Abstract
Chronic patellar tendinosis is an overuse pathology affecting both adolescents and adults who participate in jumping sports. It often can be managed with nonoperative modalities. Chronic patellar tendinosis is associated with degenerative changes to the proximal, posterior patellar tendon. Operative treatments include open or arthroscopic debridement of the pathologic tissue. When a debridement is performed, the resulting defect forms a void at the posterior segment of the proximal patellar tendon. The authors assert this defect should be addressed in elite athletes with a graft as opposed to tendon debridement alone to prevent recurrence and maximize tendon strength. Described herein is the senior author’s preferred technique for open patellar tendon debridement and allograft reinforcement with suture tape augmentation for chronic patellar tendinosis. This technique creates both a tension band construct with allograft to offload the tendon proximally and an InternalBrace construct longitudinally for patellar tendon load sharing.
Technique Video
Repetitive microtrauma to the proximal patellar tendon can lead to patellar tendinosis in which the collagen framework experiences mucoid degeneration, vascular changes, and neural changes.1 The diagnosis is made clinically, with symptoms of chronic anterior knee pain at the inferior pole of the patellar tendon reported. It is associated with necrosis in the posterior half of the proximal patellar tendon on magnetic resonance imaging.2,3 The mainstay of treatment continues to be conservative management, which fails, however, in approximately 10% of patients.4, 5, 6 Operative management of patellar tendinosis has shown favorable results with both open and arthroscopic techniques.7 The authors contend that return to play rates can be increased with use of an allograft tension band system with suture tape augmentation in addition to simple debridement. Described herein is the senior author’s (P.A.S.) preferred technique for open patellar tendon reconstruction using semitendinosus allograft with suture tape augmentation (InternalBrace; Arthrex; Naples, FL).
Surgical Technique
Graft Preparation
A 280-mm semitendinosus allograft is soaked in vancomycin solution for 20 minutes and tensioned on a graft-prep station at 15 pounds of pull for 15 minutes to eliminate tendon creep. The graft is then folded over a Tightrope (Arthrex), which is preloaded with an InternalBrace suture tape (Fig 1). At the inferior margin of the TightRope, the limbs of the graft are sutured with a No. 0 VICRYL (Ethicon; Johnson & Johnson; New Brunswick, NJ) suture to keep the folded over tails symmetric. Each free end of graft is prepared with a FiberLoop (Arthrex) suture tape in a whipstitch fashion over a distance of 15 mm. The doubled-over graft diameter is measured and typically found to be 7 to 8 mm. This measurement corresponds to the reamer diameter used at the inferior pole of the patella to create the fixation socket.
Fig 1.
Semitendinosus allograft doubled over a TightRope preloaded with a FiberTape for eventual InternalBrace creation. Note the pull sutures (∗) connected to the TightRope mechanism and the 2 limbed semitendinosus allograft (†) with FiberTape (‡).
Tendinosis Debridement
A midline incision is made over the patellar tendon and carried carefully down through subcutaneous tissue. The peritenon is incised and reflected for later closure. The area of pathology is identified by palpation of a thickened nodule beneath the patella tendon just distal to the inferior pole of the patella. The patellar tendon is incised in the midline. The healthy patellar tendon tissue both medially and laterally is reflected to expose the disorganized collagen of the deeper portion of the tendon. The pathologic tendon is sharply excised and debrided back to a margin of healthy-appearing tendon. It is common to have to undermine healthy tendon tissue medially and laterally. The soft tissue of the inferior pole of the patella is debrided with a curette and a rongeur back to bleeding bone.
Tunnel Preparation
A 1-cm incision is then made at the superior pole of the patella and sharp dissection is carried down through the quadriceps tendon longitudinally. A point-to-point drill guide is then placed with tip of the guide at the superior pole of the patella (Table 1). The guide pin is advanced from the inferior to superior pole of the patella (Fig 2A). Orthogonal fluoroscopic images are obtained to verify placement of the guide pin in the center of the patella on both projections. An 18- to 20-mm depth socket is then created by reaming over the guide pin with a 7- to 8-mm reamer (as determined by allograft diameter). The socket is irrigated to remove bony debris and a FiberLink (Arthrex) passing suture is shuttled through the patella.
Table 1.
Pearls and Pitfalls of Patellar Tendon Reconstruction With Suture Tape Augmentation as a Treatment for Recalcitrant Patellar Tendinosis
| Pearls | Pitfalls |
|---|---|
| Point-to-point drill guide for patellar drilling and check intraoperative fluoroscopy to insure optimal position in patella | Avoid over-resection of healthy patellar tendon |
| Knee at 100° during all points of fixation especially for InternalBrace fixation | Risk of overconstraint with either graft or InternalBrace |
| Hemostat under suture tape to avoid overtensioning | Avoid allograft socket and FiberTak fixation anchor convergence |
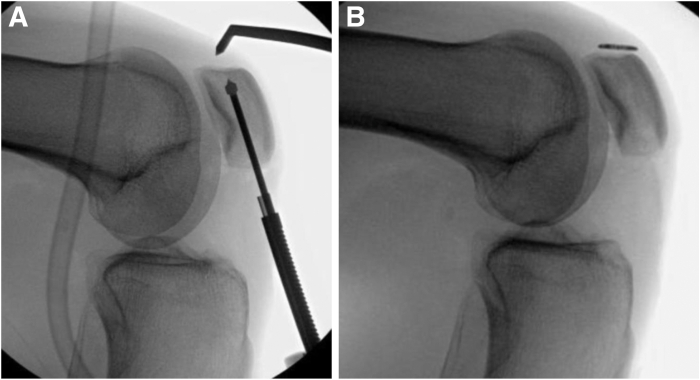
Fig 2.
Intraoperative lateral right knee fluoroscopy images demonstrating (A) drilling of the patella from the inferior to superior pole using a guide pin and point to point guide and (B) the TightRope fixation button flipped at the superior pole of the patella.
Graft Passage and Fixation
The TightRope with InternalBrace fixation button is passed through the patella with the FiberLink shuttling suture. The button is then flipped at the superior pole of the patella with fluoroscopic confirmation (Fig 2B). The doubled semitendinosus graft is then delivered into the patellar socket by pulling on the shortening strands of the TightRope mechanism (Fig 3).
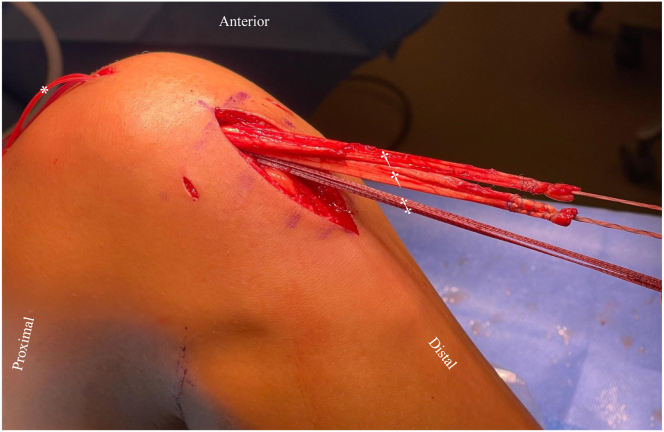
Fig 3.
Lateral right knee clinical photograph demonstrating the allograft in place at the inferior pole of the patella. Note the pull sutures (∗) connected to the TightRope mechanism proximally exiting the superior pole of the patella and the two limbed semitendinosus allograft (†) with FiberTape (‡) for InternalBrace creation exiting the inferior pole of the patella.
A free needle is then used to pass each free limb of the whipstitched allograft tendon distally through the patellar tendon on both the medial and lateral sides from deep to superficial around the remaining intact patellar tendon (Fig 4B). Attention is turned toward fixation of the InternalBrace suture tape distally. The fixation site is identified just above the tibial tubercle midline on the tibia. A 4.5-mm drill is used to create a pilot hole, which is subsequently tapped. The knee is placed in 100° of flexion. A hemostat is placed under the InternalBrace construct to prevent overtightening and a 4.75-mm BioComposite SwiveLock (Arthrex) is secured distally (Fig 4A). The knee is cycled through a full range of motion to ensure full flexion.
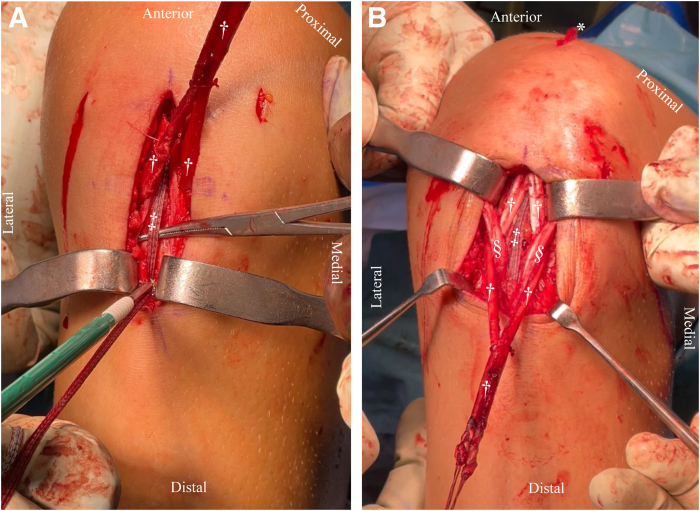
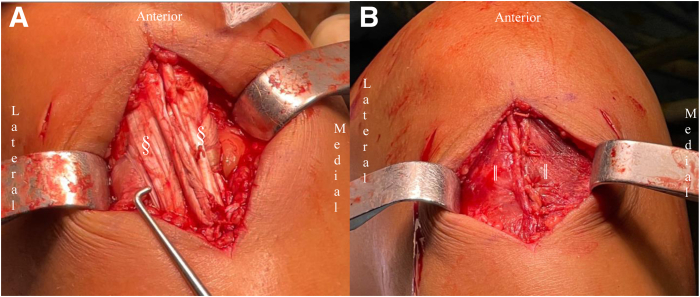
Fig 4.
Right knee clinical photographs demonstrating the allograft and InternalBrace placement. Note the pull sutures (∗) connected to the TightRope mechanism proximally exiting the superior pole of the patella and the 2 limbed semitendinosus allograft (†) with FiberTape (‡) for InternalBrace creation exiting the inferior pole of the patella. The InternalBrace construct is fixated distally at the tibial tubercle with a SwiveLock anchor (A). The InternalBrace construct is fixated in 100° of knee flexion with a hemostat under the FiberTape to prevent over tensioning and stress shielding. The semitendinosus allograft (†) is weaved obliquely (B) through remaining healthy patellar tendon medially and laterally (§).
Finally, the allograft tension band augmentation is completed by fixating the remaining allograft free ends projecting through the medial and lateral margins of healthy remaining patellar tendon back proximally to the inferior pole of the patella (Fig 5). This is facilitated by linking the 2 free ends of allograft with a No. 0 VICRYL suture to unitize the limbs for fixation. A knotless knee FiberTak (Arthrex) anchor is placed at the inferior pole of the patella, with care taken to avoid the previously made and filled socket (Fig 5A, Table 1). The No. 0 FiberWire (Arthrex) repair suture preloaded into the FiberTak anchor is passed through the two free limbs of the graft in a mattress fashion (Fig 5B). The free end of the repair suture is passed through the anchor using the shuttling suture and then tensioned to reduce the graft to the inferior pole of the patella in an onlay fashion (Fig 5C). The excess graft is excised (Fig 5D).
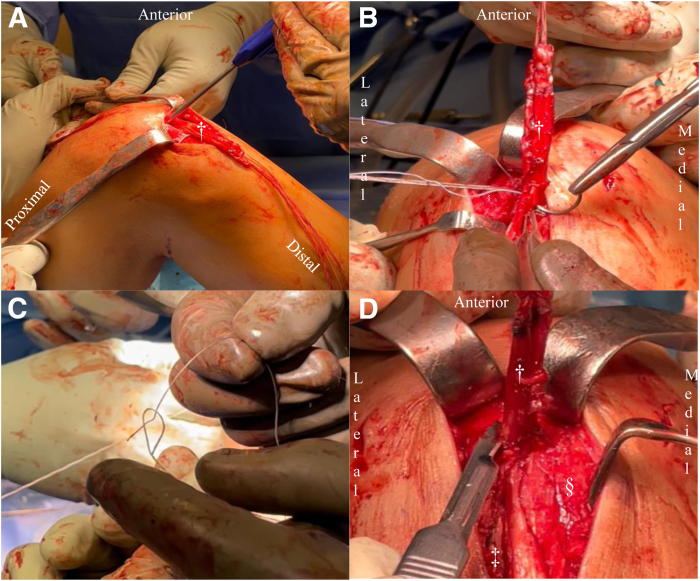
Fig 5.
Right knee clinical photographs demonstrating fixation of the remaining allograft to the inferior pole of the patella using a knotless knee FiberTak anchor. (A) Drilling for the anchor, with care taken to avoid the previously made and filled socket. (B) The repair suture preloaded into the FiberTak anchor is passed through the 2 free limbs of the graft in a mattress fashion. (C) The free end of the repair suture is passed through the anchor using the shuttling suture and then tensioned to reduce the graft to the inferior pole of the patella in an onlay fashion. (D) The excess graft is excised. Key: (†) 2 limbed semitendinosus allograft, (‡) FiberTape for InternalBrace creation, (§) remaining healthy proximal patellar tendon.
The wound is then thoroughly irrigated. With the knee still in 100° of flexion, the remaining normal patellar tendon tissue is then reapproximated incorporating the graft tissue proximally and in the midline with No. 0 mattress VICRYL sutures (Fig 6A). The peritenon is closed over the patellar tendon with interrupted 2-0 VICRYL mattress sutures (Fig 6B). Subcutaneous followed by skin closure of the proximal and distal wounds are then performed as per personal preference. The extremity is then placed in a hinged knee brace locked in full extension.
Fig 6.
Right knee clinical photographs demonstrating a multilayered closure. (A) Incorporation of healthy remaining tendon (§) into allograft. (B) Closure of peritenon (‖) over the reconstructed tendon.
Postoperative Rehabilitation Protocol
The patient is started on early active motion with an emphasis on quadriceps exercises and straight leg raises. The exercise bike is started after 2 weeks. The patient is partial-weight bearing with a hinged knee brace locked in extension for the first 6 weeks. Weight-bearing is progressed, and the patient is allowed off crutches once no extensor lag and good leg control is demonstrated. Closed-chain exercises are initiated once the patient is full weight-bearing. No open-chain quadriceps exercises are done to protect the patellar tendon. Jogging starts usually at 3 months with functional return to sport type exercises at 4 months. Return to sport is in the 5- to 6-month range, depending on individual progress.
Discussion
The described technique creates both a tension band construct with allograft to increase collagen density while offloading the tendon proximally. In addition, it adds an InternalBrace construct longitudinally for patellar tendon load sharing. This technique is a variation of Woodmass et al.’s 8 technique for the treatment of patellar tendon ruptures with residual tendon gapping. Chronic patellar tendinosis can lead to tendon degeneration and necrosis. After the tendinosis is excised, a large defect can be observed. In high-level athletes, the authors believe it is essential to fill this defect with new tendon and augment the remaining tendon.
When considering surgical intervention for patellar tendinosis, many factors must be considered including the extent of tendinous degeneration as well as the patient’s return to sport needs. Some authors contend that return to sport may be faster with arthroscopic surgery7; however, one retrospective cohort study found no difference in time to return to sport when comparing open versus arthroscopic intervention.9 Studies report return to the same level of sport to be greater than 80% for both arthroscopic and open modalities.2,10 Unfortunately, symptoms recur in approximately 10% of operatively managed patients.11 It is the authors’ opinion that symptom recurrence may be due to inadequately debrided pathologic tissue or the presence of remaining proximal tissue undergoing significant strain. This may also have implications in rates of return to play.
This described technique has several advantages and potential disadvantages (Table 2). It allows for the creation of an allograft tension band construct that both increases collagen density and provides load-sharing to the proximal aspect of the remaining patellar tendon following complete debridement of all nonviable tissue. Additional load-sharing is provided by an InternalBrace construct via a FiberTape to prevent further tendon injury while allowing for early and aggressive rehabilitation motion protocols. Unlike arthroscopic approaches, this technique results in minimal trauma to the Hoffa fat pad, a structure known to be exceedingly well innervated,1 while allowing for complete debridement of diseased tissue. Potential risks include patella fracture, over-tensioning, and over-resection of too much healthy patellar tendon leading to patellar tendon rupture. Further outcomes studies are needed to determine the long-term outcomes of this technique with a specific focus on symptom recurrence and return to play.
Table 2.
Advantages and Disadvantages of Patellar Tendon Reconstruction With Suture Tape Augmentation as a Treatment for Recalcitrant Patellar Tendinosis
| Advantages | Disadvantages |
|---|---|
| Allograft tension band | Morbidity of open approach |
| Suture tape augmentation | Risk of overtensioning/stress shielding |
| Removal of unhealthy tissue | Cost |
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: J.A.R. reports nonassociated funding grants from Arthrex. P.A.S. reports consulting or advisory, funding grants, and speaking and lecture fees from Arthrex; and equity or stocks from Spinal Simplicity. All other authors (D.R.W. and A.D.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Supplementary Data
Shown is a technique for right knee patellar tendon reconstruction using semitendinosus allograft with suture tape augmentation for recalcitrant patellar tendinosis. This technique highlights graft preparation, tendinosis debridement, tunnel preparation, graft passage and fixation, and the postoperative rehabilitation protocol.
References
- 1.Sanchis-Alfonso V., Roselló-Sastre E., Subías-Lopez A. Neuroanatomic basis for pain in patellar tendinosis ("jumper's knee"): A neuroimmunohistochemical study. Am J Knee Surg. 2001;14:174–177. [PubMed] [Google Scholar]
- 2.Shelbourne K.D., Henne T.D., Gray T. Recalcitrant patellar tendinosis in elite athletes: Surgical treatment in conjunction with aggressive postoperative rehabilitation. Am J Sports Med. 2006;34:1141–1146. doi: 10.1177/0363546505284239. [DOI] [PubMed] [Google Scholar]
- 3.Arner J.W., Kaeding C.C., Bradley J.P. Management of patellar tendinopathy. Arthroscopy. 2024;40:13–15. doi: 10.1016/j.arthro.2023.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Marigi E.M., Buckley P., Razi F., et al. Patellar tendinopathy: Critical analysis review of current nonoperative treatments. JBJS Rev. 2022;10 doi: 10.2106/JBJS.RVW.21.00168. [DOI] [PubMed] [Google Scholar]
- 5.Santander J., Zarba E., Iraporda H., Puleo S. Can arthroscopically assisted treatment of chronic patellar tendinopathy reduce pain and restore function? Clin Orthop Rel Res. 2012;470:993–997. doi: 10.1007/s11999-011-1886-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maffulli N., Giai Via A., Oliva F. Revision surgery for failed patellar tendinopathy exploration. Sports Med Arthrosc Rev. 2017;25:36–40. doi: 10.1097/JSA.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 7.Brockmeyer M., Diehl N., Schmitt C., Kohn D.M., Lorbach O. Results of surgical treatment of chronic patellar tendinosis (jumper's knee): A systematic review of the literature. Arthroscopy. 2015;31:2424–2429.E3. doi: 10.1016/j.arthro.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Woodmass J.M., Johnson J.D., Wu I.T., Krych A.J., Stuart M.J. Patellar tendon repair with ipsilateral semitendinosus autograft augmentation. Arthrosc Tech. 2017;6:e2177–e2181. doi: 10.1016/j.eats.2017.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cucurulo T., Louis M.L., Thaunat M., Franceschi J.P. Surgical treatment of patellar tendinopathy in athletes. A retrospective multicentric study. Orthop Traumatol Surg Res. 2009;95:S78–S84. doi: 10.1016/j.otsr.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Lee D.W., Kim J.G., Kim T.M., Kim D.H. Refractory patellar tendinopathy treated by arthroscopic decortication of the inferior patellar pole in athletes: Mid-term outcomes. Knee. 2018;25:499–506. doi: 10.1016/j.knee.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Maier D., Bornebusch L., Salzmann G.M., Südkamp N.P., Ogon P. Mid- and long-term efficacy of the arthroscopic patellar release for treatment of patellar tendinopathy unresponsive to nonoperative management. Arthroscopy. 2013;29:1338–1345. doi: 10.1016/j.arthro.2013.05.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Shown is a technique for right knee patellar tendon reconstruction using semitendinosus allograft with suture tape augmentation for recalcitrant patellar tendinosis. This technique highlights graft preparation, tendinosis debridement, tunnel preparation, graft passage and fixation, and the postoperative rehabilitation protocol.