Abstract
Chronic pain represents a significant unmet medical need, affecting one‐fifth of the U.S. population. EC5026 is a small molecule inhibitor of the enzyme soluble epoxide hydrolase (sEH) which is being developed as a novel non‐opioid, non‐NSAID analgesic. EC5026 prolongs the action of epoxy fatty acids, endogenous analgesic lipid mediators that are rapidly metabolized by sEH. We evaluated the safety and pharmacokinetic profile of EC5026 in two phase I trials, a single‐ascending dose (SAD) study and a fed‐fasted study. The SAD study evaluated EC5026 doses ranging from 0.5 to 24 mg in healthy volunteers. EC5026 was well tolerated. No treatment‐emergent adverse events were considered related to EC5026. No apparent treatment‐ or dose‐related trends in laboratory results, vital signs, physical examinations, or electrocardiograms were observed. A linear, near‐dose‐proportional increase in exposure was observed with progressive doses in the SAD study; plasma exposure was below or near the lower limit of quantification after 0.5–2 mg doses. Mean half‐lives ranged from 41.8 to 59.1 h. for doses of 8–24 mg, supporting a once‐daily dosing regimen. In the fed‐fasted study using 8 mg EC5026 tablets, higher peak concentrations (66%) and total exposures (53%) were observed under the fed condition. Plasma concentrations declined in a monoexponential manner with mean half‐lives of 59.5 h. in the fed state and 66.9 h. in the fasted state. Future clinical trials using EC5026 for the treatment of pain are justified based on the favorable outcomes from both clinical trials along with preclinical evidence of analgesic activity.
Abbreviations
- ACTH
adrenocorticotrophic hormone
- Ae0–48
amount excreted in 48 h
- AUC
Area under the curve
- CCI
chronic constriction injury
- CIPN
chemotherapy‐induced peripheral neuropathy
- CL/F
apparent total body clearance
- Cmax
maximal plasma concentration
- COX
cyclooxygenase
- CV
coefficient of variation
- EpFAs
epoxy fatty acids
- ER
endoplasmic reticulum
- GLP
Good Laboratory Practice
- HME
hot melt extrusion
- HPA
hypothalamic‐pituitary adrenal
- HPG
hypothalamic‐pituitary gonadal
- IV
intravenous
- LOX
lipoxygenase
- NC
not calculated
- NOAEL
No Observed Adverse Effect Level
- NSAIDs
nonsteroidal anti‐inflammatory drugs
- PEG
polyethylene glycol
- PK
pharmacokinetics
- SAD
single ascending dose
- sEH
soluble epoxide hydrolase
- SRC
Safety Review Committee
- t 1/2
half‐life
- TEAE
Treatment Emergent Adverse Event
- Tmax
time to maximal plasma concentration
- TMDD
target‐mediated drug disposition
- Vz/F
apparent volume of distribution based on the terminal elimination rate constant
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
Soluble epoxide hydrolase inhibitors (sEHI) have shown promising antinociceptive profiles in both experimental and pathological (natural onset) inflammatory and neuropathic pain in rodents, dogs, cats, and horses. EC5026 is the first sEHI to be selected for clinical development as a novel non‐opioid analgesic.
WHAT QUESTION DID THIS STUDY ADDRESS?
These first‐in‐man clinical studies were designed to evaluate the safety, pharmacokinetics, and food effect of single‐dose exposures of EC5026 in humans.
WHAT DOES THIS STUDY ADD TO OUR KNOWLEDGE?
The two phase Ia clinical trials reported here show that EC5026 has a small (statistically significant but clinically insignificant) food effect. C max and AUC0‐48 were increased by 66% and 53% in the fed state; the half‐life was essentially unchanged at ~ 2–2.5 days. These data show that EC5026 may be suitable for once‐daily administration in future clinical trials without regard to fed vs. fasted state. No treatment‐emergent adverse events related to EC5026 were observed in either study at doses that are anticipated to substantially exceed the anticipated therapeutic dose range in humans.
HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?
Based upon animal studies and limited human studies performed to date with EC5026 and other sEHI, these data suggest that sEHI may represent an entirely new class of non‐opioid therapeutics for treating pain and other neurological disorders. Data from the current study support advancing EC5026 into multiple ascending dose (MAD) studies. If human efficacy studies confirm the analgesic potential of EC5026, this could add an entirely new method of treating acute and chronic pain in humans and animals.
INTRODUCTION
Recent national studies have shown that chronic pain affects an estimated 20.4% of United States adults 1 and is associated with a high disease burden for both the individual and society. 2 , 3 Currently available treatments often show only modest efficacy associated with dose‐limiting and/or serious adverse effects. 3 , 4 , 5 , 6 More than half of patients suffering from chronic pain do not achieve satisfactory pain relief. As a result, opioids are often prescribed to manage symptoms, which may be associated with the risks of opioid misuse, side effects, and addiction. 7 , 8 , 9 Therefore, there is an unmet medical need for new, highly effective, and safer non‐opioid analgesic drugs for use in chronic pain conditions.
Epoxygenated fatty acids formed from polyunsaturated fatty acids by cytochrome P450 enzymes, known as epoxy fatty acids (EpFAs), are potent endogenous analgesics. 10 , 11 , 12 EpFAs are produced biologically at efficacious local concentrations in areas of tissue damage and inflammation but are rapidly metabolized by an enzyme named soluble epoxide hydrolase (sEH) into inactive or pro‐inflammatory compounds. 13 Inhibition of sEH activity prolongs the ability of EpFAs to exert their natural analgesic and inflammation‐resolving activity. In fact, pharmacologic inhibition of the sEH has shown efficacy for the treatment of severe neuropathic and inflammatory pain in preclinical models 10 , 14 , 15 , 16 including natural onset equine laminitis pain 17 and osteoarthritis pain in beagles. 10 Potent and effective synthetic sEH inhibitors represent a completely new approach to analgesic pharmacotherapy, with a unique mechanism of action and a target that is different from all available pain therapeutics.
EC5026 (Figure 1) is a potent and selective inhibitor of sEH in multiple mammalian species that is under development by EicOsis Human Health as an oral analgesic. 18 , 19 EC5026 has demonstrated potent analgesia and a favorable dose–response relationship in two rodent neuropathic pain models, 18 , 20 providing a strong pharmacodynamic rationale for studying EC5026 in patients with neuropathic pain.
FIGURE 1.
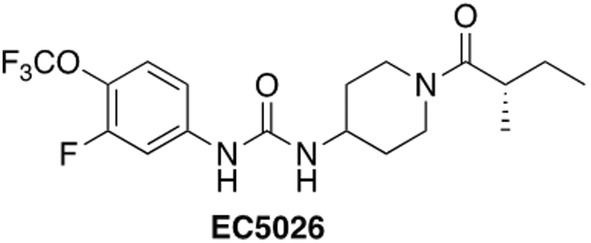
EC5026 chemical structure. Ref. [18]
The pharmacokinetics (PK) of EC5026 was characterized in rats and dogs as single intravenous (iv) and oral doses (Data on File, IND 142,184; EicOsis Human Health). When dosed in a polyethylene glycol (PEG) 300 or PEG 400 vehicle or in hot melt extrusion (HME) tablet form, EC5026 has good oral absorption and bioavailability. Following oral administration in PEG 300, EC5026 was absorbed rapidly with maximum plasma concentration (C max) occurring at 2–3 h in both rats and dogs. The bioavailability was 96% in rats. In dogs, the bioavailability was estimated to be about 60% in one study, and 59%–75% in another study using 100% PEG 400 as the vehicle for oral dosing. Based on these data, good bioavailability of EC5026 is also expected in humans.
EC5026 did not significantly inhibit human CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP2C8, or CYP3A4 at its limit of solubility. 18 Similarly, EC5026 did not induce human CYP1A2, CYP2B6, or CYP3A4 in vitro in human hepatocytes at clinically relevant concentrations. Additionally, in vitro data suggest that at 10 μM EC5026 is not an inhibitor of P‐gp, OCT1, MATE2‐K, MRP1, MPR1, MPR3, OAT1, OCT2, BSEP, NTCP, OATP1B1, or MATE1. 18 EC5026 inhibited BCRP, OATP1B3, and OAT3 with IC50 values of 1.4, 5.8, and 9.1 μM, respectively. EC5026 is not a substrate of the OATP1B1 and OATP1B3 but is likely a substrate of human P‐gp and BCRP. Considering the high permeability of EC5026 (in vitro and in non‐clinical species), the impact of P‐gp and BCRP inhibition on EC5026 exposure is expected to be limited. These data suggest the potential for drug–drug interactions in clinical trials is low; however, because EC5026 is metabolized by CYP3A4 and inhibits BCRP at clinically significant concentrations, medications and natural products that are classified as moderate‐strong CYP3A4 inhibitors and inducers, and compounds that have a narrow therapeutic index and are eliminated by BCRP, are excluded from initial clinical studies.
Safety pharmacology studies with EC5026 in rats and dogs have not identified any central nervous system, respiratory, or cardiovascular adverse risks. Notably, unlike opioid analgesics, sEH inhibition has shown no evidence thus far of tolerance, dependence, or addiction liability with chronic exposure in animals. 18 , 21 , 22
Here we report the findings of two first‐in‐human phase Ia clinical trials in healthy volunteers designed (a) to investigate the safety, tolerability, and pharmacokinetics (PK) of EC5026 drug substance dissolved in 80% PEG 400/20% PEG 3350 and filled into hard gelatin capsules, and (b) to evaluate potential food effects on PK and safety in a single‐dose fed‐fasted study using HME solid tablets suitable for commercial use.
METHODS
Two phase Ia clinical trials, an SAD study (NCT04228302) and a fed‐fasted study (NCT04908995), were conducted in accordance with International Council for Harmonization Good Clinical Practice guidelines and ethical principles from the Declaration of Helsinki. Study protocols were reviewed and approved by an investigational review board, and informed consent was obtained from each participant prior to entering the study. Both studies were conducted at a single clinical research unit (Austin Clinical Research Unit – PPD Phase I Clinic; Austin, TX 78744).
SAD study (EC5026‐1‐01): Dose selection; overall clinical design
Study EC5026‐1‐01 was a phase Ia, SAD first‐in‐human trial. It was a randomized, double‐blind, placebo‐controlled study to investigate the safety, tolerability, and PK of EC5026 in healthy male and female participants. Five cohorts with 8 participants each were enrolled. The starting oral dose of EC5026 was 0.5 mg, based in part on analgesic efficacy studies in two different neuropathic pain models in rats [chronic constriction injury (CCI) and chemotherapy‐induced peripheral neuropathy (CIPN) efficacy at 0.3–3 mg/kg orally] 18 , 20 and an oral No Observed Adverse Effect Level (NOAEL) of 5 mg/kg/day in rats [the most sensitive species from 28‐day Good Laboratory Practice (GLP) safety studies]. We established an ~20‐fold safety factor for the starting dose using allometric conversions of rat to human doses following recommendations from the Food and Drug Administration (FDA). 23 A priori planned doses for subsequent cohorts were 2, 8, 16, and 32 mg, with an optional dose of 48 mg. The doses were escalated in a stepwise fashion following acceptable safety and tolerability reviews of the preceding dose(s) as determined by a Safety Review Committee (SRC). According to the PK stopping criteria established based on animal safety data, the SRC agreed to a final 5th dose level of 24 mg. Therefore, the optional cohort 6 at a dose of 48 mg was not enrolled in this study.
Separate groups of healthy volunteers were enrolled in each cohort, aiming at an approximately equal number of male and female participants per cohort (Table 1). In each cohort, 6 participants were randomly assigned to receive EC5026 and 2 participants received placebo. A blinded sentinel group of 2 participants (one active and one placebo) was dosed before the remaining 6 participants (5 active and one placebo). Blinding was maintained throughout the study by using active and placebo capsules of similar appearance.
TABLE 1.
Demographic characteristics of single‐ascending dose (SAD) study.
| EC5026 | Pooled placebo (N = 10) | Total (N = 40) | |||||
|---|---|---|---|---|---|---|---|
| 0.5 mg (N = 6) | 2 mg (N = 6) | 8 mg (N = 6) | 16 mg (N = 6) | 24 mg (N = 6) | |||
| Age (years) | |||||||
| Mean (SD) | 41.2 (11.02) | 36.8 (12.70) | 37.8 (16.53) | 40.7 (12.42) | 37.8 (6.43) | 41.9 (12.40) | 39.6 (11.66) |
| Minimum, maximum | 30, 58 | 20, 58 | 26, 62 | 25, 53 | 29, 46 | 22, 57 | 20, 62 |
| Sex, n (%) | |||||||
| Male | 4 (66.7) | 3 (50.0) | 2 (33.3) | 2 (33.3) | 2 (33.3) | 5 (50.0) | 18 (45.0) |
| Female | 2 (33.3) | 3 (50.0) | 4 (66.7) | 4 (66.7) | 4 (66.7) | 5 (50.0) | 22 (55.0) |
| Race, n (%) | |||||||
| White | 3 (50.0) | 3 (50.0) | 3 (50.0) | 5 (83.3) | 6 (100.0) | 6 (60.0) | 26 (65.0) |
| Black or African American | 3 (50.0) | 3 (50.0) | 3 (50.0) | 1 (16.7) | 0 | 4 (40.0) | 14 (35.0) |
| Ethnicity, n (%) | |||||||
| Hispanic or Latino | 2 (33.3) | 1 (16.7) | 2 (33.3) | 3 (50.0) | 5 (83.3) | 4 (40.0) | 17 (42.5) |
| Not Hispanic or Latino | 4 (66.7) | 5 (83.3) | 4 (66.7) | 3 (50.0) | 1 (16.7) | 6 (60.0) | 23 (57.5) |
| Height (cm) | |||||||
| Mean (SD) | 173.75 (13.1) | 169.88 (10.8) | 162.40 (5.4) | 164.88 (12.0) | 167.20 (10.7) | 171.08 (13.9) | 168.49 (11.5) |
| Minimum, maximum | 161.6, 194.2 | 152.6, 183.9 | 157.6, 172.4 | 152.8, 186.8 | 155.1, 184.4 | 153.8, 190.1 | 152.6, 194.2 |
| Weight (kg) | |||||||
| Mean (SD) | 76.88 (8.8) | 73.95 (19.0) | 67.12 (5.9) | 65.85 (10.5) | 68.20 (8.7) | 78.10 (11.2) | 72.33 (11.8) |
| Minimum, maximum | 60.7, 85.6 | 53.7, 101.7 | 57.2, 73.6 | 53.3, 81.9 | 58.4, 78.9 | 59.9, 96.9 | 53.3, 101.7 |
| Body mass index (kg/m 2 ) | |||||||
| Mean (SD) | 25.85 (5.16) | 25.30 (3.97) | 25.45 (1.70) | 24.23 (2.93) | 24.40 (2.03) | 26.74 (2.95) | 25.47 (3.21) |
| Minimum, maximum | 20.5, 31.7 | 19.9, 30.1 | 22.3, 26.8 | 20.9, 28.5 | 22.0, 27.6 | 21.2, 30.9 | 19.9, 31.7 |
Note: All percentages are based on the safety population within each treatment and overall.
Qualifying participants were admitted to the clinical trial site (Day −1) and received a single oral dose of EC5026 or placebo on the following day (Day 1). The study participants remained on the site until Day 5 and were monitored for safety and PK assessments at assigned intervals throughout the in‐house study period. After discharge, participants returned for follow‐ups of safety and additional blood draws on Day 7 and Day 14 (end‐of‐study). The study schema for each individual cohort is available in the supplemental material (Figure S1).
Fed‐fasted study (EC5026‐1‐03): Dose selection; overall clinical design
Study EC5026‐1‐03 was a phase Ia, single‐center, double‐blind, placebo‐controlled, single‐dose, fed‐fasted, crossover study to investigate the safety, tolerability, PK, and food effects on the PK after a single oral 8 mg dose of EC5026 in healthy male and female volunteers. The study was planned to have a single cohort of 18 participants, with approximately equal numbers of male and female participants.
The study comprised a screening period and 2 dosing periods (one in the fed state and one in the fasted state) consisting of an inpatient stage (Day −1 to Day 4) and a follow‐up stage (up to 28 days). Eligible participants were admitted on Day −1 of Dosing, Period 1, and randomly assigned at a ratio of 2:1 to active: placebo prior to dosing on Day 1. Within the EC5026 treatment group, participants were randomized 1:1 to one of 2 dosing sequences: Dosing Sequence A (dosed in a fed state in Dosing Period 1 and in a fasted state in Dosing Period 2) or Dosing Sequence B (fasted state in Dosing Period 1 and fed state in Dosing Period 2). Participants in the placebo group were also randomized 1:1 in a fed: fasted state in Dosing Period 1 (to maintain the double‐blind during Dosing Period 1) but did not return to the study site for dosing in Dosing Period 2. Dosing Period 2 was conducted on an unblinded basis, as only participants randomized to receive the active study drug returned to complete the fed‐fasted crossover trial.
In fasted conditions, the oral dose of EC5026 or placebo was administered with 240 mL of water following an overnight fast of at least 10 h. Additional water was allowed ad libitum except for 1 h before and after the administration of the drug. The study subjects did not consume any food for at least 4 h after the dose.
In fed conditions, following an overnight fast of at least 10 h, the study subjects started the recommended high‐fat breakfast meal 30 min before the drug administration. Study subjects completed this meal in 30 min or less. The oral dose of EC5026 or placebo was administered with 240 mL of water. Additional water was allowed ad libitum except for 1 h before and after drug administration. The study subjects did not consume any food for at least 4 h after the dose. Composition of the high‐fat breakfast meal is based on FDA recommendations and is provided in Appendix S1.
Each dosing period consisted of a day for check‐in (Day −1), a day for investigation drug administration (Day 1), an inpatient dosing and observation period (Days from 1 to 4), follow‐ups (Days from 5 to 21 for Dosing Period 1 and Days from 5 to 14 for Dosing Period 2), and a visit for the end‐of‐study (Day 21 of Dosing Period 1 for participants receiving placebo and Day 28 of Dosing Period 2 for participants receiving EC5026). There was a 3‐week washout period between the two dosing periods, starting on Day 1 of Dosing Period 1. The study schema is available in (Figure S1).
The end‐of‐study visit for subjects in the placebo treatment groups was on Day 21 (Period 1). Subjects in the placebo treatment groups did not return to the study site for Period 2. Subjects in the EC5026 treatment groups continued to Period 2 on Day 21 (Period 1), which was considered Day −1 in Period 2. The end‐of‐study visit for subjects in the EC5026 treatment groups was on Day 28 (Period 2).
To assess the impact of food on C max and AUC parameters, a linear mixed‐effect model was fitted to ln‐transformed data with treatment, sequence, and period as fixed effects and subject within sequence as a random effect. Fed/Fasted ratios were presented as percentages. Nonparametric methods (Wilcoxon signed‐rank test) were used to examine the differences in T max for EC5026 between fed‐fasted conditions. The Hodges‐Lehmann estimate and its 90% CI were calculated for the median difference between treatments, and a p‐value was generated by the Wilcoxon signed‐rank test.
Participant eligibility
Healthy male and female participants aged 18–70 years were enrolled in these studies. A full listing of Inclusion and Exclusion Criteria is provided in Appendix S1.
Study assessments
Safety and tolerability assessments included monitoring and recording of adverse events (AEs), vital sign measurements, clinical laboratory results (hematology, coagulation, serum chemistry, and urinalysis), 12‐lead ECGs results, ECG telemetry, and physical examination findings. All AEs reported during the study were listed, documenting course, severity, relationship to the study drug and outcome. AEs were coded using MedDRA Version 22.1. Additional exploratory safety assessments were included in the fed‐fasted study, as described in Appendix S1.
For the phase Ia SAD study, blood samples for the determination of plasma concentrations of EC5026 were collected at the following time points: pre‐dose (0 h), and at 1.25, 2.25, 4.25, 6.25, 8.25, 12.25, 24, 36, 48, 72, 84, 96, and 108 h after dosing. Additional blood samples were obtained on Day 8 and Day 14, or at early termination. For the Fed‐Fasted study, blood samples were obtained at pre‐dose (0 h), and at 0.5, 1.25, 2.25, 4.25, 6.25, 8.25, 12.25, 24, 36, 48, 72, 84, 96, and 108 h after dosing. Additional blood samples were obtained on Day 6, Day 8, Day 10, and Day 14, or at early termination.
Urine samples from the phase Ia SAD study were collected for analysis of EC5026 before dosing and 0–8 h, 8–16 h, 16–24 h, 24–32 h, 32–40 h, and 40–48 h after dosing.
PK samples were analyzed using a validated liquid chromatography coupled with tandem mass spectrometry assay for EC5026 in human plasma and urine. 24 Plasma and urine concentration–time data for EC5026 were analyzed by non‐compartmental analysis to determine PK parameters for the SAD study.
Statistical methods
Sample sizes for both studies were based on clinical and practical considerations and not on a formal statistical power calculation. 25 , 26 The safety population included all participants who received a single dose of EC5026. The PK population included participants who received a single dose of EC5026 and had sufficient concentration data to support an accurate estimation of at least one PK parameter. Participants were excluded from the PK population when there were fewer than three quantifiable plasma samples.
Non‐compartmental PK analyses were performed using Phoenix® WinNonlin® software version 8.0 (Certara USA, Inc., Princeton, NJ); statistical analyses of safety data were performed using SAS software version 9.4 (SAS Institute, Cary, North Carolina).
Detailed methods are available in Appendix S1.
RESULTS
Study population
SAD study
Forty healthy male and female volunteers were randomized (3:1, EC5026:placebo) and completed the study treatment between December 10, 2019, and July 3, 2020. One participant discontinued the study before completing follow‐up due to a coronavirus infection (COVID‐19) that was considered mild and was diagnosed during the outpatient follow‐up period. Overall, 55% of the study population was female and the mean age was 39.6 years (SD = 11.66 years, range 20–62 years). The majority of the participants were white (26/40; 65%) and 42.5% were Hispanic or Latino (17/40).
Fed‐fasted study
Eighteen healthy male and female volunteers were enrolled. Due to a dosing error on Day 1 (Period 1), 2 participants were randomized to receive placebo but received EC5026 treatment. Both subjects were included in the PK analysis for the active treatment. Fourteen participants (9 female and 5 male) were randomized to receive the active drug administered as an 8‐mg single oral dose, and 4 participants (2 female and 2 male) were randomized to receive a placebo. Overall, 61% of the population was female and the mean age was 44.2 years (SD = 10.84 years, range 26–63 years). The majority were white (15/18; 83.3%) and 44.4% were Hispanic or Latino (8/18).
The demographic characteristics of study participants for each study are summarized in Tables 1 and 2.
TABLE 2.
Demographic characteristics of fed‐fasted study.
| EC5026 (8 mg) | Placebo | Total (N = 18) | |||
|---|---|---|---|---|---|
| Sequence A | Sequence B | Sequence A | Sequence B | ||
| (N = 7) | (N = 7) | (N = 2) | (N = 2) | ||
| Age (years) | |||||
| Mean (SD) | 47.4 (13.02) | 40.6 (9.22) | 37.5 (7.78) | 52.0 (5.66) | 44.2 (10.84) |
| Minimum, maximum | 26, 63 | 31, 56 | 32, 43 | 48, 56 | 26, 63 |
| Sex, n (%) | |||||
| Male | 2 (28.6) | 3 (42.9) | 1 (50.0) | 1 (50.0) | 7 (38.9) |
| Female | 5 (71.4) | 4 (57.1) | 1 (50.0) | 1 (50.0) | 11 (61.1) |
| Race, n (%) | |||||
| White | 7 (100.0) | 5 (71.4) | 2 (100.0) | 1 (50.0) | 15 (83.3) |
| Black or African American | 0 | 1 (14.3) | 0 | 1 (50.0) | 2 (11.1) |
| Asian | 0 | 1 (14.3) | 0 | 0 | 1 (5.6) |
| Ethnicity, n (%) | |||||
| Hispanic or Latino | 4 (57.1) | 4 (57.1) | 0 | 0 | 8 (44.4) |
| Not Hispanic or Latino | 2 (28.6) | 3 (42.9) | 2 (100.0) | 2 (100.0) | 9 (50.0) |
| Not Reported | 1 (14.3) | 0 | 0 | 0 | 1 (5.6) |
| Height (cm) | |||||
| Mean (SD) | 162.01 (8.4) | 166.49 (8.5) | 175.55 (4.3) | 173.70 (3.5) | 166.91 (8.6) |
| Minimum, maximum | 153.1, 1 73.3 | 154.9, 177.1 | 172.5, 178.6 | 171.2, 176.2 | 153.1, 178.6 |
| Weight (kg) | |||||
| Mean (SD) | 70.21 (11.4) | 73.87 (12.3) | 78.05 (5.7) | 82.55 (13.5) | 73.88 (11.3) |
| Minimum, maximum | 56.3, 86.9 | 54.5, 94.4 | 74.0, 82.1 | 73.0, 92.1 | 54.5, 94.4 |
| Body mass index (kg/m 2 ) | |||||
| Mean (SD) | 26.40 (3.41) | 26.54 (3.04) | 25.30 (0.57) | 27.30 (3.39) | 26.43 (2.88) |
| Minimum, maximum | 22.6, 30.7 | 22.7, 30.8 | 24.9, 25.7 | 24.9, 29.7 | 22.6, 30.8 |
Note: All percentages are based on the safety population within each treatment and overall. Sequence A represents Fed‐Fasted sequence; Sequence B represents Fasted‐Fed sequence.
Safety and tolerability
SAD study
Single doses of 0.5, 2, 8, 16, and 24 mg EC5026 were well tolerated. Overall, 19 of 40 participants (47.5%) reported at least one treatment‐emergent adverse event (TEAE) during the study (Table 3). No TEAE was considered related to the study treatment. The most common TEAEs were dermatitis related to ECG electrode placement (12/40; 30.0%) followed by headache (3/40; 7.5%). With the exception of two TEAEs of medical device site dermatitis that were considered to be of moderate intensity, all TEAEs were mild in severity. No severe AEs were reported during the study. With the exception of one TEAE (ventricular extrasystoles) that was considered mild and not related to the study drug, all TEAEs were resolved by the end of the study. No apparent treatment‐ or dose‐related trends were observed in clinical laboratory test results (hematology, coagulation, serum chemistry, or urinalysis), vital sign measurements, physical examination findings, or 12‐lead ECG results.
TABLE 3.
Treatment‐emergent adverse events in phase Ia SAD study.
| EC5026 | Pooled placebo (n = 10) | Total (n = 40) | |||||
|---|---|---|---|---|---|---|---|
| 0.5 mg (n = 6) | 2 mg (n = 6) | 8 mg (n = 6) | 16 mg (n = 6) | 24 mg (n = 6) | |||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| AE summary | |||||||
| Any AE | 2 (33.3) | 4 (66.7) | 3 (50.0) | 6 (100.0) | 4 (66.7) | 5 (50.0) | 24 (60.0) |
| Any TEAE | 2 (33.3) | 4 (66.7) | 2 (33.3) | 4 (66.7) | 4 (66.7) | 3 (30.0) | 19 (47.5) |
| Any moderate TEAE | 0 | 1 (16.7) | 0 | 0 | 0 | 1 (10.0) | 2 (5.0) |
| Any severe TEAE | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Any serious TEAE | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Any treatment‐related TEAE | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| AE by system organ class | |||||||
| General disorders and administration site conditions | |||||||
| Medical device site dermatitis | 0 | 2 (33.3) | 0 | 4 (66.7) | 3 (50.0) | 3 (30.0) | 12 (30.0) |
| Feeling hot | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 1 (2.5) |
| Infections and infestation | |||||||
| Coronavirus infection (COVID‐19) | 0 | 0 | 0 | 0 | 1 (16.7) | 0 | 1 (2.5) |
| Laryngitis | 1 (16.7) | 0 | 0 | 0 | 0 | 0 | 1 (2.5) |
| Trichomoniasis | 0 | 1 (16.7) | 0 | 0 | 0 | 0 | 1 (2.5) |
| Urinary tract infection | 1 (16.7) | 0 | 0 | 0 | 0 | 0 | 1 (2.5) |
| Nervous system disorders | |||||||
| Headache | 1 (16.7) | 1 (16.7) | 0 | 0 | 1 (16.7) | 0 | 3 (7.5) |
| Cardiac disorders | |||||||
| Palpitations | 0 | 1 (16.7) | 0 | 0 | 0 | 0 | 1 (2.5) |
| Ventricular extrasystoles | 0 | 1 (16.7) | 0 | 0 | 0 | 0 | 1 (2.5) |
| Injury, poisoning and procedural complications | |||||||
| Limb injury | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 1 (2.5) |
| Psychiatric disorders | |||||||
| Insomnia | 0 | 0 | 0 | 0 | 0 | 1 (10.0) | 1 (2.5) |
| Renal and urinary disorders | |||||||
| Dysuria | 0 | 0 | 0 | 0 | 1 (16.7) | 0 | 1 (2.5) |
| Respiratory, thoracic and mediastinal disorders | |||||||
| Dyspnea | 0 | 1 (16.7) | 0 | 0 | 0 | 0 | 1 (2.5) |
A detailed listing of AEs from the SAD study is provided in Table S1.
Fed‐fasted study
A single oral dose of 8 mg EC5026 administered in tablet form was well tolerated in the study participants in both fasted and fed states. Three of 18 participants (16.7%) reported at least one TEAE during the study (Table 4). No TEAE was considered related to study treatment. The reported TEAEs were photophobia (1/18; 5.5%), injection site reactions following adrenocorticotrophic hormone (ACTH) stimulation test (1/18; 5.5%), urinary tract infection (1/18; 5.5%), and headache (1/18; 5.5%). All TEAEs were mild in severity and resolved. Therefore, no participants were discontinued from the study due to a TEAE. No apparent treatment‐related trends in clinical laboratory test results (hematology, coagulation, serum chemistry, or urinalysis), vital sign measurements, physical examination findings, or 12‐lead ECG results were observed.
TABLE 4.
Treatment‐emergent adverse events in phase Ia fed‐fasted study.
| EC5026 (8 mg) | Placebo | |||
|---|---|---|---|---|
| Fed (n = 14) | Fasted (n = 13) | Fed (n = 2) | Fasted (n = 2) | |
| n (%) | n (%) | n (%) | n (%) | |
| AE summary | ||||
| Any AE | 2 (14.3) | 1 (7.7) | 0 | 0 |
| Any TEAE | 2 (14.3) | 1 (7.7) | 0 | 0 |
| Any Moderate TEAE | 0 | 0 | 0 | 0 |
| Any Severe TEAE | 0 | 0 | 0 | 0 |
| Any Serious TEAE | 0 | 0 | 0 | 0 |
| Any Treatment‐Related TEAE | 0 | 0 | 0 | 0 |
| AE by system organ class | ||||
| General disorders and administration site conditions | ||||
| Injection site reaction | 1 (7.1) | 0 | 0 | 0 |
| Infections and infestation | ||||
| Urinary tract infection | 0 | 1 (7.7) | 0 | 0 |
| Nervous system disorders | ||||
| Headache | 1 (7.1) | 0 | 0 | 0 |
| Eye disorders | ||||
| Photophobia | 1 (7.1) | 0 | 0 | 0 |
A detailed listing of AEs from the fed‐fasted study is provided in Table S2.
Pharmacokinetics
SAD study
Following single oral dose administration of EC5026, peak plasma concentrations were rapidly reached with the median time to maximum concentration (T max) of 1.25 hours across all dose groups. Thereafter, plasma concentrations declined slowly (mean terminal half‐lives of ~2.6 days as indicated above); PK values were recorded through 14 days after dosing. Plasma concentrations following 0.5 mg of EC5026 were below the limit of quantification for all participants at all time points. For two participants in the EC5026 2 mg dose group, plasma concentrations were quantifiable in fewer than three samples. These participants were excluded from the PK population by study design. Mean plasma concentrations of EC5026 vs. time are presented in Figure S2 in the Supplemental Material.
Geometric mean peak (C max) and total (AUC0–t ) exposures increased with increasing doses from 2 to 24 mg (Table 5). At the 2 mg dose level, plasma exposures were highly variable due to concentrations being near the lower limit of quantification with geometric coefficient of variation (CV) values of 45.8% (C max) and 145.4% (AUC0–t ). For the dose range of 8–24 mg, there was low‐to‐moderate variability in plasma exposures with geometric CV values ranging from 11.1% to 16.2% (C max) and 22.1%–28.4% (AUC0–t ). The mean half‐life (t 1/2) was 143 h at the 2 mg dose level and decreased as the dose increased. The mean t 1/2 values for the 8, 16, and 24 mg dose groups were 59.1, 44.8, and 41.8 h, respectively. Given that plasma concentrations for the 2 mg dose group were near the limit of quantification, the estimates for t ½ at the two lowest doses should be viewed with caution. The mean apparent total body clearance (CL/F) and volume of distribution (Vz/F) were similar across dose groups at 8–24 mg, with mean CL/F values ranging from 2.23 to 2.62 L/h and Vz/F values ranging from 146 to 178 L.
TABLE 5.
PK parameters of EC5026 in phase Ia SAD study.
| Parameter (unit) | EC5026 | |||
|---|---|---|---|---|
| 2 mg (N = 4) | 8 mg (N = 6) | 16 mg (N = 6) | 24 mg (N = 6) | |
| C max (ng/mL) | 4.69 (45.8) | 82.7 (11.1) | 220 (16.2) | 301 (14.6) |
| T max (h) | 1.25 (1.25, 1.30) | 1.25 (1.25, 1.30) | 1.25 (1.25, 1.25) | 1.25 (1.25, 1.25) |
| AUC0–t (ng•h/mL) | 258 (145.4) | 3450 (28.4) | 6780 (23.1) | 9030 (22.1) |
| AUC0–inf (ng•h/mL) | NC | 3690 (26.3) | 6960 (22.1) | 9310 (21.1) |
| AUC0‐48 (ng•h/mL) | 119 (59.7) | 1870 (7.9) | 4450 (14.7) | 6130 (13.4) |
| t ½ (h) | 143 (44.3) a | 59.1 (32.2) | 44.8 (31.3) | 41.8 (34.9) |
| CL/F (L/h) | NC | 2.23 (25.2) | 2.35 (22.2) | 2.62 (20.8) |
| Vz/F (L) | NC | 178 (11.8) | 146 (23.6) | 153 (6.3) |
Note: Data are presented as geometric mean (geometric CV) except for t ½, CL/F and Vz/F, which are arithmetic mean (arithmetic CV). For T max, the median (minimum, maximum) values are presented. Subjects were excluded from the PK population when there were fewer than 3 quantifiable plasma samples. All concentrations were below the limit of quantification for the EC5026 0.5 mg dose group. Values for AUC0–inf, CL/F, and Vz/F were excluded from summary statistics when %AUCextrap was >20%.
Abbreviation: NC, not calculated.
n = 3; given that plasma concentrations for the 2 mg dose group were near the limit of quantification, the estimates for t½ should be viewed with caution.
Exposure parameters (C max and AUC) increased in a greater‐than‐dose‐proportional manner from 2 to 24 mg, and based on statistical analysis the 90% CI of the slope was not contained within the criteria for dose proportionality (0.91, 1.09) for C max, AUC0–t , or AUC0–48 (Table 6). When considering only the dose range from 8 to 24 mg, exposure parameters (C max and AUC) of EC5026 increased in a near‐dose‐proportional manner (Table 6). Based on statistical analysis of dose proportionality for EC5026 exposure over the dose range of 8–24 mg, the 90% CI of the slope (1.06, 1.35) fell outside the upper limit of the criteria for dose proportionality (0.80, 1.20) for C max and 90% CI of the slope (0.98, 1.22) fell just outside the upper limit of the criteria for dose proportionality (0.80, 1.20) for AUC0–48. For AUC0–t and AUC0–inf, the 90% CI of the slope ([AUC0–t 0.67, 1.10], [AUC0–inf 0.65, 1.05]) fell outside the lower limit of the criteria for dose proportionality (0.80, 1.20).
TABLE 6.
Statistical analysis of dose proportionality for EC5026 based on SAD study.
| Dose range | Parameter (units) | Estimated slope | Standard error of the slope | 90% CI of the slope | Dose proportionality criteria |
|---|---|---|---|---|---|
| 2–24 mg | C max (ng/mL) | 1.69 | 0.080 | (1.55, 1.83) | (0.91, 1.09) |
| AUC0–t (ng•h/mL) | 1.43 | 0.131 | (1.20, 1.65) | (0.91, 1.09) | |
| AUC0–48 (ng•h/mL) | 1.59 | 0.084 | (1.45, 1.74) | (0.91, 1.09) | |
| 8–24 mg | C max (ng/mL) | 1.20 | 0.082 | (1.06, 1.35) | (0.80, 1.20) |
| AUC0–t (ng•h/mL) | 0.89 | 0.124 | (0.67, 1.10) | (0.80, 1.20) | |
| AUC0–48 (ng•h/mL) | 1.10 | 0.069 | (0.98, 1.22) | (0.80, 1.20) | |
| AUC0–inf (ng•h/mL) | 0.85 | 0.116 | (0.65, 1.05) | (0.80, 1.20) |
Note: Subjects were excluded from the PK population when there were fewer than 3 quantifiable plasma samples. Values for AUC0–inf were excluded from summary statistics when %AUCextrap was >20%. The power model, ln(parameter) = intercept + slope × ln(dose), was used to estimate the slope and corresponding 90% CI. Dose proportionality was concluded if the 90% CI of the slope (β) lies entirely within [1 + ln(0.8)/ln(r), 1 + ln(1.25)/ln(r)], where r is the dose range (highest dose/lowest dose).
Urine concentrations of EC5026 were below the limit of quantification for all participants and all timepoints for the 0.5 and 2 mg dose groups. For the 8, 16, and 24 mg dose groups, the total amount of EC5026 excreted in urine over 48 h (Ae0–48) was low and ranged from 0.0127 to 0.0487 mg, corresponding to 0.132%–0.203% of the EC5026 dose.
Fed‐fasted study
Following a single oral dose of 8 mg EC5026 in either the fed or fasted state, mean plasma concentration vs. time profiles of EC5026 were characterized by a rapid absorption phase until C max, followed by a steady monophasic decline through 312 hours (13 days) after dosing with arithmetic mean (t 1/2) of 59.5 and 66.9 h, respectively (Figure S3 in the Supplemental Material and Table 7).
TABLE 7.
PK parameters of EC5026 in phase Ia fed‐fasted study.
| Parameter (unit) | EC5026 treatment group | |
|---|---|---|
| Fed (N = 14) | Fasted (N = 13) | |
| n | 13 a | 13 b |
| C max (ng/mL) | 55.6 (23.3) | 35.0 (32.1) |
| T max (h) | 8.25 (4.25, 24.17) | 4.25 (1.28, 36.00) |
| AUC0–t (ng•h/mL) | 4120 (20.5) | 3120 (23.2) |
| AUC0–inf (ng•h/mL) | 4260 (20.2) | 3260 (22.0) |
| AUC0–48 (ng•h/mL) | 1930 (20.1) | 1310 (25.2) |
| t 1/2 (h) | 59.5 (17.7) | 66.9 (17.2) |
| CL/F (L/h) | 1.91 (19.4) | 2.51 (23.3) |
| Vz/F (L) | 164 (43.7) | 244 (30.6) |
Note: Fed Treatment = 8 mg single oral dose of EC5026 in the fed state; Fasted Treatment = 8 mg single oral dose of EC5026 in the fasted state. Data are presented as geometric mean (geometric CV) except for t 1/2, CL/F, and Vz/F, which are arithmetic mean (arithmetic CV). For T max, the median (minimum, maximum) values are presented.
One subject received a pre‐dose meal 70 minutes prior to dosing (40 minutes outside of the window) in Period 1 (Fed Treatment); therefore, that subject was excluded from the calculation of summary statistics for the Fed Treatment.
One subject was dosed as planned in Period 1 (Fed Treatment) and was included in the calculation of summary statistics for the Fed Treatment but was withdrawn prior to Period 2 (Fasted Treatment).
Peak and total exposures (C max, AUC0–48, AUC0–t , and AUC0–inf) to EC5026 were 34%–66% higher under fed conditions compared with those under fasted conditions. The 90% CIs around the ratio excluded unity in all instances and p‐values were <0.05, indicating that the difference was statistically significant (Table 8). The difference between the median T max estimates, as determined from the Hodges‐Lehman estimate, was small (0.08 h) and not statistically significant (p‐value = 0.9375).
TABLE 8.
Statistical analysis of plasma PK parameters of EC5026 based on fed‐fasted study.
| Pharmacokinetic parameter (units) | Treatment | n a | Geometric LS means | Ratio (%) of geometric LS means | 90% CI of the ratio | p‐Value | Intra‐subject CV% |
|---|---|---|---|---|---|---|---|
| Cmax (ng/mL) | Fed | 12 | 58.6 | 165.75 | (137.50, 199.80) | 0.0001 | 26.6 |
| Fasted | 12 | 35.3 | |||||
| AUC0–48 (ng•h/mL) | Fed | 12 | 2020 | 152.75 | (133.36, 174.95) | 0.0002 | 18.2 |
| Fasted | 12 | 1320 | – | – | – | – | |
| AUC0–t (ng•h/mL) | Fed | 12 | 4200 | 135.22 | (119.77, 152.67) | 0.0011 | 16.3 |
| Fasted | 12 | 3100 | – | – | – | – | |
| AUC0–inf (ng•h/mL) | Fed | 12 | 4330 | 133.76 | (119.26, 150.03) | 0.0010 | 15.4 |
| Fasted | 12 | 3240 | – | – | – | – |
Note: Fed Treatment = 8 mg single oral dose of EC5026 in the fed state; Fasted Treatment = 8 mg single oral dose of EC5026 in the fasted state. A linear mixed‐effect model was fitted to ln‐transformed data with treatment, sequence, and period as fixed effects and subject within sequence as a random effect; results are presented as percentages.
n is the number of subjects with non‐missing values for both Fed and Fasted treatments. Two subjects were excluded from the statistical analysis as only data for one treatment were available for each subject; one subject received a pre‐dose meal 70 minutes prior to dosing (40 minutes outside of the window) in Period 1 (Fed Treatment), and another subject was dosed as planned in Period 1 (Fed Treatment) but was withdrawn prior to Period 2 (Fasted Treatment). Geometric LS Means are derived from ln‐transformed Least Squares Means data.
Arithmetic mean CL/F values were 1.91 and 2.51 L/h in the fed and fasted states, respectively, and arithmetic mean Vz/F values were 164 and 244 L, respectively (Table 7). Between‐subject variability in systemic exposure to EC5026 was low‐to‐moderate for both the fed and fasted states, with geometric CV values for C max and all AUC parameters ranging from 20.1%–32.1% across both treatments. Within‐subject variability in systemic exposure to EC5026, as assessed by the linear mixed‐effect model, was low, ranging from 15.4% to 26.6% (Table 8).
DISCUSSION
These two studies represent the first‐in‐human phase Ia clinical trials of oral EC5026 in healthy male and female volunteers. EC5026 was well tolerated after a single oral dose of either 0.5, 2, 8, 16, or 24 mg and also 8 mg in both the fed and fasted states. No treatment‐emergent adverse events (TEAEs) were considered related to EC5026 in either study. In addition, no apparent treatment‐ or dose‐related trends were observed in clinical laboratory test results, vital sign measurements, physical examination findings, or 12‐lead ECG results.
A linear, near‐dose‐proportional increase in exposure was observed with single oral EC5026 doses from 8 to 24 mg in the phase Ia SAD study. However, plasma exposures of EC5026 were below the limit of quantification following a 0.5 mg dose for all participants and were highly variable from four participants at the 2 mg dose level. Mean half‐lives after a single dose of 8, 16, and 24 mg ranged from 41.8 to 59.1 h, supporting a once‐daily dosing regimen. Overall, these PK findings may represent the presence of target‐mediated drug disposition (TMDD), which is a phenomenon known to affect some potent small molecule drugs with high affinity to their pharmacologic target. 27 , 28 For TMDD to occur, in addition to having high affinity for its target, a compound needs to bind to it specifically, without substantial non‐specific tissue binding happening concurrently. In these cases, when a low dose is given, a significant proportion of the dose is sequestered by the target, leaving only a small amount available in the systemic circulation. When the dose increases, the proportion of a dose sequestered by the target decreases in terms of the total dose, and more of it becomes available for systemic circulation. 27 This phenomenon results in linear dose‐proportional PK only at higher doses, with non‐linearity present at low, single doses.
In the fed‐fasted study, after an oral dose of 8 mg of EC5026 administered in tablet form, peak (66%) and total exposures (53%) to EC5026 under fed conditions were significantly higher compared with those under fasted conditions. The median T max values were observed slightly later under fed conditions, but the difference in the median T max (0.08 hour) was not statistically significant. In addition, EC5026 concentrations declined in a monoexponential manner in both the fed and fasted state, with arithmetic mean apparent terminal half‐lives (t 1/2) of 59.5 and 66.9 h, respectively.
Pain is one of the most common reasons why people seek medical attention. 29 In the United States, at least 20% of the population is affected by chronic pain at any one time 1 and the national economic cost of pain has been estimated to range from $560 to $635 billion annually. 30 Chronic pain of different etiologies results in an incrementally increased burden to patients beyond that of the underlying condition that causes it. 31 , 32 , 33 , 34 , 35 In 2018, the FDA held a public meeting to hear perspectives from patients living with chronic pain. 3 The patient input generated through this effort underscored the devastating toll chronic pain takes on all aspects of the patients' lives, including the loss or significant changes to their careers, limited social interactions, financial challenges, decreased ability to perform common activities, decreased quality of life, and the emotional burden of living with chronic pain. 3 Chronic pain patients emphasized the difficulty in achieving pain relief and the need for effective, non‐opioid treatment options. In fact, despite the high prevalence and the associated individual, economic, and societal burden of disease, chronic pain is generally poorly managed by a limited number of existing therapeutic interventions. 4 , 5 , 6 Inadequate response to drug treatments in many patients constitutes a substantial unmet need, particularly in patients with neuropathic pain. 6 Improved pain management approaches are needed to address this issue and improve the health and well‐being of those affected by chronic pain. This unmet need reflects a pressing demand to develop novel classes of analgesics that are effective and have diminished adverse effects and a lower abuse liability than currently available treatments.
Currently, available pharmacologic therapies for chronic pain include nonsteroidal anti‐inflammatory drugs (NSAIDs), antiepileptic drugs (i.e., gabapentin or pregabalin), selected antidepressants (i.e., tricyclic antidepressants and serotonin–norepinephrine reuptake inhibitors), and opioids. These treatment options have varying levels of analgesic efficacy, typically providing only partial relief to most patients, and generally associated with multiple undesirable adverse effects. Opioids are one of the most commonly prescribed medication classes for patients with chronic pain but have limited efficacy in noncancer chronic pain. 9 Opioids may be associated with serious adverse effects, and with continued dosing, produce tolerance, dependence, and abuse liability. 7 , 8 , 36 There is widespread recognition of the need for novel, effective, and non‐addictive analgesics for chronic pain. Ideally, novel therapeutics should mimic or target endogenous pain‐resolution mechanisms. 37
More than half of the currently available analgesic drugs act on the cyclooxygenase (COX) and lipoxygenase (LOX) pathways of the arachidonic acid cascade. Of these, the COX branch has been the most studied and predominantly exploited by NSAIDs and COX‐2 inhibitors. sEH inhibitors work on the more recently discovered CYP450 branch that is largely an analgesic and inflammation‐resolving branch of the cascade. This novel pathway is unique to any of the available therapies for chronic pain. The approach is based on the recognition that EpFAs are potent, naturally occurring analgesics that are rapidly degraded by the sEH enzyme. 38 sEH inhibition may increase plasma and cellular levels of EpFAs to therapeutic levels and prolong their duration of activity from minutes to hours or days. The increased levels of EpFAs have been proven to act at the cellular level to reduce pain, resolve inflammation, and maintain endothelial function. 38 The underlying mechanism of action involves limiting endoplasmic reticulum (ER) stress and protecting against mitochondrial dysfunction, thereby supporting cellular homeostasis and functioning as well as limiting inflammation. 39 , 40 , 41 Pharmacological inhibition of sEH has been shown to increase the concentration of beneficial EpFAs, producing strong analgesic effects in animal models of acute and chronic neuropathic and inflammatory pain. 15 , 16 , 38 , 42 Notably, studies of sEH inhibition in chronic pain assessing the addictive potential of sEH inhibition‐mediated analgesia showed no reward‐seeking behavior. 15 Additional studies using local administration of EpFAs demonstrated both analgesic efficacy against neuropathic pain as well as a lack of rewarding side effects. 42 EC5026 is the first sEH inhibitor being developed for the treatment of pain in humans. 18 Our data show that EC5026 produces potent analgesia and a favorable dose–response relationship in multiple preclinical neuropathic pain and inflammatory pain models, and safety pharmacology studies have not identified any central nervous system, respiratory, or cardiovascular risks. 18
CONCLUSION
EC5026 was well tolerated in healthy volunteers at single doses up to 24 mg and showed linear and near‐dose‐proportional PK properties (results of the SAD study). Food may delay time to peak activity, but has only a modest but statistically significant impact of increased C max and AUC values (results from the fed‐fasted study). This safety profile and PK data, together with the mechanistic and preclinical evidence of analgesic activity, suggest that future clinical trials of EC5026 for the treatment of pain are justified. EC5026 is currently being evaluated in a phase Ib multiple ascending dose (MAD) study in healthy volunteers and is planned to be investigated soon in two pilot studies of participants with chronic inflammatory pain (osteoarthritis) or neuropathic pain (spinal cord injury) in future nested‐design MAD studies.
AUTHOR CONTRIBUTIONS
I.C‐P., C.B.M., and W.K.S. wrote the manuscript. I.C‐P., W.K.S., C.B.M., J.Y., T.L.P., and B.D.H. designed the research. T.T.P. and T.H. performed the research. I.C‐P., W.K.S., C.B.M., G.E.C., S.H.H., and K.M.W. analyzed the data.
FUNDING INFORMATION
Funding for this study was provided by the National Institute of Environmental Health Sciences (NIEHS) grant R44 ES025598, by Blueprint Neurotherapeutics Grant 3UH2NS094258 from the National Institute of Neurological Disorders and Stroke (NINDS), and by HEAL grant UG3DA048767 from the NINDS.
CONFLICT OF INTEREST STATEMENT
WKS, ICP, CBM, GEC, SHH, JY, TLP, KMW, and BDH were employees of EicOsis Human Health at the time that this study was conducted and own stock or hold stock options in EicOsis Human Health. TTP and TH were employees of PPD and declared no competing interests for this work.
Supporting information
Appendix S1.
Schmidt WK, Cortés‐Puch I, McReynolds CB, et al. Randomized, double‐blind, phase 1a single‐ascending dose and food effect studies assessing safety and pharmacokinetics of EC5026 in healthy volunteers. Clin Transl Sci. 2024;17:e70033. doi: 10.1111/cts.70033
ClinicalTrials.gov Identifiers: NCT04228302 (SAD study) and NCT04908995 (fed‐fasted study).
REFERENCES
- 1. Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high‐impact chronic pain among U.S. adults, 2019. NCHS Data Brief. 2020;390:1‐8. [PubMed] [Google Scholar]
- 2. Duenas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457‐467. doi: 10.2147/JPR.S105892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Center for Drug Evaluation and Research (CDER), U.S. Food and Drug Administration (FDA) . The Voice of the Patient. Chronic Pain. Report Date: March 2019.
- 4. Reid KJ, Harker J, Bala MM, et al. Epidemiology of chronic non‐cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr Med Res Opin. 2011;27(2):449‐462. doi: 10.1185/03007995.2010.545813 [DOI] [PubMed] [Google Scholar]
- 5. Moore A, Derry S, Eccleston C, Kalso E. Expect analgesic failure; pursue analgesic success. BMJ. 2013;346:f2690. doi: 10.1136/bmj.f2690 [DOI] [PubMed] [Google Scholar]
- 6. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta‐analysis. Lancet Neurol. 2015;14(2):162‐173. doi: 10.1016/S1474-4422(14)70251-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boscarino JA, Withey CA, Dugan RJ, Hu Y, Auciello J, Alfieri T. Opioid medication use among chronic non‐cancer pain patients assessed with a modified drug effects questionnaire and the association with opioid use disorder. J Pain Res. 2020;13:2697‐2705. doi: 10.2147/JPR.S275397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569‐576. doi: 10.1097/01.j.pain.0000460357.01998.f1 [DOI] [PubMed] [Google Scholar]
- 9. Busse JW, Wang L, Kamaleldin M, et al. Opioids for chronic noncancer pain: a systematic review and meta‐analysis. JAMA. 2018;320(23):2448‐2460. doi: 10.1001/jama.2018.18472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McReynolds CB, Hwang SH, Yang J, et al. Pharmaceutical effects of inhibiting the soluble epoxide hydrolase in canine osteoarthritis. Front Pharmacol. 2019;10:533. doi: 10.3389/fphar.2019.00533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wagner K, Inceoglu B, Gill SS, Hammock BD. Epoxygenated fatty acids and soluble epoxide hydrolase inhibition: novel mediators of pain reduction. J Agric Food Chem. 2011;59(7):2816‐2824. doi: 10.1021/jf102559q [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Inceoglu B, Jinks SL, Schmelzer KR, Waite T, Kim IH, Hammock BD. Inhibition of soluble epoxide hydrolase reduces LPS‐induced thermal hyperalgesia and mechanical allodynia in a rat model of inflammatory pain. Life Sci. 2006;79(24):2311‐2319. doi: 10.1016/j.lfs.2006.07.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McReynolds C, Hammock B, Morisseau C. Regulatory lipid vicinal diols counteract the biological activity of epoxy fatty acids and can act as biomarkers and mechanisms for disease progression. Pharmacol Ther. 2023;248:108454. doi: 10.1016/j.pharmthera.2023.108454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Inceoglu B, Wagner KM, Yang J, et al. Acute augmentation of epoxygenated fatty acid levels rapidly reduces pain‐related behavior in a rat model of type I diabetes. Proc Natl Acad Sci USA. 2012;109(28):11390‐11395. doi: 10.1073/pnas.1208708109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wagner K, Yang J, Inceoglu B, Hammock BD. Soluble epoxide hydrolase inhibition is antinociceptive in a mouse model of diabetic neuropathy. J Pain. 2014;15(9):907‐914. doi: 10.1016/j.jpain.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wagner K, Gilda J, Yang J, et al. Soluble epoxide hydrolase inhibition alleviates neuropathy in Akita (Ins2 Akita) mice. Behav Brain Res. 2017;326:69‐76. doi: 10.1016/j.bbr.2017.02.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guedes AG, Morisseau C, Sole A, et al. Use of a soluble epoxide hydrolase inhibitor as an adjunctive analgesic in a horse with laminitis. Vet Anaesth Analg. 2013;40(4):440‐448. doi: 10.1111/vaa.12030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hammock BD, McReynolds CB, Wagner K, et al. Movement to the Clinic of Soluble Epoxide Hydrolase Inhibitor EC5026 as an analgesic for neuropathic pain and for use as a nonaddictive opioid alternative. J Med Chem. 2021;64(4):1856‐1872. doi: 10.1021/acs.jmedchem.0c01886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee KSS, Ng JC, Yang J, et al. Preparation and evaluation of soluble epoxide hydrolase inhibitors with improved physical properties and potencies for treating diabetic neuropathic pain. Bioorg Med Chem. 2020;28(22):115735. doi: 10.1016/j.bmc.2020.115735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Takeshita AA, Hammock BD, Wagner KM. Soluble epoxide hydrolase inhibition alleviates chemotherapy induced neuropathic pain. Front Pain Res (Lausanne). 2022;3:1100524. doi: 10.3389/fpain.2022.1100524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wagner KM, Atone J, Hammock BD. Soluble epoxide hydrolase inhibitor mediated analgesia lacks tolerance in rat models. Brain Res. 2020;1728:146573. doi: 10.1016/j.brainres.2019.146573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wan X, Fujita Y, Chang L, et al. Lack of rewarding effects of a soluble epoxide hydrolase inhibitor TPPU in mice: comparison with morphine. Neuropsychopharmacol Rep. 2020;40(4):412‐416. doi: 10.1002/npr2.12136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. US Food and Drug Administration's Guidance for Industry: estimating the maximum safe starting dose in initial clinical trials for therapeutics in adult healthy volunteers. https://www.fda.gov/media/72309/download
- 24. FDA . Bioanalytical method validation guidance for industry, guidance document. Accessed 6/15/2019. https://www.fda.gov/regulatory‐information/search‐fda‐guidance‐documents/bioanalytical‐method‐validation‐guidance‐industry
- 25. Shen J, Swift B, Mamelok R, Pine S, Sinclair J, Attar M. Design and conduct considerations for first‐in‐human trials. Clin Transl Sci. 2019;12(1):6‐19. doi: 10.1111/cts.12582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Department of Health and Human Services (DHHS), Food and Drug Administration, Center for Drug Evaluation and Research (CDER) . Guidance document: assessing the effects of food on drugs in INDs and NDAs — clinical pharmacology considerations. Guidance for Industry; 2022. Accessed 2022 Oct 12. https://www.fda.gov/regulatory‐information/search‐fda‐guidance‐documents/assessing‐effects‐food‐drugs‐inds‐and‐ndas‐clinical‐pharmacology‐considerations [Google Scholar]
- 27. An G. Concept of pharmacologic target‐mediated drug disposition in large‐molecule and small‐molecule compounds. J Clin Pharmacol. 2020;60(2):149‐163. doi: 10.1002/jcph.1545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Levy G. Pharmacologic target‐mediated drug disposition. Clin Pharmacol Ther. 1994;56(3):248‐252. doi: 10.1038/clpt.1994.134 [DOI] [PubMed] [Google Scholar]
- 29. Dubois MY, Gallagher RM, Lippe PM. Pain medicine position paper. Pain Med. 2009;10(6):972‐1000. doi: 10.1111/j.1526-4637.2009.00696.x [DOI] [PubMed] [Google Scholar]
- 30. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715‐724. doi: 10.1016/j.jpain.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 31. Choiniere M, Dion D, Peng P, et al. The Canadian STOP‐PAIN project – part 1: who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):539‐548. doi: 10.1007/s12630-010-9305-5 [DOI] [PubMed] [Google Scholar]
- 32. Rapti E, Damigos D, Apostolara P, Roka V, Tzavara C, Lionis C. Patients with chronic pain: evaluating depression and their quality of life in a single center study in Greece. BMC Psychol. 2019;7(1):86. doi: 10.1186/s40359-019-0366-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Domenichiello AF, Ramsden CE. The silent epidemic of chronic pain in older adults. Prog Neuro‐Psychopharmacol Biol Psychiatry. 2019;93:284‐290. doi: 10.1016/j.pnpbp.2019.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vartiainen P, Heiskanen T, Sintonen H, Roine RP, Kalso E. Health‐related quality of life and burden of disease in chronic pain measured with the 15D instrument. Pain. 2016;157(10):2269‐2276. doi: 10.1097/j.pain.0000000000000641 [DOI] [PubMed] [Google Scholar]
- 35. Langley PC, Van Litsenburg C, Cappelleri JC, Carroll D. The burden associated with neuropathic pain in Western Europe. J Med Econ. 2013;16(1):85‐95. doi: 10.3111/13696998.2012.729548 [DOI] [PubMed] [Google Scholar]
- 36. Volkow ND, McLellan AT. Opioid abuse in chronic pain–misconceptions and mitigation strategies. N Engl J Med. 2016;374(13):1253‐1263. doi: 10.1056/NEJMra1507771 [DOI] [PubMed] [Google Scholar]
- 37. Price TJ, Basbaum AI, Bresnahan J, et al. Transition to chronic pain: opportunities for novel therapeutics. Nat Rev Neurosci. 2018;19(7):383‐384. doi: 10.1038/s41583-018-0012-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wagner KM, McReynolds CB, Schmidt WK, Hammock BD. Soluble epoxide hydrolase as a therapeutic target for pain, inflammatory and neurodegenerative diseases. Pharmacol Ther. 2017;180:62‐76. doi: 10.1016/j.pharmthera.2017.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Inceoglu B, Bettaieb A, Trindade da Silva CA, Lee KS, Haj FG, Hammock BD. Endoplasmic reticulum stress in the peripheral nervous system is a significant driver of neuropathic pain. Proc Natl Acad Sci USA. 2015;112(29):9082‐9087. doi: 10.1073/pnas.1510137112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. El‐Sikhry HE, Alsaleh N, Dakarapu R, Falck JR, Seubert JM. Novel roles of Epoxyeicosanoids in regulating cardiac mitochondria. PLoS One. 2016;11(8):e0160380. doi: 10.1371/journal.pone.0160380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Inceoglu B, Bettaieb A, Haj FG, Gomes AV, Hammock BD. Modulation of mitochondrial dysfunction and endoplasmic reticulum stress are key mechanisms for the wide‐ranging actions of epoxy fatty acids and soluble epoxide hydrolase inhibitors. Prostaglandins Other Lipid Mediat. 2017;133:68‐78. doi: 10.1016/j.prostaglandins.2017.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wagner K, Lee KS, Yang J, Hammock BD. Epoxy fatty acids mediate analgesia in murine diabetic neuropathy. Eur J Pain (London, England). 2017;21(3):456‐465. doi: 10.1002/ejp.939 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.


