Abstract
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare, autoinflammatory bone disorder most often seen in children and adolescents characterized by recurrent episodes of sterile osteolytic osseous lesions. Diagnosing CRMO requires the exclusion of other conditions, which is often challenging due to its varied presentations and progression. However, adult-onset CRMO and exclusive spinal cases are extremely rare events, highlighting the importance of this case. Our case presents a 38-year-old female with chronic back pain for 6 months of postepidural anesthesia during a C-section. The pain was progressive, exacerbated by movement, and partially relieved by painkillers. The patient had tenderness on physical examination in the thoracolumbar region. MRI of the spine showed multiple endplate changes, and extensive laboratory tests and biopsy ruled out infectious cause and malignancy, leading to the diagnosis of CRMO. The connection between pain and epidural anesthesia was only an incidental finding. The patient was treated effectively with steroids and etanercept. CRMO is mainly a childhood disease, with adult cases being very rare. Isolated spinal involvement in CRMO is particularly rare and can make the diagnosis challenging. This case highlights that CRMO should be considered in adults with an atypical isolated spinal lesion. NSAIDs are the main treatment, with corticosteroids and TNF inhibitors used in unresponsive cases. This case underscores the need for heightened awareness of CRMO's potential to present in adults with atypical isolated spinal lesions, which could lead to more timely and accurate diagnoses.
Keywords: Adult-onset, Sterile osteolytic lesions, CRMO diagnosis
Introduction
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare, inflammatory skeletal disease of unknown origin, which mainly affects children and adolescents. CRMO was first described by Giedion et al. in 1972 as multifocal, recurrent attacks of sterile bone lesions [1]. In most cases, laboratory studies show nonspecific signs of inflammation. Histology and radiologic imaging are similar to those of infected osteomyelitis. Patients typically have multiple painful osseous localizations when they first show [2], but clinical diagnosis can be difficult because of the wide range of presenting symptoms and disease progression. The most commonly involved areas are the metaphyses of the long bones, pelvis, and clavicles; the jaw and vertebrae are also frequently affected [2].
Our case report is distinctive in that it involves an adult patient, an atypical age group for CRMO, which predominantly affects children and adolescents. Moreover, the condition is localized solely in the spine, another unusual presentation for CRMO, which typically manifests in multiple bones making this case more unique.
Epidemiological data in CRMO is very limited, and include only small case series and regional cohorts. CRMO primarily affects children aged 7 to 12 years [3]. Only 10% of the patients are older than 20 years [4]. The Eurofever international registry, spanning 19 countries, has the largest documented cohort of CRMO patients, consisting of 486 cases that document only 31 adult patients with an average age of onset of 33 years (range 19-62.4 years) [5]. The condition was initially documented in Europe but it has subsequently been reported in other parts of the world including North America, Australia and New Zealand, Israel, Japan, and Hong Kong [6].
The pathophysiology of CRMO is unclear, some reports suggested its relation with other inflammatory conditions, including inflammatory bowel disease, acne, ankylosing spondylitis, and psoriasis [7]. Recent genetic information shows that CRMO might be a member of a class of osseous-expressing autoinflammatory illnesses as it shares the same gene mutation with these syndromes that includes DIRA syndrome (mutations in IL1RN), PAPA syndrome (mutations in PSTPIP1), and Majeed syndrome(LPIN2 mutations) [2]. The mutations in these syndromes produce proinflammatory cytokines which cause sterile bone infection as in CRMO. For example, in Majeed syndrome mutation in LPIN2 causes increased production of IL-6 and TNFα and in PAPA and DIRA syndromes mutations cause decreased production of NLRP3 inflammasome IL-1 receptor antagonist which leads to a pro-inflammatory state and causes bone inflammation [7]. However, due to insufficiency of data, it suggests that CRMO etiology is probably more multifactorial [2].
Case presentation
Our case presents a 38-year-old female with a history of chronic back pain for 6 months. The pain started after epidural anesthesia was administered during c-section 6 months ago. It was constant, progressive in nature, aggravated by sitting up and walking, and temporarily relieved by painkillers. There was no history of fever or any weight loss. Due to the severity of her pain, and disease progression, she was unable to walk or bear any. Initially, she was treated with antibiotics and muscle relaxants but that did not show any improvement. Additionally, she developed a perianal abscess due to constipation because of her infrequent visits to the bathroom due to limited mobility.
On physical examination, tenderness was noted in the thoracolumbar region, especially at T12, L1, and L2. There was also a paraspinal muscular spasm. Neurological examination was unremarkable; the patient could move all extremities without difficulty, and Sphincter control was normal. Both motor and sensory systems of the lower extremities were intact.
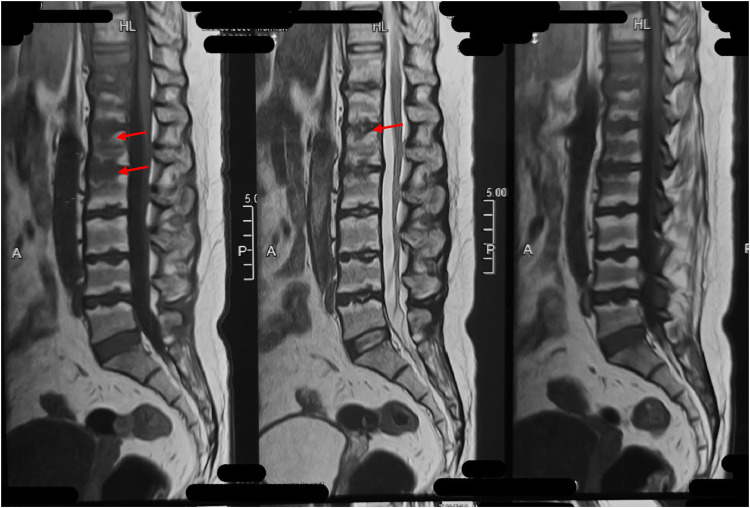
To rule out differentials, a series of tests were performed. MRI of the spine revealed multiple endplate changes in the lumbar and thoracic spine especially at T11 and T12 as shown in Fig. 1. These findings were correlated to the physical examination findings. Complete blood count (CBC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were advised to check for any septic or infective spondylodiscitis. Cultures, sensitivity tests, and gene Xpert of the lesion were negative for Tuberculosis or any other infection ruling out infective osteomyelitis. Serum vitamin D levels were also within normal range. Biopsy of the lesion showed no granuloma or malignancy but inflammatory infiltrates were present in the bone lesions.
Fig. 1.
MRI showing multiple endplate changes in thoracic and lumbar region.
Initially, an infective pathology was suspected given the history of epidural anesthesia, and treated with antibiotics. However, a biopsy confirmed the diagnosis of CRMO, and the connection between pain and epidural anesthesia was found to be only an incidental finding. The patient was started on steroids and etanercept which led to a significant improvement in her symptoms.
Discussion
CRMO is an uncommon inflammatory bone disorder that primarily affects younger age group. The mean age of onset of the disease is 10 years. CRMO is mainly a diagnosis of exclusion especially in patients who present with lytic or sclerotic bone lesions and periosteal reaction with serological and histological findings negative for infection and malignancy [8]. The disease can result in multiple bone lesions, mostly affecting the metaphysis of long bones, pelvis, jaw, and vertebrae. According to King et al. [9] for making the diagnosis of CRMO, the following criteria should be met: (a) multifocal (2 or more) bone lesions (b) a prolonged course (over 6 months) marked by fluctuating disease activity, and with most of the patients remain healthy between recurrent attacks of swelling, pain and tenderness, (c) lack of response to antibiotics therapy given for a minimum period of 1 month, (d) typical lytic regions surrounded by sclerosis on radiograph plus increased uptake on bone scan, and (e) unable to find an identifiable organism.
Our case report presents several unique aspects that differ from other cases of CRMO and contribute to the broader understanding of CRMO. Firstly, the patient is an adult, which is unusual as CRMO is primarily diagnosed in children. Adult-onset CRMO is exceedingly rare, with only a few cases documented in the literature. The Eurofever international registry, which documented 486 cases, reported only 31 adult patients, making our patient's presentation at 38 years old an uncommon occurrence [5]. Secondly, the disease in our patient is localized solely in the spine. Although spinal involvement is documented in CRMO, it typically occurs alongside lesions in other bones. Diagnosing isolated spinal presentations can be difficult since they may mimic other conditions like neoplasms, infections, or inflammatory diseases such as spondyloarthropathies.
CRMO is usually a diagnosis of exclusion because there are no universally recognized disease criteria and a lack of specific disease biomarkers. Just as the diagnosis of each disease is determined through a combination of patient history, physical examination, and laboratory investigations, the diagnosis of CRMO is generally made based on the history of long-term bone pain and physical examination findings of tenderness. Further testing such as radiological and histological investigations are used only to confirm the diagnosis. Baseline testing such as complete blood count (CBC) and other inflammatory markers such as ESR and CRP may be normal or may show slight inflammation [10]. X-rays, computed tomography (CT), magnetic resonance imaging (MRI), PET scans, and nuclear bone scans are usually used to see any structural changes in the bones. Imaging studies usually reveal inflammatory bone lesions that typically appear as radiolucent, osteolytic, or sclerotic lesions although they may appear normal in early stages [11]. MRI studies are particularly sensitive, especially during the early stages of the disease. In cases where the diagnosis is uncertain, bone biopsies are performed to rule out other diseases such as cancers, persistent infections, and systemic diseases [10]. Ruling out other conditions like spinal infection, spondyloarthritis, cancers, and other similar conditions is the most important process in diagnosing CRMO as it is mainly the diagnosis of exclusion. Biopsy usually demonstrates nonspecific inflammatory bone changes with bone remodeling and sclerosis [2].
There are no official treatment guidelines regarding CRMO. The mainstays of treatment consist of nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs, such as methotrexate), corticosteroids, and anti-TNF agents. NSAIDs are considered the first-line treatment of CRMO. They are highly efficient and not only provide pain relief but can also prevent further bone damage in most patients. Among 40% to 80% of patients, children respond better than adults [12]. Most of the patients experience continuous remission of disease especially after 2 years of the treatment [13]. For patients who do not respond to NSAIDs, steroids are considered the next best therapy [14]. Corticosteroids appear to quickly and efficiently reduce inflammatory activity though they rarely lead to long-term remission. As the use of long-term steroids can cause so many side effects, they are used only for short periods of time. The usage of biological therapies to treat CRMO has been increasing these days; the literature has shown multiple case reports of effective uses of etanercept, and infliximab [14]. The use of DMARDS as a single monotherapy is ineffective in most patients and is mostly used with NSAIDs. The management of our patient involved the use of steroids for 1 month and etanercept for 6 months because NSAIDs provided only temporary relief. Given the patient's inadequate response to NSAIDs, steroids were introduced to quickly manage the inflammatory activity, and etanercept was added to sustain remission and reduce the need for long-term steroid use. Currently, the patient is in a remission state and is feeling much better, with regular follow-ups every 2 months to monitor her condition.
Documenting such cases helps to enhance the understanding of this condition's spectrum, including its clinical manifestations, diagnosis, and management strategies. This knowledge helps establish CRMO as a potential differential diagnosis for bone pain, thereby reducing unnecessary testing and leading to more accurate and efficient patient care.
Conclusion
This case highlights the importance of considering CRMO in the differential diagnosis of chronic back pain in adults, particularly when presenting with atypical isolated spinal lesions. It also enhances awareness and understanding of CRMOs varied presentations which leads to more accurate diagnoses and better patient outcomes through timely and appropriate treatment interventions.
Patient consent
Written and Informed consent was taken from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Ahmad Ismail, Email: ahmadismail@kemu.edu.pk.
Muhammad Fawad Ashraf, Email: fawad1110@gmail.com, fawadashraf@kemu.edu.pk.
References
- 1.Giedion A., Holthusen W., Masel L.F., Vischer D. Subacute and chronic “symmetrical” osteomyelitis. Ann Radiol (Paris) 1972;15(3):329–342. [PubMed] [Google Scholar]
- 2.Wipff J, Costantino F, Lemelle I, Pajot C, Duquesne A, Lorrot M, Faye A, Bader‐Meunier B, Brochard K, Despert V, Jean S. A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis & rheumatology. 2015;67(4):1128–1137. doi: 10.1002/art.39013. [DOI] [PubMed] [Google Scholar]
- 3.Borzutzky A, Stern S, Reiff A, Zurakowski D, Steinberg EA, Dedeoglu F, et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012;130:e1190–e11e7. doi: 10.1542/peds.2011-3788. [DOI] [PubMed] [Google Scholar]
- 4.Mahady S, Ladani A. Clinical and diagnostic considerations for atypical, adult onset presentation of chronic recurrent multifocal osteomyelitis (CRMO) Case Rep Rheumatol. 2019;2019(1) doi: 10.1155/2019/8206892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Girschick H, Finetti M, Orlando F, Schalm S, Insalaco A, Ganser G, Nielsen S, Herlin T, Koné-Paut I, Martino S, Cattalini M. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Rheumatology. 2018;57(7):1203–1211. doi: 10.1093/rheumatology/key058. [DOI] [PubMed] [Google Scholar]
- 6.Jurriaans E, Singh NP, Finlay K, Friedman L. Imaging of chronic recurrent multifocal osteomyelitis. Radiol Clin North Am. 2001;39(2):305–327. doi: 10.1016/s0033-8389(05)70279-7. [DOI] [PubMed] [Google Scholar]
- 7.Morbach H, Hedrich CM, Beer M, Girschick HJ. Autoinflammatory bone disorders. Clin Immunol. 2013;147(3):185–196. doi: 10.1016/j.clim.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser D, Bolt I, Hofer M, Relly C, Berthet G, Bolz D, et al. Chronic nonbacterial osteomyelitis in children: a retrospective multicenter study. Pediatr Rheumatol Online J. 2015;13:25. doi: 10.1186/s12969-015-0023-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King SM, Laxer RM, Manson D, Gold R. Chronic recurrent multifocal osteomyelitis: a non-infectious inflammatory process. Pediatr Infect Dis. 1987;6:907–911. doi: 10.1097/00006454-198710000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Hofmann SR, Kapplusch F, Girschick HJ, Morbach H, Pablik J, Ferguson PJ, Hedrich CM. Chronic recurrent multifocal osteomyelitis (CRMO): presentation, pathogenesis, and treatment. Curr Osteoporos Rep. 2017;15:542–554. doi: 10.1007/s11914-017-0405-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Probst FP, Bjorksten B, Gustavson KH. Radiological aspect of chronic recurrent multifocal osteomyelitis. Ann Radiol (Paris) 1978;21:115–125. [PubMed] [Google Scholar]
- 12.Girschick HJ, Zimmer C, Klaus G, Darge K, Dick A, Morbach H. Chronic recurrent multifocal osteomyelitis: what is it and how should it be treated? Nat Clin Pract Rheumatol. 2007;3(12):733–738. doi: 10.1038/ncprheum0653. [DOI] [PubMed] [Google Scholar]
- 13.Schnabel A, Range U, Hahn G, Berner R, Hedrich CM. Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44(7):1058–1065. doi: 10.3899/jrheum.161255. [DOI] [PubMed] [Google Scholar]
- 14.Roderick MR, Sen ES, Ramanan AV. Chronic recurrent multifocal osteomyelitis in children and adults: current understanding and areas for development. Rheumatology (Oxford) 2018;57(1):41–48. doi: 10.1093/rheumatology/kex066. [DOI] [PubMed] [Google Scholar]