Abstract
We present the case of a 26-year old woman who developed obstructive jaundice and massive abdominal swelling. Investigations revealed a huge choledochal cyst with obstructive pattern of hyperbilirubinaemia. She had exploratory laparotomy, drainage and excision of the choledochal cyst and Roux-en-Y hepaticojejunostomy. She has been followed up for 6 months in good clinical condition.
Keywords: Adult, choledochal cyst, Nigeria
Introduction
Choledochal cyst is a congenital disorder characterized by cystic dilatation of parts or all of the biliary tree [Table 1]. It is an uncommon condition with incidence ranging from 1 in 1000 to 1 in 150,000 live births[1,2] The true incidence in Nigeria is not known even though several hospital-based cohorts have been reported.[3,4,5] While choledochal cysts are most commonly diagnosed in childhood, reports of presentation in adults have been documented.[6,7,8] The majority of diagnoses in adults were made in asymptomatic patients being investigated for other abdominal conditions[8]
Table 1.
Todani and Alonso-Lej’s classification of choledochal cyst
| Type I | Dilation of extrahepatic biliary duct. |
| Type II | Diverticular dilation of the extrahepatic duct. |
| Type III | Cystic dilation of the intraduodenal part of the common bile duct. |
| Type IVa | Extrahepatic and intrahepatic dilation of bile ducts. |
| Type IVb | Dilation of many portions extrahepatic biliary duct. |
| Type V | Limited dilation of intrahepatic ducts (Caroli disease). |
We present a rare case of a 26-year-old female who developed obstructive jaundice due to a huge choledochal cyst
Case Presentation
The patient is a 26-year-old woman who has had recurrent upper abdominal pain for about 5 years. She developed jaundice, pale stools, generalized pruritus, and upper abdominal swelling a year before presentation. The progressive upper abdominal distention was associated with recurrent vomiting, easy fullness, and progressive weight loss. Initial intermittent jaundice then became progressive. Clinical examination revealed deep jaundice, pallor, and a hugely distended abdomen with more prominence in the upper abdomen.
Laboratory reports revealed deranged liver function tests with markedly elevated serum total and conjugated bilirubin. hypoalbuminemia, elevated alkaline phosphatase, and gamma glutaryl transferase. She also had hypokalemia, hypomagnesemia, deranged clothing profile with an international normalized ratio of 1.5 and her packed cell volume was 27%.
An abdominal ultrasound scan showed huge intra-abdominal cystic masses, which were fairly circumscribed and thick-walled with fine internal echoes extending from the right hypochondriac region to the epigastric region. The gallbladder was markedly distended, with gross dilatation of intrahepatic ducts. The cystic dilatation did not allow for visualization of the extrahepatic biliary tree and the pancreas.
Computer tomography (CT) showed a giant cystic fusiform dilatation of the entire common bile duct, reaching 197 × 137 × 134 mm with fusiform dilatation of the common hepatic duct (CHD) and intrahepatic ducts. The right and left CHD measured 37 and 23 mm, respectively, with a dilated gallbladder, and the finding was consistent with a choledochal cyst (Todani Type IVa) as depicted in Figures 1 and 2.
Figure 1.
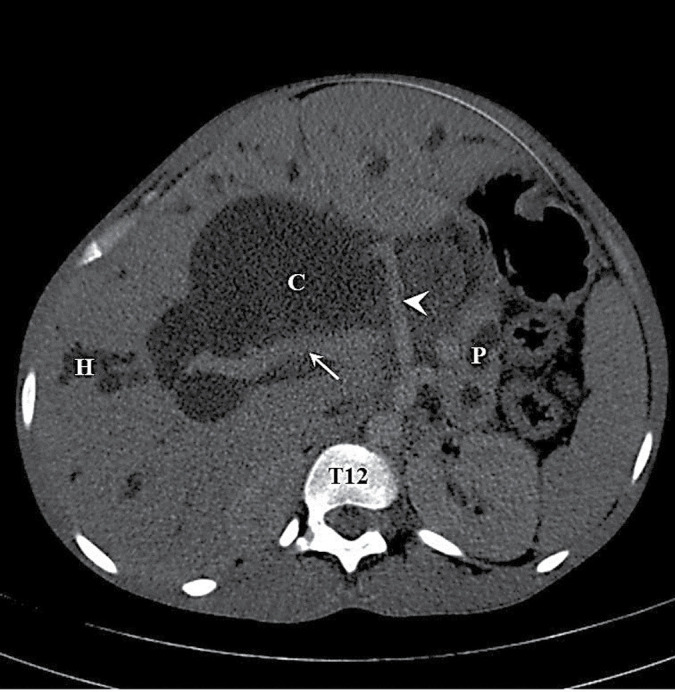
Axial IV-contrast enhanced computed tomographic image of the patient (portal venous phase) at the porta hepatis showing hepatomegaly with dilated intrahepatic ducts (H) and cystic fusiform dilatation of the common bile duct (C). The portal vein (arrow), main hepatic artery (arrow head), and pancreatic body with its dilated main pancreatic duct (P) are also noted
Figure 2.
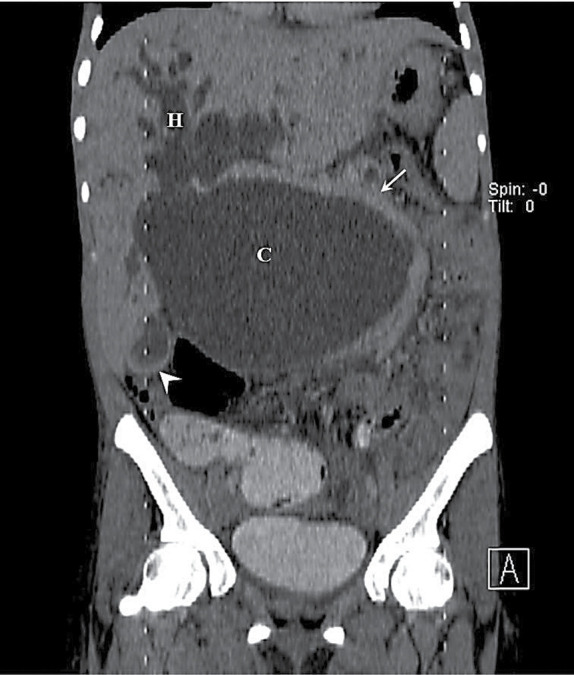
Coronal reformatted image of IV-contrast abdominopelvic computed tomography scan of the patient (portal venous phase) showing hepatomegaly with dilated intrahepatic ducts (H) and cystic fusiform dilatation of the entire common bile duct (C) consistent with Todani type IVa choledochal cyst. The portal vein (arrow) is bowed laterally while the dilated gall bladder neck (arrow head) is also noted
The patient was worked up for surgery. She had six units of fresh frozen plasma and a pint of fresh whole blood to correct anemia and clotting derangement. Serum potassium and hypoalbuminemia were also corrected. She had a laparotomy during which exploration showed hepatomegaly with biliary cirrhosis. The common bile duct was grossly dilated, thick-walled, and filled with about 3 L of altered bile [Figure 3]. Its wall has a pseudocyst, which projected into the lesser sac, extended up to and displaced the stomach and spleen superior-laterally. The gallbladder was markedly distended and the cystic duct was also dilated. There was moderate ascites.
Figure 3.
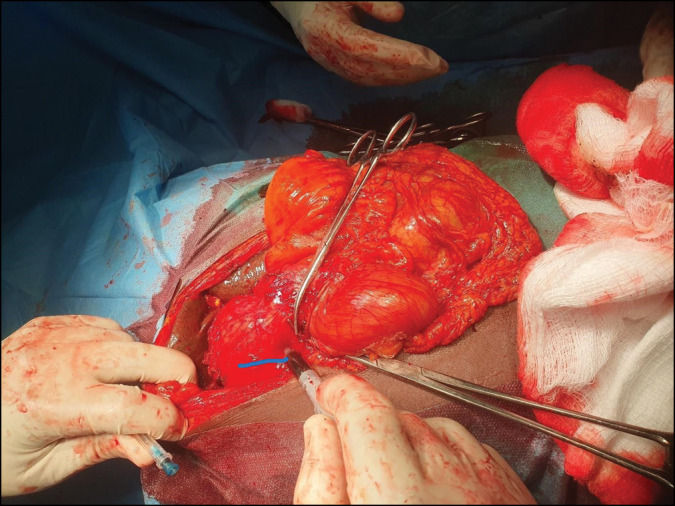
Intra-operative picture showing grossly dilated common bile duct with bile aspirate noted in the syringe (arrow)
Cholecystectomy was done and the choledochal cyst was incised and its content drained. Its thick wall was excised up to the CHD [Figure 4]. A Roux-en-Y hepaticojejunostomy was performed and the abdomen was irrigated and closed in layers after inserting a subhepatic drain. Postoperatively, the patient developed a bile leak that lasted for 10 days. An abdominopelvic ultrasound confirmed no residual collection and the drain was removed. Serum total and conjugated bilirubin reduced drastically from preoperative levels of 390 and 320 to 62 and 43 mmol/L, respectively. She gained 5 kg in weight 2 weeks after the operation. She has been followed up for more than 3 months in conjunction with the gastroenterologists.
Figure 4.
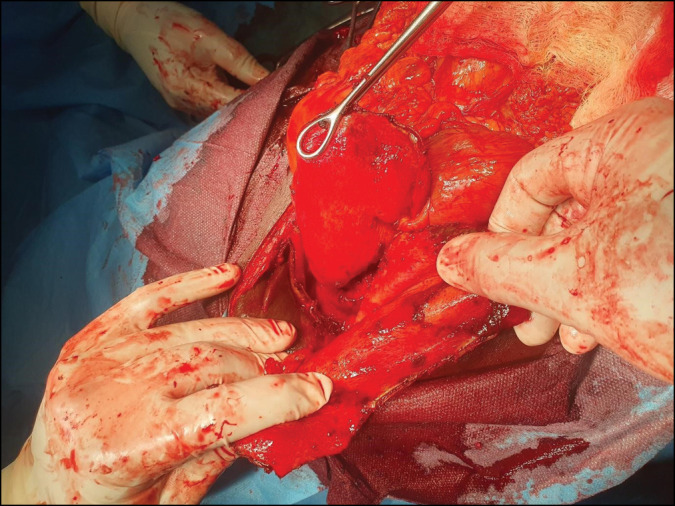
The thick wall of the choledochal cyst grabbed in forceps before excision
Discussion
The presentation of choledochal cysts in adults is very rare in Nigeria. A search of PubMed using the term “choledochal cyst, adult, Nigeria” yielded only two articles, a case report[4] and a review article citing a case series of three patients published a decade earlier.[3] It is however possible that several such cases are not diagnosed, and may be misdiagnosed or treated without being reported. The case we have illustrated also happened to have managed mild upper abdominal symptoms since childhood with presentations in different healthcare facilities where first aid treatments were offered without investigations or definitive diagnosis of the cause of the symptoms.
Choledochal cysts in adults have varied presentations. A review of an international multi-institutional database reported that the majority of adult patients will present with abdominal pain of varying severity with only a small fraction presenting with jaundice.[9] The index patient has had different investigations for obstructive jaundice which she developed a year before presentation. Unfortunately, the huge size of the choledochal cyst and the age of the patient did not aid diagnosis on initial ultrasonography done at the referring hospital until a CT scan was ordered and a radiologist review reported the findings. This suggests that though rare, a high index of suspicion of choledochal cyst will be helpful in diagnosis when a long-standing history of upper abdominal symptoms exists.
It has been reported that nearly half of the adult cases of choledochal cysts occur on a background of biliary tract malignancy with nearly half of those cases occurring in those who have had internal drainage of choledochal cysts.[4,10] Our patient’s presentation with profound weight loss and anorexia alongside huge abdominal distension and jaundice heightened this suspicion despite her young age. This was further heightened by the initial ultrasound report of ascites. We bore this in mind until the clear findings at the operation where no gross features of malignancies were seen. Histopathology confirmed that this was a benign condition buttressing the fact that delay in presentation and delay in diagnosis at the peripheral hospitals complicated the pattern of presentation as well as the treatment.
The commonest modality of surgical treatment of Type 4a choledochal cysts is complete cyst excision and hepaticojejunostomy. This was successfully carried out in our patient with a very good clinical outcome. We are keen on her long-term outcome and she has also been adherent to follow-up. We believe her case can be projected to encourage early detection, presentation, and treatment.
In conclusion, choledochal cysts rarely occur in adults in Nigeria, however long-standing obstructive jaundice in young adults should raise a suspicion. Following radiological diagnosis, surgical treatment is attended by a good outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bhavsar MS, Vora HB, Giriyappa VH. Choledochal cysts: A review of the literature. Saudi J Gastroenterol. 2012;18:230–6. doi: 10.4103/1319-3767.98425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Gendi AM, El-Gendi A, El-Shafei M, Bedewy E. Choledochal cysts in adults: The clinicopathological features and surgical outcomes in a single institute. Kasr El Aini J Surg. 2019;20:65–75. [Google Scholar]
- 3.Akinyinka OO, Falade AG, Akinbami FO, Alli T, Atalabi M, Irabor D, et al. Choledochal cysts in African infants: A report of 3 cases and a review of the literature. Trop Gastroenterol. 2005;26:34–6. [PubMed] [Google Scholar]
- 4.Alatise OI, Oke OA, Adesunkanmi AK, Olaofe OO, Asaleye CM. Management of adult choledochal cyst coexisting with gallbladder carcinoma: A case report and review of literature. Niger J Surg. 2016;22:43–7. doi: 10.4103/1117-6806.169870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gall BM, Madziga AG, Hamid AU. Choledochal cyst: A case report and review of literature. Niger J Med. 2004;13:295–9. [PubMed] [Google Scholar]
- 6.Sallahu F, Hasani A, Limani D, Shabani S, Beka F, Zatriqi S, et al. Choledochal cyst—Presentation and treatment in an adult. Acta Inform Med. 2013;21:138–9. doi: 10.5455/aim.2013.21.138-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao J, Chen M, Hong T, Qu Q, Li B, Liu W, et al. Surgical management and prognosis of congenital choledochal cysts in adults: A single Asian center cohort of 69 cases. J Oncol. 2022;2022:9930710. doi: 10.1155/2022/9930710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gong L, Qu Q, Xiang X, Wang J. Clinical analysis of 221 cases of adult choledochal cysts. Am Surg. 2012;78:414–8. [PubMed] [Google Scholar]
- 9.Soares KC, Kim Y, Spolverato G, Maithel S, Bauer TW, Marques H, et al. Presentation and clinical outcomes of choledochal cysts in children and adults: A multi-institutional analysis. JAMA Surg. 2015;150:577–84. doi: 10.1001/jamasurg.2015.0226. [DOI] [PubMed] [Google Scholar]
- 10.Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: Presentation, clinical differentiation, and management. J Am Coll Surg. 2014;219:1167–80. doi: 10.1016/j.jamcollsurg.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]


