Abstract
The UNAIDS 95-95-95 targets are an important metric for guiding national HIV programs and measuring progress towards ending the HIV epidemic as a public health threat by 2030. Nevertheless, as proportional targets, the outcome of reaching the 95-95-95 targets will vary greatly across, and within, countries owing to the geographic diversity of the HIV epidemic. Countries and subnational units with a higher initial prevalence and number of people living with HIV (PLHIV) will remain with a larger number and higher prevalence of virally unsuppressed PLHIV—persons who may experience excess morbidity and mortality and can transmit the virus to others. Reliance on achievement of uniform proportional targets as a measure of program success can potentially mislead resource allocation and progress towards equitable epidemic control. More granular surveillance information on the HIV epidemic is required to effectively calibrate strategies and intensity of HIV programs across geographies and address current and projected health disparities that may undermine efforts to reach and sustain HIV epidemic control even after the 95 targets are achieved.
Introduction
In 2014 the Joint United Nations Programme on HIV/AIDS (UNAIDS) rolled out the “Fast-Track” strategy to end the AIDS epidemic by 2030 [1, 2]. Since then, 144 countries adopted the ambitious Fast-Track treatment targets, aiming that by 2020, 90% of people living with HIV know their HIV status, 90% of those who know their status are on antiretroviral treatment (ART), and 90% of those on ART achieve viral load suppression (i.e. the 90-90-90 targets); and further, by 2025, aiming to achieve the even more ambitious 95-95-95 targets (95% of people living with HIV know their status, 95% with known status on ART, 95% on ART virally suppressed). The latter targets equate to 85.7% of all PLHIV being on ART and virally suppressed.
With an estimated 20.6 million people living with HIV (PLHIV), the 21 countries in Eastern and Southern Africa (ESA) accounted for over 80% of PLHIV on the continent, 54% of all PLHIV, and 45% (670,000) of new HIV infections worldwide in 2021 [3]. Overall, in 2021, 90% of PLHIV in the region knew their status, 78% of all PLHIV were on ART and 73% of all PLHIV had suppressed viral load [3]. Six ESA countries achieved the 90-90-90 targets by 2020, with several having also met, or made substantial progress towards, the second and third 95 targets and epidemic control [4]. As countries strive to reach or sustain the 95-95-95 targets with international aid decreasing [4] and national health budgets stretched to meet competing demands, addressing gaps in health equity and equality has emerged among the highest priorities of the global HIV response [4–6].
Whereas the need to address health inequity among specific populations (e.g., adolescent girls and young women, children, female sex workers, men who have sex with men, and persons who inject drugs) has featured strongly in global guidance for HIV programs, the need to address health inequities among geographically defined subpopulations with high burden of HIV has received less attention [6, 7]. We used published estimates of the number of adult (aged 15 years and above) PLHIV in the Eastern and Southern Africa region to assess the absolute number and population-prevalence of people living with HIV who are expected to remain virally unsuppressed (not on ART, or on ART but not virally suppressed [viral load >1,000 copies/ml]) regionally and nationally after reaching the 95-95-95 targets. We further explored the expected outcome of reaching the 95-95-95 targets at sub-national levels in two country case studies, Kenya, and South Africa.
Methods
National and subnational data on the estimated number of PLHIV aged 15 years and above in 2022 were obtained from published UNAIDS modeled estimates [8, 9]. Population data on persons aged 15 years and above were obtained from published population estimates and projections [10] (S1 Table). We summed the overall number of PLHIV expected to be missed along each step of the 95-95-95 cascade to estimate the total number of virally unsuppressed PLHIV expected to remain in each country after meeting all three of the 95 targets. We then calculated the estimated prevalence of virally unsuppressed PLHV (viral load > 1,000 copies/ml); subsequently referred to as the “prevalence of virally unsuppressed PLHIV” expected to remain after reaching the 95-95-95 targets among the population of persons potentially susceptible to HIV infection. The population susceptible to HIV infection (i.e. HIV-negative population) was calculated by subtracting the total estimated number of PLHIV aged 15+ years from the total population aged 15+ years. We applied the same methodology to further calculate the number and prevalence of virally unsuppressed PLHIV at subnational levels in Kenya and South Africa using publicly available subnational HIV estimates and census data. Calculations were done using R version 4.3.0 [11]. Maps showing spatial variation in results among and within countries were generated using ArcGIS Enterprise version 10.6.1. This project was reviewed in accordance with CDC human research protection procedures and was determined to be non-research.
Results
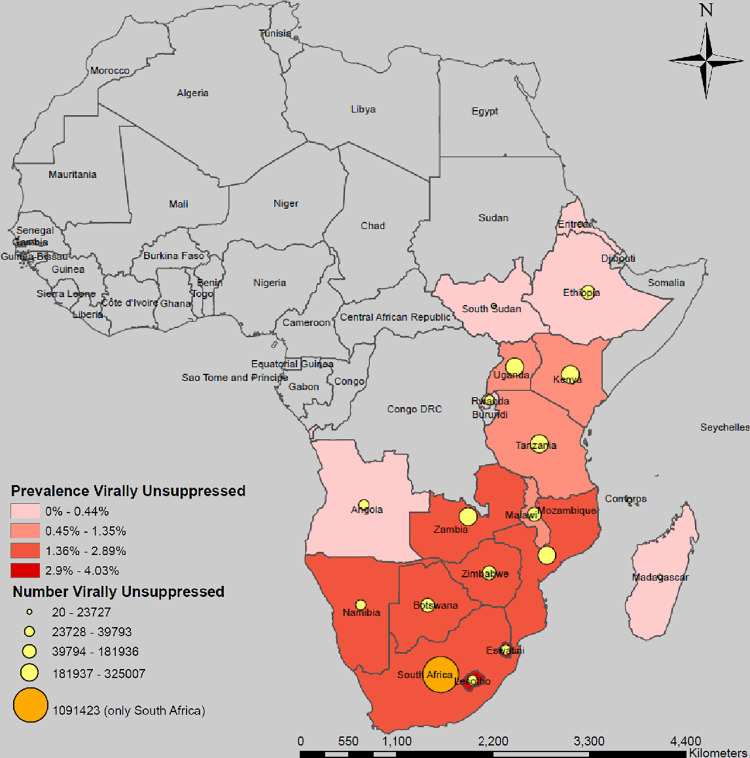
Among the 21 countries included, 20 had national, and 15 had subnational estimates of PLHIV available. The number of virally unsuppressed PLHIV aged 15 years and above expected to remain after reaching all three 95 targets in the ESA region is 2,869,865 ranging from less than 2,000 in Comoros, Eritrea, and Mauritius to over 1.09 million in South Africa (Fig 1, Table 1). After reaching the 95-95-95 targets, eight countries are expected to remain with more than 100,000 virally unsuppressed PLHIV. The projected regional prevalence of virally unsuppressed PLHIV is 0.94%, and highest in Eswatini (4.03%), Lesotho (3.08%), South Africa (2.89%) and Botswana (2.87%).
Fig 1. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by country, Eastern and Southern Africa Region.
Maps were created using a licensed ArcGIS by ESRI version 10.6.1 GIS Mapping Software, Location Intelligence & Spatial Analytics | Esri; Base map from: Office of the Geographer and Global Issues, U.S. Department of State. https://catalog.data.gov/dataset/large-scale-international-boundaries; June 14, 2024.
Table 1. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by country, Eastern and Southern Africa Region.
| After reaching 1st 95 | After reaching 2nd 95 | After reaching 3rd 95 | After reaching all 95-95-95 targets | |||||
|---|---|---|---|---|---|---|---|---|
| Estimated number of PLHIV aged 15+ years | National prevalence of HIV, age 15+ years | Remain un-diagnosed | Know HIV status but not on ART | On ART but not virally suppressed | Total no. of virally non-suppressed PLHIV | Population denominator* | Prevalence virally non-suppressed PLHIV | |
| Angola | 278,549 | 1.42% | 13,927 | 13,231 | 12,570 | 39,728 | 19,574,219 | 0.20% |
| Botswana | 345,055 | 19.58% | 17,253 | 16,390 | 15,571 | 49,213 | 1,713,277 | 2.87% |
| Comoros | 140 | 0% | 7 | 7 | 6 | 20 | 506,880 | 0.00% |
| Eritrea | 12,000 | 0.60% | 600 | 570 | 542 | 1,712 | 2,169,680 | 0.08% |
| Eswatini | 216,083 | 27.17% | 10,804 | 10,264 | 9,751 | 30,819 | 764,458 | 4.03% |
| Ethiopia | 573,538 | 0.91% | 28,677 | 27,243 | 25,881 | 81,801 | 63,266,546 | 0.13% |
| Kenya | 1,309,914 | 4.14% | 65,496 | 62,221 | 59,110 | 186,826 | 31,447,763 | 0.59% |
| Lesotho | 266,871 | 20.98% | 13,344 | 12,676 | 12,043 | 38,062 | 1,233,981 | 3.08% |
| Madagascar | 57,000 | 0.30% | 2,850 | 2,708 | 2,572 | 8,130 | 17,473,980 | 0.05% |
| Malawi | 949,975 | 7.98% | 47,499 | 45,124 | 42,868 | 135,490 | 11,769,331 | 1.15% |
| Mauritius | 12,000 | 1.10% | 600 | 570 | 542 | 1,712 | 1,072,680 | 0.16% |
| Mozambique | 2,278,754 | 12.14% | 113,938 | 108,241 | 102,829 | 325,007 | 18,450,997 | 1.76% |
| Namibia | 208,155 | 12.62% | 10,408 | 9,887 | 9,393 | 29,688 | 1,619,880 | 1.83% |
| Rwanda | 228,772 | 2.80% | 11,439 | 10,867 | 10,323 | 32,629 | 8,132,303 | 0.40% |
| South Africa | 7,652,395 | 17.40% | 382,620 | 363,489 | 345,314 | 1,091,423 | 37,755,782 | 2.89% |
| South Sudan | 1,632,461 | 2.00% | 8,318 | 7,902 | 7,507 | 23,727 | 7,132,561 | 0.33% |
| Tanzania | 1,352,968 | 4.71% | 81,623 | 77,542 | 73,665 | 232,830 | 34,462,677 | 0.68% |
| Uganda | 1,344,900 | 5.51% | 67,648 | 64,266 | 61,053 | 192,967 | 24,340,286 | 0.79% |
| Zambia | 1,235,851 | 12.00% | 67,245 | 63,883 | 60,689 | 191,816 | 11,020,044 | 1.74% |
| Zimbabwe | 1,632,461 | 12.08% | 61,793 | 58,703 | 55,768 | 176,263 | 10,050,707 | 1.75% |
| Eastern and Southern Africa | 19,955,382 | 1,006,087 | 955,784 | 907,994 | 2,869,865 | 303,958,032 | 0.94% | |
*Population denominator = Sum of total susceptible (HIV-negative) population aged 15+ years and the total number of PLHIV aged 15+ years who remain virally unsuppressed after reaching the 95-95-95 targets.
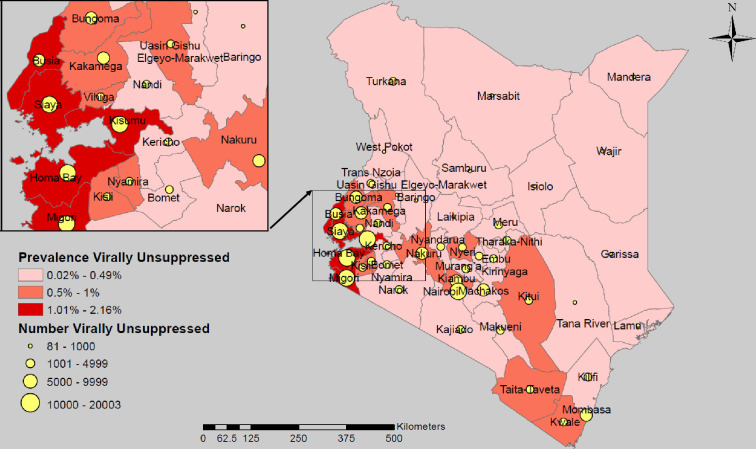
The implications of national achievement of the 95 targets differ greatly at subnational level. In Kenya, the projected outcome of meeting the 95-95-95 targets nationally leaves 186,826 virally unsuppressed PLHIV, yielding a national prevalence of virally unsuppressed PLHIV of 0.59% (Fig 2, Table 2). Approximately 50% (91,359) of the remaining unsuppressed PLHIV reside in 7 of the 47 subnational units (counties): Homa Bay, Kisumu, Siaya, Migori, Mombasa, Nakuru and Nairobi. The prevalence of unsuppressed PLHIV is expected to be 2-fold higher than the regional estimate for ESA, and over 3-fold higher than the Kenya national estimate in four counties in western Kenya around Lake Victoria, namely, Kisumu (2.16%), Homa Bay (2.15%), Migori (2.03%) and Siaya (1.92%).
Fig 2. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by subnational unit, Kenya.
Maps were created using a licensed ArcGIS by ESRI version 10.6.1 GIS Mapping Software, Location Intelligence & Spatial Analytics | Esri, Desktop Help 10.0 - Redistribution rights (arcgis.com); Base map from: Esri. "Kenya_4_Counties_2022_Nov”[basemap]. Kenya_4_Counties_2022_Nov (FeatureServer)(arcgis.com); (June 14, 2024).
Table 2. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by subnational unit, Kenya.
| After reaching | After reaching | After reaching | After reaching | |||||
|---|---|---|---|---|---|---|---|---|
| 1st 95 | 2nd 95 | 3rd 95 | all 95-95-95 targets | |||||
| Subnational Unit | Estimated number of PLHIV aged 15+ years | HIV prevalence (%) | Remain undiagnosed | Know HIV status, not on ART | On ART, not virally suppressed | Total no. of virally non-suppressed PLHIV | Population denominator* | Prevalence virally non-suppressed PLHIV |
| Central | 119,495 | 2.99% | 5,975 | 5,676 | 5,392 | 17,043 | 3,977,974 | 0.43% |
| Kiambu | 65,438 | 3.62% | 3,272 | 3,108 | 2,953 | 9,333 | 1,800,642 | 0.52% |
| Kirinyaga | 11,586 | 2.45% | 579 | 550 | 523 | 1,652 | 471,689 | 0.35% |
| Murang’a | 17,723 | 2.28% | 886 | 842 | 800 | 2,528 | 776,495 | 0.33% |
| Nyandarua | 7,386 | 1.65% | 369 | 351 | 333 | 1,053 | 445,668 | 0.24% |
| Nyeri | 17,362 | 3.57% | 868 | 825 | 783 | 2,476 | 483,478 | 0.51% |
| Coast | 113,196 | 4.01% | 5,660 | 5,377 | 5,108 | 16,145 | 2,805,399 | 0.58% |
| Kilifi | 21,735 | 2.40% | 1,087 | 1,032 | 981 | 3,100 | 903,425 | 0.34% |
| Kwale | 23,085 | 4.44% | 1,154 | 1,097 | 1,042 | 3,292 | 516,215 | 0.64% |
| Lamu | 1,731 | 1.82% | 87 | 82 | 78 | 247 | 94,854 | 0.26% |
| Mombasa | 56,559 | 6.42% | 2,828 | 2,687 | 2,552 | 8,067 | 872,960 | 0.92% |
| Taita-Taveta | 8,420 | 3.47% | 421 | 400 | 380 | 1,201 | 241,526 | 0.50% |
| Tana River | 1,667 | 0.94% | 83 | 79 | 75 | 238 | 176,418 | 0.13% |
| Eastern | 130,880 | 2.73% | 6,544 | 6,217 | 5,906 | 18,667 | 4,776,826 | 0.39% |
| Embu | 10,184 | 2.22% | 509 | 484 | 460 | 1,453 | 457,188 | 0.32% |
| Isiolo | 1,991 | 1.24% | 100 | 95 | 90 | 284 | 160,356 | 0.18% |
| Kitui | 29,958 | 3.98% | 1,498 | 1,423 | 1,352 | 4,273 | 748,288 | 0.57% |
| Machakos | 35,224 | 3.33% | 1,761 | 1,673 | 1,589 | 5,024 | 1,053,961 | 0.48% |
| Makueni | 19,266 | 2.78% | 963 | 915 | 869 | 2,748 | 690,362 | 0.40% |
| Marsabit | 1,340 | 0.49% | 67 | 64 | 60 | 191 | 274,163 | 0.07% |
| Meru | 25,723 | 2.31% | 1,286 | 1,222 | 1,161 | 3,669 | 1,108,721 | 0.33% |
| Tharaka | 7,194 | 2.53% | 360 | 342 | 325 | 1,026 | 283,787 | 0.36% |
| Nithi | ||||||||
| Nairobi | 140,251 | 4.44% | 7,013 | 6,662 | 6,329 | 20,003 | 3,137,702 | 0.64% |
| North Eastern | 3,029 | 0.21% | 151 | 144 | 137 | 432 | 1,466,100 | 0.03% |
| Garissa | 1,480 | 0.23% | 74 | 70 | 67 | 211 | 648,345 | 0.03% |
| Mandera | 981 | 0.24% | 49 | 47 | 44 | 140 | 411,669 | 0.03% |
| Wajir | 568 | 0.14% | 28 | 27 | 26 | 81 | 406,087 | 0.02% |
| Nyanza | 432,991 | 11.00% | 21,650 | 20,567 | 19,539 | 61,755 | 3,875,668 | 1.59% |
| Homa Bay | 100,073 | 14.76% | 5,004 | 4,753 | 4,516 | 14,273 | 663,638 | 2.15% |
| Kisii | 30,346 | 3.73% | 1,517 | 1,441 | 1,369 | 4,328 | 808,314 | 0.54% |
| Kisumu | 113,236 | 14.79% | 5,662 | 5,379 | 5,110 | 16,150 | 749,349 | 2.16% |
| Migori | 92,275 | 13.94% | 4,614 | 4,383 | 4,164 | 13,161 | 648,782 | 2.03% |
| Nyamira | 14,385 | 3.64% | 719 | 683 | 649 | 2,052 | 392,680 | 0.52% |
| Siaya | 82,676 | 13.23% | 4,134 | 3,927 | 3,731 | 11,792 | 612,904 | 1.92% |
| Rift Valley | 214,541 | 2.59% | 10,727 | 10,191 | 9,681 | 30,599 | 8,239,727 | 0.37% |
| Baringo | 4,668 | 1.14% | 233 | 222 | 211 | 666 | 407,707 | 0.16% |
| Bomet | 10,019 | 1.79% | 501 | 476 | 452 | 1,429 | 559,395 | 0.26% |
| Elgeyo- | 5,781 | 1.99% | 289 | 275 | 261 | 825 | 290,045 | 0.28% |
| Marakwet | ||||||||
| Kajiado | 23,829 | 3.10% | 1,191 | 1,132 | 1,075 | 3,399 | 764,464 | 0.44% |
| Kericho | 17,503 | 2.89% | 875 | 831 | 790 | 2,496 | 602,715 | 0.41% |
| Laikipia | 6,309 | 1.75% | 315 | 300 | 285 | 900 | 358,585 | 0.25% |
| Nakuru | 55,481 | 3.70% | 2,774 | 2,635 | 2,504 | 7,913 | 1,490,503 | 0.53% |
| Nandi | 14,073 | 2.39% | 704 | 668 | 635 | 2,007 | 587,718 | 0.34% |
| Narok | 12,157 | 1.85% | 608 | 577 | 549 | 1,734 | 655,696 | 0.26% |
| Samburu | 3,329 | 1.90% | 166 | 158 | 150 | 475 | 175,002 | 0.27% |
| Trans Nzoia | 14,588 | 2.32% | 729 | 693 | 658 | 2,081 | 626,085 | 0.33% |
| Turkana | 12,099 | 2.12% | 605 | 575 | 546 | 1,726 | 568,278 | 0.30% |
| Uasin Gishu | 32,320 | 3.95% | 1,616 | 1,535 | 1,458 | 4,610 | 813,889 | 0.57% |
| West Pokot | 2,384 | 0.70% | 119 | 113 | 108 | 340 | 339,643 | 0.10% |
| Western | 155,531 | 4.87% | 7,777 | 7,388 | 7,018 | 22,183 | 3,168,367 | 0.70% |
| Bungoma | 43,303 | 4.15% | 2,165 | 2,057 | 1,954 | 6,176 | 1,037,912 | 0.60% |
| Busia | 41,182 | 7.23% | 2,059 | 1,956 | 1,858 | 5,874 | 564,040 | 1.04% |
| Kakamega | 51,645 | 4.33% | 2,582 | 2,453 | 2,330 | 7,366 | 1,185,615 | 0.62% |
| Vihiga | 19,400 | 5.06% | 970 | 921 | 875 | 2,767 | 380,800 | 0.73% |
| Kenya | 1,309,914 | 4.14% | 65,496 | 62,221 | 59,110 | 186,826 | 31,447,763 | 0.59% |
*Population denominator = Sum of the total susceptible (HIV-negative) population aged 15+ years and the total number of PLHIV aged 15+ years who remain virally unsuppressed after reaching the 95-95-95 targets.
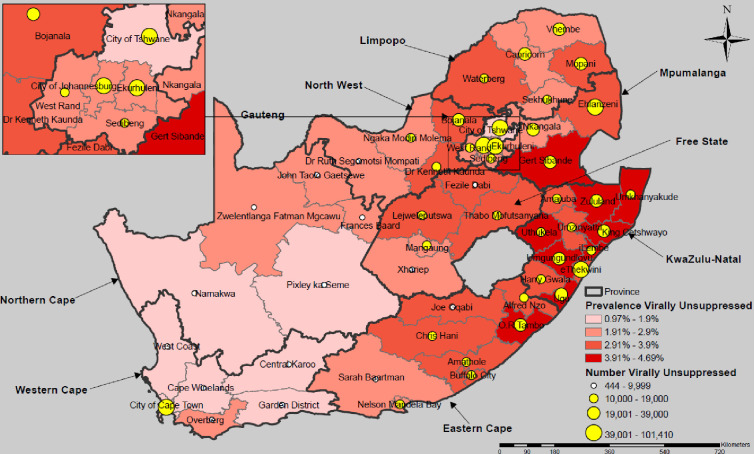
In South Africa the projected outcome of meeting the 95-95-95 targets leaves 1,091,423 virally unsuppressed PLHIV, translating to a national prevalence of unsuppressed PLHIV of 2.89%. Outcomes vary widely across the nine provinces and 52 municipalities (districts) (Fig 3, Table 3). Fifteen (29%) districts remain with fewer than 10,000 virally unsuppressed PLHIV, 31 (60%) with 10,000–39,000, and 6 (11%) with over 40,000. Nearly one-half (26 districts) have a projected prevalence of virally unsuppressed PLHIV of 3.0% and above—≥ 3-fold higher than the regional estimate for ESA—with highest expected prevalence in districts in KwaZulu Natal Province (range 3.48%–4.69%).
Fig 3. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by subnational unit, South Africa.
Maps were created using a licensed ArcGIS by ESRI version 10.6.1 GIS Mapping Software, Location Intelligence & Spatial Analytics | Esri, Desktop Help 10.0 - Redistribution rights (arcgis.com); Base map from: Esri. “SouthAfrica_5_Districts_2022_Nov”[basemap]. SouthAfrica_5_Districts_2022_Nov (FeatureServer) (arcgis.com); (June 14, 2024).
Table 3. Estimated number and prevalence of virally unsuppressed people living with HIV aged 15+ years expected to remain after reaching the 95-95-95 targets by subnational unit, South Africa.
| After reaching 1st 95 | After reaching 2nd 95 | After reaching 3rd 95 | After reaching all 95-95-95 targets | |||||
|---|---|---|---|---|---|---|---|---|
| Subnational Unit | Estimated no. PLHIV aged 15+ years | HIV prevalence (%) | Remain undiagnosed | Know HIV status, not on ART | On ART, not virally suppressed | Total no. virally non-suppressed PLHIV | Population denominator* | Prevalence virally non-suppressed PLHIV |
| Eastern Cape Province | 868,185 | 18.5% | 43,409 | 41,239 | 39,177 | 123,825 | 4,027,238 | 3.07% |
| Alfred Nzo District | 105,157 | 20.7% | 5,258 | 4,995 | 4,745 | 14,998 | 436,250 | 3.44% |
| Amathole District | 95,046 | 17.9% | 4,752 | 4,515 | 4,289 | 13,556 | 456,053 | 2.97% |
| Buffalo City Metropolitan | 120,808 | 19.5% | 6,040 | 5,738 | 5,451 | 17,230 | 531,907 | 3.24% |
| Chris Hani District | 90,656 | 19.0% | 4,533 | 4,306 | 4,091 | 12,930 | 409,713 | 3.16% |
| Oliver Tambo District | 232,589 | 23.6% | 11,629 | 11,048 | 10,496 | 33,173 | 847,326 | 3.92% |
| Joe Gqabi District | 42,317 | 18.0% | 2,116 | 2,010 | 1,910 | 6,035 | 197,755 | 3.05% |
| Nelson Mandela Bay | 126,821 | 18.4% | 6,341 | 6,024 | 5,723 | 18,088 | 829,236 | 2.18% |
| Sarah Baartman District | 54,791 | 14.8% | 2,740 | 2,603 | 2,472 | 7,815 | 318,998 | 2.45% |
| Free State Province | 400,276 | 19.4% | 20,014 | 19,013 | 18,062 | 57,089 | 1,778,361 | 3.21% |
| Lejweleputswa District | 94,784 | 20.1% | 4,739 | 4,502 | 4,277 | 13,519 | 404,948 | 3.34% |
| Thabo Mofutsanyane | 113,022 | 21.8% | 5,651 | 5,369 | 5,100 | 16,120 | 445,035 | 3.62% |
| District | ||||||||
| Fezile Dabi District | 69,696 | 19.2% | 3,485 | 3,311 | 3,145 | 9,940 | 312,891 | 3.18% |
| Mangaung Metropolitan | 109,947 | 17.4% | 5,497 | 5,222 | 4,961 | 15,681 | 541,877 | 2.89% |
| Xhariep District | 12,827 | 15.0% | 641 | 609 | 579 | 1,829 | 73,611 | 2.48% |
| Gauteng Province | 1,800,724 | 14.4% | 90,036 | 85,534 | 81,258 | 256,828 | 10,726,635 | 2.39% |
| City of Johannesburg | 711,023 | 14.7% | 35,551 | 33,774 | 32,085 | 101,410 | 4,159,706 | 2.44% |
| Metropolitan | ||||||||
| City of Tshwane | 344,530 | 11.5% | 17,227 | 16,365 | 15,547 | 49,139 | 2,582,677 | 1.90% |
| Metropolitan | ||||||||
| Ekurhuleni Metropolitan | 530,480 | 16.8% | 26,524 | 25,198 | 23,938 | 75,660 | 2,712,327 | 2.79% |
| Sedibeng District | 731,014 | 14.2% | 5,176 | 4,918 | 4,672 | 14,766 | 628,672 | 2.35% |
| West Rand District | 747,968 | 14.9% | 5,558 | 5,280 | 5,016 | 15,855 | 643,252 | 2.46% |
| KwaZulu Natal Province | 1,949,499 | 24.1% | 97,475 | 92,601 | 87,971 | 278,047 | 6,953,144 | 4.00% |
| eThekwini Metropolitan | 645,186 | 21.0% | 32,259 | 30,646 | 29,114 | 92,020 | 2,647,386 | 3.48% |
| Harry Gwala District | 75,117 | 22.9% | 3,756 | 3,568 | 3,390 | 10,714 | 281,642 | 3.80% |
| King Cetshwayo District | 180,842 | 28.3% | 9,042 | 8,590 | 8,160 | 25,793 | 550,502 | 4.69% |
| Ugu District | 140,644 | 26.0% | 7,032 | 6,681 | 6,347 | 20,059 | 464,323 | 4.32% |
| uMgungundlovu District | 229,654 | 27.7% | 11,483 | 10,909 | 10,363 | 32,754 | 714,067 | 4.59% |
| Uthukela District | 119,695 | 26.1% | 5,985 | 5,686 | 5,401 | 17,071 | 393,857 | 4.33% |
| Zululand District | 147,574 | 26.7% | 7,379 | 7,010 | 6,659 | 21,048 | 475,934 | 4.42% |
| Amajuba District | 90,340 | 23.0% | 4,517 | 4,291 | 4,077 | 12,885 | 337,871 | 3.81% |
| iLembe District | 124,487 | 25.9% | 6,224 | 5,913 | 5,617 | 17,755 | 412,661 | 4.30% |
| Umkhanyakude District | 117,662 | 27.2% | 5,883 | 5,589 | 5,309 | 16,782 | 371,923 | 4.51% |
| Umzinyathi District | 78,298 | 22.2% | 3,915 | 3,719 | 3,533 | 11,167 | 302,977 | 3.69% |
| Limpopo Province | 682,578 | 17.2% | 34,129 | 32,422 | 30,801 | 97,353 | 3,406,584 | 2.86% |
| Capricorn District | 150,837 | 17.1% | 7,542 | 7,165 | 6,807 | 21,513 | 760,696 | 2.83% |
| Mopani District | 161,120 | 20.2% | 8,056 | 7,653 | 7,271 | 22,980 | 687,588 | 3.34% |
| Sekhukhune District | 112,749 | 14.5% | 5,637 | 5,356 | 5,088 | 16,081 | 666,659 | 2.41% |
| Vhembe District | 153,859 | 15.8% | 7,693 | 7,308 | 6,943 | 21,944 | 835,664 | 2.63% |
| Waterberg District | 104,013 | 19.6% | 5,201 | 4,941 | 4,694 | 14,835 | 455,977 | 3.25% |
| Mpumalanga Province | 735,931 | 20.9% | 36,797 | 34,957 | 33,209 | 104,962 | 3,021,013 | 3.47% |
| Ehlanzeni District | 300,316 | 23.2% | 15,016 | 14,265 | 13,552 | 42,833 | 1,114,169 | 3.84% |
| Gert Sibande District | 235,240 | 24.8% | 11,762 | 11,174 | 10,615 | 33,551 | 817,366 | 4.10% |
| Nkangala District | 200,375 | 15.8% | 10,019 | 9,518 | 9,042 | 28,578 | 1,089,478 | 2.62% |
| Northern Cape Province | 107,485 | 13.8% | 5,374 | 5,106 | 4,850 | 15,330 | 667,472 | 2.30% |
| Frances Baard District | 41,433 | 16.9% | 2,072 | 1,968 | 1,870 | 5,909 | 210,586 | 2.81% |
| John Taolo Gaetsewe | 27,044 | 17.2% | 1,352 | 1,285 | 1,220 | 3,857 | 135,327 | 2.85% |
| District | ||||||||
| Namakwa District | 4,732 | 6.6% | 237 | 225 | 214 | 675 | 61,637 | 1.10% |
| Pixley ka Seme District | 13,297 | 10.5% | 665 | 632 | 600 | 1,896 | 108,798 | 1.74% |
| Zwelentlanga Fatman | 20,979 | 11.9% | 1,049 | 997 | 947 | 2,992 | 151,124 | 1.98% |
| Mgcawu District | ||||||||
| North West Province | 524,486 | 17.8% | 26,224 | 24,913 | 23,667 | 74,805 | 2,534,153 | 2.95% |
| Bojanala Platinum District | 268,067 | 18.5% | 13,403 | 12,733 | 12,097 | 38,233 | 1,247,310 | 3.07% |
| Dr Kenneth Kaunda | 109,260 | 19.0% | 5,463 | 5,190 | 4,930 | 15,583 | 494,766 | 3.15% |
| District | ||||||||
| Ngaka Modiri Molema | 99,852 | 16.2% | 4,993 | 4,743 | 4,506 | 14,241 | 531,105 | 2.68% |
| District | ||||||||
| Dr Ruth Segomotsi | 47,307 | 15.6% | 2,365 | 2,247 | 2,135 | 6,747 | 260,973 | 2.59% |
| Mompati District | ||||||||
| Western Cape Province | 583,231 | 10.8% | 29,162 | 27,704 | 26,318 | 83,183 | 4,641,182 | 1.79% |
| City of Cape Town | 399,320 | 11.1% | 19,966 | 18,968 | 18,019 | 56,953 | 3,089,927 | 1.84% |
| Metropolitan | ||||||||
| Cape Winelands District | 66,742 | 9.3% | 3,337 | 3,170 | 3,012 | 9,519 | 614,897 | 1.55% |
| Central Karoo District | 3,115 | 5.9% | 156 | 148 | 141 | 444 | 45,605 | 0.97% |
| Garden Route District | 49,476 | 10.7% | 2,474 | 2,350 | 2,233 | 7,057 | 398,689 | 1.77% |
| Overberg District | 27,016 | 11.9% | 1,351 | 1,283 | 1,219 | 3,853 | 195,586 | 1.97% |
| West Coast District | 37,562 | 10.9% | 1,878 | 1,784 | 1,695 | 5,357 | 296,478 | 1.81% |
| South Africa Overall | 7,652,395 | 17.4% | 382,620 | 363,489 | 345,314 | 1,091,423 | 37,755,782 | 2.89% |
*Population denominator = Sum of total susceptible (HIV-negative) population aged 15+ years and the total number of PLHIV aged 15+ years who remain virally unsuppressed after reaching the 95-95-95 targets.
Discussion
Our analysis demonstrates, that although the UNAIDS 95-95-95 targets are an important metric for guiding and monitoring national HIV programs, the application of uniform proportional targets across the geographically heterogeneous HIV epidemic in ESA fails to fully address health inequities. Using HIV estimates for 2022 we show that if all countries had reached all three of the UNAIDS 95-95-95 targets, those with a higher initial HIV prevalence and number of PLHIV would remain with a greater number and prevalence of virally unsuppressed PLHIV—essentially, a greater number and prevalence of PLHIV who, without treatment, may have poor health outcomes and can transmit the virus. We further demonstrate that these limitations, and corresponding concerns about equitable epidemic control, persist when applied across subnational units in the case studies of Kenya and South Africa.
Kenya, with approximately 1,310,000 million PLHIV aged 15+ years, had a UNAIDS target achievement of 96-89-94 in 2021 [4]. With annual HIV incidence of 1.17 per 1,000 adults aged 15–49 years, and estimated new HIV infections (~35,000) falling below deaths among PLHIV (~36,000) [4], Kenya is among numerous countries in ESA nearing both the 95-95-95 targets and widely used definitions of HIV epidemic control [4, 12]. Our analysis highlights that despite these promising national metrics, geographic disparities in the remaining burden of HIV will persist at county-level, particularly in western Kenya around Lake Victoria. These counties will need to achieve a population-level viral load suppression that exceeds 85.7% (i.e., exceeds the 95-95-95 targets) to reach a prevalence of unsuppressed PLHIV equivalent to the national projection. For example, Kisumu County, would need approximately 96% (108,706) of its 113,236 PLHIV to be virally suppressed—nearly a 99-99-99 target achievement—to reach the current projected national prevalence of 0.59%.
In South Africa, with an estimated 7.5 million PLHIV, 94% are aware of their HIV status; however, gaps remain in treatment uptake among those who know their status (76%), and to a lesser degree, viral load suppression among those on ART (92%). Nationally, the number of new HIV infections in 2021 was 210,000, corresponding to an HIV incidence of 6.9 per 1,000 adults aged 15–49 years [3]. Owing to the sheer magnitude of the HIV epidemic, the expected number and prevalence of virally unsuppressed PLHIV after reaching the 95-95-95 targets in South Africa far exceeds the projected remaining burden for other countries in the region. Overall, 94.4% (7,224,438/7,652,395) of South Africa’s PLHIV would need to be virally suppressed, a 98-98-98 national target achievement, to reach a prevalence of unsuppressed PLHIV equivalent to the ESA regional projection (1.03%). Differences are even more pronounced at subnational levels, where, after reaching the 95s (85.7% population VL suppression) some provinces (KwaZulu-Natal, Gauteng) are expected to remain with a larger number and prevalence of virally unsuppressed PLHIV than some countries had nationally at baseline before applying the 95-95-95 target cascade.
Both case studies underscore the value of subnational estimates of PLHIV [9] and need for a more granular approach to defining and assessing progress towards ending HIV as a public health threat within and across geographically diverse HIV epidemics. In areas with generalized HIV epidemics, such as the ESA, the impact of achieving the 95-95-95 treatment targets by 2030, and recently expanded set of HIV prevention targets by 2025, is estimated using the Goals Age-Structured Model (Goals-ASM), described elsewhere [13]. Briefly, the Goals-ASM model incorporates data on behaviors, epidemiological factors, and biomedical and behavioral interventions that can influence the probability of HIV transmission, together with data on HIV prevalence, key populations size estimates and intervention coverage, all stratified by age and sex, to generate estimates of expected trends in new infections and AIDS-related deaths. Indicators are generated at national level and aggregated up to produce a global impact estimate, which is validated against results from other models [13, 14].
Whereas the Goals-ASM model of the global HIV epidemic focuses on national and regional outcomes, our analysis points to a critical need for models that assess the prevention and treatment intervention coverage required at the subnational level to effectively, and equitably, reduce the number and prevalence of virally unsuppressed PLHIV, new HIV infections and deaths across a geographically diverse epidemic. Finer detail could assist national HIV programs to effectively calibrate strategies and the intensity of programing across geographic areas, and to address current and projected health disparities that may undermine efforts to reach and sustain HIV epidemic control even after the 95 targets are achieved.
Population-level surveys are key sources of data on incidence and prevalence of HIV, knowledge of HIV status, prevalence of viral load non-suppression in the population of PLHIV, and prevalence of behavioral factors that can affect the risk of HIV transmission—these data are essential for monitoring program impact and gaps, and as a source of national and subnational HIV model inputs and assumptions [9, 15, 16]. Numerous countries in ESA region have supported one or more periodic (approximately every 5 years) national population-based HIV serological and behavioral surveys in the last 10 years, in some cases oversampling geographic areas with high burden of HIV to provide subnational estimates of key HIV indicators [17–19]. The relative infrequency and cost of national surveys in an era of a rapidly evolving HIV response limits timely access to valuable data for decision-making, an issue that could be addressed by more frequent population surveys economized to focus on geographic areas and subpopulations with greatest burden of HIV and/or greatest potential barriers to accessing care [18]. HIV case surveillance systems provide ongoing longitudinal data on key outcomes (HIV diagnosis, viral load status, mortality) among persons with HIV infection who have accessed care. Case surveillance data can be used to monitor HIV epidemics, inform HIV programing and guide rapid public health action at a granular level [20]; however, the status of implementation of case surveillance, including collection of mortality events, varies widely across countries [21]. Expansion of effective HIV case surveillance systems [21], including linkage to high quality vital registration data [22], together with more frequent localized population surveys could improve the availability of timely, granular data needed to guide HIV programing, effectively track, model, and control the HIV epidemic, and address existing and emergent inequities at subnational levels.
Limitations
Our analysis has limitations. Firstly, we used census projections for 2018–2021; any differences between projected and actual population aged 15 years could result in an over- or under-estimation of the calculated prevalence of virally unsuppressed PLHIV. Secondly, this analysis relied on modeled estimates of the number of PLHIV. Published HIV estimates and associated credible intervals are generated using a robust, standardized process [9], but are nevertheless impacted by the quality and timeliness of model inputs for each country. Finally, as our analysis applied the 95-95-95 targets to current national and subnational estimates targets to calculate projected outcomes, it did not account for longitudinal changes in population structure, transmission dynamics, migration [23, 24] or the public health response (e.g. expanded access to pre-exposure prophylaxis), which over time could impact the course of the HIV epidemic in the general population, key and priority populations (i.e., female sex workers, men who have sex with men, people who inject drugs, adolescent girls and young women). Models tailored to the local (geographic) context would lend further insight into how these may impact projected outcomes. Despite these limitations, the underlying principle that health inequities result when a uniform set of targets is applied across a heterogeneous HIV epidemic remains unchanged.
Conclusions
The UNAIDS 95-95-95 targets are an important metric for guiding and monitoring national HIV programs. Our analysis demonstrates that reliance on uniform targets across a geographically diverse HIV epidemic can lead to remarkably different outcomes, and potentially mislead program strategies, resource allocation, and progress towards equitable epidemic control. More granular surveillance information on the HIV epidemic could assist national HIV programs to effectively calibrate strategies and intensity of programing across geographic areas to address current and projected health disparities that may undermine efforts to reach and sustain HIV epidemic control even after the 95 targets are achieved.
Supporting information
Description of data sources and available data for calculation of the number and prevalence of virally unsuppressed people living with HIV by country.
(DOCX)
Data Availability
All data used for the analysis are publicly available at https://naomi-spectrum.unaids.org/. The data used for the calculations is in the paper's tables.
Funding Statement
The authors received no specific funding for this work.
References
- 1.(UNAIDS). Joint United Nations Programme on HIV/AIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic. 2014. Available from: http://www.unaids.org/en/resources/documents/2017/90-90-90. [Google Scholar]
- 2.UNAIDS. UNAIDS Data 2018 2018. Available from: https://www.unaids.org/en/resources/documents/2018/unaids-data-2018. [Google Scholar]
- 3.(UNAIDS). AIDSinfo. Eastern and Southern Africa Regional Fact Sheets 2022. Available from: https://aidsinfo.unaids.org/. [Google Scholar]
- 4.(UNAIDS). Joint United Nations Programme on HIV/AIDS. IN DANGER: UNAIDS Global AIDS Update 2022. Geneva2022. Available from: https://www.aidsdatahub.org/resource/danger-unaids-global-aids-update-2022. [Google Scholar]
- 5.Nsanzimana S, Mills EJ. Estimating HIV incidence in sub-Saharan Africa. Lancet HIV. 2023;10(3):e146–e8. Epub 20230123. doi: 10.1016/S2352-3018(22)00366-6 . [DOI] [PubMed] [Google Scholar]
- 6.(PEPFAR). U.S. President’s Emergency Plan for AIDS Relief. Reimagining PEPFAR’s Stretegic Direction: Fullfilling America’s Promist to End the HIV/AIDS Pandemic by 2030 2022. Available from: https://www.state.gov/wp-content/uploads/2022/09/PEPFAR-Strategic-Direction_FINAL.pdf. [Google Scholar]
- 7.(UNAIDS). Joint United Nations Programme on HIV/AIDS. Dangerous inequalities: World AIDS Day report 2022. Geneva2022 [cited Licence: CC BY-NC-SA 3.0 IGO]. Available from: https://www.unaids.org/sites/default/files/media_asset/dangerous-inequalities_en.pdf. [Google Scholar]
- 8.UNAIDS. HIV sub-national estimates viewer 2022. [updated February 11, 2023]. Available from: https://naomi-spectrum.unaids.org/. [Google Scholar]
- 9.Eaton JW, Dwyer-Lindgren L, Gutreuter S, O’Driscoll M, Stevens O, Bajaj S, et al. Naomi: a new modelling tool for estimating HIV epidemic indicators at the district level in sub-Saharan Africa. J Int AIDS Soc. 2021;24 Suppl 5(Suppl 5):e25788. doi: 10.1002/jia2.25788 ; PubMed Central PMCID: PMC8454682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Population Prospects 2022: Summary of Results [Internet]. 2022. Available from: https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022. [Google Scholar]
- 11.Team RC. R: A language and environment for statistical computing Vienna, Austria: R Foundation for Statistical Computing; 2017. Available from: https://www.r-project.org/. [Google Scholar]
- 12.Galvani AP, Pandey A, Fitzpatrick MC, Medlock J, Gray GE. Defining control of HIV epidemics. Lancet HIV. 2018;5(11):e667–e70. Epub 20181009. doi: 10.1016/S2352-3018(18)30178-4 . [DOI] [PubMed] [Google Scholar]
- 13.(UNAIDS). Joint United Nations Programme on HIV and AIDS. World AIDS Day Report 2020: Prevailing Against Pandemics by Putting People at the Center Geneva 2020. Available from: https://aidstargets2025.unaids.org/assets/images/prevailing-against-pandemics_en.pdf. [Google Scholar]
- 14.Kerr CC SR, Gray R, Shattock AJ. Optima: A Model for HIV Epidemic Analysis, Program Prioritization, and Resource Optimization. Journal of Acquired Immune Deficiency Syndromes. 2015;69. doi: 10.1097/QAI.0000000000000605 [DOI] [PubMed] [Google Scholar]
- 15.Stover J, Glaubius R, Mofenson L, Dugdale CM, Davies MA, Patten G, et al. Updates to the Spectrum/AIM model for estimating key HIV indicators at national and subnational levels. AIDS. 2019;33 Suppl 3(Suppl 3):S227–S34. doi: 10.1097/QAD.0000000000002357 ; PubMed Central PMCID: PMC6919230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson LF, Meyer-Rath G, Dorrington RE, Puren A, Seathlodi T, Zuma K, et al. The Effect of HIV Programs in South Africa on National HIV Incidence Trends, 2000–2019. J Acquir Immune Defic Syndr. 2022;90(2):115–23. Epub 20220207. doi: 10.1097/QAI.0000000000002927 . [DOI] [PubMed] [Google Scholar]
- 17.Simbayi LC ZK, Zungu N, Moyo S, et al. South African National HIV Prevalence, Incidence, Behaviour, and Communication Survey, 2017. Cape Town2019. Available from: https://hsrc.ac.za/uploads/pageContent/10779/SABSSM%20V.pdf. [Google Scholar]
- 18.Project P-bHIAP. Uganda Refugee Population-based HIV Impact Assessment [Report]. 2023. Available from: https://phia.icap.columbia.edu/wp-content/uploads/2023/04/230323_RR1_SS_RUPHIA-2021.pdf. [Google Scholar]
- 19.(NASCOP). National AIDS and STI Control Programme. Kenya Population-based HIV Impact Assessment (KENPHIA) 2018: Final Report Nairobi: NASCOPAugust 2022. Available from: https://phia.icap.columbia.edu/kenya-final-report-2018/. [Google Scholar]
- 20.(WHO). World Health Organization. Consolidated guidelines on person-centred HIV patient monitoring and case surveillance. Geneva, Switzerland: 2017.
- 21.Holmes JR, Dinh TH, Farach N, Manders EJ, Kariuki J, Rosen DH, et al. Status of HIV Case-Based Surveillance Implementation—39 U.S. PEPFAR-Supported Countries, May-July 2019. MMWR Morb Mortal Wkly Rep. 2019;68(47):1089–95. Epub 20191129. doi: 10.15585/mmwr.mm6847a2 ; PubMed Central PMCID: PMC6881050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahiane SG, Eaton JW, Glaubius R, Case KK, Sabin KM, Marsh K. Updates to Spectrum’s case surveillance and vital registration tool for HIV estimates and projections. J Int AIDS Soc. 2021;24 Suppl 5(Suppl 5):e25777. doi: 10.1002/jia2.25777 ; PubMed Central PMCID: PMC8454676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Low A, Sachathep K, Rutherford G, Nitschke AM, Wolkon A, Banda K, et al. Migration in Namibia and its association with HIV acquisition and treatment outcomes. PLoS One. 2021;16(9):e0256865. Epub 20210902. doi: 10.1371/journal.pone.0256865 ; PubMed Central PMCID: PMC8412347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Low AJ, Frederix K, McCracken S, Manyau S, Gummerson E, Radin E, et al. Association between severe drought and HIV prevention and care behaviors in Lesotho: A population-based survey 2016–2017. PLoS Med. 2019;16(1):e1002727. Epub 20190114. doi: 10.1371/journal.pmed.1002727 ; PubMed Central PMCID: PMC6331084. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of data sources and available data for calculation of the number and prevalence of virally unsuppressed people living with HIV by country.
(DOCX)
Data Availability Statement
All data used for the analysis are publicly available at https://naomi-spectrum.unaids.org/. The data used for the calculations is in the paper's tables.