Abstract
Although endoscopic sinus surgery (ESS) is beneficial in improving asthma symptoms, its impact on the lung function in patients with asthma and chronic rhinosinusitis remains unclear. We herein report a case of severe asthma with eosinophilic chronic rhinosinusitis, in which ESS substantially improved airflow limitation and concomitantly reduced fractional exhaled nitric oxide and blood eosinophil counts. ESS likely relieved airflow limitation by suppressing type 2 inflammatory pathways. This case highlights ESS as a promising strategy for achieving clinical remission in patients with severe asthma and chronic rhinosinusitis.
Keywords: chronic rhinosinusitis, endoscopic sinus surgery, severe asthma, airflow limitation, asthma remission
Introduction
Asthma often coexists with comorbid chronic rhinosinusitis (CRS), with eosinophilic CRS and asthma sharing a common type 2 (T2) inflammatory pathophysiology (1,2). T2 cytokines, such as interleukin (IL)-4, IL-5, and IL-13, circulate in the bloodstream, causing eosinophil infiltration into the upper and lower airways, contributing to the disease burden in both CRS and asthma. Patients with severe asthma coupled with CRS with nasal polyps (CRSwNP) have increased asthma exacerbations and oral corticosteroid usage (3), ultimately impairing the pulmonary function (4).
Although sinus surgery improves asthma symptoms (5,6), its impact on the lung function in patients with asthma and CRS remains unclear. We herein report a case of severe asthma with eosinophilic CRS (ECRS) in which sinus surgery significantly improved airflow limitation concurrently with the suppression of T2 airway inflammation.
Case Report
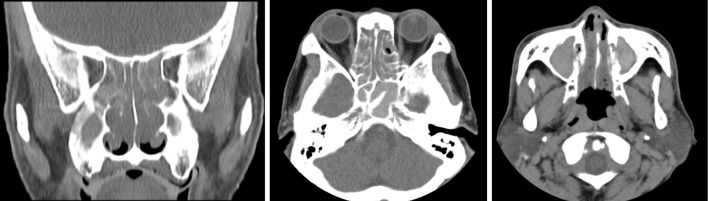
A 63-year-old man with asthma and CRS presented with the following clinical findings during the initial visit: Asthma Control Test score of 20 points, forced expiratory volume in 1 s (FEV1) of 1.40 L, percent predicted FEV1 (%FEV1) of 50.1%, blood eosinophil count (b-Eos) of 1,400 cells/μL, and fractional exhaled nitric oxide (FeNO) of 160 parts per billion (ppb). Sinus computed tomography (CT) revealed significant mucosal thickening and fluid retention in the maxillary, ethmoid, sphenoid, and frontal sinuses (Fig. 1). The JESREC score in this patient was 13 (diseased side: both sides, CT shadow: ethmoid ≥ maxillary, eosinophils in peripheral blood >5%). He was diagnosed with ECRS based on a JESREC score of >11 points, which designates ECRS (7).
Figure 1.
Sinus CT before endoscopic sinus surgery depicting extensive mucosal thickening and fluid retention in the bilateral maxillary, ethmoid, sphenoid, and frontal sinuses. CT: computed tomography
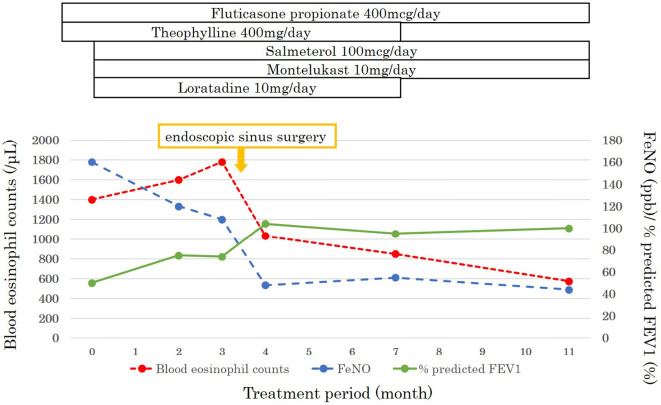
Inhaled fluticasone propionate (400 μg daily, medium dose) and theophylline (400 mg daily) were administered, and salmeterol (100 μg daily), montelukast (10 mg daily), and loratadine (10 mg daily) were also administered as part of the treatment regimen. After 3 months of these asthma maintenance therapies, the FEV1 increased to 2.03 L (Fig. 2). However, the patient still showed residual airflow limitation (%FEV1 74.1%), along with significantly elevated levels of both b-Eos and FeNO (1,780 /μL and 108 ppb). Given the uncontrolled asthma (airflow limitation) despite a medium-dose inhaled corticosteroid, long-acting beta-agonists, and leukotriene receptor antagonist, the patient was diagnosed with severe asthma according to the European Respiratory Society/American Thoracic Society guidelines (8).
Figure 2.
Patient treatment progression. FeNO: fractional exhaled nitric oxide, FEV1: forced expiratory volume in 1 s
Before an evaluation of the initial effects of asthma treatment, the patient underwent endoscopic sinus surgery (ESS) to relieve CRS symptoms, including olfactory disorders and nasal obstruction, but not for asthma. A postoperative pathological examination confirmed the diagnosis of ECRS. After ESS, the olfactory disorders and nasal obstruction were alleviated. The patient did not receive oral corticosteroids (OCSs) postoperatively. The asthma control test score improved from 20 to 25 points after the ESS. The asthma treatment was the same before and after ESS.
One month post-ESS, the FEV1 and %FEV1 had dramatically increased (FEV1 +820 mL; %FEV1 +30.1%). Concurrently, the b-Eos and FeNO levels dropped to 1,032 /μL and 48 ppb, respectively. At 8 months post-ESS, subsequent blood tests and lung function assessments indicated a b-Eos of 574 /μL, FEV1 of 2.71 L, %FEV1 of 99.7%, and FeNO of 44 ppb. Refractory airflow limitation, which was unresponsive to standard asthma maintenance treatments, exhibited significant improvement following ESS. This improvement was accompanied by a consistent reduction in both b-Eos and FeNO levels.
Discussion
In this case, the use of inhaled corticosteroids alongside a long-acting beta 2 agonist and other asthma-controlling agents (such as leukotriene receptor antagonist and theophylline) failed to attain effective asthma control. Nevertheless, ESS yielded a remarkable enhancement of airflow limitation concomitant with the suppression of airway and systemic T2 inflammation. To our knowledge, this is the first report demonstrating concurrent amelioration of both airflow limitation and T2 inflammation through ESS in a patient with asthma and CRS.
In this instance, the intervention targeting ECRS (specifically ESS) markedly ameliorated the severity of asthma conditions, underscoring ECRS as a viable therapeutic focus in asthma management, which is characterized as a treatable trait. Treatable traits, defined as discernible therapeutic targets characterized by clinical phenotypes, have recently gained prominence as a precision medicine approach for chronic airway diseases, such as asthma and chronic obstructive pulmonary disease (9). These treatable traits are not restricted to pulmonary domains, encompassing elements such as T2 inflammation and airflow limitation, and include extrapulmonary aspects such as chronic rhinosinusitis. ECRS, frequently comorbid with severe asthma, is an important extrapulmonary treatable trait that warrants attention in asthma management.
ESS improved both the airway and systemic T2 inflammation. This case aligns with our previous investigation, wherein ESS demonstrated suppression of both airway and systemic T2 inflammation in 25 patients with asthma and ECRS (10). A cluster analysis of CRS patients revealed that patients with CRSwNP showed strong T2 airway inflammation (11). Sinus tissues in patients with CRSwNP exhibit elevated levels of T2 inflammatory mediators, including IL-5, IL-13, eosinophil cationic protein, and monocyte chemoattractant protein-4, compared to those in healthy subjects (12). These findings suggest that the key mediators of T2 inflammation are discharged from nasal polyps and unfavorably affect both the upper and lower airways through the bloodstream. Surgical removal of nasal polyps through ESS appears to improve both airway and systemic T2 inflammation by curtailing T2 cytokines, leading to favorable effects on the lower and upper airways.
The substantial enhancement in airflow limitation (FEV1 increase of 820 mL) observed following ESS may be attributed to the suppression of T2 inflammation. Several studies have indicated that controlling T2 inflammation in patients with severe asthma leads to improved airflow limitations. For instance, a previous study showed that 1-year treatment with mepolizumab (anti-IL-5 therapy) in 44 patients with severe eosinophilic asthma and CRSwNP yielded enhancements in %FEV1, along with a substantial reduction in blood eosinophil count and sinonasal outcome test-22 scores (13). Another study showed that dupilumab (anti-IL-4/13 therapy) significantly improved airflow limitation and reduced T2 inflammatory markers, such as FeNO and immunoglobulin E (IgE), in patients with moderate-to-severe asthma (14). A plausible explanation for the improvement in airflow limitation stemming from treatments targeting T2 cytokines is that the suppression of these mediators results in reduced mucus secretion in the airways and bronchoconstriction, which provides relief from airflow limitation (15). Thus, the substantial improvement in FEV1 observed through ESS in this case may be attributed to the suppression of T2 inflammatory pathways, which is consistent with findings from previous studies on biological agents that target T2 cytokines. We suspect that this patient might not have airway remodeling due to the dramatic improvement in airflow limitation by ESS. It is difficult to accurately evaluate airway remodeling during routine practice. Nonetheless, even CRSwNP patients with asthma who have airway remodeling might benefit from ESS through improvement of asthma symptoms and T2 airway inflammation.
This case indicates that ESS can lead to clinical remission in patients with severe asthma and CRS. Recent advancements in asthma treatment, particularly the introduction of biologics targeting the T2 inflammatory pathways, have made achieving remission in severe asthma a feasible objective. Definitions of clinical/deep remission and bio-free remission have recently been proposed for severe asthma (16-18), including with regard to various aspects of asthma, such as symptoms, exacerbations, lung function, and airway inflammation. Achieving control over CRS in patients with asthma is pivotal for achieving asthma remission (19). Consequently, ESS has the potential to contribute significantly to both asthma remission and the underlying biological mechanisms. Previous studies have shown that ESS for CRS can alleviate asthma symptoms, mitigate the risk of OCS use, and exacerbate asthma. A multicenter prospective study demonstrated that ESS improved the Mini-Asthma Quality of Life Questionnaire and Asthma Control Test scores in 86 asthmatic patients with CRS (6). A previous meta-analysis investigating ESS in patients with asthma and CRS, which included 22 studies involving 891 patients, revealed reductions of 84.8% in asthma exacerbations, 64.4% in hospitalizations, and 72.8% in the utilization of OCS across the patient population (5). Nonetheless, our case demonstrated that ESS markedly improved airflow limitation, presumably through suppression of T2 inflammation, suggesting that ESS may be a promising approach for achieving clinical remission in patients with severe asthma and CRS.
CRSwNP has a high recurrence rate after ESS. One study with 18 months of follow-up after ESS reported polyp recurrence in 40% of the patients (20). Recurrent CRSwNP is likely to worsen asthma control. Re-operation or introduction of biologics should be considered for recurrent CRSwNP, but certain views are not yet available. A study of patients with refractory CRSwNP treated with mepolizumab showed that mepolizumab reduced the risk of further sinus surgery (21), suggesting that the introduction of biologics is a good option for patients with recurrent CRSwNP.
ESS is often recommended as a preliminary step before resorting to biologics for CRSwNP, mainly owing to cost-effectiveness considerations (22,23). However, these previous reports may have underestimated the indirect costs associated with postoperative complications and the need for reoperation. In addition, they did not account for the potential benefits of biologics, such as their positive impact on comorbid asthma and the potential reduction in costs associated with adverse events caused by OCSs owing to decreased usage and/or discontinuation (24). No direct comparative trials have evaluated the effectiveness of ESS versus biologics in alleviating nasal and respiratory symptoms in patients with CRSwNP and asthma. Further comprehensive studies are needed to verify whether ESS, biologics, or a combination of the two is a more efficacious strategy for managing CRSwNP alongside asthma. Furthermore, given the distinct treatment modalities and associated costs, effective collaboration among patients, otolaryngologists, and respiratory physicians is crucial in the treatment decision-making process.
Conclusion
In conclusion, this case demonstrates that ESS has a significant impact on relieving airflow limitation, presumably through the suppression of T2 airway inflammation pathways. These findings suggest that ESS can serve as an additional treatment option to achieve clinical remission in patients with severe asthma and CRS. Further investigations are necessary to confirm whether or not ESS contributes to clinical remission in patients with severe asthma and CRS.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Brinke AT, Grootendorst DC, Schmidt JT, et al. Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol 109: 621-626, 2002. [DOI] [PubMed] [Google Scholar]
- 2.Boulet LP, Boulay MÈ. Asthma-related comorbidities. Expert Rev Respir Med 5: 377-393, 2011. [DOI] [PubMed] [Google Scholar]
- 3.Canonica GW, Malvezzi L, Blasi F, et al. Chronic rhinosinusitis with nasal polyps impact in severe asthma patients: evidences from the Severe Asthma Network Italy (SANI) registry. Respir Med 166: 105947, 2020. [DOI] [PubMed] [Google Scholar]
- 4.Novelli F, Bacci E, Latorre M, et al. Comorbidities are associated with different features of severe asthma. Clin Mol Allergy 16: 25, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vashishta R, Soler ZM, Nguyen SA, Schlosser RJ. A systematic review and meta-analysis of asthma outcomes following endoscopic sinus surgery for chronic rhinosinusitis. Int Forum Allergy Rhinol 3: 788-794, 2013. [DOI] [PubMed] [Google Scholar]
- 6.Schlosser RJ, Smith TL, Mace J, Soler ZM. Asthma quality of life and control after sinus surgery in patients with chronic rhinosinusitis. Allergy 72: 483-491, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tokunaga T, Sakashita M, Haruna T, et al. Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 70: 995-1003, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 43: 343-373, 2014. [DOI] [PubMed] [Google Scholar]
- 9.Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 47: 410-419, 2016. [DOI] [PubMed] [Google Scholar]
- 10.Hamada K, Oishi K, Chikumoto A, et al. Impact of sinus surgery on type 2 airway and systemic inflammation in asthma. J Asthma 58: 750-758, 2021. [DOI] [PubMed] [Google Scholar]
- 11.Tomassen P, Vandeplas G, Van Zele T, et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol 137: 1449-1456.e4, 2016. [DOI] [PubMed] [Google Scholar]
- 12.Stevens WW, Ocampo CJ, Berdnikovs S, et al. Cytokines in chronic rhinosinusitis. Role in eosinophilia and aspirin-exacerbated respiratory disease. Am J Respir Crit Care Med 192: 682-694, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Detoraki A, Tremante E, D'Amato M, et al. Mepolizumab improves sino-nasal symptoms and asthma control in severe eosinophilic asthma patients with chronic rhinosinusitis and nasal polyps: a 12-month real-life study. Ther Adv Respir Dis 15: 17534666211009398, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castro M, Rabe KF, Corren J, et al. Dupilumab improves lung function in patients with uncontrolled, moderate-to-severe asthma. ERJ Open Res 6: 00204-2019, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maspero J, Adir Y, Al-Ahmad M, et al. Type 2 inflammation in asthma and other airway diseases. ERJ Open Res 8: 00576-2021, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menzies-Gow A, Bafadhel M, Busse WW, et al. An expert consensus framework for asthma remission as a treatment goal. J Allergy Clin Immunol 145: 757-765, 2020. [DOI] [PubMed] [Google Scholar]
- 17.Oishi K, Hamada K, Murata Y, et al. A real-world study of achievement rate and predictive factors of clinical and deep remission to biologics in patients with severe asthma. J Clin Med 12: 2900, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamada K, Oishi K, Murata Y, Hirano T, Matsunaga K. Feasibility of discontinuing biologics in severe asthma: an algorithmic approach. J Asthma Allergy 14: 1463-1471, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Westerhof GA, Coumou H, de Nijs SB, Weersink EJ, Bel EH. Clinical predictors of remission and persistence of adult-onset asthma. J Allergy Clin Immunol 141: 104-109.e3, 2018. [DOI] [PubMed] [Google Scholar]
- 20.DeConde AS, Mace JC, Levy JM, et al. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 127: 550-555, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fokkens WJ, Mullol J, Kennedy D, et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): in-depth sinus surgery analysis. Allergy 78: 812-821, 2023. [DOI] [PubMed] [Google Scholar]
- 22.Scangas GA, Wu AW, Ting JY, et al. Cost utility analysis of dupilumab versus endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps. Laryngoscope 131: E26-E33, 2021. [DOI] [PubMed] [Google Scholar]
- 23.Kato A, Peters AT, Stevens WW, Schleimer RP, Tan BK, Kern RC. Endotypes of chronic rhinosinusitis: relationships to disease phenotypes, pathogenesis, clinical findings, and treatment approaches. Allergy 77: 812-826, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Lans RJL, Hopkins C, Senior BA, Lund VJ, Reitsma S. Biologicals and endoscopic sinus surgery for severe uncontrolled chronic rhinosinusitis with nasal polyps: an economic perspective. J Allergy Clin Immunol Pract 10: 1454-1461, 2022. [DOI] [PubMed] [Google Scholar]