Key Points
-
•
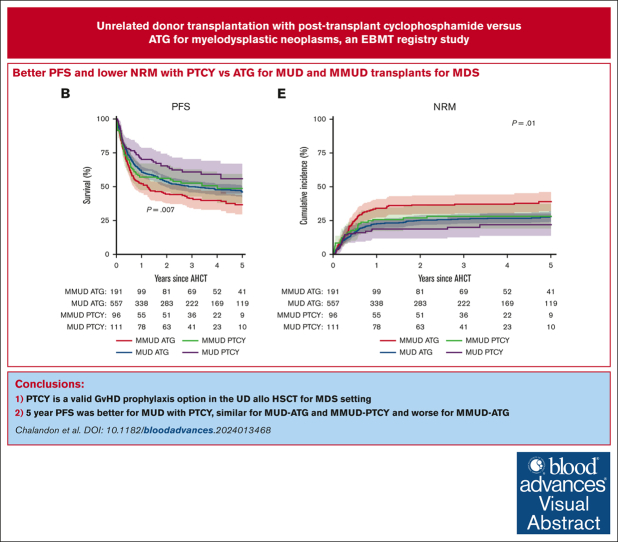
UDs transplant with PTCY for myelodysplastic neoplasms may improve OS and PFS as compared with ATG.
-
•
PTCY may also decrease the incidence of grade 2 to 4 acute GVHD.
Visual Abstract
Abstract
It has been reported in prospective randomized trials that antithymocyte globulin (ATG)–based graft-versus-host disease (GVHD) prophylaxis has benefits in the setting of allogeneic hematopoietic stem cell transplantation (allo-HSCT) with unrelated donors (UDs). However, the optimal GVHD prophylaxis strategy has been challenged recently by the increasing use of posttransplant cyclophosphamide (PTCY). We report from the European Society for Blood and Marrow Transplantation registry the outcomes of 960 patients with myelodysplastic neoplasms who underwent allo-HSCT from UD with PTCY or ATG as GVHD prophylaxis. The primary outcomes were overall survival (OS) and progression-free survival (PFS). The disease characteristics were similar in both groups. Day 28 neutrophil engraftment was significantly better with ATG (93% vs 85%). Over a median follow-up of 4.4 years, the 5-year OS was 58% with PTCY, and 49% in the ATG group. The 5-year PFS was higher for PTCY at 53% vs 44% for ATG. Grade 2 to 4 acute GVHD incidence was lower when PTCY was used (23%), whereas there was no difference in the incidence of chronic GVHD at 5 years. Multivariable analyses confirmed better OS and PFS with PTCY with a hazard ratio (HR) for ATG of 1.32 (1-1.74) and a better PFS for PTCY with a HR for ATG of 1.33. This study suggests that GVHD prophylaxis using PTCY instead of ATG in this setting remains a valid option. Further prospective randomized studies would be essential to confirm these results.
Introduction
Myelodysplastic syndromes (MDS) or neoplasms are a heterogenous group of myeloid malignancies that are characterized by abnormal marrow cellular maturation and that frequently lead to varying degrees of cytopenia and an inherent risk for transformation to acute myeloid leukemia (AML).1,2 A number of prognostic scores have been developed to guide the decision-making process, because patients with low-risk scores may need supportive care alone. Conversely, higher-risk patients may be candidates for hypomethylating agents (HMAs) or allogeneic hematopoietic stem cell transplantation (allo-HSCT), which remains the only curative option depending on individual characteristics, such as age and performance status.3,4 In recent years, advances in allo-HSCT conditioning regimens and intensity have led to lower rates of transplant-related toxicity, hence, extending this potential option to older patients or to those with comorbidities.5, 6, 7 Notably, improvements in graft-versus-host disease (GVHD) prophylaxis strategies have contributed to lower toxicity rates. Indeed, phase 3 trials have demonstrated the advantage of antithymocyte or antilymphocyte globulins (ATGs) over observation or placebo treatment with a lower incidence of chronic GVHD.8, 9, 10 Although posttransplantation cyclophosphamide (PTCY) has been successfully used in the haplo-identical transplant setting, it has more recently been extended successfully to the HLA-matched donor allo-HSCT setting and in the mismatched unrelated donor (MMUD) allo-HSCT setting.11, 12, 13, 14, 15, 16 Indeed, PTCY has been reported in phase 2 and 3 trials to improve graft-versus-host–free, disease-free survival (GRFS) in patients with hematological malignancies when compared with PTCY-free GVHD prophylaxis.11, 12, 13, 14, 15, 16 After a myeloablative conditioning (MAC) regimen and in the HLA-matched donor setting, the phase 3 BMT CTN1301 trial reported similar outcomes following PTCY use alone when compared with tacrolimus in combination with mycophenolate mofetil (MMF).14 The phase 3 BMT CTN1703 compared PTCY, tacrolimus, and MMF with tacrolimus and methotrexate in the HLA matched, reduced intensity conditioning regimen (RIC) setting, showing lower risks for grade 3 to 4 acute GVHD (aGVHD) and chronic GVHD (cGVHD) and a consequent improvement in GRFS.11 In a similarly selected population (RIC and HLA matched), the phase 3 HOVON 96 trial compared PTCY and cyclosporin with ciclosporin and MMF, highlighting lower risks for grade 2 to 4 aGVHD and cGVHD.13 However, in these prospective trials, the reference arm did not contain ATG, and the analysis included all diseases with the majority representing AML and no specific subgroup analysis for MDS. PTCY and ATG have both been used for patients with myeloid malignancies who underwent allo-HSCT in the setting of matched unrelated donors (MUD) with outcomes approaching those of transplants with matched related donors.5,9,17, 18, 19, 20, 21 However, the optimal GVHD prophylaxis strategy for patients with MDS who underwent allo-HSCT with an UD remains controversial. Therefore, we performed a retrospective, European Society for Blood and Marrow Transplantation (EBMT) registry–based study to evaluate the outcomes of patients with MDS who underwent a first allo-HSCT from a MUD or an HLA- MMUD and who received either ATG or PTCY as GVHD prophylaxis.
Patients and methods
This was a retrospective, multicenter, registry-based study that was approved by the Chronic Malignancies Working Party of the EBMT in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. The EBMT is a nonprofit scientific society that represents >600 transplant centers, mainly in Europe. EBMT centers commit to obtain informed consent according to the local regulations applicable at the time of transplantation to report pseudonymized data to the EBMT. The data are entered, managed, and maintained in a central database with Internet access; each EBMT center is represented in this database. Patient selection included patients who underwent their first allo-HSCT for MDS between 2012 to 2019 from a MUD (10/10) or MMUD (<10/10) and who received either PTCY-based or ATG-based GVHD prophylaxis (supplemental Figure 1). Allo-HSCTs that used other donor types, alternative stem cell sources, or ex vivo T-cell depletion were excluded. Performance status was assessed using the reported Karnofsky Performance Status and comorbidities via the hematopoietic cell transplantation-specific comorbidity index (HCT-CI). Based on these criteria, a total of 960 adults were identified in the EBMT registry database.
Neutrophil engraftment was defined as the first day of 3 consecutive days of a neutrophil count >0.5 × 109/L and platelet engraftment was defined as the first day of a platelet count >20 × 109/L for 7 consecutive days without transfusion support. Primary graft failure was defined as failure to reach a neutrophil count >0.5 × 109/L in the first 28 days after stem cell transplantation or documentation of autologous reconstitution by chimerism analysis in the absence of relapse. Secondary graft failure was defined by the treating physician; standard criteria across Europe would be loss of a functioning graft demonstrated by cytopenia in at least 2 lineages and loss of donor chimerism without relapse of the primary disease. Complete remission was defined if all the following were achieved: hemoglobin >11 g/dL, platelet >100 × 10/L9, and neutrophils >1.5 × 109/L with <5% blasts in the bone marrow. Relapse was defined as loss of complete remission. Conditioning regimens were defined as MAC if they contained either total body irradiation with a dose of >6 Gy, oral busulfan dosage >8 mg/kg, or a dose of IV busulfan >6.4 mg/kg.22,23 aGVHD was graded according to 2 different established criteria depending on the year of aGVHD diagnosis.24,25 cGVHD was assessed using 2 established National Institutes of Health criteria.26 Following the information reported in the EBMT registry, the severity of cGVHD was graded according to the National Institutes of Health criteria (mild, moderate, and severe).
Statistics
The type of GVHD prophylaxis used for allo-HSCT (PTCY based vs ATG based) was considered the main variable of interest in this study. The primary outcomes were overall survival (OS), progression-free survival (PFS), and grade 3 to 4 aGVHD and extensive cGVHD-free and relapse-free survival (GRFS). Secondary outcomes were relapse, nonrelapse mortality (NRM), aGVHD and cGVHD, and neutrophil and platelet engraftment.
Statistics followed the EBMT guidelines.27 OS, PFS, and GRFS were estimated using the Kaplan-Meier product limit estimation method, and differences in subgroups were assessed using the log-rank test. The median follow-up was determined using the reverse Kaplan-Meier method. The cumulative incidences of relapse or NRM, aGVHD grade 2 to 4 and 3 to 4, overall cGVHD, and limited and extensive cGVHD were analyzed separately in a competing risks framework. In all GVHD-related outcomes, relapse and death were considered competing events. Relapse and death were competing events for NRM and relapse incidence (RI), respectively. Competing risks analyses were also used to analyze the cumulative incidences of neutrophil engraftment and platelet engraftment, each with competing event death. Subgroup differences in the cumulative incidences were assessed using Gray test. In univariable analyses, patients who were alive and in follow-up by 5 years after the transplant were censored at that time with the exception of aGVHD, platelet, and neutrophil engraftment, which were censored at days 100, 100, and 28, respectively. All estimates are given with 95% confidence intervals (CIs) in parentheses when appropriate.
The impact of the main explanatory variable (type of GVHD prophylaxis) and other risk factors on OS and PFS were explored using multivariable Cox regression analyses. The baseline risk factors included in each of the multivariable models were selected based on clinical judgment before the analysis. Cases with missing data for covariates or outcomes were excluded from the respective model. The models included the main study variable of GVHD prophylaxis (ATG based vs PTCY based). Any other included covariates are considered adjustment factors. All models additionally included the covariate constellation Revised International Prognostic Scoring System (IPSS-R) cytogenetics at diagnosis (intermediate, poor, and very poor vs good), donor match (MMUD vs MUD), age at allo-HSCT (by decade), HMA pretreatment (yes vs no), HCT-CI (intermediate and high vs low risk), and MDS stage at diagnosis (excess blast [EB] type 1/2 vs other). A potential center effect was accommodated for by the inclusion of a gamma frailty random effect for center. The corresponding P values were calculated using likelihood ratio tests by comparing models with identical fixed effects with and without the frailty term. P values were calculated using unadjusted Wald tests.
Continuous pretransplant variables were summarized using the median and interquartile range (IQR) and categorical pretransplant variables were summarized using percentages within the group of patients with available data. Group differences between the PTCY based and other prophylaxis subgroups were assessed using χ2 tests for categorical baseline variables and t tests for continuous baseline variables. All P values were 2-sided, and P <.05 was considered significant. Statistical analyses were performed using R, version 3.6.0 (R Development Core Team, Vienna, Austria), and the packages survival, prodlim, cmprsk, frailtyEM, and risk Regression.
Results
Patient characteristics
The patient characteristics are described in Table 1. A total of 209 patients received PTCY, and 751 received ATG as GVHD prophylaxis. We had data on 569 of 751 (76%) patients who received ATG with 305 (53.5%) receiving ATG in the form of Thymoglobulin at a median dose of 5 mg/kg (range, 1-10) and 264 (46.4%) receiving Grafalon at a median dose of 30 mg/kg (range, 20-60). Of note, 14 patients received Thymoglobulin at a dose of ≥10 mg/kg and 63 received Grafalon at a dose of ≥60 mg/kg. Patients within the ATG cohort were older (60.1 years [IQR, 50.6-65.2] vs 57.1 years [IQR, 46.5-63.9]; P = .006). Disease characteristics were similar across the PTCY and ATG groups. There was a total of 576 patients in the entire group with MDS with EB; at diagnosis, there were 503 patients with MDS-EB and 206 patients transformed into AML at the time of allo-HSCT. Among patients with available data to calculate the IPSS-R (n = 533) at diagnosis, risk categorization was as follows: 35 (6.6%) were very low, 86 (16.1%) were low, 146 (27.4%) were intermediate, 157 (29.5%) were high, and 109 (20.5%) were very high. Patients within the PTCY cohort were more likely to receive HMA before the transplant (56.1% vs 42.3%; P = .001) and underwent transplantation more frequently using an HLA-mismatched 9/10 donor (46.4% vs 25.4%; P < .001). Conditioning regimen intensity was more frequently classified as MAC in the PTCY cohort (55.8% vs 38.9%; P < .001). There was less use of methotrexate (1.4% vs 53.1%) and calcineurin inhibitors (80.9% vs 98%) and more use of MMF (59.3% vs 41.3%) in the PTCY group than in the ATG group (P < .001; Table 1).
Table 1.
Patient characteristics
| Variables | Total |
PTCY |
ATG |
P value |
|---|---|---|---|---|
| N (%) | n (%) | n (%) | ||
| Patient number | 960 (100) | 209 (21.8) | 751 (78.2) | |
| Median age at transplant (IQR), y | 59.3 (49.2-65) | 57.1 (46.5-63.9) | 60.1 (50.6-65.2) | .006 |
| Sex at birth | ||||
| Male | 603 (62.8) | 122 (58.4) | 481 (64.0) | .16 |
| Female | 357 (37.2) | 87 (41.6) | 270 (36.0) | |
| Patient CMV serology | ||||
| Positive | 673 (71.1) | 160 (77.7) | 513 (69.2) | .023 |
| Negative | 274 (28.9) | 46 (22.3) | 228 (30.8) | |
| Missing | 13 | 3 | 10 | |
| Disease at diagnosis | ||||
| RA/RARS/del5q | 69 (7.4) | 16 (7.7) | 53 (7.3) | .54 |
| RCMD/RCMD-RS/MDS-U | 292 (31.2) | 58 (28.0) | 234 (32.1) | |
| MDS-EB | 576 (61.5) | 133 (64.3) | 443 (60.7) | |
| Missing | 23 | 2 | 21 | |
| IPSS-R at diagnosis | ||||
| Very low | 35 (6.6) | 6 (4.4) | 29 (7.3) | .24 |
| Low | 86 (16.1) | 16 (11.8) | 70 (17.6) | |
| Intermediate | 146 (27.4) | 36 (26.5) | 110 (27.7) | |
| High | 157 (29.5) | 46 (33.8) | 111 (28.0) | |
| Very high | 109 (20.5) | 32 (23.5) | 77 (19.4) | |
| Missing | 427 | 73 | 354 | |
| Cytogenetics | ||||
| Normal | 396 (45.6) | 86 (46.0) | 310 (45.5) | .98 |
| Abnormal | 472 (54.4) | 101 (54.0) | 371 (54.5) | |
| Missing | 92 | 22 | 70 | |
| IPSS-R cytogenetics | ||||
| Good | 448 (53.6) | 99 (55.0) | 349 (53.2) | .95 |
| Intermediate | 141 (16.9) | 28 (15.6) | 113 (17.2) | |
| Poor | 124 (14.8) | 27 (15.0) | 97 (14.8) | |
| Very poor | 123 (14.7) | 26 (14.4) | 97 (14.8) | |
| Missing | 124 | 29 | 95 | |
| Treatment before HSCT | ||||
| Untreated | 232 (24.4) | 47 (22.6) | 185 (24.9) | .55 |
| Treated | 718 (75.6) | 161 (77.4) | 557 (75.1) | |
| Missing | 10 | 1 | 9 | |
| HMA before HSCT | ||||
| Yes | 411 (45.3) | 111 (56.1) | 300 (42.3) | .001 |
| No | 496 (54.7) | 87 (43.9) | 409 (57.7) | |
| Missing | 53 | 11 | 42 | |
| Disease at HSCT | ||||
| MDS without EB | 232 (24.7) | 50 (24.3) | 182 (24.8) | .56 |
| MDS with EB | 503 (53.5) | 116 (56.3) | 387 (52.7) | |
| MDS-AML | 206 (21.9) | 40 (19.4) | 166 (22.6) | |
| Missing | 19 | 3 | 16 | |
| Donor type | ||||
| MUD (10/10) | 672 (70) | 112 (53.6) | 560 (74.6) | <.001 |
| MMUD | 288 (30) | 97 (46.4) | 191 (25.4) | |
| 9/10 | 241 (83.7) | 79 (81.4) | 162 (84.8) | .72 |
| 8/10 | 45 (15.6) | 17 (17.5) | 28 (14.7) | |
| 7/10 | 2 (0.7) | 1 (1.0) | 1 (0.5) | |
| Performance status | ||||
| >80 | 661 (71.3) | 150 (72.8) | 511 (70.9) | .65 |
| ≤80 | 266 (28.7) | 56 (27.2) | 210 (29.1) | |
| Missing | 33 | 3 | 30 | |
| HCT-CI | ||||
| Low | 422 (45.7) | 89 (43.4) | 333 (46.4) | .31 |
| Intermediate | 234 (25.4) | 48 (23.4) | 186 (25.9) | |
| High | 267 (28.9) | 68 (33.2) | 199 (27.7) | |
| Missing | 37 | 4 | 33 | |
| Conditioning regimen | ||||
| MAC | 408 (42.5) | 116 (55.8) | 292 (38.9) | <.001 |
| RIC | 551 (57.5) | 92 (44.2) | 459 (61.1) | |
| Missing | 1 | 1 | ||
| Stem cell source | ||||
| BM | 59 (6.1) | 12 (5.7) | 47 (6.3) | .91 |
| PB | 901 (93.9) | 197 (94.3) | 704 (93.7) | |
| GVHD prophylaxis | ||||
| Calcineurin inhibitors | 905 (94.3) | 169 (80.9) | 736 (98.0) | <.001 |
| MMF | 434 (45.2) | 124 (59.3) | 310 (41.3) | <.001 |
| Methotrexate | 402 (41.9) | 3 (1.4) | 399 (53.1) | <.001 |
BM, bone marrow; CMV, cytomegalovirus; MDS-AML, myelodysplastic syndrome transformed to AML; MDS-U, myelodysplastic syndrome unclassifiable; PB, peripheral blood; R, refractory anemia; RARS, refractory anemia with ring sideroblasts; RCMD, refractory cytopenia with multilineage dysplasia; RCMD-RS, refractory cytopenia with multilineage dysplasia and with ring sideroblasts.
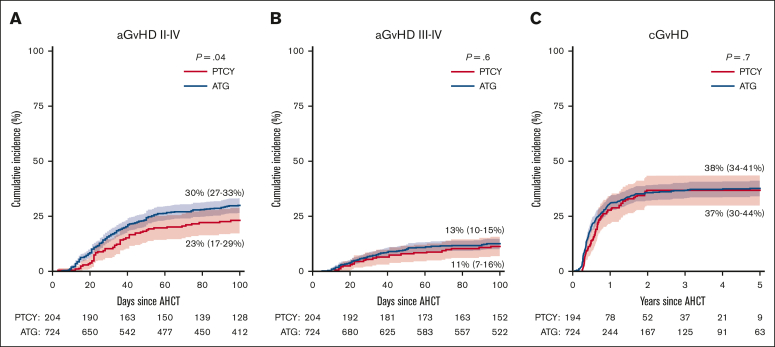
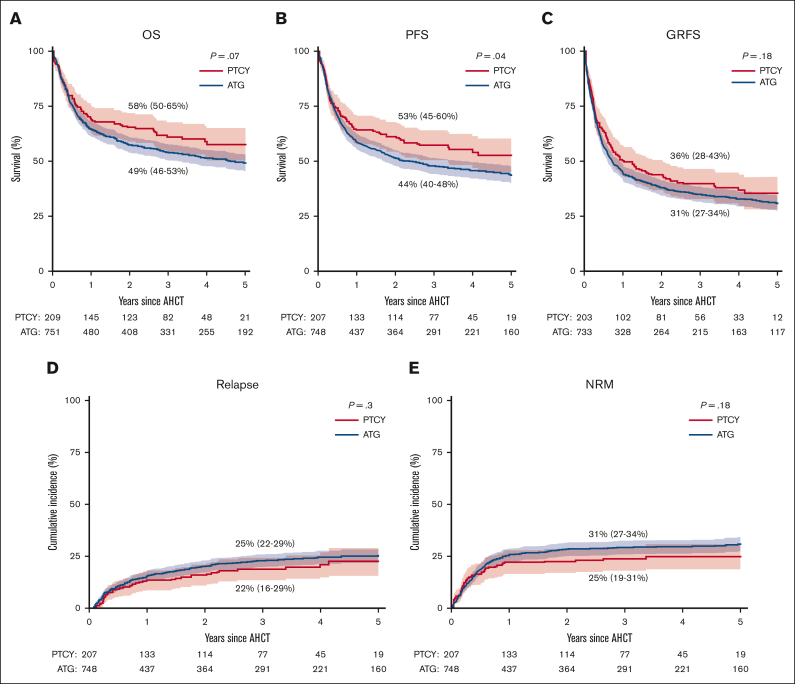
Outcomes
The cumulative incidence of neutrophil engraftment at 28 days was significantly better with ATG (93% vs 85% in the PTCY group; P < .001; Table 2). The median time to neutrophil engraftment was 16 days (95% CI, 16-17) vs 20 days (95% CI, 19-21), and platelet engraftment occurred at a median of 15 days (95% CI, 14-16) vs 21 days (95% CI, 19-23) with cumulative platelet recovery at day 100, which was also significantly better with ATG (90% vs 86% for the PTCY group; P < .001; Table 2). Primary graft failure was significantly higher with use of PTCY than with ATG (6% vs 3%; P = .025). Grade 2 to 4 aGVHD incidence was lower using PTCY (23%; 95% CI, 17-29 vs 30%; 95% CI, 27-33; P = .044; Figure 1A). Grade 3 to 4 aGVHD incidence did not differ significantly between the PTCY and ATG cohorts (11%; 95% CI, 7-16 vs 13%; 95% CI, 10-15, respectively; P value = .6; Figure 1B). In parallel, there was also no difference in cGVHD incidence (37%; 95% CI, 33-44 with PTCY and 38%; 95% CI, 34-41 at 5-years; P = .7; Table 2; Figure 1C). There was a tendency toward a lower incidence of severe cGVHD with PTCY (4%; 95% CI, 1-7 vs 8%; 95% CI, 6-10; P = .08) and a tendency toward better cGVHD-free survival, which was 24% (95% CI, 17-31) vs 20% (95% CI, 17-23; P = .07) for PTCY and ATG, respectively (Table 2). After a median follow-up of 4.4 years (95% CI, 4.2-4.8), a total of 445 patients died. Causes of death did not differ between the 2 cohorts; 37.8% and 38.3% died from relapse or progression of the primary disease in the PTCY and ATG cohorts, respectively. The 5-year OS was 58% (95% CI, 50-65) with PTCY and 49% (95% CI, 46-53) in the ATG group (P = .07; Table 2; Figure 2A). The 5-year PFS was better with PTCY at 53% (95% CI, 45-60) vs 44% (95% CI, 40-48) with ATG (P = .043; Table 2; Figure 2B). The 5-year GRFS was 36% (95% CI, 28-43) with PTCY vs 31% (95% CI, 27-34) with ATG (P = .18; Table 2; Figure 2C). The 5-year cumulative incidence of relapse was similar in the 2 cohorts (22%; 95% CI, 16-29 in PTCY vs 25%; 95% CI, 22-29 in ATG; P = .3; Table 2; Figure 2D). The 5-year NRM was 25% (95% CI, 19-31) vs 31% (95% CI, 27-34) in PTCY and ATG, respectively (P = .18; Table 2; Figure 2E).
Table 2.
Outcome of myelodysplastic neoplasms with unrelated donor transplants: PTCY vs ATG (univariable)
| Variables | Total | PTCY | ATG | P value |
|---|---|---|---|---|
| Patient number | 960 | 209 | 751 | |
| D28 neutrophil engraftment (95% CI) | 91% (89-93) | 85% (80-89) | 93% (91-94) | <.001 |
| D100 platelet engraftment (95% CI) | 89% (87-91) | 86% (82-91) | 90% (88-92) | <.001 |
| D100 primary graft failure | 3% (2-5) | 6% (3-9) | 3% (2-4) | .025 |
| 5-y OS | 51% (48-54) | 58% (50-65) | 49% (46-53) | .07 |
| 5-y PFS | 46% (42-49) | 53% (45-60) | 44% (40-48) | .043 |
| 5-y relapse/progression | 25% (22-28) | 22% (16-29) | 25% (22-29) | .3 |
| 5-y NRM | 30% (27-33) | 25% (19-31) | 31% (27-34) | .18 |
| D100 aGVHD (95% CI) | ||||
| aGVHD grade 2-4 | 28% (26-31) | 23% (17-29) | 30% (27-33) | .044 |
| aGVHD grade 3-4 | 12% (10-14) | 11% (7-16) | 13% (10-15) | .6 |
| 5-y cGVHD (95% CI) | ||||
| All | 38% (34-41) | 37% (30-44) | 38% (34-41) | .7 |
| Mild | 12% (10-15) | 16% (10-21) | 12% (9-14) | .15 |
| Moderate | 10% (8-12) | 12% (7-17) | 10% (7-12) | .4 |
| Severe | 7% (6-9) | 4% (1-7) | 8% (6-10) | .08 |
| 5-y cGVHD-free survival | 21% (18-23) | 24% (17-31) | 20% (17-23) | .07 |
| 5-y GRFS (95% CI) | 32% (29-35) | 36% (28-43) | 31% (27-34) | .18 |
Figure 1.
Incidence of GVHD. (A) Cumulative incidence at day 100 of aGVHD grade 2 to 4. (B) Cumulative incidence at day 100 of aGVHD grade 3 to 4. (C) Cumulative incidence of cGVHD at 5 years among patients with MDS who received PTCY or ATG as GVHD prophylaxis for UD allo-HSCT. Numbers below the graph show the number of patients at risk.
Figure 2.
Outcomes of patients with MDS transplanted with PTCY vs ATG. (A) OS, (B) PFS, (C) GRFS, (D) RI, and (E) NRM of patients with MDS who received PTCY or ATG as GVHD prophylaxis for UD allo-HSCT and stratified by donor type (MUD vs MMUD). Numbers below the graph show the number of patients at risk.
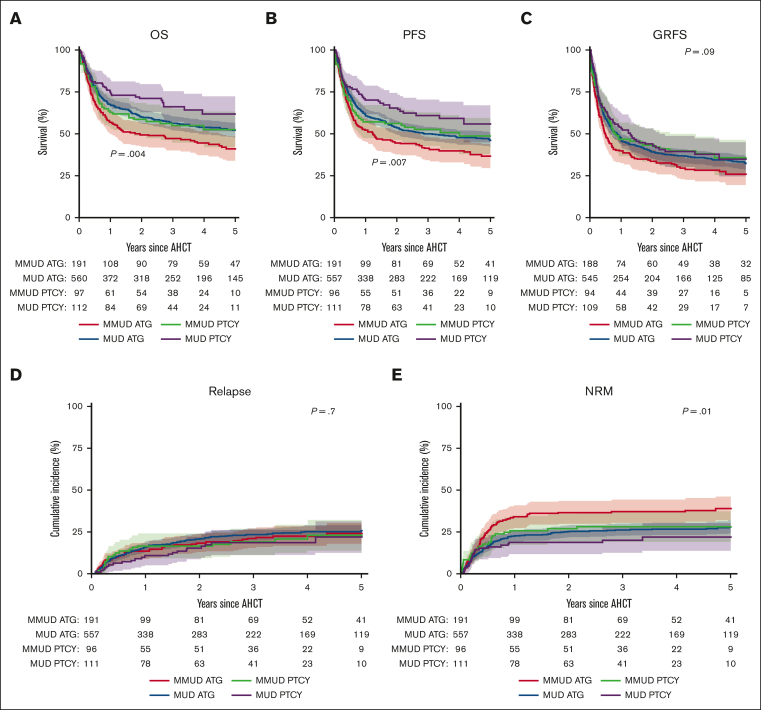
When comparing MUD with MMUD transplants, the 5-year OS was better for the MUD cohort than for the MMUD cohort (54%; 95% CI, 50-58 vs 44%; 95% CI, 38-51; P = .005; Table 3). It was remarkable to observe that in the MUD setting, PTCY achieved the best OS and MUD-ATG and MMUD-PTCY had similar outcomes, whereas MMUD-ATG had the worse outcome (Figure 3A). Similar findings were observed in terms of the 5-year PFS, which was 48% (95% CI, 44-52) for MUD and 40% (95% CI, 34-46) for MMUD (P = .016; Table 3; Figure 3B). There was a nonsignificant tendency for better GRFS with MUD of 33% (95% CI, 29-37) vs 29% (95% CI, 23-35) for MMUD (P = .1; Table 3; Figure 3C). The worse OS and PFS for MMUD was related to an increase in NRM in the MMUD group, which was 36% (95% CI, 30-41) vs 27% (95% CI, 24-31) with MUD transplants (P = .005; Table 3; Figure 3E). The RI was similar in both cohorts (25%; 95% CI, 21-28 with MUD vs 24%; 95% CI, 19-29 with MMUD; P = .7; Table 3; Figure 3D).
Table 3.
Outcome of myelodysplastic neoplasms with unrelated donor transplants by donor type (univariable)
| Variables | MUD | MMUD | P value |
|---|---|---|---|
| Patient number | 672 | 288 | |
| 5-y OS (95% CI) | 54% (50-58) | 44% (38-51) | .005 |
| 5-y PFS (95% CI) | 48% (44-52) | 40% (34-46) | .016 |
| 5-y relapse/progression (95% CI) | 25% (21-28) | 24% (19-29) | .7 |
| 5-y NRM (95% CI) | 27% (24-31) | 36% (30-41) | .005 |
| D100 aGVHD (95% CI) | |||
| aGVHD grade 2-4 | 27% (24-31) | 31% (26-36) | .3 |
| aGVHD grade 3-4 | 11% (9-13) | 15% (11-19) | .09 |
| 5-y cGVHD (95% CI) | |||
| All | 39% (36-43) | 33% (27-39) | .07 |
| Mild | 14% (11-16) | 10% (6-14) | .14 |
| Moderate | 12% (9-14) | 7% (4-10) | .0034 |
| Severe | 8% (6-10) | 6% (15-25) | .4 |
| 5-y cGVHD-free survival (95% CI) | 21% (18-24) | 20% (15-25) | .6 |
| 5-y GRFS (95% CI) | 33% (29-37) | 29% (23-35) | .1 |
Figure 3.
Outcomes of patients with MDS transplanted with PTCY vs ATG. (A) OS was 60% (95% CI, 52-72) for patients who underwent a MUD transplant and received PTCY, 53% (95% CI, 42-63) for patients who underwent a MMUD transplant and received PTCY, 52% (95% CI, 48-57) for patients who underwent a MUD transplant and received ATG, and 41% (95% CI, 34-49) for patients who underwent a MMUD transplant and received ATG (P = .004). (B) PFS was 56% (95% CI, 45-67) for patients who underwent a MUD transplant and received PTCY, 49% (95% CI, 38-60) for patients who underwent a MMUD transplant and received PTCY, 46% (95% CI, 42-51) for patients who underwent a MUD transplant and received ATG, and 37% (95% CI, 30-44) for patients who underwent a MMUD transplant and received ATG (P = .007). (C) GRFS was 35% (95% CI, 25-45) for patients who underwent a MUD transplant and received PTCY, 36% (95% CI, 25-46) for patients who underwent a MMUD transplant and received PTCY, 32% (95% CI, 28-37) for patients who underwent a MRD transplant and received ATG, and 26% (95% CI, 19-33) for patients who underwent a MMUD transplant and received ATG (P = .09). (D) RI was 22% (95% CI, 12-31) for patients who underwent a MUD transplant and received PTCY, 23% (95% CI, 14-32) for patients who underwent a MMUD transplant and received PTCY, 26% (95% CI, 22-29) for patients who underwent a MUD transplant and received ATG, and 24% (95% CI, 18-31) for patients who underwent a MMUD transplant and received ATG (P = .7). (E) NRM was 22% (95% CI, 14-30) for patients who underwent a MUD transplant and received PTCY, 28% (95% CI, 19-37) for patients who underwent a MMUD transplant and received PTCY, 28% (95% CI, 24-32) for patients who underwent a MUD transplant and received ATG, and 39% (95% CI, 32-46) for patients who underwent a MMUD transplant and received ATG (P = .009) when stratified by donor type (MUD vs MMUD). Numbers below the graph show the number of patients at risk.
We also looked at the outcome in terms of different ATG treatments given, specifically either Thymoglobulin or Grafalon, with no differences in term of OS, PFS, GRFS, aGVHD, or cGVHD except for more aGVHD grade 3 to 4 in the Thymoglobulin group with an incidence of 15% (95% CI, 11-19) vs 9% (95% CI, 5-12) in the Grafalon group (P = .027; supplemental Figures 2 and 3).
There were also some differences in outcome based on the year of transplant with better OS (P = .04), PFS (P = .003), and lower aGVHD grade 2 to 4 (P = .03) after 2016 but no differences in terms of RI (P = .13), NRM (P = .07), GRFS (P = .08), aGVHD grade 3 to 4 (P = .7), or cGVHD (P = .3; supplemental Figures 4 and 5).
A relationship between transplant volume and outcome was observed. Patients who received a transplant in centers with larger numbers of patients in this cohort were less likely to have an adverse event. There was an improved OS (hazard ratio [HR] per 10 patient increase, 0.85; 95% CI, 0.77-0.95; P = .005) and PFS (HR, 0.87; 95% CI, 0.78-0.96; P = .008) related to a lower NRM (HR, 0.81; 95% CI, 0.7-0.94; P = .005; supplemental Table 1).
In the univariable analysis, patients who underwent a transplant with a MAC regimen had an improved OS and PFS when compared with those who had a RIC regimen (P = .036 and P = .015, respectively; supplemental Figure 6).
Risk factors
The multivariable analyses were adjusted for all variables prognostic for at least 1 outcome (OS, PFS, GRFS, NRM, RI, aGVHD, and cGVHD). Those variable were MDS classification, IPSS-R cytogenetics, donor/recipient HLA mismatch, recipient age, HMA given before allo-HSCT, HCT-CI risk, and center effect, and it revealed significantly better OS for PTCY with an HR for ATG of 1.32 (95% CI, 1.0-1.74, P = .05) and a superior PFS for PTCY with an HR for ATG of 1.33 (95% CI, 1.03-1.73; P = .03; Table 4). The full Cox model is available in supplemental Table 2. There was no apparent interaction between GVHD prophylaxis (PTCY or ATG) and IPSS-R or HLA matching, suggesting that the effects of ATG and PTCY were not dependent on these risk factors. Namely, the benefit of PTCY for OS and PFS is true in both the MUD and MMUD settings. There was also a tendency of improved GRFS, NRM, and relapse, which was not statistically significant, for patients who received PTCY as GVHD prophylaxis (Table 4). The risk for acute grade 2 to 4 GVHD was significantly increased among patients who received ATG when compared with those who received PTCY (HR, 1.61; 95% CI, 1.12-2.33; P = .01), whereas there was no difference in the incidence of cGVHD. The risk for acute grade 3 to 4 GVHD was similar in the 2 groups (data not shown). The other factors that impacted OS were the degree of HLA matching with an HR of 1.48 (95% CI, 1.19-1.82) for MMUD (P < .001), the IPSS-R cytogenetic risk profile with the very poor risk group having an HR of 2.37 (95% CI, 1.73-2.96; P<.001), the age at transplant with an HR of 1.15 (95% CI, 1.05-1.27) for older age (P = .003), and the HCT-CI with an HR for high risk (≥3) of 1.26 (95% CI, 1-1.59; P = .05; supplemental Table 2). In contrast, neither pretransplant HMA use nor the presence of EBs at diagnosis negatively impacted OS (supplemental Table 2). Regarding PFS, a similar signal as for OS was found (supplemental Table 2). The variables that significantly impacted GRFS were an IPSS-R cytogenetics risk of intermediate with an HR of 1.32 (95% CI, 1.03-1.68; P = .03), a risk of very poor with an HR of 1.85 (95% CI, 1.45-2.36; P < .001), an HCT-CI high-risk score with an HR of 1.32 (95% CI 1.09-1.61; P = .006), and a MMUD with an HR of 1.27 (95% CI, 1.05-1.53; P = .01; supplemental Table 2). Grade 2 to 4 acute GVHD was only influenced by the use of PTCY when compared with ATG with an HR of 1.58 (95% CI, 1.12-2.24; P = .01). Of note, the better outcome found in univariable analysis for OS and PFS in favor of MAC was not confirmed in the multivariable analysis (P = .3 and P = .2, respectively).
Table 4.
PTCY vs ATG in adjusted Cox models for PFS, GRFS, NRM, relapse, and grade 2 to 4 GVHD
| Outcome | No. | Events | HR (95% CI) | P value |
|---|---|---|---|---|
| OS | ||||
| PTCY | 166 | 65 | ||
| ATG | 597 | 301 | 1.32 (1-1.74) | .05 |
| PFS | ||||
| PTCY | 165 | 75 | ||
| ATG | 595 | 328 | 1.33 (1.03-1.73) | .03 |
| GRFS | ||||
| PTCY | 162 | 102 | ||
| ATG | 580 | 392 | 1.24 (0.99-1.56) | .06 |
| NRM | ||||
| PTCY | 165 | 40 | ||
| ATG | 595 | 184 | 1.39 (0.97-2.01) | .07 |
| Relapse/progression | ||||
| PTCY | 165 | 35 | ||
| ATG | 595 | 144 | 1.29 (0.88-1.88) | .2 |
| aGVHD grade 2-4 | ||||
| PTCY | 164 | 41 | ||
| ATG | 575 | 197 | 1.61 (1.12-2.33) | .01 |
| cGVHD | ||||
| PTCY | 155 | 56 | ||
| ATG | 578 | 224 | 1.06 (0.77-1.47) | .7 |
Effect estimates are given with 95% CI and corresponding P values were calculated using the Wald test.
Discussion
This retrospective registry study describes the outcome of patients with MDS who underwent allo-HSCT with MUD or MMUD between 2012 and 2019 and who received either PTCY or ATG as GVHD prophylaxis. This study is, to our knowledge, the first to focus on MDS allo-HSCT in the UD setting and to compare outcomes following GVHD prophylaxis with either ATG or PTCY. Leveraging the large EBMT network, we were able to show that the risks for acute grade 2 to 4 GVHD, PFS, and OS were decreased by PTCY when compared with ATG. However, because the structure of the registry was not aimed to prospectively collect details on ATG administration and the heterogeneity in ATG delivery and dosing, there is clearly a need for randomized prospective trials to confirm our results in this setting. Indeed, the brand and ATG dosing may also influence the results as already reported.28 However, we failed to find any difference between Thymoglobulin and Grafalon in terms of OS, disease-free survival (DFS), NRM, or GRFS. Currently, results from prospective trials that compared PTCY with ATG remain scarce. Brissot et al have reported the results of a prospective phase 2 trial that compared PTCY with ATG and showed similar outcomes for all end points.29 In addition, several registry studies are available and summarized in supplemental Table 3.17,18,21,30, 31, 32, 33, 34, 35, 36 Most large available studies included patients with acute leukemia in the setting of an unrelated donor. Regarding aGVHD, PTCY is regularly reported to decrease the risk for grade 2 to 4 or grade 3 to 4 (supplemental Table 3). Studies that included only allo-HSCT that used an MMUD have reported a systematical decreased risk for aGVHD,30,31,35 suggesting a strong protective effect of PTCY against aGVHD in the setting of a MMUD. However, it has also been reported that PCTY decreased the aGVHD risk in the setting of MUD, even if results are more conflicting (supplemental Table 3).34 Regarding cGVHD, PTCY has been reported to decrease the risk or have a minor impact, as is the case in our present study (supplemental Table 3).
Engraftment and neutrophil and platelet recovery were worse when using PTCY in our study. Of note, this delay occurred despite the vast majority of allo-HSCTs being performed with peripheral blood stem cell (PBSC) as the stem cell source (93.9%). This is in concordance with most of the studies in this setting for which there was information on engraftment that showed either a lower or delayed neutrophil and platelet engraftment with the exception of 1 report with a small number of patients in which there was no difference in the time to neutrophil and platelet engraftment.21,31,33,34,37 Altogether, it seems that PTCY negatively impacts the time to engraftment and graft failure, although this does not seem to convert to a higher risk for mortality, possibly compensated by a lower incidence of GVHD.
In this study, PTCY was predictive for better OS and PFS, whereas the NRM and relapse risks were not significantly impacted by GVHD prophylaxis type. The survival advantage of PTCY has also been reported by other groups (supplemental Table 3). One hypothesis is that the mortality related to GVHD and infections is reduced and that was confirmed in an MDACC registry study.34 Unfortunately, we lack this information in the registry and could not check if the overall infection rate was decreased with the use of PTCY when compared with ATG. Nonetheless, in this study, causes of mortality were superimposable in the PTCY or ATG cohorts. The advantage of survival was seen in the MUD and in the MMUD setting, confirming the effect of PTCY in both groups of patients.
Limitations of this study are those inherent to a registry-based design, which may confer some bias. This study cannot replace a randomized trial, especially because there was big heterogeneity in terms of GVHD prophylaxis, conditioning regimen, and the reason why PCTY or ATG was chosen, which was unknown.
In contrast, a strength was that this study included a substantial number of patients with a high number of centers (92), and the heterogeneity of the procedures reflect real life and may emphasize the findings.
In summary, the results of this study suggest that for patients with MDS who proceed with UD allo-HSCT, PTCY is a valid GVHD prophylaxis option that may improve PFS and OS and decrease the rates of grade 2 to 4 aGVHD at the expense of delayed engraftment and an increased graft failure rate. These results applied to both MUD and to MMUD, but MUD donors are still associated with a better outcome than MMUD donors. Moreover, this strategy is cost-effective and may reduce the costs of UD allo-HSCT, particularly in countries in which ATG is more difficult to obtain. Further cooperative and prospective randomized studies would be essential to confirm these results.
Conflict-of-interest disclosure: Y.C reports receiving consulting fees for serving on the advisory board from Merck Sharp & Dohne, Novartis, Incyte, Bristol Myers Squibb (BMS), Pfizer, AbbVie, Roche, Jazz, Gilead, Amgen, AstraZeneca, Servier, and Pierre Fabre; and travel support from MSD, Roche, Gilead, Amgen, Incyte, AbbVie, Janssen, AstraZeneca, Jazz, Sanofi, and Pierre Fabre all via the institution. I.Y.-A. reports receiving honoraria from BMS, Novartis, Kite, and Miltenyi Biomedecine. M. Robin reports receiving research support from AbbVie, Astex, Novartis, Neovii, and Medac. The remaining authors declare no competing financial interests.
Acknowledgments
The authors thank all the centers that reported data to the European Society for Blood and Marrow Transplantation contributing to this study, all those who have worked on the data registry, the health team that cared for the patients, and all of the patients.
Authorship
Contribution: Y.C. and M. Robin designed the study; Y.C., I.M., F.C., L.K., J.V., J.P., M. Rovira, T.O., T.G.-D., N.K., V.P., I.Y.-A., A.R., M.I.-R., A.T., F.O., C.G., C.S., J.D.-S., K.R., D.P.M., and M. Robin contributed data and reviewed the manuscript; Y.C., D.-J.E., and M. Robin analyzed the data; and Y.C., D.-J.E., D.P.M., and M. Robin wrote the manuscript.
Footnotes
D.P.M. and M. Robin are joint senior authors.
According to the European Society for Blood and Marrow Transplantation Policy, data cannot be shared but are available upon reasonable request from the Chronic Malignancies Working Party (cmwp@ebmt.org).
The full-text version of this article contains a data supplement.
Contributor Information
Yves Chalandon, Email: yves.chalandon@hcuge.ch.
Marie Robin, Email: marie.robin@aphp.fr.
Supplementary Material
References
- 1.Khoury JD, Solary E, Abla O, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36(7):1703–1719. doi: 10.1038/s41375-022-01613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia-Manero G. Myelodysplastic syndromes: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98(8):1307–1325. doi: 10.1002/ajh.26984. [DOI] [PubMed] [Google Scholar]
- 3.de Witte T, Bowen D, Robin M, et al. Allogeneic hematopoietic stem cell transplantation for MDS and CMML: recommendations from an international expert panel. Blood. 2017;129(13):1753–1762. doi: 10.1182/blood-2016-06-724500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeFilipp Z, Ciurea SO, Cutler C, et al. Hematopoietic cell transplantation in the management of myelodysplastic syndrome: an evidence-based review from the American Society for Transplantation and Cellular Therapy Committee on practice guidelines. Transplant Cell Ther. 2023;29(2):71–81. doi: 10.1016/j.jtct.2022.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Kröger N, Iacobelli S, Franke G-N, et al. Dose-reduced versus standard conditioning followed by allogeneic stem-cell transplantation for patients with myelodysplastic syndrome: a prospective randomized phase III study of the EBMT (RICMAC trial) J Clin Oncol. 2017;35(19):2157–2164. doi: 10.1200/JCO.2016.70.7349. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura R, Saber W, Martens MJ, et al. Biologic assignment trial of reduced-intensity hematopoietic cell transplantation based on donor availability in patients 50-75 years of age with advanced myelodysplastic syndrome. J Clin Oncol. 2021;39(30):3328–3339. doi: 10.1200/JCO.20.03380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kröger N, Sockel K, Wolschke C, et al. Comparison between 5-azacytidine treatment and allogeneic stem-cell transplantation in elderly patients with advanced MDS according to donor availability (VidazaAllo Study) J Clin Oncol. 2021;39(30):3318–3327. doi: 10.1200/JCO.20.02724. [DOI] [PubMed] [Google Scholar]
- 8.Walker I, Panzarella T, Couban S, et al. Pretreatment with anti-thymocyte globulin versus no anti-thymocyte globulin in patients with haematological malignancies undergoing haemopoietic cell transplantation from unrelated donors: a randomised, controlled, open-label, phase 3, multicentre trial. Lancet Oncol. 2016;17(2):164–173. doi: 10.1016/S1470-2045(15)00462-3. [DOI] [PubMed] [Google Scholar]
- 9.Kröger N, Solano C, Wolschke C, et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med. 2016;374(1):43–53. doi: 10.1056/NEJMoa1506002. [DOI] [PubMed] [Google Scholar]
- 10.Finke J, Bethge WA, Schmoor C, et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 2009;10(9):855–864. doi: 10.1016/S1470-2045(09)70225-6. [DOI] [PubMed] [Google Scholar]
- 11.Bolaños-Meade J, Hamadani M, Wu J, et al. Post-transplantation cyclophosphamide-based graft-versus-host disease prophylaxis. N Engl J Med. 2023;388(25):2338–2348. doi: 10.1056/NEJMoa2215943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolaños-Meade J, Reshef R, Fraser R, et al. Prevention of graft versus host disease with hematopoietic cell transplantation with reduced intensity conditioning—a comparison of three prophylaxis regimens (tacrolimus/mycophenolate mofetil/cyclophosphamide, tacrolimus/methotrexate/bortezomib or tacrolimus/methotrexate/maraviroc) versus tacrolimus/methotrexate: a randomised phase 2 trial with a non-randomised contemporaneous control group (BMT CTN 1203) Lancet Haematol. 2019;6(3):e132–e143. doi: 10.1016/S2352-3026(18)30221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broers AEC, de Jong CN, Bakunina K, et al. Posttransplant cyclophosphamide for prevention of graft-versus-host disease: results of the prospective randomized HOVON-96 trial. Blood Adv. 2022;6(11):3378–3385. doi: 10.1182/bloodadvances.2021005847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luznik L, Pasquini MC, Logan B, et al. Randomized phase III BMT CTN trial of calcineurin inhibitor-free chronic graft-versus-host disease interventions in myeloablative hematopoietic cell transplantation for hematologic malignancies. J Clin Oncol. 2022;40(4):356–368. doi: 10.1200/JCO.21.02293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw BE, Jimenez-Jimenez AM, Burns LJ, et al. National marrow donor program-sponsored multicenter, phase II trial of HLA-mismatched unrelated donor bone marrow transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2021;39(18):1971–1982. doi: 10.1200/JCO.20.03502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaw BE, Jimenez-Jimenez AM, Burns LJ, et al. Three-year outcomes in recipients of mismatched unrelated bone marrow donor transplants using post-transplantation cyclophosphamide: follow-up from a national marrow donor program-sponsored prospective clinical trial. Transplant Cell Ther. 2023;29(3):208.e1–208.e6. doi: 10.1016/j.jtct.2022.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moiseev IS, Pirogova OV, Alyanski AL, et al. Graft-versus-host disease prophylaxis in unrelated peripheral blood stem cell transplantation with post-transplantation cyclophosphamide, tacrolimus, and mycophenolate mofetil. Biol Blood Marrow Transplant. 2016;22(6):1037–1042. doi: 10.1016/j.bbmt.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Brissot E, Labopin M, Moiseev I, et al. Post-transplant cyclophosphamide versus antithymocyte globulin in patients with acute myeloid leukemia in first complete remission undergoing allogeneic stem cell transplantation from 10/10 HLA-matched unrelated donors. J Hematol Oncol. 2020;13(1):87. doi: 10.1186/s13045-020-00923-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanz J, Galimard J-E, Labopin M, et al. Post-transplant cyclophosphamide after matched sibling, unrelated and haploidentical donor transplants in patients with acute myeloid leukemia: a comparative study of the ALWP EBMT. J Hematol Oncol. 2020;13(1):46. doi: 10.1186/s13045-020-00882-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah MV, Saliba RM, Rondon G, et al. Pilot study using post-transplant cyclophosphamide (PTCy), tacrolimus and mycophenolate GVHD prophylaxis for older patients receiving 10/10 HLA-matched unrelated donor hematopoietic stem cell transplantation. Bone Marrow Transplant. 2019;54(4):601–606. doi: 10.1038/s41409-018-0367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aydin M, de Leeuw DC, Rutten CE, et al. ATG versus PTCy in matched unrelated donor haematopoietic stem cell transplantations with non-myeloablative conditioning. Br J Haematol. 2023;203(3):439–445. doi: 10.1111/bjh.19031. [DOI] [PubMed] [Google Scholar]
- 22.Bacigalupo A, Ballen K, Rizzo D, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15(12):1628–1633. doi: 10.1016/j.bbmt.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giralt S, Ballen K, Rizzo D, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. report of a workshop convened by the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2009;15(3):367–369. doi: 10.1016/j.bbmt.2008.12.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weisdorf DJ, Hurd D, Carter S, et al. Prospective grading of graft-versus-host disease after unrelated donor marrow transplantation: a grading algorithm versus blinded expert panel review. Biol Blood Marrow Transplant. 2003;9(8):512–518. doi: 10.1016/s1083-8791(03)00162-9. [DOI] [PubMed] [Google Scholar]
- 25.Harris AC, Young R, Devine S, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: a report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22(1):4–10. doi: 10.1016/j.bbmt.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee SJ, Wolff D, Kitko C, et al. Measuring therapeutic response in chronic graft-versus-host disease. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: IV. The 2014 Response Criteria Working Group report. Biol Blood Marrow Transplant. 2015;21(6):984–999. doi: 10.1016/j.bbmt.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iacobelli S, EBMT Statistical Committee Suggestions on the use of statistical methodologies in studies of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2013;48(suppl 1):S1–S37. doi: 10.1038/bmt.2012.282. [DOI] [PubMed] [Google Scholar]
- 28.Teramoto M, Takahashi T, Matsumoto K, et al. Individualized rabbit anti-thymocyte globulin dosing in adult haploidentical hematopoietic cell transplantation with high-risk hematologic malignancy: exposure-response analysis and population pharmacokinetics simulations. Am J Hematol. 2024;99(3):387–395. doi: 10.1002/ajh.27195. [DOI] [PubMed] [Google Scholar]
- 29.Brissot E, Labopin M, Labussière H, et al. Post-transplant cyclophosphamide versus anti-thymocyte globulin after reduced intensity peripheral blood allogeneic cell transplantation in recipients of matched sibling or 10/10 HLA matched unrelated donors: final analysis of a randomized, open-label, multicenter, phase 2 trial. Blood Cancer J. 2024;14(1):31. doi: 10.1038/s41408-024-00990-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Battipaglia G, Labopin M, Kröger N, et al. Posttransplant cyclophosphamide vs antithymocyte globulin in HLA-mismatched unrelated donor transplantation. Blood. 2019;134(11):892–899. doi: 10.1182/blood.2019000487. [DOI] [PubMed] [Google Scholar]
- 31.Modi D, Kondrat K, Kim S, et al. Post-transplant cyclophosphamide versus thymoglobulin in HLA-mismatched unrelated donor transplant for acute myelogenous leukemia and myelodysplastic syndrome. Transplant Cell Ther. 2021;27(9):760–767. doi: 10.1016/j.jtct.2021.06.018. [DOI] [PubMed] [Google Scholar]
- 32.Battipaglia G, Labopin M, Hamladji R-M, et al. Post-transplantation cyclophosphamide versus antithymocyte globulin in patients with acute myeloid leukemia undergoing allogeneic stem cell transplantation from HLA-identical sibling donors: a retrospective analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Cancer. 2021;127(2):209–218. doi: 10.1002/cncr.33255. [DOI] [PubMed] [Google Scholar]
- 33.Bailén R, Kwon M, Pascual-Cascón MJ, et al. Post-transplant cyclophosphamide for GVHD prophylaxis compared to ATG-based prophylaxis in unrelated donor transplantation. Ann Hematol. 2021;100(2):541–553. doi: 10.1007/s00277-020-04317-7. [DOI] [PubMed] [Google Scholar]
- 34.Mehta RS, Saliba RM, Rondon G, et al. Post-transplantation cyclophosphamide versus tacrolimus and methotrexate graft-versus-host disease prophylaxis for HLA-matched donor transplantation. Transplant Cell Ther. 2022;28(10):695.e1–695.e10. doi: 10.1016/j.jtct.2022.07.021. [DOI] [PubMed] [Google Scholar]
- 35.Jimenez JA, Komanduri K, Brown S, et al. Improved GRFS after posttransplant cyclophosphamide-based vs ATG-based HLA-mismatched unrelated donor transplant. Blood Adv. 2022;6(15):4491–4500. doi: 10.1182/bloodadvances.2022007596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giebel S, Labopin M, Salmenniemi U, et al. Posttransplant cyclophosphamide versus antithymocyte globulin in patients with acute lymphoblastic leukemia treated with allogeneic hematopoietic cell transplantation from matched unrelated donors: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Cancer. 2023;129(23):3735–3745. doi: 10.1002/cncr.35004. [DOI] [PubMed] [Google Scholar]
- 37.Lee M-W, Yeon SH, Seo W-H, et al. A comparison of post-transplantation cyclophosphamide versus antithymocyte-globulin in patients with hematological malignancies undergoing HLA-matched unrelated donor transplantation. Medicine (Baltim) 2020;99(34) doi: 10.1097/MD.0000000000021571. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.