Abstract
Objective
This study aimed to assess the association between preoperative neutrophil–lymphocyte ratio (NLR) and febrile urinary tract infection (fUTI) in patients who underwent percutaneous nephrolithotomy (PCNL).
Patients and Methods
The clinical data of patients who underwent PCNL at our hospital between March 2020 and May 2023 were retrospectively analyzed. According to whether fUTI occurs after operation, collected data were divided to the patients into fUTI and non-fUTI. Univariate analysis, relative operating characteristic (ROC) curves and multivariate logistic regression analysis were performed on the data.
Results
A total of 405 patients were enrolled in the study. The procedure was successfully performed in all patients, and the incidence of fUTI was 8.4% (34/405). Eight patients eventually developed sepsis, and the incidence of sepsis in fUTI patients was 23.5%. The result shows a significant correlation between NLR and fUTI (95% confidence interval [CI],1.21–1.83, Odds ratio [OR]=1.49, p<0.001). The predictive ability of NLR on the occurrence of fUTI was assessed by plotting relative operating characteristic (ROC) curves. The area under the curve (AUC) in the ROC curve for NLR was 0.718 according to the Youden index, and the best cut-off value of NLR was 2.71. Furthermore, logistic multiple regression model adjustment was carried out to further confirm the robustness of the relationship between NLR and fUTI. The results indicated robustness regardless of whether NLR was a continuous variable or a categorical variable.
Conclusion
NLR can be used as a simple and effective preoperative indicator for the prediction of fUTI in patients undergoing PCNL.
Keywords: percutaneous nephrolithotomy, febrile urinary tract infection, neutrophil–lymphocyte ratio
Introduction
Percutaneous nephrolithotomy (PCNL) is recommended as the primary option for kidney stones larger than 2 cm and infected stones. In cases of failed extracorporeal shock wave lithotripsy (ESWL) and endourology for stones between 1 and 2 cm, PCNL is still an effective treatment method.1,2 Severe infection may occur after PCNL, and some patients may even develop sepsis. According to relevant literature reports, the incidence rate of sepsis is between 2.4% and 5.1%.3,4 Therefore, preoperatively identifying the patients at a high risk of postoperative infection holds great significance. Clinicians can take corresponding measures to reduce postoperative infection complications.
Systemic inflammatory response syndrome (SIRS) is regarded as the initial condition for sepsis.5 It is determined by monitoring respiratory rate, heart rate, body temperature, and blood test. There was also a study that reported a correlation between preoperative neutrophil–lymphocyte ratio (NLR) and postoperative SIRS.6 In practical situations, respiratory rate and heart rate may be affected by some objective or subjective factors, such as postoperative pain, patient’s nervousness, and some heart diseases, which may affect the doctor’s diagnosis of SIRS. However, fever is the main early symptom of sepsis and is also one of the diagnostic criteria for SIRS, which is hardly affected by other factors. Postoperative febrile urinary tract infection (fUTI) is defined as postoperative fever body temperature ≥38°C, which is the most common complication after PCNL. By the time patients developing fUTI after PCNL exhibit symptoms, SIRS or sepsis has likely occurred. The condition eventually leads to prolonged hospitalization and increased financial burden. Although NLR is a well-known marker of systemic inflammation and infection, the association between NLR and fUTI remains unclear in patients undergoing PCNL.
A retrospective observational study was conducted to solve this problem. This study aimed to evaluate the association between NLR and fUTI in patients who underwent PCNL.
Materials and Methods
Materials
The clinical data from a tertiary hospital (302 Hospital of China Guizhou Aviation Industry Group) between March 2020 and May 2023 were retrospectively analyzed. These patients were subjected to PCNL in the prone position. All patients underwent computed tomography to accurately measure the stones and relevant blood biochemical tests were performed within two days before surgery. None of the patients had a fever for three days before surgery. Inclusion Criteria: 1. All patients with definite preoperative diagnosis and no surgical contraindications to undergo PCNL; 2. Postoperative fUTI diagnosis was clear, without any other infection site; 3. Preoperative nitrite was negative. Patients with blood system diseases, tumors or abnormal immune function, positive urine culture, other infections, or two-stage surgery were excluded from the study. Patients with preoperative infection were treated with antibiotics. The patients were administered antibiotics 30 min before the surgery as standard antibiotic prophylaxis. Opioids were given for postoperative pain relief, and non-steroidal anti-inflammatory drugs were not given. Blood and urine cultures were performed in patients with fUTI.
Procedure of Operation
The patient was placed in the lithotomy position of the bladder after under general anesthesia. An F5 ureteral catheter was inserted into the affected renal pelvis through an F8/9.8 rigid ureteroscope through the urethra to create an “artificial hydronephrosis” for convenient positioning. The area between the posterior axillary line and the shoulder line of the affected side was examined under ultrasound, and the zebra guide wire was inserted after the puncture. The fascia dilator was used to establish the surgical channel in sequence. After using the holmium laser, the ureteral catheter was pulled out, and the F6.0 double J tube was indwelling along the zebra guide wire anterograde; the endoscope was removed and the fixed nephrostomy tube was placed. The intraoperative renal pelvic lavage pressure was maintained at a constant level and the operation process and surgical instruments were the same.
Data Collection
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection.7 The vital signs of patients were routinely monitored up to 72 hours after surgery. Patient information was collected from the hospital information system. The preoperative and operative conditions of the patient were collected, including general clinical data, preoperative blood test results, stone characteristics, and surgical data. In addition, the occurrence of fUTI in each patient after surgery and the outcome of each patient was recorded.
Statistical Analysis
For continuous variables, data are shown as mean± standard deviation (SD) or median with interquartile range (IQR) and for categorical variables as frequency or percentage. Univariate analysis was conducted to verify the relationship between fUTI and each variable. Significant variables in the univariate analysis and important clinical factors such as age were included as covariates. Subsequently, multivariable logistic regression analysis was performed to evaluate the independent association between NLR and fUTI. An extended logistic analysis was applied to analyze different covariates-adjusted models. We plotted the receiver operating characteristic (ROC) curve to evaluate the diagnostic value of NLR for fUTI.
All the analyses were performed with the statistical software packages R 3.3.2 (http://www.R-project.org, The R Foundation) and Free Statistics software version 1.8. For data analysis results, p value <0.05 was considered statistically significant.
Results
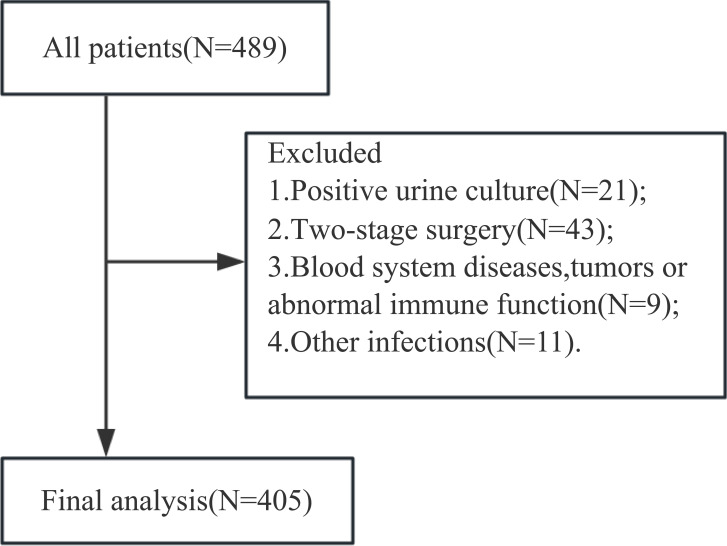
The clinical data of 489 patients were collected, following the strict inclusion and exclusion criteria, 405 patients (135 females and 270 males) were finally enrolled in the study (Figure 1).
Figure 1.
Flowchart of patient selection steps.
The baseline characteristics between groups with and without fUTI are presented in Table 1. The incidence of fUTI was 8.4% (34/405) and 8 of the patients developed sepsis; the incidence of sepsis in fUTI patients was 23.5%. Three were transferred to the intensive care unit after surgery due to their critical condition and were finally discharged after recovery. None of the patients died in this study. The general clinical characteristics of the two groups were compared, revealing significant differences in gender, neutrophil count, lymphocyte count, hemoglobin, albumin, globulin, stone size, and operative time (p<0.05). In contrast, no statistically significant differences were observed in age, body mass index (BMI), underlying diseases (diabetes, hypertension, and heart disease), stone characteristics (stone number and staghorn stone), and surgical puncture channel (p>0.05). Furthermore, univariate analysis with logistic regression was performed to explore the confounding factors of fUTI after PCNL, as displayed in Table 2. The results indicated a significant correlation between NLR and fUTI (95% confidence interval [CI],1.21–1.83, Odds ratio [OR]=1.49, p<0.001). In addition, gender (p=0.013), neutrophil count (p=0.031), lymphocyte count (p=0.013), albumin (p=0.011), globulin (p=0.006), hemoglobin (p<0.001), stone size (p=0.023), and operation time (p=0.004) were correlated with the occurrence of fUTI.
Table 1.
The Baseline Characteristics of the Subjects Between fUTI Group and Non- fUTI Group
| Variables | Total (N = 405) | Non-fUTI (N = 371) | fUTI (N = 34) | p |
|---|---|---|---|---|
| Gender | 0.011 | |||
| Female | 135 (33.3) | 117 (31.5) | 18 (52.9) | |
| Male | 270 (66.7) | 254 (68.5) | 16 (47.1) | |
| Age(years) | 48.6 ± 14.5 | 48.3 ± 14.4 | 52.3 ± 14.8 | 0.124 |
| BMI(kg/m2) | 23.3 (21.0, 25.7) | 23.3 (21.0, 25.7) | 22.8 (20.7, 25.6) | 0.986 |
| Diabetes | 0.179 | |||
| No | 372 (91.9) | 343 (92.5) | 29 (85.3) | |
| Yes | 33 (8.1) | 28 (7.5) | 5 (14.7) | |
| Hypertension (%) | 0.929 | |||
| No | 324 (80.0) | 297 (80.1) | 27 (79.4) | |
| Yes | 81 (20.0) | 74 (19.9) | 7 (20.6) | |
| Heart disease (%) | 0.495 | |||
| No | 375 (92.6) | 342 (92.2) | 33 (97.1) | |
| Yes | 30 (7.4) | 29 (7.8) | 1 (2.9) | |
| Hb(g/L) | 144.0 (130.0, 156.0) | 145.0 (132.0, 156.0) | 125.0 (105.5, 140.0) | < 0.001 |
| Neutrophil count(×109) | 4.1 (3.3, 5.0) | 4.0 (3.2, 4.9) | 4.5 (3.8, 5.2) | 0.035 |
| Lymphocyte count(×109) | 1.6 (1.2, 1.9) | 1.6 (1.3, 1.9) | 1.2 (1.0, 1.7) | 0.004 |
| Albumin(g/L) | 42.8 (39.7, 45.0) | 42.9 (40.0, 45.2) | 41.6 (37.2, 44.0) | 0.016 |
| Globin(g/L) | 30.3 (27.4, 33.6) | 30.1 (27.3, 33.2) | 32.1 (29.5, 35.2) | 0.006 |
| NLR | 2.5 (2.0, 3.3) | 2.4 (2.0, 3.3) | 3.3 (2.8, 4.5) | < 0.001 |
| Stone size(cm) | 2.0 (1.8, 2.5) | 2.0 (1.8, 2.5) | 2.3 (2.0, 2.5) | 0.007 |
| Stone number | 0.2 | |||
| Single | 57 (14.1) | 55 (14.8) | 2 (5.9) | |
| Multiple | 348 (85.9) | 316 (85.2) | 32 (94.1) | |
| Staghorn stone | 1 | |||
| No | 377 (93.1) | 345 (93) | 32 (94.1) | |
| Yes | 28 (6.9) | 26 (7) | 2 (5.9) | |
| Puncture channel | 0.558 | |||
| Small channel | 365 (90.1) | 333 (89.8) | 32 (94.1) | |
| Standard channel | 40 (9.9) | 38 (10.2) | 2 (5.9) | |
| OT(minutes) | 68.0 (58.0, 85.0) | 68.0 (57.0, 84.5) | 87.0 (65.0, 104.5) | 0.005 |
Notes: For continuous variables, data are showed as mean± standard deviation or median with interquartile range and for categorical variables as frequency or percentage.
Abbreviations: fUTI, febrile urinary tract infection; BMI, body mass index; Hb, hemoglobin; NLR, neutrophil–lymphocyte ratio; OT, operation time.
Table 2.
Univariate Analyses for Predicting fUTI After PCNL
| Variable | OR 95% CI | p |
|---|---|---|
| Gender | 0.41 (0.20~0.83) | 0.013 |
| Age | 1.02 (0.99~1.05) | 0.125 |
| BMI | 1.01 (0.9~1.12) | 0.908 |
| Diabetes | 2.11 (0.76~5.88) | 0.153 |
| Hypertension | 1.04 (0.44~2.48) | 0.929 |
| Heart disease | 0.36 (0.05~2.71) | 0.319 |
| Hb | 0.96 (0.94~0.98) | <0.001 |
| Neutrophil count | 1.30 (1.02~1.65) | 0.031 |
| Lymphocyte count | 0.37 (0.17~0.81) | 0.013 |
| Albumin | 0.9 (0.83~0.98) | 0.011 |
| Globin | 1.09 (1.03~1.17) | 0.006 |
| NLR | 1.49 (1.21~1.83) | <0.001 |
| Stone size | 1.77 (1.08~2.9) | 0.023 |
| Stone number | 2.78 (0.65~11.96) | 0.168 |
| Staghorn stone | 0.83 (0.19~3.65) | 0.805 |
| Puncture channel | 0.55 (0.13~2.38) | 0.421 |
| OT | 1.02 (1.01~1.04) | 0.004 |
Abbreviations: fUTI, febrile urinary tract infection; PCNL, percutaneous nephrolithotomy; BMI, body mass index; Hb, hemoglobin; NLR, neutrophil–lymphocyte ratio; OT, operation time. OR: odds ratio.
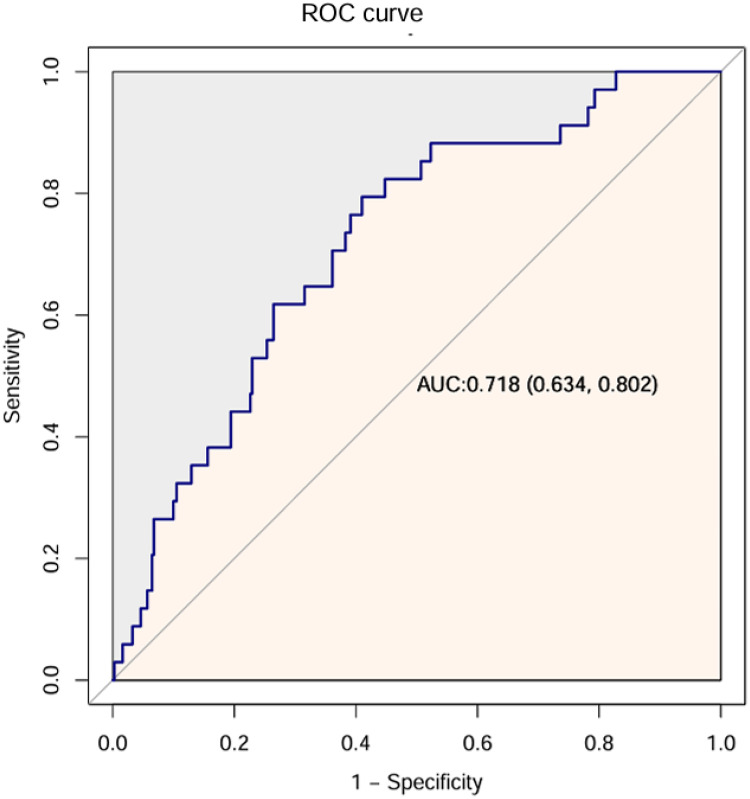
To further assess the predictive ability of NLR on the occurrence of fUTI, ROC curves were plotted (Figure 2). The area under the curve (AUC) in the ROC curve was 0.718 according to the Youden index, and the best cut-off value of NLR was 2.71. Patients from the high and low NLR groups were compared in Table 3, and patients in the high NLR groups were older (p<0.001) and had higher neutrophil counts (p<0.001) and lower lymphocyte counts (p<0.001). To further evaluate the robustness of the association between NLR and fUTI, logistic multiple-regression model adjustment was conducted, as shown in Table 4. The results revealed its robustness regardless of whether NLR was a continuous variable or a categorical variable.
Figure 2.
ROC curve analysis results of NLR in predicting postoperative fUTI.
Abbreviations: ROC, relative operating characteristic; AUC, area under the curve; fUTI, febrile urinary tract infection; NLR, neutrophil–lymphocyte ratio.
Table 3.
Baseline Characteristics of Patients with Low and High NLR
| Variables | Lower NLR (NLR <2.71) | Higher NLR (NLR ≥2.71) | p |
|---|---|---|---|
| No. of patients | 226 | 179 | |
| fUTI(%) | 7 (3.1) | 27 (15.1) | < 0.001 |
| Gender(%) | 0.887 | ||
| Female | 76 (33.6) | 59 (33) | |
| Male | 150 (66.4) | 120 (67) | |
| Age(years) | 46.0 ± 14.1 | 51.9 ± 14.3 | < 0.001 |
| BMI(kg/m2) | 23.4 (21.0, 25.7) | 22.8 (20.9, 25.7) | 0.441 |
| Diabetes | 0.562 | ||
| No | 206 (91.2) | 166 (92.7) | |
| Yes | 20 (8.8) | 13 (7.3) | |
| Hypertension (%) | 0.121 | ||
| No | 187 (82.7) | 137 (76.5) | |
| Yes | 39 (17.3) | 442 (23.5) | |
| Heart disease (%) | 0.921 | ||
| No | 209 (92.5) | 166 (92.7) | |
| Yes | 17 (7.5) | 13 (7.3) | |
| Hb(g/L) | 145.0 (132.0, 156.0) | 141.0 (126.0, 155.0) | 0.084 |
| Neutrophil count(×109) | 3.6 (3.0, 4.3) | 4.8 (3.9, 5.8) | < 0.001 |
| Lymphocyte count(×109) | 1.8 (1.5, 2.1) | 1.3 (1.0, 1.6) | < 0.001 |
| Albumin(g/L) | 42.9 (40.0, 45.2) | 42.4 (39.4, 44.5) | 0.338 |
| Globin(g/L) | 30.3 (27.2, 33.2) | 30.5 (27.6, 34.0) | 0.356 |
| Stone size(cm) | 2.0 (1.8, 2.5) | 2.1 (2.0, 2.5) | 0.054 |
| Stone number | 0.731 | ||
| Single | 33 (14.6) | 24 (13.4) | |
| Multiple | 193 (85.4) | 1155 (86.6) | |
| Staghorn stone | 0.084 | ||
| No | 206 (91.2) | 171 (95.5) | |
| Yes | 220 (8.8) | 8 (4.5) | |
| Puncture channel | 0.057 | ||
| Small channel | 198 (87.6) | 1167 (93.3) | |
| Standard channel | 28 (12.4) | 112 (6.7) | |
| OT(minutes) | 70.0 (56.2, 85.0) | 66.5 (58.0, 85.0) | 0.771 |
Abbreviations: fUTI, febrile urinary tract infection; BMI, body mass index; Hb, hemoglobin; NLR, neutrophil–lymphocyte ratio; OT, operation time.
Table 4.
The Association Between NLR and fUTI by Multivariate Logistic Regression Analysis
| Nonadjusted | Adjust I | Adjust II | Adjust III | |
|---|---|---|---|---|
| NLR | 1.49 (1.21~1.83) | 1.49 (1.2~1.86) | 1.07 (0.5~2.29) | 1.1 (0.5~2.39) |
| NLR<2.71 | 1 | 1 | 1 | 1 |
| NLR≥2.71 | 5.56 (2.36~13.09) | 5.63 (2.34~13.53) | 5.02 (1.42~17.8) | 5.23 (1.44~18.99) |
Notes: data presented are ORs and 95% CIs. Adjust I model adjusts for age and gender; adjust II model adjusts for adjust I + hemoglobin, albumin, globin, neutrophil count, lymphocyte count and stone size; adjust III model adjusts for adjust II + operation time.
Abbreviations: fUTI, febrile urinary tract infection; NLR, neutrophil–lymphocyte ratio; OR, odds ratio; CI, confidence interval.
Discussion
The occurrence of fUTI after PCNL is relatively common. There were few studies exploring the relationship in patients treated by PCNL between preoperative NLR and fUTI, so we conducted a retrospective study to assess whether there was an association. NLR was found to be an independent risk factor for fUTI after PCNL and showed good predictive power. Moreover, gender, neutrophil count, lymphocyte count, albumin, globulin, hemoglobin, stone size, and operation time were risk factors for fUTI. This minimally invasive procedure was also associated with a higher risk of infection and bleeding complications.8,9 Despite the advent of flexible ureteroscopic lithotripsy to treat upper urinary stones,10 PCNL remains irreplaceable in some cases due to stone load and location.1
Preoperative NLR is related to the prognosis of tumors and is closely related to the occurrence of postoperative infection.11,12 It is a readily available inflammatory biomarker. A meta-analysis of 12 studies confirmed preoperative NLR as a predictor of postoperative infectious complications.13 In a large database analysis, procalcitonin and NLR exhibited important predictive value for bloodstream infection, while lactate concentration and white blood cell count had little value.14 Inflammatory mediators are released due to the presence of stones, which in turn increases neutrophil counts, while the immune response is suppressed by the inflammatory response with decreasing the cytolytic activity of lymphocytes, T cells, and natural killer cells.6 The increase in neutrophil counts and decline in lymphocyte counts are features of physiological immune response of circulating leucocytes to all kinds of stressful events.15 Percutaneous nephrolithotomy is often accompanied by impaired vascular integrity and an increase in renal pelvic pressure; hence, a large number of inflammatory mediators are released into the blood, eventually leading to persistent hyperinflammation and immunosuppression.16 Postoperative fever is relatively common following PCNL,17 and complications related to infection after PCNL include transient fever, SIRS, and sepsis, which depend on the severity.5 A body temperature ≥38°C after PCNL is one of the main clinical manifestations of infection. Attention should be paid to fUTI after surgery, and corresponding measures should be undertaken as soon as possible to avoid further progression.
Many related studies have investigated infection after PCNL.3,18–20 Sen performed a study of 487 patients who underwent PCNL and concluded that there was a significant relationship between the preoperative NLR and the occurrence of postoperative sepsis. The ROC curve analysis revealed an NLR cut-off of 2.50 for predicting the occurrence of SIRS/sepsis.4 Kriplani also conducted a retrospective study, reporting that preoperative NLR as early identification of PCNL was an effective predictor of postoperative SIRS or sepsis.6 These studies also indicated that the preoperative NLR is associated with infection after percutaneous nephrolithotripsy, which is consistent with the report of our study.
Infection is one of the major complications after PCNL, while SIRS is an early disease manifestation stage of sepsis.21 In particular, many studies have explored the correlation between preoperative clinical indicators and postoperative SIRS.1,5,6,22,23 It needs to measure the patient’s heart rate and respiratory rate after surgery, which is affected by the patient’s underlying disease or non-infectious factors. This study only measured the patient’s body temperature after surgery, which is a relatively simple process. In addition, our patients had strict inclusion and exclusion criteria. Unlike previous research, the current study confirmed the reliability of the results by performing adjustments of multiple regression models, which added to the robustness of the results.
Nevertheless, the limitations of the study should be acknowledged. First, this is a retrospective and single-center analysis, which may include some bias in the data selection. Secondly, this study defined fUTI as postoperative body temperature ≥38°C, and the entire research was based on this premise. Third, on account of the limited sample scale, subgroup analyses were not carried out to avoid drawing unreliable conclusions. Finally, in this study, we only used NLR as an infection marker for analysis, without adding other infection marker such as procalcitonin and C-reactive protein. In the future, large multicenter prospective studies across different regions and simultaneous analysis of multiple markers of infection are required to confirm these results.
Conclusion
This study evaluated the association between preoperative NLR and fUTI, and the results showed that a higher preoperative NLR was significantly associated with the occurrence of fUTI. Therefore, NLR helps to identify patients at high risk for postoperative fUTI. However, the manifestations of infection are diverse, and other markers of infection have not been studied, so we need a comprehensive evaluation of many aspects in order to make the best decision to reduce the occurrence of infection.
Funding Statement
This study was supported by grants from Medical Health Science and Technology Project of Guizhou Provincial Health Commission: gzwkj2023-376, gzwkj2023-378, Guizhou Provincial Basic Research Program(Natural Science):QianKeHe Basic-ZK[2023]General 472 and Guangzhou Core Medical Disciplines Project(2021-2023).
Data Sharing Statement
Data are available upon reasonable request, but the data are not publicly available due to them containing information that could compromise research participant privacy.
Ethics Approval
This study was approved by the Ethics Committee of 302 Hospital of China Guizhou Aviation Industry Group (reference number: KJLL202001), and all the research processes were performed in strict compliance with the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.De Lorenzis E, Zanetti SP, Boeri L, Montanari E. Is there still a place for percutaneous nephrolithotomy in current times? J Clin Med. 2022;11(17):5157. doi: 10.3390/jcm11175157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghani KR, Andonian S, Bultitude M, et al. Percutaneous nephrolithotomy: update, trends, and future directions. Eur Urol. 2016;70(2):382–396. doi: 10.1016/j.eururo.2016.01.047 [DOI] [PubMed] [Google Scholar]
- 3.Bultitude M, Thomas K. Predicting sepsis after percutaneous nephrolithotomy. BJU Int. 2019;123(6):914–915. doi: 10.1111/bju.14623 [DOI] [PubMed] [Google Scholar]
- 4.Sen V, Bozkurt IH, Aydogdu O, et al. Significance of preoperative neutrophil-lymphocyte count ratio on predicting postoperative sepsis after percutaneous nephrolithotomy. Kaohsiung J Med Sci. 2016;32(10):507–513. doi: 10.1016/j.kjms.2016.08.008 [DOI] [PubMed] [Google Scholar]
- 5.Wu W, Zhang D, Jin T, Lu T, Zhou F. Progress in the study of biomarkers for early prediction of systemic inflammatory response syndrome after percutaneous nephrolithotomy. Front Immunol. 2023;14:1142346. doi: 10.3389/fimmu.2023.1142346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kriplani A, Pandit S, Chawla A, et al. Neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR) and lymphocyte-monocyte ratio (LMR) in predicting systemic inflammatory response syndrome (SIRS) and sepsis after percutaneous nephrolithotomy (PNL). Urolithiasis. 2022;50(3):341–348. doi: 10.1007/s00240-022-01319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganpule AP, Vijayakumar M, Malpani A, Desai MR. Percutaneous nephrolithotomy (PCNL) a critical review. Int J Surg. 2016;36(Pt D):660–664. doi: 10.1016/j.ijsu.2016.11.028 [DOI] [PubMed] [Google Scholar]
- 9.Mykoniatis I, Pietropaolo A, Pyrgidis N, et al. Mini percutaneous nephrolithotomy versus standard percutaneous nephrolithotomy for the management of renal stones over 2 cm: a systematic review and meta-analysis of randomized controlled trials. Minerva Urol Nephrol. 2022;74(4):409–417. doi: 10.23736/S2724-6051.22.04678-X [DOI] [PubMed] [Google Scholar]
- 10.Proietti S, Knoll T, Giusti G. Contemporary ureteroscopic management of renal stones. Int J Surg. 2016;36(Pt D):681–687. doi: 10.1016/j.ijsu.2016.11.130 [DOI] [PubMed] [Google Scholar]
- 11.Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88(1):218–230. doi: 10.1016/j.critrevonc.2013.03.010 [DOI] [PubMed] [Google Scholar]
- 12.Takahara K, Tamura R, Kuranari Y, Karatsu K, Akiyama T, Toda M. Prognostic significance of preoperative neutrophil-to-lymphocyte ratio in surgically resected schwannomas. Front Oncol. 2023;13:1099384. doi: 10.3389/fonc.2023.1099384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qian B, Zheng Y, Jia H, Zheng X, Gao R, Li W. Neutrophil-lymphocyte ratio as a predictive marker for postoperative infectious complications: a systematic review and meta-analysis. Heliyon. 2023;9(5):e15586. doi: 10.1016/j.heliyon.2023.e15586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marik PE, Stephenson E. The ability of procalcitonin, lactate, white blood cell count and neutrophil-lymphocyte count ratio to predict blood stream infection. Analysis of a large database. J Crit Care. 2020;60:135–139. doi: 10.1016/j.jcrc.2020.07.026 [DOI] [PubMed] [Google Scholar]
- 15.de Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14(5):R192. doi: 10.1186/cc9309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG, van de Veerdonk FL. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17(7):407–420. doi: 10.1038/nri.2017.36 [DOI] [PubMed] [Google Scholar]
- 17.Wollin DA, Preminger GM. Percutaneous nephrolithotomy: complications and how to deal with them. Urolithiasis. 2018;46(1):87–97. doi: 10.1007/s00240-017-1022-x [DOI] [PubMed] [Google Scholar]
- 18.Peng C, Li J, Xu G, Jin J, Chen J, Pan S. Significance of preoperative systemic immune-inflammation (SII) in predicting postoperative systemic inflammatory response syndrome after percutaneous nephrolithotomy. Urolithiasis. 2021;49(6):513–519. doi: 10.1007/s00240-021-01266-2 [DOI] [PubMed] [Google Scholar]
- 19.Ganesan V, Brown RD, Jiménez JA, De S, Monga M. C-reactive protein and erythrocyte sedimentation rate predict systemic inflammatory response syndrome after percutaneous nephrolithotomy. J Endourol. 2017;31(7):638–644. doi: 10.1089/end.2016.0884 [DOI] [PubMed] [Google Scholar]
- 20.Chen D, Jiang C, Liang X, et al. Early and rapid prediction of postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones. BJU Int. 2019;123(6):1041–1047. doi: 10.1111/bju.14484 [DOI] [PubMed] [Google Scholar]
- 21.Ismail J, Sankar J. Systemic inflammatory response syndrome (sirs) and sepsis - an ever-evolving paradigm. Indian J Pediatr. 2015;82(8):675–676. doi: 10.1007/s12098-015-1810-7 [DOI] [PubMed] [Google Scholar]
- 22.Zhou H, Xie T, Gao Y, Yao X, Xu Y. The relationship between preoperative urine culture and post-percutaneous nephrostolithotomy systemic inflammatory response syndrome: a single-center retrospective study. J Pers Med. 2023;13(2):187. doi: 10.3390/jpm13020187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu H, Hu L, Wei X, et al. The predictive value of preoperative high-sensitive c-reactive protein/albumin ratio in systemic inflammatory response syndrome after percutaneous nephrolithotomy. J Endourol. 2019;33(1):1–8. doi: 10.1089/end.2018.0632 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request, but the data are not publicly available due to them containing information that could compromise research participant privacy.