Abstract
Introduction
Globally, about 45 million under-five children have suffered from wasting where Asian and African countries have the major share of these wasted children. Despite wasting is affected all types of populations, the long and short term effect is more severe and sensitive in under-two aged children. Hence, this review was intended to assess pooled prevalence and associated factors of wasting among under-two children in Ethiopia.
Methods
The search was done using electronic data bases (Hinari, PubMed, Google scholar, Scopus) and research repositories from June 19–22/2023. The review included articles published between January 2013 and December 2023.The study included Cross-sectional/case control studies which report the prevalence and associated factors of wasting in under-two aged children. The quality of included studies was assessed using the Joanna Briggs Institute (JBI) quality assessment checklists for observational studies. The presence of heterogeneity between included studies was evaluated using Cochrane Q-test and the I2 statistics. Publication bias was checked through graphical and statistical test. Associated factors were estimated by random effect model using DerSimonian-Laird model weight.
Results
The pooled prevalence of wasting among under-two children was 10.91% (95% CI: 8.97–12.85; I2 = 86.36%). Absence of maternal antenatal follow up (OR; 3.23: 95%CI: 1.20–5.26), no exclusive breast feeding until six months (OR; 5.30; 95%CI: 1.17–9.43), current illness of the child (OR; 2.58: 95%CI: 1.78–3.37), large family size (OR; 12.38; 95%CI: 1.37–26.13) and low wealth status of the households (OR; 3.91; 95%CI: 1. 54-8.36) were significant factors of wasting among under-two children.
Conclusions
This study disclosed that the pooled prevalence of wasting among under- two children were high in Ethiopia. Absence of maternal antenatal follow up, no exclusive breast feeding, low wealth status of the households, large family size and current illness of the child were significant factors of wasting. Strictly adherence of maternal antenatal follow up, counsel the parents to feed only breast milk until six months, limit the number of family size to the level of the household income and early treatment of the sick child were recommended. Furthermore, scale up the wealth status and living standard of the family can address the agenda of reducing and eradicating all forms of malnutrition. This review registered at PROSPERO with registration number CRD42023414914 (https://www.crd.york.ac.uk/prospero/#myprospero).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20063-1.
Keywords: Wasting, Under-two aged children, Ethiopia
Introduction
Malnutrition is still continues as a major public health problem throughout the globe that affects almost every country [1]. Undernutrition (wasting, stunting and underweight) is a particular and alarming public health concern in low and middle-income countries [2]. Wasting is a measure of acute undernutrition and represents the failure to receive adequate nutrition within short period of time [3]. It is defined as weight-for-height <-2 standard deviation (moderate wasting) or <-3standard deviation(severe wasting/ severe acute malnutrition) median of the WHO Child growth standards [4].
Childhood wasting is high risk of morbidity and mortality .It results in negative consequence of development in young children [5, 6] which is caused by an inadequate amount or quality of food and repeated infections [7].Wasted children have impaired immunity system to fight against infectious agents which leads to increased severity, duration, and susceptibility to infectious diseases that increases the risk of death [8, 9]. Evidences indicated that the risk of mortality among wasted children were ten times higher than well-nourished children [6]. Moreover, children with wasting are exposed for long term developmental delay [10], , poor cognition and learning performance, short adult stature, lower productivity, and chronic disease in the adulthood [11].
Globally, in 2022 about 45 million under-five children were suffered from wasting. Of which 13.7 million children were affected by severe wasting. Asian and African countries were a home to these severe wasted children [3]. It causes 1 in five deaths of children worldwide [12]. Evidence from 94 low and middle-income countries also revealed that the prevalence of wasting in under- two years children was 14% [13]. The pooled evidence of 32 Sub-Saharan African countries also disclosed that the prevalence of wasting among children age 6–23 months was 9.4% [14]. According to 2019 Ethiopia demographic and health survey (EDHS), the prevalence of wasted children in Ethiopia was 7% with the highest prevalence in Somali region (21%) [15].
Although wasting is affected all types of populations, the long and short term effect is more severe and sensitive in under-two aged children [16]. Because, it is a time frame/window of opportunity at which children undergo fast growth and development, susceptible to infection, and are in need of adequate and balanced nutrition [17]. Lack of required nutrition during this critical time prone the child for: growth flattering [18], concurrent wasting and stunting, compromised neurocognitive development, weakened immunity system, increase the risk of premature death in many folds [19]. The Contributing factors of wasting in under-two years children were: lack of exclusive breast feeding, inadequate food diversity [20], prelactal feeding, removal of colostrum, maternal education status [21], poor wealth index, rural settings [22], age of child (below 12 months), child with current history of diarrhea, no maternal nutrition counseling during pregnancy [23].
Currently, the world has planned and implemented several strategies like; Sustainable Development Goals (SDGs) in collaborating with World health Assembly (WHA) [24], Global Action Plan on Child Wasting [25] and USAID Multi-Sectoral Nutrition Strategy [26] to reduce the prevalence of child wasting to less than 5% by 2025 and further reduce the prevalence to less than 3% by 2030. Ethiopia also has planned and carried out similar strategies [27] to reach national and international targets of alleviating and eliminating this wide spread corrosive public health problem. Despite these targets were adopted and implemented, the recent evidence disclosed that the prevalence of wasting among children are still remain high [28].
In Ethiopia several studies has been conducted to assess the prevalence of wasting among under-two children and appeared in a fragment and inconclusive way ranging from 4.7% in Addis Ababa [29] to 17.5% in Somali region [30] respectively. In addition, the factors contributing to wasting also presented inconsistently in these studies [29, 31]. Therefore, the aim of this review was to determine the pooled national evidence of wasting among children during their window of opportunity and its associated factors. The finding of this study will help to address the national as well as international targets of reducing childhood wasting.
Methods
Prospero registration
The study protocol of this review was registered at the International Prospective Register of Systematic Reviews (PROSPERO) and can be accessed with a registration number of CRD42023414914.
Search strategy
The search was done comprehensively using electronic data bases like; Hinari, PubMed, Google scholar, Scopus and open Google. Unpublished works were also retrieved from research centers and university repositories. The search was conducted from June 19–22/2023. Reference lists of relevant papers were also searched to include any other potentially significant articles. The following keywords, search terms/MeSH headings were utilized to build a comprehensive search strategy which combined by Boolean operators “AND” “OR”:
“Prevalence“[Mesh] OR “magnitude” OR “proportion” OR “burden” OR “epidemiology” AND “Risk Factors“[Mesh] OR “predictors” OR “associated factors” OR “etiology” AND “severe acute malnutrition“[Mesh] OR “nutritional status“[Mesh] OR “acute malnutrition” OR “under nutrition” OR “acute under nutrition” AND “children 6–23 months” OR “under two years ” OR “infants and young child*”OR “children less than 2 years” OR” young child*”OR “children 6–24 months” AND Ethiopia (Table S1).
The authors were used the context; Population, Intervention, Comparison and Outcome (PICO) search format of prevalence studies to include all relevant papers.
Participants/populations: children aged less than two years and whose weight/height < -2Zscore.
Intervention/exposure group: under two years children with wasting.
Comparison/comparator: well-nourished children.
Outcome of interest: prevalence of wasting among children less than two years.
Inclusion and exclusion criteria
Cross-sectional and case control studies which report the prevalence and associated factors of wasting in under-two aged children were included. Papers with no full texts, case series, case reports, qualitative studies and articles published other than English languages were excluded. Only Cross-sectional studies were used to calculate pooled prevalence.
Measurement of outcome variables
The study has two main outcomes: The first is estimating the pooled prevalence of wasting among under-two children and the second to determine its associated factors. The pooled prevalence of wasting was determined using the adjusted odds ratios (AOR) reported from primary studies.
Study selection and quality assessment
All the relevant studies retrieved through electronic data base were reviewed independently by two reviewers (MA and BC). Version 8 Endnote software was used to exported, combined and removed duplicated studies. Full-text articles were downloaded using Endnote software and manually. AK and SZ assessed the quality of included studies using the Joanna Briggs Institute (JBI) quality assessment checklists for observational studies. Studies whose quality score is above 50% was considered as high quality. Based on this, all the included articles had 75% JBI quality assessments score (S2 checklist).
Data extraction and management
Data extraction is carried out from relevant studies by two authors independently (AK and MCA). The disparity between two authors was resolved through discussion and by the third author (MA). For each included articles; first author name, publication year, study region, study design, study setting, sample size, prevalence, associated factors effect size and standard error were extracted on Microsoft excel spread sheet.
Data analysis
After the data were extracted on Microsoft excel, exported to STATA version 17 software for analysis. The pooled estimate of wasting among under-two aged children and its associated factors were estimated by random effect model using DerSimonian-Laird model weight. The presence of heterogeneity between included studies was assessed using Cochrane Q-test and the I2 statistics. Sub-group analysis was done to adjust random variation in the presence of significant heterogeneity between primary studies. Moreover, the presence of publication bias was checked through graphical (funnel plot) and statistical (Egger’s) test.
Results
Study selection and identification
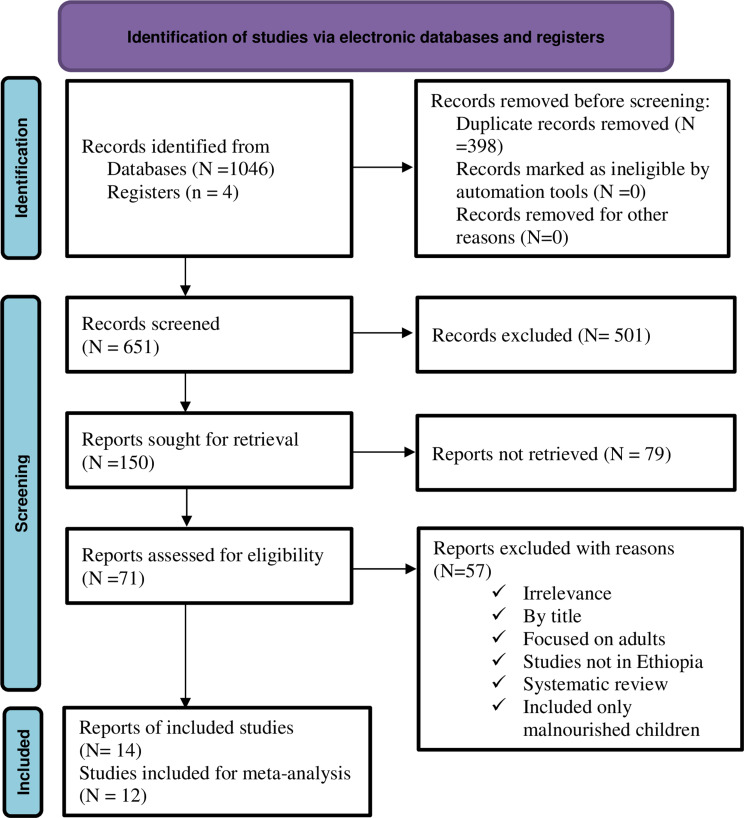
Of 1,050 total articles obtained from different electronic data bases, 398 duplicate studies were removed. And again 764 articles were removed as they are not relevant for this systematic review and meta-analysis. Reading the full title and abstract, 501 studies were excluding and after evaluating full text articles, 150 reports were retrieved. Again, 71 studies were assessed for eligibility. Finally, 14 studies were included for analysis after removal of 57 studies with reasons (Fig. 1).
Fig. 1.
PRISMA flow diagram of studies selection for systematic review and meta-analysis of the prevalence of wasting among under-two children its determinants in Ethiopia
Study characteristics
This review included the total sample of 7,815 participants where the smallest sample size from Amhara region (201) [20] and the largest is from EDHS (2146) [32]. The study has included articles published between 2013 and 2023. Twelve cross-sectional [29–40] and two case control [20, 41] studies were incorporated. Among these studies, five of them were conducted in Oromia region [35, 38–41], four in Amhara region [20, 33, 34, 38] and one study in Somali region (Table 1).
Table 1.
Characteristics of included studies and their prevalence of wasting among children age less than years in Ethiopia
| S.N | Author/year | Study region | Study design | Sample size | Events/cases | Prevalence | Study quality |
|---|---|---|---|---|---|---|---|
| 1. | Abate et al.,2016 [41] | Oromia | Case control | 288 | 143 | High | |
| 2. | Amera et al.,2019 [33] | Amhara | Cross-sectional | 431 | 35 | 8 | High |
| 3. | Derso et al.,2017 [34] | Amhara | Cross-sectional | 587 | 100 | 17 | High |
| 4. | Fekadu et al.,2015 [30] | Somalia | Cross-sectional | 214 | 37 | 17.5 | High |
| 5. | Forsido et al.,2021 [35] | Oromia | Cross-sectional | 558 | 57 | 9.7 | High |
| 6. | Geremariam et al.,2022 [20] | Amhara | Case control | 201 | 67 | High | |
| 7. | Sahiledengle et al., 2022 [32] | EDHS | Cross-sectional | 2146 | 167 | 7.8 | High |
| 8. | Sewnet et al.,2022 [36] | Amhara | Cross-sectional | 421 | 48 | 11.5 | High |
| 9. | Tadesse et al.,2017 [37] | SNNPRS | Cross-sectional | 645 | 64 | 9.9 | High |
| 10. | Tafese et al.,2020 [38] | Amhara &Oromia | Cross-sectional | 464 | 57 | 12.3 | High |
| 11. | Tafese et al.,2022 [31] | Oromia | Cross-sectional | 371 | 37 | 9.9 | High |
| 12. | Worku et al.,2021 [29] | A.A | Cross-sectional | 377 | 18 | 4.7 | High |
| 13. | Yazwe et al.,2021 [39] | Oromia | Cross-sectional | 500 | 59 | 11.8 | High |
| 14. | Yazwe et al.,2022 [40] | Oromia | Cross-sectional | 612 | 86 | 14.1 | High |
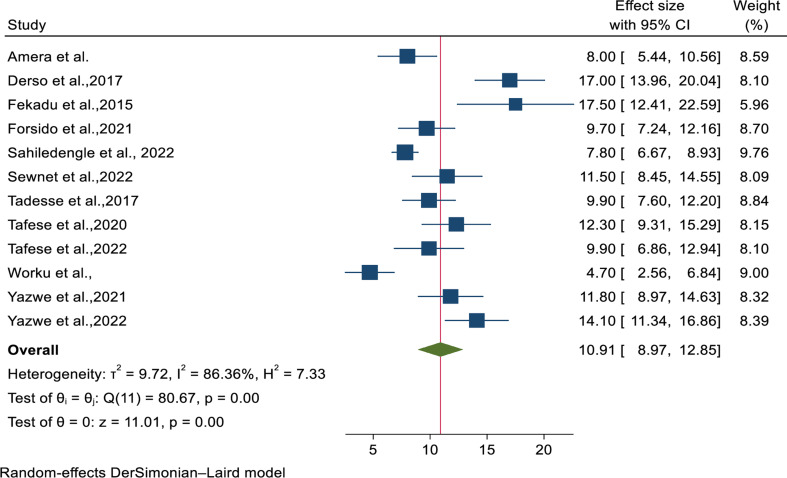
Prevalence of wasting among under-two years children in Ethiopia
Using random effects model, the pooled prevalence of wasting among under-two children was 10.91% (95% CI: 8.97–12.85). Significant heterogeneity was observed between studies (I2 = 86.36%, P-value < 0.001). Sahiledengle et al. [32]and Worku et al. [29] had the highest weight respectively and Fekadu et al. [30] has the lowest weight (Fig. 2).
Fig. 2.
Forest plot for pooled prevalence of wasting among under-two years children in Ethiopia
Small study effect
Publication bias was checked by using funnel plot and Egger’s statistical test. Accordingly, from visual inspection, there is symmetrical distribution of studies (Fig. S1). Egger’s statistical test also showed that there is absence of small study effect among studies (p-value = 0.9468).
Investigation of heterogeneity
This meta-analysis exhibited a considerable heterogeneity among studies from random effects model. Therefore, to identify the possible sources of heterogeneity, sensitivity and sub-group analysis were conducted.
Sensitivity analysis
Leave one out analysis was performed to investigate the influence of single study on the overall effect size estimate. Since the overall pooled estimate (10.91) is included within the confidence interval of all included studies, it is declared that there is no single study that significantly influences the overall effect size estimate (Fig. S2).
Sub-group analysis
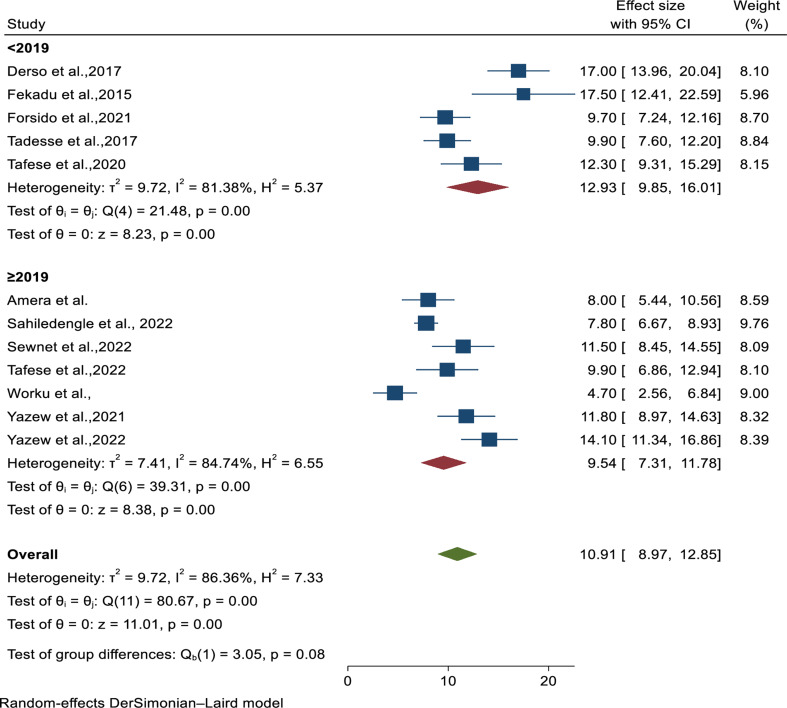
Sub-group analysis was done based on the study year, region, sample size and residence.
The pooled prevalence of wasting among under-two children was higher in studies conducted before 2019 (12.93%; 95%CI: 9.85–16.01, I2 = 81.38%, p < 0.001) as compared to studies done after 2019 (9.54%; 95%CI: 7.31–11.78, I2 = 84.74%, p < 0.001) (Fig. 3).
Fig. 3.
Subgroup analysis by study year for prevalence of wasting among under-two children in Ethiopia
From regional sub-group analysis, the highest prevalence of wasting among under-two children was observed in Amhara region (12.12%; 95%CI: 6.91–17.33; I2 = 89.86%, p < 0.001) followed by Oromia (11.36%; 95% CI: 9.33–13.40; I2 = 54.03%, p < 0.001) (Fig. S3).
The result of sub-group analysis by sample size showed that the prevalence of child wasting among studies with sample size < 600(11.14%; 95%CI: 8.54–13.75, I2 = 86.54%, p < 0.001) was higher than sample size greater than ≥ 600 (10.42%; 95%CI: 6.93–13.92, I2 = 88.89%, p < 0.001) (Fig. S4). Furthermore, the pooled estimate of wasting among under-two children was higher among studies performed in rural settings (11.88%; 95%CI: 9.60-13.99, I2 = 77.27%, p < 0.001) (Fig. S5).
Factors associated with wasting among under-two children in Ethiopia
As shown in Table 2, number of family size, wealth quartile, and maternal antenatal follow up, recent history of child illness and exclusive breast feeding until six months were significant factors of child wasting.
Table 2.
The pooled estimate of factors associated with wasting among under-two years children in Ethiopia
| Variables | Variables category | OR (95%CI) | Heterogeneity(I2,P-value) | Egger’s P-value | Total studies |
|---|---|---|---|---|---|
| Number of Family size | > 5 | 12.38(1.37–26.13) | I2 = 99.75, p < 0.001 | 0.001 | 3 |
| < 5 | 1 | ||||
| Maternal ANC follow up | No | 3.23(1.20–5.26) | I2 = 95.62, p < 0.001 | 0.389 | 2 |
| Yes | 1 | ||||
| Recent History of child illness | Yes | 2.58(1.78–3.37) | I2 = 90.86, p < 0.001 | 0.872 | 4 |
| No | 1 | ||||
| Exclusive breast feeding until 6 months | No | 5.30(1.17–9.43) | I2 = 98.71, p < 0.001 | 0.591 | 3 |
| Yes | 1 | ||||
| Wealth index of the family | Low | 3.91(1. 54-8.36) | I2 = 97.98, p < 0.001 | 2 | |
| Highest | 1 | 0.208 | |||
| Maternal education | No education | 1.51(0.97–2.05) | I2 = 83.19, p < 0.001 | 0.123 | 5 |
| Primary and above | 1 | ||||
| Age of the child | > 12month | 1.33(0.41–2.26) | I2 = 81.98, p < 0.001 | 0.026 | |
| < 12month | 1 | ||||
| Have latrine? | No | 1.59(0.39–3.56) | I2 = 0.0, p < 0.1155 | 0.126 | |
| Yes | 1 |
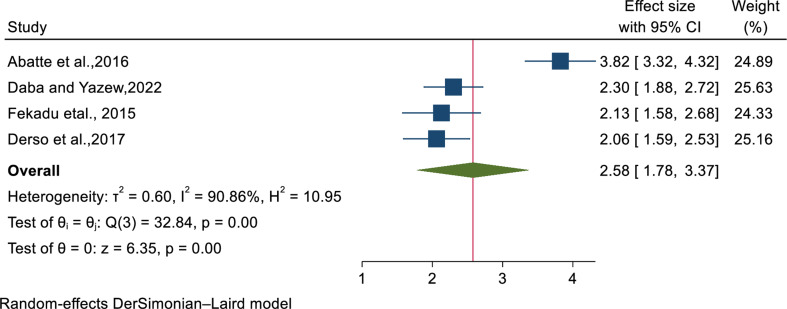
The relation between history of child illness and wasting was assessed by four studies [30, 34, 40, 41]. Children with recent history of illness were 2.58 times more likely to be wasted compared to their counterparts (OR; 2.58: 95%CI: 1.78–3.37) (Fig. 4).
Fig. 4.
Forest plot indicating the association between wasting and child illness
The pooled estimate of three studies [20, 31, 37] showed that children from family size greater than five were more likely to become wasting compared to with number of family size less than five(OR; 12.38: 95%CI:1.37–26.13). In meta-analysis of two studies [39, 40], children born from mothers with no antenatal follow up were 3.23 times more likely to develop wasting (OR; 3.23: 95%CI:1.20–5.26).
The pooled result of two [35, 40] studies revealed that low wealth status of the household has 3.9 time odds to develop childhood wasting as compared to highest wealth status(OR; 3.91: 95%CI:1.54–8.36). Exclusive breast feeding until six month has significant association to child wasting. Children who did not get exclusive breast feeding were 5.3 times odds to develop wasting than children who exclusive breast fed (OR; 5.30; 95%CI: 1.17–9.43) (Table 2).
Five studies [30–32, 34, 40] used to determine the association of maternal education status and childhood wasting. The pooled result depicted that there is no association between maternal educational status and wasting among children less than 2 years (OR; 1.51; 95%CI: 0.97–2.05).
The pooled results of three studies [32, 33, 36] showed that age of the child and wasting has no statistical association (OR; 1.33; 95%CI: 0.41–2.26). In addition, the association of child wasting and having latrine assessed in this study [20, 33, 41] and the result revealed that there is no statistical association between presence of latrine and childhood wasting (OR; 1.59: 95%CI; 0.39–3.56).
Discussion
Despite international and national unreserved interventions, wasting in children is still being continued with its devastating results particularly in under-two aged children.
Hence, the purpose of this review was to assess the pooled prevalence of wasting among under-two aged children during their window of opportunity and its associated factors.
The finding of this review disclosed that pooled prevalence of wasting among under-two children was 10.91% (95% CI: 8.97–12.85). This is similar with the studies done in Bangladesh and Uganda [42, 43], but the result is lower than the finding in Sohag Governorate, Nepal, Burkina Faso and India [44–47].The evidence from this review is also higher than the study conducted in China and Gahanna [48, 49]. This variability is justified by differences in study setting, socio-demographic and economic characteristics, time of study done and sample size. In addition, wasting in low income countries is more prevalent due to resource scarcity and poor delivery system [13].
Regarding sub-group analysis, the pooled prevalence of wasting among under-two children was higher among studies conducted before 2019 (12.93%) as compared to studies done after 2019(9.54%). This is because of Ethiopia is one of the countries who has been adapted and implemented sustainable development goal strategies to work on reducing childhood undernutrition [50] by 2030, though implementation of Seqota declaration [27] and national nutrition program [1]. Sub-group analysis based on the setting also showed that the pooled estimate of wasting among under-two children was higher among studies performed in rural settings (11.88%) as compared to children from urban settings (8.01%).This is in line with the study conducted in Sub-Saharan Africa [51] and in Papua New Guinea [52].This disparities might be due to maternal education status, access to safe drinking water and sanitation, limited access to professional education regarding to importance of optimal child feeding [53]. In contrast, the recent study of South Asia disclosed that children from urban settlement were more risk of being wasted than children from rural area [54]. Furthermore, from regional sub-group analysis, the highest prevalence of wasting among under-two children was observed in Amhara region (12.12%) followed by Oromia (11.36%).
Our review has shown that large number of family size (> five) has strong association with increasing childhood wasting. This is supported by previous studies in China [55], and Ethiopia [56]. As the number of family size increase within the household, the provision of adequate nutrition will be under question in resource limited settings due to financial constraints [57]. Other evidence from this review depicted that child with recent history of illness was associated with wasting as supported in other investigations ( [46, 58]. This is reasoned by illness such as pneumonia, diarrhea or other infections prone the children to loss of appetite and reduced the required amount of daily food intake, breast feeding and malabsorption which leads to wasting [59, 60]. In addition, undernutrion and infections are complex and bi-directional in nature that means; malnutrition cause infection by decreasing the immune system that fight against disease and infection also exposed the child for malnutrition/ wasting by experiencing decreased appetite, malabsorption, increasing nutrient requirements and compromised child nutritional status [61].
Children born from mothers with no antenatal follow up were more likely to develop wasting which is congruent with the previous studies [62, 63]. Antenatal care has great a contribution to have healthy and well-nourished children because the mothers would have a chance to get advice and counseling about the importance of both maternal and child nutrition during early life of child growth and development [63]. The study also revealed that poor wealth status of the family has 3.9 times odds of developing childhood wasting as compared to highest wealth status. This is in line with the previous studies [64–66]. Children from poor households primarily faced lack of fundamental daily nutrients which is basic for their growth and development. Most importantly, children from these families were prone for inadequate and insufficient food supply, inappropriate care, low living standard, unable to keep proper hygiene and sanitation, and also exposed for acute and chronic illness that [64, 67].
Moreover, our review disclosed that children who exclusively breast fed (EBF) were more odds to develop acute malnutrition/wasting than children who exclusive breast fed which is supported by the study conducted in Bangladesh and India [68, 69]. It is obvious that exclusively breast feeding of children until six months has tremendous impact on their normal growth and development due to its invaluable nutritional value and prevention of infection by scale upping the immunity system [70, 71]. Evidences showed that infants who EBF until six months were saved from diarrhea, pneumonia and other acute respiratory infections [68, 72, 73] which are the main cause of childhood undernutrition/wasting [74].
Study strength and limitations
This review is the first in kind that is conducted in Ethiopia and provided updated and conclusive evidence of childhood wasting and its determinants among children during window of opportunity. Sub-group analysis was attempted to minimize significant heterogeneity. Despite these strengths, the study has considerable limitations that the reader should appreciate. The review has significant heterogeneity and it included only quantitative studies. Articles written in languages other than English were also excluded.
Conclusion
This study disclosed that the pooled prevalence of wasting among under- two children were unexpectedly high in Ethiopia. Absence of maternal antenatal follow up, no exclusive breast feeding until six months, low wealth status of the households, large family size and current illness of the child were significant factors of wasting. Based on the finding, we recommended that strictly adherence of antenatal follow up, counsel the mother to feed only breast milk until six months. In addition, limit the number of family size to the level of the household income and early treatment of sick child before getting worse and cause severe acute malnutrition. Furthermore, scale up the wealth status and living standard of the family can alleviate the problem and address the agenda of reducing and eradicating all forms of malnutrition.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are grateful to acknowledge Bahir Dar University for allowing internet services to conduct this Review. We also extend our thanks to the authors of included articles in this systematic review and meta-analysis.
Abbreviations
- SDGs
Sustainable Development Goals
- EDHS
Ethiopia Demographic and Health Survey
- WHA
World Health Assembly
- USAID
United States Aid International Development
Author contributions
AK involved in conceptualization, data curation, investigation, supervision, software, resource allocation and methodology. SZ assessed the quality if included studies. DK played his role in data extraction and methodology. FDB, MCA, SZ, GA, TMA, BC, WNA, BB and MA played their role in critically revising the proposal, participated in its design, analyzed and interpreting the results and wrote the manuscript. All authors were involved in reading and approving the final manuscript.
Funding
This research did not receive any specific fund.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.FDRR. Federal democratic republic of ethiopia national nutrition program. 2016–20: Addis Ababa.
- 2.UNICEF. The state of the World’s children 2019-Growing well in a changing World. New York: UNICEF; 2019. [Google Scholar]
- 3.WHO. Levels and trends in child malnutrition: UNICEF. 2021.
- 4.WHO. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. 2019.
- 5.Magagi S, et al. Estimating the burden of wasting during COVID-19 based on empirical experiences in the Sahel. Field Exch. 2021;65:89. [Google Scholar]
- 6.Choudhary TS, et al. Severe wasting among Indian infants < 6 months: findings from the National Family Health Survey 4. Volume 15. Maternal & Child Nutrition; 2019. p. e12866. 4. [DOI] [PMC free article] [PubMed]
- 7.Cashin K, Oot L. A practical Tool for Program Planners, managers, and Implementers (Guide to Anthropometry). Washington, DC: Food and Nutrition Technical Assistance III Project (FANTA)/FHI; 2018. [Google Scholar]
- 8.System NLI. Country Profile Indicators: Interpretation Guide. 2010, WHO Geneva.
- 9.Ibrahim MK, et al. Impact of childhood malnutrition on host defense and infection. Clin Microbiol Rev. 2017;30(4):919–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ampaabeng SK, Tan CM. The long-term cognitive consequences of early childhood malnutrition: the case of famine in Ghana. J Health Econ. 2013;32(6):1013–27. [DOI] [PubMed] [Google Scholar]
- 11.Wali N, Agho KE, Renzaho AM. Wasting and associated factors among children under 5 years in five south Asian countries (2014–2018): analysis of demographic health surveys. Int J Environ Res Public Health. 2021;18(9):4578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.USAID. Wasting: A Growing Threat to Child Survival. Access date,November 18,2023]; https://www.advancingnutrition.org/spotlight/wasting
- 13.Karlsson O et al. Child wasting before and after age two years: a cross-sectional study of 94 countries. EClinicalMedicine. 2022;46. [DOI] [PMC free article] [PubMed]
- 14.Aboagye RG, et al. Dietary diversity and undernutrition in children aged 6–23 months in Sub-saharan Africa. Nutrients. 2021;13(10):3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.EPHI., Ethiopian Mini Demographic and Health Survey. 2019: Addis Ababa, Ethiopia.
- 16.Mya KS, Kyaw AT, Tun T. Feeding practices and nutritional status of children age 6–23 months in Myanmar: a secondary analysis of the 2015-16 demographic and Health Survey. PLoS ONE. 2019;14(1):e0209044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karakochuk CD, et al. The biology of the first 1,000 days. Taylor & Francis; 2018.
- 18.Martorell R. Improved nutrition in the first 1000 days and adult human capital and health. Am J Hum Biology. 2017;29(2):e22952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mertens A et al. Child wasting and concurrent stunting in low-and middle-income countries. Nature, 2023: pp. 1–10. [DOI] [PMC free article] [PubMed]
- 20.Gebremaryam T, et al. Determinants of severe acute malnutrition among children aged 6–23 months in bahir dar city public hospitals, Northwest Ethiopia, 2020: a case control study. BMC Pediatr. 2022;22(1):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma AK, Das G. Infant and maternal risk factors of severe acute malnutrition under 6 months of age. Indian J Child Health, 2020: pp. 454–8.
- 22.Mbogori T, Muriuki J. Demographic and social-economic determinants of malnutrition among children (0–23 months old) in Kenya. Int J. 2021;10(3):81. [Google Scholar]
- 23.Ahmed AT et al. Determinants of Severe Acute Malnutrition Among Children 6–36 Months in Kalafo District, Riverine Context, Ethiopia. Unmatched Case Control With Qualitative Study. 2020.
- 24.FAO. The Sustainable Development Goals,. 2015. Access date,Novevemer 20, 2023]; https://www.fao.org/3/CA3121EN/ca3121en.pdf
- 25.WHO. Global Action Plan for Child Wasting: A framework for action to accelerate progress in preventing and managing child wasting and the achievement of the Sustainable Development Goals, 2020. https://www.who.int/publications/m/item/global-action-plan-on-child-wasting-a-framework-for-action
- 26.USAID. The USAID Multi-Sectoral Nutrition Strategy, 2014–2025. https://www.usaid.gov/sites/default/files/2022-05/USAID_Nutrition_Strategy_5-09_508.pdf
- 27.FDRE. The ‘Seqota’ Declaration implementation plan(2016–2030),2016.
- 28.WHO. Global nutrition targets 2025: policy brief series. https://www.who.int/publications/i/item/WHO-NMH-NHD-14.2
- 29.Worku L et al. Under nutrition and Associated factors among infants and young children age 6–23 months attending Minilik II Hospital, Ethiopia, 2021. 2021.
- 30.Fekadu Y, et al. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: a cross-sectional study. BMC Public Health. 2015;15(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tafese Z, et al. Child undernutrition and associated factors among children 6–23 months old in largely food insecure areas of rural Ethiopia. J Nutritional Sci. 2022;11:e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sahiledengle B, et al. Determinants of undernutrition among young children in Ethiopia. Sci Rep. 2022;12(1):20945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amera MG et al. Magnitude of Undernutrition and Associated Factors among Infants and Young Children aged 6–23 Months in Sinan district, Northwest Ethiopia Amhara regional state: A crossectional study. 2021.
- 34.Derso T, et al. Stunting, wasting and associated factors among children aged 6–24 months in Dabat health and demographic surveillance system site: a community based cross-sectional study in Ethiopia. BMC Pediatr. 2017;17(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forsido SF et al. Undernutrition and associated factors among children under 2 years of age in Jimma Zone, Southwest Ethiopia. J Public Health, 2021: pp. 1–9.
- 36.Sewenet T, et al. Undernutrition and associated factors among children aged 6–23 months in Dessie Town, Northeastern Ethiopia, 2021: a community based cross-sectional study. Front Pead. 2022;10:916726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tadesse A, Hailu D, Bosha T. Nutritional status and associated factors among pastoralist children aged 6–23 months in Benna Tsemay Woreda, South Omo Zone, Southern Ethiopia. Int J Nutr Food Sci. 2018;7(1):11–23. [Google Scholar]
- 38.Tafese Z, et al. Child feeding practice and primary health care as major correlates of stunting and underweight among 6-to 23-month-old infants and young children in food-insecure households in Ethiopia. Curr Developments Nutr. 2020;4(9):nzaa137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yazew T, Bekele G, Determinants of undernutrition among infants. and young children in jima geneti district, western oromia, ethiopia. Asian J Adv Res, 2021: pp. 825–35.
- 40.Yazew T, Daba A. Associated Factors of Wasting among Infants and Young Children (IYC) in Kuyu District, Northern Oromia, Ethiopia. BioMed Research International, 2022. 2022. [DOI] [PMC free article] [PubMed]
- 41.Abate A, et al. Predictors of acute malnutrition among 6–23 months children in Hidhebu Abote Woreda, Oromia, Ethiopia. J Heal Med Dev. 2016;24:119–29. [Google Scholar]
- 42.Chowdhury TR et al. Factors associated with stunting and wasting in children under 2 years in Bangladesh. Heliyon, 2020;6(9). [DOI] [PMC free article] [PubMed]
- 43.Mokori A. Nutritional status, complementary feeding practices and feasible strategies to promote nutrition in returnee children aged 6–23 months in northern Uganda. South Afr J Clin Nutr. 2012;25(4):173–9. [Google Scholar]
- 44.Shaban AN, et al. Prevalence of Nutritional Stunting and its Associated factors among children under two years at Sohag Governorate. Assiut Sci Nurs J. 2022;10(28):53–65. [Google Scholar]
- 45.Sah AK et al. Prevalence and associated factors of stunting, underweight and wasting among children aged 6–23 months in Dalit and Non-dalit: a cross sectional comparative study of Dhanusha district. Nepal. 2020.
- 46.Paré BC et al. Prevalence of wasting and associated factors among 6 to 23 months old children in the Sahel Region of Burkina Faso. Pan Afr Med J, 2019;34(1). [DOI] [PMC free article] [PubMed]
- 47.Saha J, et al. Effects of Dietary Diversity on Growth outcomes of Children aged 6 to 23 months in India: evidence from National Family and Health Survey. Nutrients. 2022;15(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu J, et al. Prevalence of malnutrition and associated factors of stunting among 6–23-month-old infants in Central Rural China in 2019. Int J Environ Res Public Health. 2021;18(15):8165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suara S, Aryee P. Growth faltering and inadequate dietary intake among children (6–23 months old) in Sissala East District, Ghana. UDS Int J Dev. 2018;5(1):75–87. [Google Scholar]
- 50.Worku T, et al. Sustainable under nutrition reduction program and dietary diversity among children’s aged 6–23 months, Northwest Ethiopia: comparative cross-sectional study. Int J Equity Health. 2020;19(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takele BA, Gezie LD, Alamneh TS. Pooled prevalence of stunting and associated factors among children aged 6–59 months in Sub-saharan Africa countries: a bayesian multilevel approach. PLoS ONE. 2022;17(10):e0275889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pham BN, et al. Measuring wasting and stunting prevalence among children under 5 years of age and associated risk factors in Papua New Guinea: new evidence from the Comprehensive Health and Epidemiological Surveillance System. Front Nutr. 2021;8:622660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shankar B, Zanello G, Srinivasan CS. Rural-urban disparities in child nutrition in Bangladesh and Nepal. 2013. [DOI] [PMC free article] [PubMed]
- 54.Mutunga M, et al. The forgotten agenda of wasting in Southeast Asia: Burden, determinants and overlap with stunting: a review of nationally representative cross-sectional demographic and health surveys in six countries. Nutrients. 2020;12(2):559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li H, et al. Prevalence and associated factors for stunting, underweight and wasting among children under 6 years of age in rural Hunan Province, China: a community-based cross-sectional study. BMC Public Health. 2022;22(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tekile AK, Woya AA, Basha GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and Health Survey. BMC Res Notes. 2019;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gilano G, et al. Understanding child wasting in Ethiopia: cross-sectional analysis of 2019 Ethiopian demographic and Health Survey Data using generalized Linear latent and mixed models. JMIR Public Health Surveillance. 2023;9:e39744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tufa EG, et al. Magnitude of wasting and underweight among children 6–59 months of age in Sodo Zuria District, South Ethiopia: a community based cross-sectional study. BMC Res Notes. 2018;11(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lazzaroni S, Wagner N. Misfortunes never come singly structural change, multiple shocks and child malnutrition in rural Senegal Journal. 2016. [DOI] [PubMed]
- 60.Schlaudecker EP, Steinhoff MC, Moore SR. Interactions of diarrhea, pneumonia, and malnutrition in childhood: recent evidence from developing countries. Curr Opin Infect Dis. 2011;24(5):496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. 2018;31(3):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ramirez N, et al. Child malnutrition and antenatal care: evidence from three latin American countries. ISS Working Paper Series/General Ser. 2012;536(536):1–28. [Google Scholar]
- 63.Tette EM, Sifah EK, Nartey ET. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr. 2015;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aheto JMK, et al. Childhood Malnutrition and its determinants among under-five children in G hana. Paediatr Perinat Epidemiol. 2015;29(6):552–61. [DOI] [PubMed] [Google Scholar]
- 65.Harding KL, Aguayo VM, Webb P. Factors associated with wasting among children under five years old in South Asia: implications for action. PLoS ONE. 2018;13(7):e0198749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6–59 months of age in pastoral community of Dollo Ado District, Somali region, Ethiopia. Sci J Public Health. 2013;1(4):175–83. [Google Scholar]
- 67.Akombi BJ, et al. Stunting, wasting and underweight in sub-saharan Africa: a systematic review. Int J Environ Res Public Health. 2017;14(8):863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Khan MN, Islam MM. Effect of exclusive breastfeeding on selected adverse health and nutritional outcomes: a nationally representative study. BMC Public Health. 2017;17:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kumar A, Singh V. A study of exclusive breastfeeding and its impact on nutritional status of child in EAG States. J Stat Appl Probab. 2015;4(3):435. [Google Scholar]
- 70.Black RE, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. [DOI] [PubMed] [Google Scholar]
- 71.Horta B, Victora C. Short-term effects of breastfeeding: a systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality. Geneva: World Health Organization; 2013. apps. who. http://int/iris/bitstream/10665/95585/1/9789241506120_eng.pdf, 2017.
- 72.Ladomenou F, et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child. 2010;95(12):1004–8. [DOI] [PubMed] [Google Scholar]
- 73.Raheem RA, Binns CW, Chih HJ. Protective effects of breastfeeding against acute respiratory tract infections and diarrhoea: findings of a cohort study. J Paediatr Child Health. 2017;53(3):271–6. [DOI] [PubMed] [Google Scholar]
- 74.Gwela A, et al. Undernutrition, host immunity and vulnerability to infection among young children. Pediatr Infect Dis J. 2019;38(8):e175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.