Abstract
Objective: To evaluate the clinical effectiveness of surface electromyography combined with a spine 3D data system. Methods: 10 idiopathic scoliosis patients (age: 12.90±3.67 years, height: 155.90±20.07 cm, weight: 48.00±12.86 kg, 6 major thoracic lateral bends and 4 lumbar bends) who were selected to attend the outpatient clinic of Ruijin Rehabilitation Hospital, First diagnosed as scoliosis by imaging examination (EOS system), evaluation by using the surface electromyography monitoring system, the radiation-free 3D spine data acquisition and analysis system, the surface electromyography of the paravertebral muscles (root mean square value (RMS) of the resting standing and action position of the spine) and the Cobb angle of scoliosis were recorded. Results: The RMS of the convex side was larger than that of the concave side in the two postures (P<0.05), and The RMS value of bilateral action position was significantly higher than that of rest position (P<0.05). There was no correlation between RMS ratio and Cobb angle in two positions of thoracic scoliosis (P>0.05). There was a significant correlation between the RMS ratio at rest position of lumbar scoliosis and Cobb angle. At rest, the RMS value of convex side was significantly correlated with the Cobb angle measured by the EOS system and the 3D data system (P<0.05, of which P<0.01). The Cobb angle measured by 3D data system and the EOS system was significantly correlated (P<0.01). Conclusion: Surface EMG can be used to evaluate the motor function of paravertebral muscles on both sides of scoliosis patients. The new 3D data system has high accuracy in evaluating scoliosis. The combination of the two can dynamically evaluate scoliosis, which is more clinically effective.
Keywords: Surface electromyography, 3D data acquisition and analysis system, idiopathic scoliosis
Introduction
Scoliosis is a three-dimensional spinal deformity caused by primary or secondary causes. The incidence of adolescent idiopathic scoliosis (AIS) is increasing year by year [1]. The current clinically accepted diagnostic method is physical examination combined with imaging examination, but there are some limitations due to imaging examination [2]. It cannot reflect the performance difference of patients in static position and real-time movements, and there are lack of evaluation of paravertebral muscles on both sides of the spine, so it is impossible to quickly complete the evaluation of rehabilitation efficacy, which obviously limits the rapid screening of rehabilitation means and the enthusiasm of patients for rehabilitation.
Surface electromyography (sEMG) is a commonly used rehabilitation evaluation method in clinical practice that has many advantages. It can dynamically monitor and quantify the muscle activation during somatic motion [3]. At present, few patients with scoliosis use this method. At the same time, with the development and progress of evaluation methods, the non-invasive and non-radiation 3D data collection and analysis system has obvious advantages [4]. The parameters of scoliosis can be detected in real time in different positions and during manual treatment [5]. Therefore, this study intends to explore the clinical effectiveness of sEMG in scoliosis evaluation by combining it with the 3D spinal data acquisition and analysis system.
Material and methods
General information
10 AIS patients in our hospital were selected, including 8 males and 2 females; 6 cases of major thoracic scoliosis, Cobb angle 17.33±10.58, 4 cases of lumbar scoliosis, and Cobb angle 18.00±5.60; age 18.00±5.60 years; height 155.90±20.07 cm; weight 48.00±12.86 kg. Inclusion criteria: ① diagnosis of Scoliosis by the International Society for Scoliosis Research (Scoliosis Research Society, SRS), imaging confirmed scoliosis with Cobb angles greater than 10°; ② did not receive any treatment; ③ subjects and family gave informed consent for the study and signed an informed consent. Exclusion criteria: ① cognitive impairment unable to complete the examination and rehabilitation; ② mental illness; ③ vital organ dysfunction, standing position unable to maintain for 5 minutes; ④ acute episode of disease; ⑤ unwilling to join the investigator. The study was approved by the ethics committee of our hospital (ethical approval number: RKIRB2023-17).
Methods
sEMG information acquisition
Standard subjects signed informed consent using the sEMG analysis system (Nanjing Wei Medical Technology Co., Ltd., model, ZY2018000005), selected scoliosis evaluation mode, patients took the standing position, placed the electrode on the paravertebral muscle, and complete the following actions: keeping standing for 20 seconds, forward extreme flexion for 5 seconds, backward extreme flexion for 5 seconds, and at the end of the test, respectively recorded patients resting in the standing position and action position on both sides of the paravertebral muscle of the root mean square value (root mean square value, RMS).
3D detection method of data acquisition and analysis system
Using the 3D data acquisition and analysis system (Forethought 3D spine sensing system, model: FT07W) (Figure 1), the subject took a resting standing position with feet shoulder-width apart, hands naturally drooping, head up, and eyes ahead. The spinous process is used as the anatomical reference marker of the back, and the positioning point is cervical 7 to waist 5. The detector takes the whole spine scan from top to bottom, and the number of Cobb angles can be read directly at the end of the measurement (Figure 2). The 3D spine parameters obtained were correlated with the EOS parameters.
Figure 1.
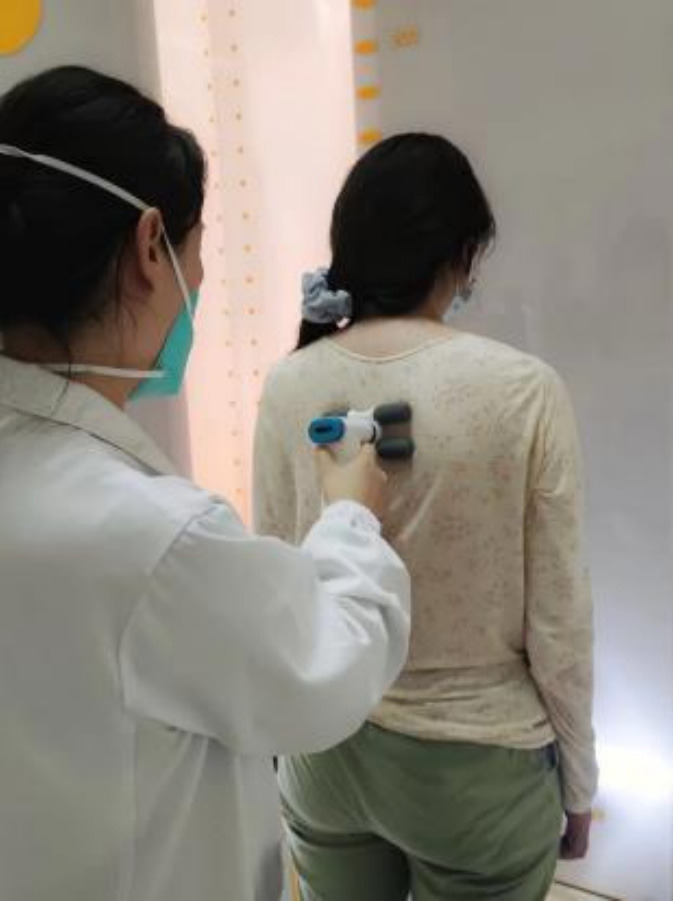
3D data acquisition and analysis system collector and subject detection.
Figure 2.

Example of detection results for 3D data acquisition and analysis system.
Analysis of observation indicators
① Compare the RMS of the paravertebral muscles on both sides of the scoliosis in resting standing and motion positions; ② Calculates the RMS ratio of the paravertebral muscles and analyses the severity of scoliosis; ③ Correlation analysis was performed on RMS of both sides of the spine and Cobb angle measured by two methods.
Statistical methods
The data were analysed by spss 26.0 software. The normally distributed measurement data were expressed as mean ± standard deviation (x̅±s), the intra-group comparison used a paired sample t-test. Pearson correlation analysis was used to study the correlation between RMS, RMS ratio, and two detection methods on both sides of the convex and concave.
Results
sEMG signals of paravertebral muscles on both sides of the convex and concave sides in two postures
The results of the RMS analysis of the paravertebral muscles on both sides of the scoliosis (Table 1) showed that the RMS of the convex side of the two postures was larger than the concave side, and the difference was statistically significant (P<0.05). The RMS value of the bilateral action position was significantly higher than the rest position (P<0.05).
Table 1.
Comparison of RMS of paravertebral muscles on both sides of scoliosis indices
| Project | Convex side RMS/μV | Concave side RMS/μV | t | P |
|---|---|---|---|---|
| Resting position | 20.25±4.20 | 15.21±2.51 | 4.920 | 0.001 |
| Active position | 54.29±19.60 | 28.69±10.11 | 6.654 | <0.001 |
| t | -5.603 | -4.141 | ||
| P | <0.001 | 0.003 |
Correlation analysis between the ratio of EMG signals on both sides of different segments and the Cobb angle
Through a comparative analysis of patients with thoracolumbar scoliosis (Table 2), the RMS ratio of thoracic scoliosis and Cobb angle showed no correlation (P>0.05). The r value of lumbar scoliosis at rest position was 0.940, P<0.05, and the correlation was very strong; The correlation of action position is low and has no statistical significance.
Table 2.
Correlation analysis of RMS ratio and Cobb angle on both sides of the thoracolumbar segment
| Project | Thoracic scoliosis | Lumbar scoliosis | ||
|---|---|---|---|---|
|
|
|
|||
| Resting position | Active position | Resting position | Active position | |
| RMS ratio (convex/concave) | 1.37±0.24 | 2.08±0.59 | 1.29±0.21 | 1.75±0.35 |
| The Cobb angle was measured by the EOS system | 17.33±10.58 | 18.00±5.60 | ||
| r | 0.179 | 0.004 | 0.940 | -0.509 |
| P | 0.367 | 0.497 | 0.030 | 0.246 |
Correlation analysis of EMG signals from both sides of the spine and Cobb angle measured by two detection methods
According to the comprehensive correlation analysis (Table 3), there is a significant positive correlation between the convex side RMS and the Cobb angle measured by the EOS system and the 3D data system at rest, with r values of 0.632 and 0.806, respectively (P<0.05, of which P<0.01). There was no significant correlation between the concave side of the rest position and the convex and concave sides of the action position and the two detection methods. The Cobb angle measured by the 3D data system and the EOS system has a significant correlation; the r value is 0.971, P<0.01.
Table 3.
Correlation analysis between RMS and two detection methods on both sides of two body positions
| Statistics | Convex side of rest position | Concave side of rest position | Convex side of action position | Concave side of action position | The Cobb angle was measured by the EOS system | Cobb angle measured by 3D data system | |
|---|---|---|---|---|---|---|---|
| Convex side of rest position | r | 1.000 | 0.588 | 0.539 | -0.085 | 0.632 | 0.806 |
| P | 0.037 | 0.054 | 0.408 | 0.025 | 0.002 | ||
| Concave side of rest position | r | 0.588 | 1.000 | 0.224 | 0.213 | 0.374 | 0.382 |
| P | 0.037 | 0.267 | 0.278 | 0.143 | 0.138 | ||
| Convex side of action position | r | 0.539 | 0.224 | 1.000 | 0.529 | 0.190 | 0.273 |
| P | 0.054 | 0.267 | 0.058 | 0.299 | 0.223 | ||
| Concave side of action position | r | -0.085 | 0.213 | 0.529 | 1.000 | 0.135 | 0.012 |
| P | 0.408 | 0.278 | 0.058 | 0.355 | 0.487 | ||
| The Cobb angle was measured by the EOS system | r | 0.632 | 0.374 | 0.190 | 0.135 | 1.000 | 0.926 |
| P | 0.025 | 0.143 | 0.299 | 0.355 | 0.000 | ||
| Cobb angle measured by 3D data system | r | 0.806 | 0.382 | 0.273 | 0.012 | 0.926 | 1.000 |
| P | 0.002 | 0.138 | 0.223 | 0.487 | <0.001 |
Discussion
AIS occurs in teenagers aged 10 to 20 years old, with different symptoms with the increase in age and shows a gradual trend of aggravation. Some patients will have the cardiopulmonary system [6]. The dysfunction of the visceral system, the most serious, is the scoliosis of the spinal cord compression, resulting in paraplegia and having a serious impact on daily life [7]. Studies have shown that the incidence of AIS in the United States is about 2-3%, while the incidence in China has reached 1-2%, and in some southern areas, it has been as high as 5.14% [8,9], Become a major harm to the physical and mental health of teenagers [10]. The lateral X-ray of the whole spine is the gold standard for the diagnosis of the disease. The EOS imaging system is a commonly used clinical diagnostic method [11]. Like other evaluation methods, the traditional imaging examination is limited by radiation, complex operation, limited space for use, and the cost of human, material, and financial resources [12,13]. On this basis, new evaluation methods are studied and applied. In this study, sEMG was combined with a new 3D data acquisition and analysis system to provide new ideas for clinical evaluation.
The sEMG is a non-invasive examination method to quantitatively detect the motor function status of muscle by collecting bioelectrical signals during muscle activity [14]. It has the significant advantages of real-time, quantifiable and easy to operate. This study applied it to the evaluation of scoliosis and found that there were differences in sEMG signals of the paravertebral muscles on both sides of the convex and concave sides of the scoliosis spine. Due to spinal deformation, the muscles on both sides of the paravertebral body cannot maintain their normal shape [15], and are in a long-term stretching state, resulting in asymmetry on both sides. The electrical signals of the muscles on the convex side are greater than those on the concave side. At the same time, the RMS values on both sides of the patient during movement are much higher than those in the stationary state, which is the same as previous similar studies. Chen et al. [16] studied the contraction of muscles on both sides of the spine in 9 AIS patients after Schroth exercise therapy, and the results showed that the sEMG activity of the muscles after exercise was higher than that of the relaxed standing state before exercise. In the study of AIS patients by He Chen et al. [17], it was found that there was a statistically significant difference in RMS between the convex and concave sides of the sEMG signal in the top vertebral area of the paravertebral muscles, with the convex side being greater than the concave side. The differences in RMS between resting and upper-limb weight-bearing standing in AIS patients were analyzed, indicating that the RMS difference further increased during weight-bearing. This indicates that sEMG is also applicable for functional evaluation in AIS patients.
This experiment divided all cases into thoracic and lumbar scolioses. After analysis and comparison, it was found that there was a significant positive correlation between the RMS ratio and the Cobb angle of the lumbar scoliosis in the resting position. Considering the limitations of the sample size in this experiment, the lumbar spine is more flexible than the thoracic spine, resulting in a much greater range of motion in the lower back compared to the chest. At the same time, there is more activation of the lower back muscles during the movement position, so there may be statistical significance when supported by the number of cases. During the experimental process, the evaluation environment and instrument interference of sEMG may cause certain errors in the evaluation results.
Correlation analysis was conducted on the RMS, the EOS system measured the Cobb angle, and the 3D data system measured the Cobb angle of all cases on both sides of the convex and concave sides in two different body positions. It was found that the correlation between the 3D data system and the EOS system measured Cobb angle was significant (P<0.01, mean difference: 1.86±1.42), indicating that this new 3D data system has higher accuracy in measuring Cobb angle. At the same time, it was found during the research process that the 3D data system takes less time and has higher applicability compared to the EOS system. The RMS value of the convex side during resting position is positively correlated with the Cobb angle measured by the EOS system and 3D data system, with P<0.01 compared to the 3D data system. This result indicates that the sEMG signal of the convex paraspinal muscle increases with the increase in Cobb angle in the patient’s resting standing position and is more correlated with the Cobb angle measured by the 3D data system. Guan et al. [18] included 100 AIS patients and found that the paraspinal muscle electromyography activity on the convex side was positively correlated with AIS severity. Consistent with the performance of pulling the muscles throughout the body, the larger the angle of lateral bending, the greater the force on the paraspinal muscles, and the greater the electromyographic signal value displayed, showing a positive correlation between the two. The effectiveness and accuracy of the 3D data system detection were confirmed in this experiment, and the results were consistent with those obtained from sEMG detection. Asymmetric RMS on both sides also assisted in the diagnosis of scoliosis. Among them, the sEMG signal on the convex side of the resting position obtained in this experiment had a higher correlation with the results measured by the 3D data system, and the equipment used in both examinations was fast and convenient, with minimal impact on patients during evaluation, achieving high satisfaction. The requirement for venue and spatial environment is relatively small, making it more clinically practical. The combined application of the two can evaluate patients in different states, especially in evaluating the immediate efficacy of manual rehabilitation treatment, providing new ideas for the evaluation of scoliosis.
This study demonstrated the clinical effectiveness of the combined application of sEMG signal detection of the paravertebral muscles on both sides of the convex and concave sides in AIS patients and evaluated it in conjunction with a new spinal 3D data acquisition and analysis system, with significant significance in diagnosing scoliosis. Both types of examinations are non-invasive and radiation free, and their combined use has high clinical effectiveness and accuracy. During the research process, it was found that two evaluation methods can achieve real-time detection during rehabilitation treatment processes, such as manipulation, which can quickly evaluate the effectiveness of rehabilitation. Compared to traditional imaging examinations, they have a positive effect on the rapid screening of rehabilitation methods. Its advantages are beneficial for both patients and healthcare workers, and it is expected to provide new directions for researchers in scoliosis related research, promoting the updating and optimization of new evaluation methods.
Acknowledgements
This study was supported by the program of Research Project in Huangpu District, Shanghai (HLQ202212).
Disclosure of conflict of interest
None.
References
- 1.Peng Y, Wang SR, Qiu GX, Zhang JG, Zhuang QY. Research progress on the etiology and pathogenesis of adolescent idiopathic scoliosis. Chin Med J (Engl) 2020;133:483–493. doi: 10.1097/CM9.0000000000000652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen XF, Tao YJ. Computer-assisted orthotopic X-ray measurement of spine length in adolescent idiopathic scoliosis. China Maternal and Child Health Research. 2020;31:1476–1480. [Google Scholar]
- 3.Wang YJ, Li JJ, Zhou HJ, Liu GL, Zheng Y, Wei B, Zhang Y, Hao CX, Kang HQ, Yuan Y, Gao LJ. Surface electromyography as a measure of trunk muscle activity in patients with spinal cord injury: a meta-analytic review. J Spinal Cord Med. 2016;39:15–23. doi: 10.1179/2045772315Y.0000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu M. Imaging study and application of adolescent scoliosis. Journal of Molecular Imaging. 2022;45:627–631. [Google Scholar]
- 5.Zhao J, Chen K, Li QH, Hang HD, Mao NF, Shen LY, Yang CW, Li M. Preliminary application of spinal morphometry based on the three-dimensional position of the surface projection space in morphometry of scoliosis. Journal of the Second Military Medical University. 2020;41:1198–1202. [Google Scholar]
- 6.Li L, Yao CC, Chen TT, Shen XY. Chest X-ray analysis of the association of senile degenerative scoliosis and pulmonary infection. Practical Medical Technology Journal. 2020;27:991–993. [Google Scholar]
- 7.Seleviciene V, Cesnaviciute A, Strukcinskiene B, Marcinowicz L, Strazdiene N, Genowska A. Physiotherapeutic scoliosis-specific exercise methodologies used for conservative treatment of adolescent idiopathic scoliosis, and their effectiveness: an extended literature review of current research and practice. Int J Environ Res Public Health. 2022;19:9240. doi: 10.3390/ijerph19159240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hengwei F, Zifang H, Qifei W, Weiqing T, Nali D, Ping Y, Junlin Y. Prevalence of idiopathic scoliosis in Chinese schoolchildren: a large, population-based study. Spine (Phila Pa 1976) 2016;41:259–264. doi: 10.1097/BRS.0000000000001197. [DOI] [PubMed] [Google Scholar]
- 9.Li M, Su L, Zhong H, Zeng L, Huang QM, Kang J, Hao HH, Li XC. Investigation and analysis of the prevalence of idiopathic scoliosis in junior high school students in Shenzhen. Shenzhen Journal of Integrated Traditional Chinese and Western Medicine. 2018;28:3–5. [Google Scholar]
- 10.Singh H, Shipra, Sharma V, Sharma I, Sharma A, Modeel S, Gupta N, Gupta G, Pandita AK, Butt MF, Sharma R, Pandita S, Singh V, Rai E, Ikegawa S, Sharma S. The first study of epidemiology of adolescent idiopathic scoliosis shows lower prevalence in females of Jammu and Kashmir, India. Am J Transl Res. 2022;14:1100–1106. [PMC free article] [PubMed] [Google Scholar]
- 11.Hey HWD, Chan CX, Wong YM, Sng JW, Ong HY, Tan CS, Liu GK, Wong HK, Quek ST. The effectiveness of full-body EOS compared with conventional chest X-ray in preoperative evaluation of the chest for patients undergoing spine operations: a preliminary study. Spine (Phila Pa 1976) 2018;43:1502–1511. doi: 10.1097/BRS.0000000000002845. [DOI] [PubMed] [Google Scholar]
- 12.Qin L, Du LJ, Yan FH. Reliability and accuracy of EOS 3D imaging evaluation of scoliosis in adults. Chinese Journal of Bone and Joint. 2016;5:568–571. [Google Scholar]
- 13.Zhang SH, Li FL, Wang S, Wang LC. Progress in new imaging techniques for adolescent idiopathic scoliosis. Journal of Clinical Orthopedics. 2022;25:595–599. [Google Scholar]
- 14.Chen C, Ma SH, Yu Y, Sheng XJ, Zhu XY. Segment-wise decomposition of surface electromyography to identify discharges across motor neuron populations. IEEE Trans Neural Syst Rehabil Eng. 2022;30:2012–2021. doi: 10.1109/TNSRE.2022.3192272. [DOI] [PubMed] [Google Scholar]
- 15.Kitagawa K, Uezono T, Nagasaki T, Nakano S, Wada C. Relationship between surface electromyography of the spinae erector muscles and subjectively adjusted step length in the supporting standing-up motion. J Phys Ther Sci. 2019;31:869–872. doi: 10.1589/jpts.31.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He C, Yang JT, Zheng Q, Mei Z, Ma CZ. How do paraspinal muscles contract during the schroth exercise treatment in patients with adolescent idiopathic scoliosis (AIS)? Bioengineering (Basel) 2022;9:234. doi: 10.3390/bioengineering9060234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He C, Li L, Li YL, Xu LF, Li HD. Symmetry of superficial EMG signals and correlation with lateral curvature angle in adolescent idiopathic scoliosis. Biomedical Engineering and Clinical. 2022;26:150–155. [Google Scholar]
- 18.Guan CL, Cao J, Mu XL, Zhi XJ, Gou RS. Correlation between severity of adolescent idiopathic scoliosis and paravertebral muscle EMG activity and lumbar mobility. Journal of Henan Medical College. 2021;33:15–18. [Google Scholar]


