Abstract
Both anaesthesiologists and surgeons experience challenges in managing airway stenosis and scar contracture in the face and neck. Herein, we report the case of a 38-year-old woman (BMI 23.1 kg/m2, third-degree burns covering 40% of her body, an American Society of Anaesthesiologists physical status III) with an unusual case of airway constriction. This patient had a predictable difficult airway (mouth opening of 2 cm, bilateral nostril scar hyperplasia, Mallampatti score III, scarring of the head and neck, and severe tracheal stenosis). Tracheal stenosis measuring 5.5 mm in width as observed 8 cm below the glottis, and the bronchoscope could not pass through it. After two failed attempts at laryngeal mask insertion, we decided to instead insert a custom-made tracheal tube under the guidance of a fiberoptic bronchoscope. The operation was successful, and the patient was transferred to the intensive care unit (ICU).
Keywords: Airway stenosis, Difficult airways, Self-made
Background
Anaesthesiologists currently have access to a variety of advanced airway devices that can be used to manage difficult airways [1]. However, anaesthesiologists and surgeons experience challenges in managing airway stenosis and scar contracture in the face and neck [4]. Establishing a stable airway and reconstructing the airway during bronchoscopic palliation is critical for these patients. Failure to do so can lead to catastrophic events and result in high risks of airway-related morbidity and mortality [6]. Anaesthesiologists must not only be proficient in the use of these airway techniques but also consider using multiple tools to solve address difficult airways.
A case presentation
A 38-year-old woman (BMI 23.1 kg/m2, third-degree burns covering 40% of her body, an American Society of Anaesthesiologists physical status III) experienced difficulty breathing because her central airways were severely narrowed. The patient had scar hyperplasia and stenosis in the airway, which led to restricted airflow (Fig. 1). Owing to the patient’s emotional stress, it was difficult to tolerate long-term interventional treatment with tracheoscopy under local anaesthesia. After discussion between the interventional and anaesthesia doctors, it was ultimately decided to perform the interventional treatment under general anaesthesia.
Fig. 1.

Facial appearance of the patient
A detailed airway management plan was prepared before surgery for this patient with a predictable difficult airway (mouth opening of 2 cm, bilateral nostril scar hyperplasia, Mallampatti score III, scarring of the head and neck, and severe tracheal stenosis). Preoperative bronchoscopy revealed granulation tissue approximately 1 cm below the glottis and necrotic material covering the surface. Moreover, tracheal stenosis measuring 5.5 mm in width was observed 8 cm below the glottis, and the bronchoscope could not pass through it (Fig. 2). Our top priority for this patient was to maintain her oxygenation. Considering the patient’s limited mouth opening and head and neck mobility, the interventionalist could not use a rigid bronchoscope. The use of high-flow nasal cannula oxygen therapy could provide higher oxygen flows and concentrations, and apneic oxygenation techniques could maintain oxygenation. At the time, however, our hospital’s medical condition did not allow us to access this device. High-frequency jet ventilation was also not suitable because of severe scar contracture on both sides of the patient’s nostrils following burns. To prevent bleeding and allow for a larger operative area, we preferred to use a supraglottic ventilation device for ventilation to avoid touching the proliferative area.
Fig. 2.

Preoperative bronchoscopy
Few successful cases of laryngeal mask airways (LMAs) used in bronchoscopic intervention for patients with multiple airway lesions have been reported [7]. Given the patient’s difficult airway, the best choice for anaesthesia during this procedure would be laryngeal mask anaesthesia with spontaneous breathing. Therefore, choosing suitable laryngeal mask types and maintaining an appropriate anaesthesia depth are two essential factors to consider. Modir H et al. reported that all researchers successfully placed LMA on the first attempt in all cases in simulated difficult airways [8]. While some studies have revealed that placing an LMA on a patient with a mouth opening of 2 cm or more is not difficult, other researchers have suggested that a mouth opening of 1.5 cm is the preferred option for LMA placement [1]. Therefore, we believe that it would be reasonable to attempt to place a LMA on such a patient.
As a next step, anaesthetics must maintain a specific depth of anaesthesia while preserving spontaneous breathing. Sevoflurane is a type of anaesthetic that is commonly used in medical settings. It is known for its quick induction of sedation, fast recovery, and minimal effect on breathing [9]. To induce sedation, we used a specific concentration of sevoflurane. Studies have shown that for obese patients who require a supraglottic airway device and spontaneous breathing, the optimal end-tidal sevoflurane concentration is 2.5% [11]. Another study revealed that a combination of sevoflurane at a minimum alveolar concentration of 2.25% and 1 mg/kg propofol can also provide an optimal level of sedation for inserting a supraglottic airway device with spontaneous respiration [12]. Therefore, we limited the sevoflurane concentration to 2.5% for this patient to ensure that they could still breathe spontaneously while achieving a certain level of sedation. We assumed that even if a patient has obvious upper airway obstruction during the induction process and if the oral airway and nasal trumpet cannot work well, the patient’s respiratory consciousness can be restored by stopping the inhalation of sevoflurane. Additionally, we prepared various models of endotracheal tubes as alternative airway management options.
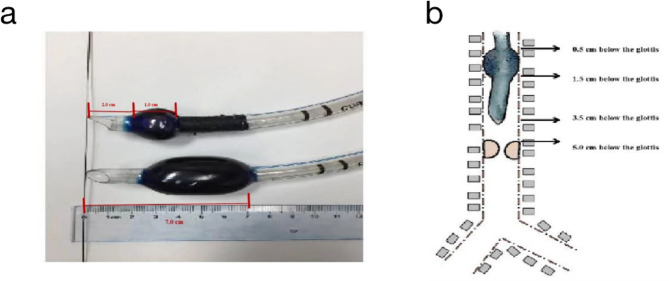
On the 10th of April 2019, the patient entered the operating room (HR 80 bpm, NBP 135/60 mmHg, SpO2 98%), and bronchodilators (2 ml of aerosolized ipratropium bromide, and 2 ml of pulmicort) were administered and a facemask with oxygen was placed. After the patient was sufficiently sedated (dexmedetomidine, loading dose: 0.5 µg/kg, 5 min; maintenance dose: 0.5 µg/kg/h) and received psychological counselling, anaesthetists used a bronchoscope to re-examine the patient’s airway. The anaesthesiologist used a fiberoptic bronchoscope and an epidural catheter to administer 5 ml of 2% lidocaine. Lidocaine was sprayed through, across, and beneath the glottis. While the procedure was performed, it was revealed that the constriction was situated 5 cm below the glottis, which deviated from the initial estimate of 8 cm (the patient’s nervousness, anxiety, intolerance, and choking during preoperative bronchoscopy may lead to inaccurate measurements). Furthermore, the bronchoscope (OD 5.5 mm) could not pass through the narrow section. The thinnest endotracheal tube available to us was ID 6.0 mm (interventional physicians use OD 5.5 mm bronchoscopes for operation), and the distance between the distal end of its cuff and the tip of the endotracheal tube was 6 cm. On the basis of the degree and location of the stenosis, the endotracheal tube was immediately modified (ID 8.0 mm). To make the insertion of the fiberoptic bronchoscope easier, we cut the end of the tracheal tube. When the structure was adequately modified, the distance between the tip of the tube and the distal edge of the cuff became 3.5 cm, which made surgical procedures easier. First, the distal cuff was bound and clasped tightly with suture lines such that the length of the cuff was 1 cm. Second, the distal tip with the Murphy eye was cut such that the distance between the tip and the distal edge of the cuff was 3.5 cm (Fig. 3). The edge was smoothed using heated metal scissors at the front end of the tracheal tube. Biological glue was applied to the knots to secure them to the surrounding area and prevent them from falling off. Finally, the tube’s cuff and valve were tested prior to use by inflating the pilot balloons. As endotracheal intubation continued, the fiberoptic bronchoscope was approximately 1.5 cm away from the stenosis at the front end.
Fig. 3.
Modified tracheal tube
After preparing airway management tools such as bronchoscopes, laryngeal masks, and custom-made tracheal tubes, we induced anaesthesia via a laryngeal mask while following the established airway management plan to preserve her ability to breathe autonomously. We used sevoflurane on the patient with the facemask, gradually increasing the concentration from 1 to 2.5% using a stepwise approach of 0.5% per three breaths until the patient achieved a bispectral index (BIS) less than 60. After successful laryngeal mask ventilation, we administered 50 mg of propofol and 10 µg of sufentanil intravenously. Once the patient was sufficiently relaxed, we inserted a 3rd flexible laryngeal mask. Placement of the LMA was attempted twice directly, but both failed because of the small mouth opening and limited neck movement. At that time, we decided to instead insert a custom-made tracheal tube under the guidance of a fiberoptic bronchoscope. Sevoflurane inhalation was stopped after the custom-made tube was inserted well, and target-controlled infusions of propofol and remifentanil were administered continuously. The BIS was maintained at 40–60.
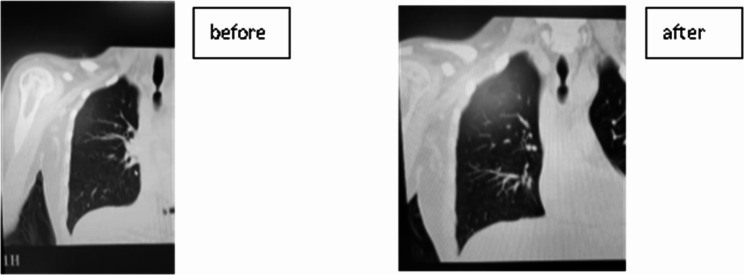
Under a bronchoscope, the interventionalist performed endotracheal scar cryosurgery and balloon dilatation. The patient’s haemodynamics were stable throughout the operation, and no hypoxemia occurred. The operation was successfully completed, and the patient was transferred to the ICU. Three and a half hours after the patient entered the ICU, her spontaneous breathing stabilized, her blood gas results were satisfactory, and the endotracheal tube was removed. Fiberoptic bronchoscopy revealed that airway stenosis was much less common than before, and patients with symptoms of dyspnoea during postoperative activities improved (Fig. 4).
Fig. 4.
Computed tomography scan after surgery
Discussion
Airway management is shared between anaesthesiologists and interventionalists, and the method needs to be discussed before the operation to ensure patient safety and to facilitate surgical treatment. Additionally, rather than prioritizing the establishment of the airway, the focus for interventionalists is on completing the treatment. As a result, anaesthesiologists are advised to perform an additional bronchoscopy prior to surgery to gain as much information as possible and ensure that the airway is effectively established.
Anaesthesiologists should have the ability to adapt to the unique characteristics of each patient’s airway and develop individualized airway management plans that are tailored to their specific needs. This requires proficiency in a variety of airway management tools and techniques. In this case, rigid bronchoscopy and high nasal flow methods were not feasible, and placement of the LMA was unsuccessful. We conducted a thorough assessment and ultimately opted to employ a custom-made endotracheal tube for the procedure. We placed the custom-made endotracheal tube above the airway stenosis, with the cuff located below the vocal cords. This method not only ensures effective ventilation but also provides the surgeon with a larger operating space during the procedure. It is crucial to utilize a range of airway management tools or even customized modifications to develop individualized airway management strategies. When we do not have the best equipment, we must effectively modify equipment and techniques to meet our individual needs for airway management. However, monitoring methods should also be optimized to prevent complications associated with the use of homemade endotracheal tubes.
Acknowledgements
None to declare.
Abbreviations
- LMA
Laryngeal mask airways
Author contributions
ZWW—designed the review article. ZY, HXJ and XRK—conducted literature search. LY and ZWW—Wrote and revised the manuscript. WXL—provided critical feedback on the manuscript and contributed to the revision process. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–52. [DOI] [PubMed] [Google Scholar]
- 2.Mushambi MC, Kinsella SM, Popat M, Swales H, Ramaswamy KK, Winton AL, et al. Obstetric Anaesthetists’ Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia. 2015;70:1286–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sabato SC, Long E. An institutional approach to the management of the ‘Can’t intubate, can’t oxygenate’ emergency in children. Paediatr Anaesth. 2016;26:784–93. [DOI] [PubMed] [Google Scholar]
- 4.Chao YK, Liu YH, Hsieh MJ, Wu YC, Liu HP, Wang CJ, et al. Controlling difficult airway by rigid bronchoscope–an old but effective method. Interact Cardiovasc Thorac Surg. 2005;4:175–9. [DOI] [PubMed] [Google Scholar]
- 5.Xue FS, Liao X, Li CW, Xu YC, Yang QY, Liu Y, et al. Clinical experience of airway management and tracheal intubation under general anesthesia in patients with scar contracture of the neck. Chin Med J (Engl). 2008;121:989–97. [PubMed] [Google Scholar]
- 6.Greenland KB, Acott C, Segal R, Goulding G, Riley RH, Merry AF. Emergency surgical airway in life-threatening acute airway emergencies–why are we so reluctant to do it? Anaesth Intensive Care. 2011;39:578–84. [DOI] [PubMed] [Google Scholar]
- 7.Arevalo-Ludena J, Arcas-Bellas JJ, Alvarez-Rementeria R, Flandes J, Moris L, Munoz Alameda LE. A comparison of the I-Gel supraglottic device with endotracheal intubation for bronchoscopic lung volume reduction coil treatment. J Clin Anesth. 2016;31:137–41. [DOI] [PubMed] [Google Scholar]
- 8.Modir H, Moshiri E, Malekianzadeh B, Noori G, Mohammadbeigi A. Endotracheal intubation in patients with difficult airway: using laryngeal mask airway with bougie versus video laryngoscopy. Med Gas Res. 2017;7:150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hakumoto Y, Takasugi Y, Kamamoto H, Shigemori S, Koga Y, Mori K. Tracheal intubation in a patient with undetectable tracheal narrowing on chest radiography. J Anesth. 2010;24:128–31. [DOI] [PubMed] [Google Scholar]
- 10.Kandasamy R, Sivalingam P. Use of sevoflurane in difficult airways. Acta Anaesthesiol Scand. 2000;44:627–9. [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Gao X, Wei W, Miao H, Meng H, Tian M. The optimum sevoflurane concentration for supraglottic airway device Blockbuster insertion with spontaneous breathing in obese patients: a prospective observational study. BMC Anesthesiol. 2017;17:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonnin M, Therre P, Albuisson E, Beaujard H, Barthelemy I, Mondie JM, et al. Comparison of a propofol target-controlled infusion and inhalational sevoflurane for fibreoptic intubation under spontaneous ventilation. Acta Anaesthesiol Scand. 2007;51:54–9. [DOI] [PubMed] [Google Scholar]
- 13.Wang HX, Miao HH, Gao X, Wei W, Ding GN, Zhang Y, et al. Optimum end-tidal concentration of sevoflurane to facilitate supraglottic airway device insertion with propofol at induction allowing spontaneous respiration in obese patients: a prospective observational study. Med (Baltim). 2017;96:e8902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.