0) | 91 (14.8) | 165 (26.8) | 168 (27.3) |
| Hispanic | 1,183 (49.1) | 124 (10.5) | 248 (20.1) | 116 (9.8) | 275 (23.3) | 420 (35.5) |
| Other/unknown | 287 (11.9) | 41 (14.3) | 35 (12.2) | 29 (10.1) | 73 (25.4) | 109 (38.0) |
| Intent, n (%) | ||||||
| Self-inflicted | 29 (1.2) | 3 (10.3) | 16 (55.2) | 0 | 1 (3.5) | 9 (31.0) |
| Assault | 1,299 (53.9) | 190 (14.6) | 288 (22.2) | 134 (10.3) | 354 (27.3) | 333 (25.6) |
| Unintentional | 930 (38.6) | 80 (8.6) | 122 (13.1) | 100 (10.8) | 170 (18.3) | 458 (49.3) |
| Undetermined | 151 (6.3) | 7 (4.6) | 31 (20.5) | 12 (8.0) | 35 (23.2) | 66 (43.7) |
| NISS, median (IQR) | 2 (1–9) | 3 (1–11) | 3 (1–10) | 1 (1–9) | 4 (1–10) | 1 (1–4) |
| <16, n (%) | 2,045 (84.9) | 221 (10.8) | 366 (17.9) | 202 (9.9) | 449 (22.0) | 807 (39.5) |
| ≥16, n (%) | 364 (15.1) | 59 (16.2) | 91 (25.0) | 44 (12.1) | 111 (30.5) | 59 (16.2) |
| AIS body region,* n (%) | ||||||
| Head and neck | 238 (9.9) | 33 (13.9) | 56 (23.5) | 26 (10.9) | 60 (25.2) | 63 (26.5) |
| Face | 84 (3.5) | 7 (8.3) | 15 (17.9) | 11 (13.1) | 28 (33.3) | 23 (27.4) |
| Chest | 349 (14.5) | 38 (10.9) | 99 (28.4) | 41 (11.8) | 103 (29.5) | 68 (19.5) |
| Abdomen | 306 (12.7) | 51 (16.7) | 78 (25.5) | 40 (30.1) | 99 (32.4) | 38 (12.4) |
| Extremity | 812 (33.7) | 97 (12.0) | 177 (21.8) | 71 (8.7) | 197 (24.3) | 270 (33.3) |
| Annual pediatric discharges, median (IQR) | 963 (156–2461) | 917 (449–1775) | 883 (232–1043) | 9115 (8286–9718) | 2474 (1735–3183) | 311 (0–795) |
Percentages calculated by column for total and by rows for each verification/level.
AIS body regions are not mutually exclusive. The remaining injuries were external.
AIS, Abbreviated Injury Score; IQR, interquartile range; NISS, New Injury Severity Score.
In-hospital mortality after firearm injury was 8.6% (n = 206; Table 2). The highest rates of in-hospital mortality were in ACS-verified adult level II trauma centers (n = 80, 17.5%). The lowest rates of in-hospital mortality were at ACS-verified pediatric trauma centers (n = 12, 4.9%).
Table 2.
Demographics and Clinical Characteristics of Children after Firearm Injury in California, 2005–2018, and In-Hospital Mortality
| Variable | Mortality n = 206 | Survival n = 2,203 | p Value |
|---|---|---|---|
| ACS verification level, n (%) | <0.001 | ||
| Non-trauma/level III/IV | 60 (6.9) | 806 (93.1) | |
| Adult level I | 18 (6.4) | 262 (93.6) | |
| Adult level II | 80 (17.5) | 377 (82.5) | |
| Pediatric | 12 (4.9) | 234 (95.1) | |
| Dual | 36 (6.4) | 524 (93.6) | |
| Annual total firearm injury, median (IQR) | 106 (38–306) | 94 (22–303) | 0.87 |
| Annual pediatric firearm injury, median (IQR) | 3.5 (2–10) | 5 (2–11) | 0.83 |
| Age, n (%) | <0.001 | ||
| 0–4 y | 52 (20.6) | 201 (79.4) | |
| 5–9 y | 31 (8.8) | 320 (91.2) | |
| 10–14 y | 123 (6.8) | 1,682 (93.2) | |
| Sex, n (%) | 0.43 | ||
| Male | 160 (8.8) | 1,657 (91.2) | |
| Female | 46 (7.8) | 566 (92.2) | |
| Race and ethnicity, n (%) | 0.28 | ||
| White non-Hispanic | 25 (7.7) | 299 (92.3) | |
| Black non-Hispanic | 49 (8.0) | 566 (92.0) | |
| Hispanic | 99 (8.4) | 1,084 (91.6) | |
| Other/unknown | 33 (11.5) | 254 (88.5) | |
| Intent, n (%) | <0.001 | ||
| Self-inflicted | 16 (55.2) | 13 (44.8) | |
| Assault | 126 (9.7) | 1,173 (90.3) | |
| Unintentional | 51 (5.5) | 879 (94.5) | |
| Undetermined | 13 (8.6) | 138 (91.4) | |
| NISS, median (IQR) | 11 (3–25) | 1 (1–6) | <0.001 |
| < 16, n (%) | 107 (5.2) | 1,938 (94.8) | <0.001 |
| ≥ 16, n (%) | 99 (27.2) | 265 (72.8) | |
| AIS body region* | |||
| Head and neck | 66 (27.7) | 172 (72.3) | <0.001 |
| Face | 5 (6.0) | 79 (94.1) | 0.39 |
| Chest | 89 (25.5) | 260 (74.5) | <0.001 |
| Abdomen | 28 (9.2) | 278 (90.9) | 0.69 |
| Extremity | 14 (1.7) | 798 (98.3) | <0.001 |
| Annual pediatric discharges, median (IQR) | 937 (246–1792) | 963 (151–2461) | 0.78 |
Percentages calculated by column for total and by row for outcomes. Analysis included Chi-square and t-test accounting for hospital level clustering.
AIS body regions are not mutually exclusive. The remaining injuries were external.
ACS, American College of Surgeons; AIS, Abbreviated Injury Score; IQR, interquartile range; NISS, New Injury Severity Score.
Mixed-effects multivariable logistic regression modeling odds of in-hospital mortality showed that children had 62% lower adjusted odds of mortality (95% CI 0.19 to 0.80) at ACS-verified adult level I, 83% lower (95% CI 0.05 to 0.61) at ACS-verified pediatric, and 52% lower (95% CI 0.25 to 0.93) at ACS-verified dual trauma centers compared to children presenting to nontrauma/level III/IV centers (Table 3). After adding annual total firearm injury volume to the mixed-effects multivariable logistic regression, the adjusted odds of mortality remained approximately the same at ACS-verified adult level I, pediatric, and dual trauma centers compared to children presenting to nontrauma/level III/IV centers. There was no association of annual total firearm injury volume with in-hospital mortality (adjusted odds ratio/10 patient increase in volume 1.00, 95% CI 0.99 to 1.02).
Table 3.
Demographic, Clinical, and Hospital Level Variables Associated with In-Hospital Mortality in Children 0–14 Years Old after Firearm Injury in California, 2005–2018
| Without volume mediator |
With volume mediator |
|||
|---|---|---|---|---|
| Variable | aOR (95% CI) | p Value | aOR (95% CI) | p Value |
|
| ||||
| ACS verification level | ||||
|
| ||||
| Nontrauma/level III/IV | Ref | Ref | ||
|
| ||||
| Adult level I | 0.38 (0.19–0.80) | 0.01 | 0.40 (0.18–0.86) | 0.02 |
|
| ||||
| Adult level II | 1.44 (0.88–2.37) | 0.15 | 1.47 (0.85–2.52) | 0.17 |
|
| ||||
| Pediatric | 0.17 (0.05–0.61) | <0.01 | 0.17 (0.05–0.61) | <0.01 |
|
| ||||
| Dual | 0.48 (0.25–0.93) | 0.03 | 0.50 (0.24–1.04) | 0.06 |
|
| ||||
| Annual total firearm injury* | — | — | 1.00 (0.98–1.01) | 0.86 |
|
| ||||
| Age | ||||
|
| ||||
| 0–4 y | 3.54 (2.25–5.58) | <0.001 | 3.53 (2.23–5.57) | <0.001 |
|
| ||||
| 5–9 y | 2.05 (1.25–3.39) | <0.01 | 2.06 (1.25–3.39) | <0.01 |
|
| ||||
| 10–14 y | Ref | Ref | ||
|
| ||||
| Sex | ||||
|
| ||||
| Male | Ref | Ref | ||
|
| ||||
| Female | 0.85 (0.56–1.29) | 0.44 | 0.85 (0.56–1.29) | 0.45 |
|
| ||||
| Race and ethnicity | ||||
|
| ||||
| White non-Hispanic | Ref | Ref | ||
|
| ||||
| Black non-Hispanic | 1.57 (0.82–3.03) | 0.18 | 1.60 (0.82–3.10) | 0.17 |
|
| ||||
| Hispanic | 1.92 (1.06–3.48) | 0.03 | 1.93 (1.07–3.50) | 0.03 |
|
| ||||
| Other/unknown | 3.34 (1.65–6.78) | <0.01 | 3.36 (1.65–6.84) | <0.01 |
|
| ||||
| Intent | ||||
|
| ||||
| Self-inflicted | Ref | Ref | ||
|
| ||||
| Assault | 0.19 (0.07–0.52) | <0.01 | 0.19 (0.07–0.53) | <0.01 |
|
| ||||
| Unintentional | 0.12 (0.04–0.35) | <0.001 | 0.12 (0.04–0.35) | <0.001 |
|
| ||||
| Undetermined | 0.16 (0.05–0.54) | <0.01 | 0.16 (0.05–0.54) | <0.01 |
|
| ||||
| NISS | 1.07 (1.05–1.09) | <0.001 | 1.07 (1.05–1.09) | <0.001 |
|
| ||||
| AIS body region† | ||||
|
| ||||
| Head and neck | 3.25 (1.92–5.48) | <0.001 | 3.24 (1.92–5.48) | <0.001 |
|
| ||||
| Face | 0.13 (0.04–0.41) | <0.001 | 0.13 (0.04–0.41) | <0.001 |
|
| ||||
| Chest | 4.82 (3.20–7.26) | <0.001 | 4.82 (3.20–7.26) | <0.001 |
|
| ||||
| Abdomen | 0.38 (0.21–0.67) | <0.01 | 0.38 (0.21–0.68) | <0.01 |
|
| ||||
| Extremity | 0.12 (0.06–0.23) | <0.01 | 0.12 (0.06–0.23) | <0.001 |
|
| ||||
| Annual pediatric discharges* | 1.00 (0.99–1.02) | 0.47 | 1.00 (0.99–1.02) | 0.47 |
Analysis included mixed-effects logistic regression with random intercept estimates fit for each hospital.
Per 10 (injury) and per 100 (discharges) annual increases in volume.
AIS body regions were treated as binary variables and not mutually exclusive, thus the reference category for each was absence of injury in that body region.
aOR, adjusted odds ratio; ACS, American College of Surgeons; NISS, New Injury Severity Score; Ref, reference.
A subgroup analysis of 364 (15.1%) severely injured children with an NISS of greater than 15 was conducted (Table 4). Overall mortality was 27.2% (n = 99). In univariate analysis, mortality was highest in patients who presented to nontrauma/level III/IV center (n = 27, 45.8%). Severely injured children less than 5 years of age had higher mortality (n = 25, 46.3%) compared to children ages 5 to 9 (n = 6, 20.7%) and children ages 10 to 14 (n = 68, 24.2%). Mortality was highest among those with self-inflicted injury (n = 12, 70.6%).
Table 4.
In-hospital Mortality of Children 0–14 Years Old after Firearm Injury in California, 2005–2018, with New Injury Severity Score Greater Than 15 Stratified into New Injury Severity Score 16–24 and New Injury Severity Score >24
| Variable | Total | Adult level I | Adult level II | Pediatric | Dual | Nontrauma/level III/IV |
|---|---|---|---|---|---|---|
| Total | 364 | 59 (16.2) | 91 (25.0) | 44 (12.1) | 111 (30.5) | 59 (16.2) |
| Mortality | 99 (27.2) | 11 (18.6) | 40 (44.0) | 6 (13.6) | 15 (13.5) | 27 (45.8) |
| NISS 16–24 | 161 (44.2) | 33 (20.5) | 29 (18.0) | 16 (9.9) | 58 (36.0) | 15 (9.3) |
| Mortality | 25 (15.5) | 4 (12.1) | 10 (34.5) | 0 (0) | 5 (8.6) | 6 (40.0) |
| NISS >24 | 203 (55.8) | 26 (12.8) | 62 (30.5) | 28 (13.8) | 53 (26.1) | 34 (16.7) |
| Mortality | 74 (36.5) | 7 (26.9) | 30 (48.4) | 6 (21.4) | 10 (18.9) | 21 (61.8) |
Data presented as n (%). Percentages were calculated by row for totals, and by column for mortality.
NISS, New Injury Severity Score.
Mixed-effects multivariable logistic regression predicting odds of mortality showed that severely injured children had an 84% lower adjusted odds of mortality (95% CI 0.06 to 0.46) at ACS-verified adult level I; 93% lower (95% CI 0.01 to 0.38) at ACS-verified pediatric; and 86% lower (95% CI 0.05 to 0.36) at ACS-verified dual trauma centers compared to children presenting to a nontrauma/level III/IV center (Table 5). When included in the model, annual total firearm injury volume did not function as a mediator and was not itself associated with mortality (adjusted odds ratio/10 patient increase in volume 1.00, 95% CI 0.97 to 1.01).
Table 5.
Demographic, Clinical, and Hospital Level Factors Associated with In-Hospital Mortality in Children 0–14 Years Old after Firearm Injury in California, 2005–2018, with New Injury Severity Score Greater Than 15
| Without volume mediator | With volume mediator | |||
|---|---|---|---|---|
|
|
||||
| Variable | aOR (95% CI) | p Value | aOR (95% CI) | p Value |
|
| ||||
| ACS verification level | ||||
|
| ||||
| Nontrauma/level III/IV | Ref | Ref | ||
|
| ||||
| Adult level I | 0.16 (0.06–0.46) | <0.01 | 0.19 (0.06–0.57) | <0.01 |
|
| ||||
| Adult level II | 0.63 (0.28–1.43) | 0.27 | 0.69 (0.29–1.65) | 0.40 |
|
| ||||
| Pediatric | 0.07 (0.01–0.38) | <0.01 | 0.07 (0.01–0.38) | <0.01 |
|
| ||||
| Dual | 0.14 (0.05–0.36) | <0.001 | 0.16 (0.05–0.47) | <0.01 |
|
| ||||
| Center annual total firearm injury* | — | — | 1.00 (0.97–1.01) | 0.51 |
|
| ||||
| Age | ||||
|
| ||||
| 0–4 y | 2.50 (1.14–5.45) | 0.02 | 2.42 (1.10–5.32) | 0.03 |
|
| ||||
| 5–9 y | 1.19 (0.37–3.82) | 0.77 | 1.17 (0.37–3.77) | 0.79 |
|
| ||||
| 10–14 y | Ref | Ref | ||
|
| ||||
| Sex | ||||
|
| ||||
| Male | Ref | Ref | ||
|
| ||||
| Female | 0.64 (0.30–1.35) | 0.24 | 0.65 (0.31–1.37) | 0.26 |
|
| ||||
| Race and ethnicity | ||||
|
| ||||
| White non-Hispanic | Ref | Ref | ||
|
| ||||
| Black non-Hispanic | 1.27 (0.44–3.64) | 0.66 | 1.37 (0.46–4.06) | 0.57 |
|
| ||||
| Hispanic | 2.02 (0.74–5.54) | 0.17 | 2.12 (0.76–5.87) | 0.15 |
|
| ||||
| Other/unknown | 2.72 (0.68–10.81) | 0.16 | 2.84 (0.71–11.33) | 0.14 |
|
| ||||
| Intent | ||||
|
| ||||
| Self-inflicted | Ref | Ref | ||
|
| ||||
| Assault | 0.30 (0.07–1.38) | 0.12 | 0.31 (0.07–1.41) | 0.13 |
|
| ||||
| Unintentional | 0.27 (0.06–1.26) | 0.10 | 0.26 (0.06–1.23) | 0.09 |
|
| ||||
| Undetermined | 0.34 (0.05–2.31) | 0.27 | 0.33 (0.05–2.31) | 0.27 |
|
| ||||
| NISS | 1.04 (1.01–1.07) | <0.01 | 1.04 (1.01–1.07) | <0.01 |
|
| ||||
| AIS body region† | ||||
|
| ||||
| Head and neck | 2.47 (1.10–5.54) | 0.03 | 2.43 (1.09–5.45) | 0.03 |
|
| ||||
| Face | 0.07 (0.02–0.28) | <0.001 | 0.07 (0.02–0.28) | <0.001 |
|
| ||||
| Chest | 0.78 (0.39–1.57) | 0.49 | 0.78 (0.39–1.57) | 0.49 |
|
| ||||
| Abdomen | 0.33 (0.15–0.70) | <0.01 | 0.32 (0.15–0.69) | <0.01 |
|
| ||||
| Extremities | 0.23 (0.10–0.54) | <0.01 | 0.23 (0.10–0.55) | <0.01 |
|
| ||||
| Annual pediatric discharges* | 1.01 (0.99–1.03) | 0.54 | 1.01 (0.99–1.02) | 0.57 |
Analysis included mixed-effects logistic regression with random intercept estimates fit for each hospital.
Per 10 (injury) and per 100 (discharges) annual increases in volume.
AIS body regions were treated as binary variables and not mutually exclusive, thus the reference category for each was absence of injury in that body region.
ACS, American College of Surgeons; aOR, adjusted odds ratio; NISS, New Injury Severity Score; Ref, reference.
A second subgroup analysis was performed among 253 children less than 5 years of age (10.5%). In-hospital mortality was 20.6% (n = 52; Supplemental Digital Content 2, http://links.lww.com/JACS/A290). In univariate analysis, patients who presented to ACS-verified adult level II centers had the highest mortality (n = 20, 34.5%). Mixed-effects logistic regression modeling demonstrated no association between in-hospital mortality and ACS trauma center verification level or center annual firearm injury volume (Supplemental Digital Content 3, http://links.lww.com/JACS/A290).
DISCUSSION
Where to take a child after firearm injury can present a challenge given the availability of few and sparsely distributed pediatric trauma centers. The California OSHPD PDD and ED data included encounters of all individuals who presented to an acute care hospital after firearm injury. This study explored whether center firearm injury volume impacted the relationship between ACS trauma center verification level and in-hospital mortality after firearm injury in children. We found that presentation to an ACS-verified adult level I, pediatric, or dual trauma center was associated with lower adjusted odds of mortality compared to nontrauma/level III/IV centers. Annual total firearm injury volume was not associated with adjusted odds of mortality after firearm injury, nor did it act as a mediator for the association between ACS trauma center verification level and in-hospital mortality. These findings suggest that ACS verification ensured that centers could achieve optimal care of firearm-injured children regardless of volume.
California has the largest population in the country and is home to 12% of the nation’s children.29 The state size and the combination of both metropolitan and rural areas creates a unique microcosm to study firearm injury in a pediatric population. There are 81 local designated and 66 ACS-verified trauma centers, including 17 pediatric trauma centers.30 There are 33 LEMSAs, all of which have different protocols for the triage of injured children.30 In a previous study using OSHPD data, treatment at local designated trauma centers was associated with decreased mortality among severely injured children ages 0 to 18 years.31 Previous studies have demonstrated similarly high rates of presentation of injured children to nontrauma/level III/IV centers as found in this study.32–34 Within Northern California, initial transport to a nontrauma/level III/IV center within close proximity to a local designated trauma center was recognized as a challenge that led to delays in definitive pediatric trauma care.29 These findings raise the question of whether relative higher likelihood of mortality for those severely injured children who presented to a non-trauma/level III/IV may have been attributable to trauma system factors.
Although care at an ACS-verified adult level I, pediatric, or dual trauma center was found to be associated with lower likelihood of firearm injury-associated mortality among children, ACS-verified adult level II centers had the highest rates of mortality. In California, many of the adult level II as well as nontrauma/level III/IV centers are located in less densely populated rural areas, but adult level I, pediatric, and dual trauma centers are in more densely populated urban areas.30,34 The higher mortality rates at ACS-verified adult level II centers could potentially be attributed to differences in prehospital time. As patients who were retriaged or transferred were excluded, the survivors who were initially stabilized at these centers then subsequently transferred may have resulted in inflated mortality rates.
Center annual total firearm injury volume was not associated with or a mediator for the association between ACS trauma center verification level and in-hospital mortality. These findings suggest that other elements specific to ACS-verified trauma centers such as the presence of specialists and trainees may have contributed to decreased mortality. Additionally, previous experience of staff in working with pediatric patients cannot be directly measured but may contribute. These findings have important implications that ACS trauma center verification processes are rigorous enough regardless of centers’ firearm injury volume, thus reinforcing the value of 6 decades of robust trauma system development in California and across the US.
This study has limitations. First, our cohort only included children who presented to a California acute care hospital after firearm injury and excluded retriaged as well as interfacility transferred children. This was done because delays in retriage have been well documented to increase mortality and would have confounded our results.35 Because our question was where should pediatric firearm patients be taken, we focused only on patients who were cared for at the same hospital to which they were taken. Second, children who died before hospital arrival were not captured in these data. A previous California-based study on mortality in adults after firearm injury estimated that the OSHPD dataset captured only 25.2% of mortality compared to the data from the CDC Fatal Injury Reports with the remainder never reaching an acute care hospital emergency department.2 Similarly, another California-based study showed that the fatality rate in pediatric patients after firearm injury nearly doubled when using statewide data accounting for deaths in the field.3 As a result, our results were undoubtedly an underestimate of the burden and volume of pediatric firearm injuries. However, because only 30% of deaths in the field have been shown to be preventable, it is unclear if capture would have biased our results.36 Third, this study used data from a single state. The generalizability of our findings may be limited given the variation in states’ trauma systems. Nonetheless, we used ACS verification level as the primary predictor to ensure homogeneity in primary predictor definition. California is the most populous state and extremely diverse with a decentralized trauma system spanning dense urban to extremely rural areas; therefore, it serves as a microcosm for the US. Fourth, this study used administrative data that have limited clinical information. We used established methods to control injury severity and heterogeneity to address this limitation. We believe that complete capture of all firearm-injured children presenting to any hospital during 14 years in the most populous state provides a unique birds-eye view of how ACS verification level, center firearm injury volume, and in-hospital mortality are related. Last and most importantly, there is almost certainly some residual selection bias in where patients were transported introduced by Emergency Medical Services that cannot be completely accounted for.37 A future direction is an instrumental variable analysis quantifying association of distance between injury and closest ACS-verified adult, dual or pediatric trauma center with in-hospital mortality.
CONCLUSIONS
Presentation to an ACS-verified adult level I, pediatric, or dual trauma center was associated with lower adjusted odds of mortality after pediatric firearm injury. ACS trauma center verification level, regardless of trauma center volume, was associated with lower in-hospital mortality among firearm-injured children in California. These findings suggest that the ACS verification process contributing to the achievement of optimal outcomes for children after injury.
Supplementary Material
Support:
Dr Reddy receives salary support from the NIH. Dr Visenio is supported by the NIH. Dr Stey is supported by the American Association for the Surgery of Trauma, The American College of Surgeons and the NIH/National Heart Lung and Blood Institute (K23HL157832-01).
Disclosures outside the scope of this work:
Dr Reiter received a one-time honorarium from Intuitive Surgical in March 2022.
Abbreviations and Acronyms
- ACS
American College of Surgeons
- ED
Emergency Department Data
- LEMSAs
Local Emergency Medical Services Agencies
- NISS
New Injury Severity Score
- OSHPD
Office of Statewide Health Planning and Development
- PDD
Patient Discharge Data
Footnotes
Disclosure Information: Nothing to disclose.
Contributor Information
Gwyneth A Sullivan, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL; Division of Pediatric Surgery, Department of Surgery, Rush University Medical Center, Chicago, IL.
Susheel Reddy, Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL.
Audra J Reiter, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL.
Suhail Zeineddin, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL.
Michael Visenio, Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL.
Andrew Hu, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL.
Robert Mackersie, Department of Surgery, University of California San Francisco, San Francisco, CA.
Rashmi Kabre, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL.
Mehul V Raval, Division of Pediatric Surgery, Department of Surgery, Northwestern University Feinberg School of Medicine, Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL.
Anne M Stey, Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL.
REFERENCES
- 1.Goldstick JE, Cunningham RM, Carter PM. Current causes of death in children and adolescents in the United States. N Engl J Med 2022;386:1955–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spitzer SA, Pear VA, McCort CD, Wintemute GJ. Incidence, distribution, and lethality of firearm injuries in California from 2005 to 2015. JAMA Netw Open 2020;3:e2014736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theodorou CM, Beyer CA, Vanover MA, et al. The hidden mortality of pediatric firearm violence. J Pediatr Surg 2022;57:897–902. [DOI] [PubMed] [Google Scholar]
- 4.Byrne JP, Nance ML, Scantling DR, et al. Association between access to pediatric trauma care and motor vehicle crash death in children: an ecologic analysis of United States counties. J Trauma Acute Care Surg 2021;91:84–92. [DOI] [PubMed] [Google Scholar]
- 5.Friedman J, Hoof M, Smith A, et al. Pediatric firearm incidents: it is time to decrease on-scene mortality. J Trauma Acute Care Surg 2019;86:791–796. [DOI] [PubMed] [Google Scholar]
- 6.Carr BG, Nance ML. Access to pediatric trauma care: alignment of providers and health systems. Curr Opin Pediatr 2010;22:326–331. [DOI] [PubMed] [Google Scholar]
- 7.Ertl AM, Beyer KMM, Tarima S, et al. The spatial epidemiology of pediatric trauma: a statewide assessment. J Trauma Acute Care Surg 2017;83:225–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nance ML, Carr BG, Branas CC. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med 2009;163:512–518. [DOI] [PubMed] [Google Scholar]
- 9.Potoka DA, Schall LC, Gardner MJ, et al. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma 2000;49:237–245. [DOI] [PubMed] [Google Scholar]
- 10.Osler TM, Vane DW, Tepas JJ, et al. Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J Trauma 2001;50:96–101. [DOI] [PubMed] [Google Scholar]
- 11.Sathya C, Alali AS, Wales PW, et al. Mortality among injured children treated at different trauma center types. JAMA Surg 2015;150:874–881. [DOI] [PubMed] [Google Scholar]
- 12.Hatchimonji JS, Swendiman RA, Goldshore MA, et al. Pediatric firearm mortality in the United States, 2010 to 2016: A National Trauma Data Bank analysis. J Trauma Acute Care Surg 2020;88:402–407. [DOI] [PubMed] [Google Scholar]
- 13.Swendiman RA, Luks VL, Hatchimonji JS, et al. Mortality after adolescent firearm injury: effect of trauma center designation. J Adolesc Health 2021;68:978–984. [DOI] [PubMed] [Google Scholar]
- 14.Miyata S, Cho J, Lebedevskiy O, et al. Trauma experts versus pediatric experts: comparison of outcomes in pediatric penetrating injuries. J Surg Res 2017;208:173–179. [DOI] [PubMed] [Google Scholar]
- 15.Miyata S, Cho J, Park H, et al. Comparison of outcomes in severe pediatric trauma at adult trauma centers with different trauma case volumes. J Pediatr Surg 2017;52:1831–1835. [DOI] [PubMed] [Google Scholar]
- 16.Fu CY, Bajani F, Tatebe L, et al. Right hospital, right patients: penetrating injury patients treated at high-volume penetrating trauma centers have lower mortality. J Trauma Acute Care Surg 2019;86:961–966. [DOI] [PubMed] [Google Scholar]
- 17.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–1457. [DOI] [PubMed] [Google Scholar]
- 18.California Office of Administrative Law. Chapter 7. Trauma Care Systems. Article 3 Trauma Center Requirements. Available at: https://emsa.ca.gov/wp-content/uploads/sites/71/2017/10/Regulations-Chapter-7.pdf. Accessed March 29, 2022. [Google Scholar]
- 19.California Emergency Medical Services Authority. Trauma. Available at: https://emsa.ca.gov/trauma/. Accessed March 29, 2022. [Google Scholar]
- 20.Black A, Clark D. icdpicr: “ICD” programs for injury categorization in R. 2021. Available at: https://CRAN.R-project.org/package=icdpicr. Accessed March 29, 2022. [Google Scholar]
- 21.Chun M, Zhang Y, Becnel C, et al. New injury severity score and trauma injury severity score are superior in predicting trauma mortality. J Trauma Acute Care Surg 2022;92:528–534. [DOI] [PubMed] [Google Scholar]
- 22.Copes WS, Champion HR, Sacco WJ, et al. The injury severity score revisited. J Trauma 1988;28:69–77. [DOI] [PubMed] [Google Scholar]
- 23.McLaughlin C, Zagory JA, Fenlon M, et al. Timing of mortality in pediatric trauma patients: a National Trauma Data Bank analysis. J Pediatr Surg 2018;53:344–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herrin J CLTEST: Stata modules for performing cluster-adjusted chi-square and t-tests (Statistical Software Component S424901). Boston, MA: Boston College, Department of Economics; 2002. [Google Scholar]
- 25.Johnston R, Jones K, Manley D. Confounding and collinearity in regression analysis: a cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual Quant 2018;52:1957–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology 2016;6:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans J, Murch H, Begley R, et al. Mortality in adolescent trauma: a comparison of children’s, mixed and adult major trauma centres. Emerg Med J 2021;38:488–494. [DOI] [PubMed] [Google Scholar]
- 28.Mitchell RJ, Curtis K, Testa L et al. Differences in survival outcome for severely injured paediatric trauma by type of trauma centre. J Paediatr Child Health 2017;53:808–813. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau. Child population data. 2020.
- 30.California Emergency Medical Services Authority. California trauma system. Available at: https://emsa.ca.gov/trauma/. Accessed July 21, 2022.
- 31.Wang NE, Saynina O, Vogel LD, et al. The effect of trauma center care on pediatric injury mortality in California, 1999 to 2011. J Trauma Acute Care Surg 2013;75:704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Acosta CD, Kit Delgado M, Gisondi MA, et al. Characteristics of pediatric trauma transfers to a level I trauma center: implications for developing a regionalized pediatric trauma system in California. Acad Emerg Med 2010;17:1364–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogel LD, Vongsachang H, Pirrotta E, et al. Variations in pediatric trauma transfer patterns in Northern California pediatric trauma centers (2001–2009). Acad Emerg Med 2014;21:1023–1030. [DOI] [PubMed] [Google Scholar]
- 34.Wang NE, Ewbank C, Newton CR, et al. Regionalization patterns for children with serious trauma in California (2005–2015): a retrospective cohort study. Prehosp Emerg Care 2021;25:103–116. [DOI] [PubMed] [Google Scholar]
- 35.Delgado MK, Yokell MA, Staudenmayer KL, et al. Factors associated with the disposition of severely injured patients initially seen at non-trauma center emergency departments: disparities by insurance status. JAMA Surg 2014;149:422–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beck B, Smith K, Mercier E, et al. Potentially preventable trauma deaths: a retrospective review. Injury 2019;50:1009–1016. [DOI] [PubMed] [Google Scholar]
- 37.Newgard CD, Nelson MJ, Kampp M, et al. Out-of-hospital decision making and factors influencing the regional distribution of injured patients in a trauma system. J Trauma 2011;70:1345–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.