Abstract
Background
Kinesiophobia is common in patients after total knee arthroplasty and is an important risk factor for post-operative recovery outcomes. Little is known about the complex intercorrelations between different components of pain catastrophizing, self-efficacy, and kinesiophobia. This study aimed to identify the central components of kinesiophobia and to explore the interconnectedness between components of pain catastrophizing, self-efficacy, and kinesiophobia.
Methods
A total of 216 patients after total knee arthroplasty were recruited in this study. Pain Catastrophizing Scale, Self-efficacy of Rehabilitation Outcome Scale and Tampa Scale for Kinesiophobia were used to assess pain catastrophizing, self-efficacy and kinesiophobia. R software was used to visualize the networks and analyze the centrality of the networks. The index “strength” and “bridge expected influence” were employed to identify the central components and the bridge components of the networks.
Results
In the item network of kinesiophobia, three items (“Simply being careful that I do not make any unnecessary movements is the safest thing I can do to prevent my pain from worsening”, “My accident has put my body at risk for the rest of my life”, and “My body is telling me I have something dangerously wrong”) had the highest strength centrality. In the pain catastrophizing/self-efficacy–kinesiophobia network, rumination had the highest positive bridge expected influence, while coping self-efficacy had the highest negative value.
Conclusion
The three central components of kinesiophobia identified in this study, as well as two bridge variables (rumination and coping self-efficacy), could be promising and effective targets for prevention and intervention of kinesiophobia.
Keywords: pain catastrophizing, self-efficacy, kinesiophobia, total knee arthroplasty, network analysis
Introduction
Knee osteoarthritis (KOA) is the most common osteoarticular disorder and a leading cause of disability worldwide.1 Meanwhile, total knee arthroplasty (TKA) is considered the most optimal and effective surgical treatment option for patients with end-stage KOA, providing more pain relief and functional improvement.2,3 In China, almost 400,000 TKA are conducted each year, and the number is expected to continue to increase.4 Functional exercise is an essential step toward regaining more normal joint function for daily activities after TKA.5–8 Previous studies reported a medium-low level of adherence to exercise among patients after TKA.9–11 Poor adherence to rehabilitation exercise in patients after TKA has been associated with complications such as increased pain, muscle weakness, and functional disability.12,13
Kinesiophobia, also known as fear of movement, is characterized as an excessive, irrational, and debilitating fear of activity resulting from a feeling of vulnerability to painful injury or reinjury.14 Kinesiophobia may lead to patients’ psychological fear of physical activity and exercise, thereby avoiding physical activity and exercise behaviors, resulting in reduced physical function and disuse syndrome, thus creating a vicious circle of physical inactivity and disability.15 Kinesiophobia is common in patients after TKA. A recent study reported the prevalence of kinesiophobia assessed by the Tampa Scale for Kinesiophobia (TSK) was 38.4% in patients with knee arthroplasty.16 Kinesiophobia is acknowledged as a significant obstacle for patients after TKA to adhere to functional exercise programs.17,18 Given the negative impact of kinesiophobia on functional exercise, it is vital to address kinesiophobia among patients after TKA.
A significant psychological component in understanding kinesiophobia, pain catastrophizing is described as excessive focus on pain symptoms (rumination), exaggerated rating of the threat value of pain (magnification), and awareness to be unable to control the pain (helplessness).19,20 According to catastrophizing thoughts and fear of movement model, catastrophizing in a pain context, patients tend to avoid and escape from pain-inducing activities due to their excessive focus on pain, thus leading to fear of movement.14,21,22 Earlier evidence has indicated that pain catastrophizing are significantly related to kinesiophobia.16,23 Another candidate target to address kinesiophobia is self-efficacy. Self-efficacy for rehabilitation exercise can be defined as the individual’s ability to self-manage when faced with exercise tasks.24 Low self-efficacy would increase patients’ perceived difficulty of rehabilitation exercise, enhance their fear and lead to avoid behaviors.25 Earlier evidence has reported that self-efficacy was closely linked to kinesiophobia.26,27 Furthermore, a self-efficacy enhancement intervention could significantly reduce fear of avoidance behaviors in older patients after TKA.
Previous studies have assessed the level of kinesiophobia in patients after TKA via sum scores of the instruments and a rate based on cut-off value.26 The TSK, a widely used tool to assess kinesiophobia, contains 17 items that reflect different kinesiophobia experiences and are also interrelated.28 Even if individuals with the same kinesiophobia severity may have very different kinesiophobia experiences. Understanding kinesiophobia phenomenon from a component perspective is beneficial for developing targeted interventions to reduce kinesiophobia. Furthermore, many researchers have used total scores for pain catastrophizing, self-efficacy and kinesiophobia to explore the correlations rather than dimensions/items scores, which ignores different constructs. For example, pain catastrophizing has three different constructs (rumination, magnification and helplessness).19,20 This indicates that it is necessary to analyze different constructs of pain catastrophizing, self-efficacy, and kinesiophobia, which is useful to deeper understanding the connections among them and provide references for relevant measures and interventions. However, little is known about the central components of kinesiophobia and the bridge constructs between pain catastrophizing, self-efficacy and kinesiophobia.
Network analysis is a novel method to analyze and visualize the relationship among complex psychological constructs. It is particularly useful for understanding the finger-grained connection pathway between psychological constructs.29 Network theory presents an alternative perspective to conceptualize psychological constructs, regarding psychological constructs as interactive systems, as their components interact with each other and actively participate in the construct rather than the passive indicators of the construct.30 Network analysis can also provide node centrality and bridge centrality indices to identify the central nodes and the most influential bridge connections within a network model, which may help health professionals (HCPs) develop more targeted intervention strategies.31
From network perspectives, identifying the most important component of kinesiophobia and the bridge components is helpful to construct more effective and efficient measures to reduce kinesiophobia, thereby promoting functional exercise after TKA and obtaining better patient reported outcome measures (PROMS). Thus, this study aimed to use network analysis to explore the most important components of kinesiophobia and to identify the most influential bridge constructs between pain catastrophizing, self-efficacy, and kinesiophobia.
Methods
Participants
This cross-sectional study was conducted from September 2022 to June 2023 at the orthopedics units of a tertiary hospital (with over 2000 beds) in Baoding, a city in northern China. The study flow chart is presented in Figure 1. As part of a larger study, entitled “Factors associated with exercise adherence of patients after TKA”, this study reports findings regarding kinesiophobia. Factors related to exercise adherence has been reported elsewhere.32
Figure 1.
The flow chart of research.
Potential Participants met the following criteria: 1) a definite diagnosis of osteoarthritis by an orthopedic physician; 2) underwent primary total knee arthroplasty; 3) age ≥ 18 years. We excluded participants if they had 1) cancer or other severe diseases and 2) a mental disorder that prevented them from understanding the questionnaires. This study conformed with the principles outlined in the Declaration of Helsinki. Each participant signed an informed consent form before participating in this study. After obtaining written informed consent, participants were asked to complete questionnaires under the guidance of the trained investigators at the inpatient orthopedic ward 4–6 days after TKA. The survey and the brief interview commonly took about 20 minutes to complete.
Measures
Demographic and Clinical Information
The sociodemographic characteristics: age, gender, marital status, education attainment and economic status; The clinical variables: joint pain duration and replacement site.
Kinesiophobia
Kinesiophobia was assessed by the Chinese Version of TSK.33 TSK consists of 17 items, each of which is rated on a 4-point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). A total sum is calculated after the reversion of items 4, 8, 12, and 16. The Chinese version TSK has been reported as reliable and valid in the Chinese population with orthopedics diseases.26 The Cronbach’s α was 0.84 in this study.
Pain Catastrophizing
Pain catastrophizing was evaluated with the Chinese Version of the Pain Catastrophizing Scale (PCS), a 13-item scale that Measures negative perceptions related to pain.34 The PCS comprises three dimensions: rumination, magnification, and helplessness. Each item is rated using 5–point Likert scale (0 = “not at all” to 4 = “all the time”). The PCS is a well-validated tool for assessing pain catastrophizing in individuals with orthopedic diseases.35 The Cronbach’s α was 0.90 in this study.
Self-Efficacy
Self-efficacy was measured with the Chinese Version of the Self-efficacy for Rehabilitation Outcome Scale (SER) developed by Waldrop et al.24 This scale has been translated into Chinese and widely used in the Chinese population to assess participants’ beliefs about their confidence to perform behaviors typical in physical rehabilitation for hip and knee surgery.36 This 12-item scale consists of two dimensions: rehabilitation exercise self-efficacy and coping self-efficacy. Items are scored on an 11-point Likert scale ranging from 0 (I cannot do it) to 10 (certain I can do it). In this study, Cronbach’s α for SER was 0.88.
Statistical Analyses
All data were computerized and analyzed by the Statistical Package for the Social Sciences (SPSS 26.0, Chicago, IL, USA) and R statistical software (version 4.3.1). SPSS 26.0 was used to describe sociodemographic and clinical characteristics. R 4.3.1 was used to construct networks.
Networks Estimation
The presented networks were estimated via Gaussian graphical model.37 Within a network model, each component is viewed as a node and the connection between two nodes is represented as an edge.38 Gaussian graphical model is undirected network, and its edge represents the partial correlation between nodes after controlling for all other nodes in the network.39 The least absolute shrinkage and selection operator (LASSO) and extended Bayesian information criteria (EBIC) were applied to shorten edges in the networks and select relevant tuning parameters, resulting in a sparser and easier-to-interpret network.40 The Fruchterman-Reingold algorithm was adopted to visualize the network.41 Thicker edges represented stronger correlations between two nodes.42,43
Centrality and Stability
The centrality of strength was used to quantify the importance of each node in the item network of kinesiophobia, which is the sum of the absolute value of the edge weights attached to a node for each node. The strength is an indicator of network connectivity, used to identify the central nodes.38 And rs was used to represent the strength centrality. To examine the interconnections between pain catastrophizing, self-efficacy and kinesiophobia, we divided nodes into two communities, namely, the pain catastrophizing/self-efficacy community (dimensions from PCS and SER) and the kinesiophobia community (items from TSK). Bridge expected influence (BEI) was calculated to identify bridge components. The BEI of one node is the summed edge weights to the nodes of all other communities.31 The higher the positive value of BEI, the greater the activation capacity to other communities; while the higher the negative value of BEI, the greater the deactivation capacity to other communities.31
The 95% confidence intervals (CI) of all edges were calculated using a nonparametric bootstrap approach (2000 bootstrap samples) to ensure the accuracy of edge weights. The correlation stability (CS) coefficient of the strength/BEI was computed by using a case-dropping subset bootstrap (with 2000 bootstrap samples) to evaluate the stability.44 The value of the CS coefficient should not be less than 0.25 and preferably greater than 0.5.44 Bootstrapped difference tests (2000 bootstrap samples) for edge weights, strength, and BEI were conducted.
Results
Descriptive Statistics
Table 1 shows the sample characteristics (n=216). The mean age of the sample was 66.7 (SD 6.1), ranging from 51 to 81 years old. The mean scores of items of kinesiophobia are presented in Table 2.
Table 1.
Socio-Demographic and Clinical Characteristics (N=216)
| n | % | |
|---|---|---|
| Age | ||
| <65 | 78 | 36.1 |
| ≥65 | 138 | 63.9 |
| Gender | ||
| Men | 44 | 20.4 |
| Women | 172 | 79.6 |
| Marital status | ||
| Married or with life partner | 181 | 83.8 |
| Single (includes divorced, widowed, separated) | 35 | 16.2 |
| Education attainment | ||
| Junior high school or lower | 179 | 82.9 |
| Senior high school or higher | 37 | 17.1 |
| Income monthly per person | ||
| <2000 RMB (274$) | 121 | 56.0 |
| 2000–4000 RMB (274–548$) | 65 | 30.1 |
| ≥4000 RMB (548$) | 30 | 13.9 |
| Joint pain duration | ||
| <5 years | 56 | 25.9 |
| 5–10 years | 42 | 19.5 |
| ≥10 years | 118 | 54.6 |
| Replacement site | ||
| Left joint | 110 | 50.9 |
| Right joint | 106 | 49.1 |
Table 2.
Abbreviation, Mean Scores, and Standard Deviations for Items of the Tampa Scale for Kinesiophobia
| Number | Items | Mean | SD |
|---|---|---|---|
| TSK1 | I am afraid that I might injury myself if I exercise | 2.3 | 1.1 |
| TSK2 | If I were to try to overcome it, my pain would increase | 2.0 | 0.8 |
| TSK3 | My body is telling me I have something dangerously wrong | 1.7 | 0.8 |
| TSK4* | My pain would probably be relieved if I were to exercise | 2.2 | 0.9 |
| TSK5 | People are not taking my medical condition seriously enough | 1.6 | 0.8 |
| TSK6 | My accident has put my body at risk for the rest of my life | 2.0 | 1.0 |
| TSK7 | Pain always means I have injured my body | 2.3 | 1.0 |
| TSK8* | Just because something aggravates my pain does not mean it is dangerous | 2.2 | 0.9 |
| TSK9 | I am afraid that I might injure myself accidentally | 2.3 | 1.0 |
| TSK10 | Simply being careful that I do not make any unnecessary movements is the safest thing I can do to prevent my pain from worsening | 2.2 | 1.1 |
| TSK11 | I would not have this much pain if there were not something potentially dangerous going on in my body | 1.9 | 0.8 |
| TSK12* | Although my condition is painful, I would be better off if I were physically active | 2.2 | 0.9 |
| TSK13 | Pain lets me know when to stop exercising so that I do not injure | 3.2 | 0.7 |
| TSK14 | It’s really not safe for a person with a condition like mine to be physically active | 2.1 | 0.9 |
| TSK15 | I cannot do all the things normal people do because it’s too easy for me to get injured | 1.8 | 0.9 |
| TSK16* | Even though something is causing me a lot of pain, I do not think it’s actually dangerous | 2.0 | 0.7 |
| TSK17 | No one should have to exercise when he/she is in pain | 3.0 | 0.9 |
Notes: *Negatively worded, reversed scored items.
Abbreviation: SD, Standard Deviations.
The Item of Kinesiophobia Network Structure
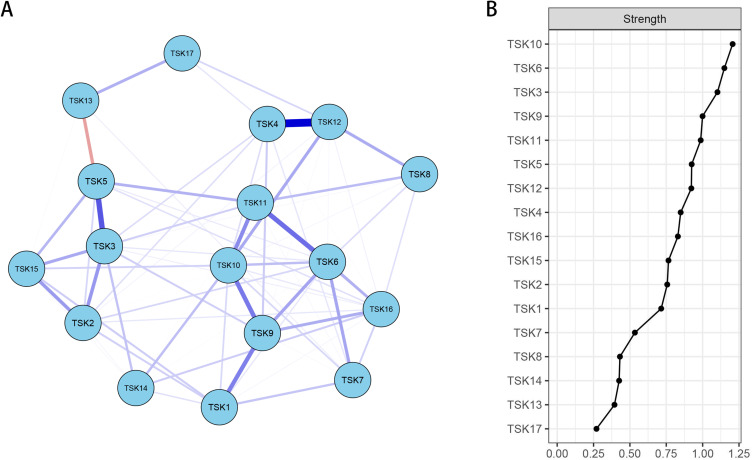
The item network of kinesiophobia is shown in Figure 2A. Two positive edges with strongest partial correlations existed between TSK4–TSK12 (weight=0.47) and TSK3–TSK5 (weight=0.31), were thicker than other edges, indicating that these two correlations were stronger than other relations. The bootstrap 95% CI is relatively narrow, indicating that the item network is considered to be accurate (Figure s1). Figure s2 shows the bootstrapped difference test for edge weights.
Figure 2.
Network structure of kinesiophobia and centrality index (A) Item network of kinesiophobia in patients after total knee arthroplasty; (B) Strength centrality index of the network. Note: Blue edges represent positive correlations, and red edges represent negative correlations. The thickness of the edge reflects the magnitude of the correlation.
Figure 2B displays the strength centrality. Three nodes with the highest strength were TSK10 (rs =1.5), TSK6 (rs =1.3) and TSK3 (rs =1.1). The CS coefficient of strength was 0.44, which was above the recommended cut-off (Figure s3). Figure s4 shows the bootstrapped difference tests for strength.
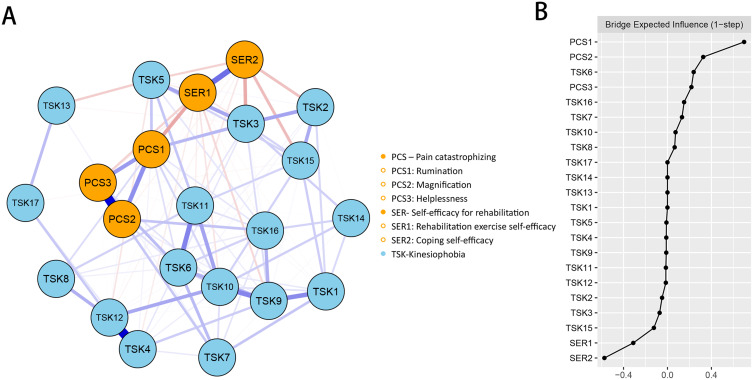
The Pain Catastrophizing/Self-Efficacy-Kinesiophobia Network Structure
The pain catastrophizing/self-efficacy-Kinesiophobia network structure is presented in Figure 3A. The strongest positive edges between communities were between PCS1-TSK3 (weight=0.14) and PCS3-TSK6 (weight=0.13) and the strongest negative edges were SER2-TSK3 (weight=−0.16) and SER2-TSK15 (weight=−0.13). The bootstrap 95% CI plot supported the edges in this network are accurate (Figure s5). Figure s6 shows the bootstrapped difference test for edge weights.
Figure 3.
Network structure of pain catastrophizing/self-efficacy-kinesiophobia and centrality index (A) Network construction of different components of pain catastrophizing (PCS), self-efficacy for rehabilitation (SER) and kinesiophobia in patients after total knee arthroplasty; (B) Bridge expected influence centrality index of the network. Note: Blue edges represent positive correlations, and red edges represent negative correlations. The thickness of the edge reflects the magnitude of the correlation.
Figure 3B depicts the BEI for each node within the pain catastrophizing/self-efficacy-Kinesiophobia network. In the pain catastrophizing/self-efficacy community, PCS1 (“rumination”) has the highest positive value of BEI (0.70), indicating the strongest positive relations with kinesiophobia community from the network perspective, and SER2 (“coping self-efficacy”) has the highest negative value of BEI (−0.57), suggesting the strongest negative correlations with kinesiophobia community. The CS-coefficient of BEI is 0.36, which was above the recommended cut-off (Figure s7). Figure s8 shows the bootstrapped difference tests for BEI.
Discussion
To our knowledge, this is the first study to apply network analysis to explore the interconnections among components of kinesiophobia and the correlations between constructs of pain catastrophizing, self-efficacy, and kinesiophobia in patients after TKA. This study provides a new insight to develop more effective interventions to address kinesiophobia, and promote better PROMS.
Within the item network of kinesiophobia, two positive edges with the strongest weights were TSK4 (My pain would probably be relieved if I were to exercise)-TSK12 (Although my condition is painful, I would be better off if I were physically active) and TSK3 (My body is telling me I have something dangerously wrong)-TSK5 (People are not taking my medical condition seriously enough). The strong edge weight between the two nodes indicates that these two nodes have a high co-occurrence.42,43 TSK4 and TSK12 are similar statements that describe that patients consider active physical activity and exercise beneficial in relieving pain; therefore, there is a strong correlation between them. For TSK3-TSK5, inadequate attention and support from significant others might lead to lower confidence to deal with disease, thus perceiving more dangers of disease or pain symptoms. These findings represent the strong connections pathways between components of kinesiophobia, providing a new theoretical insight to better understanding the interrelationships.
Network analysis can help identify the relative importance of each node, and nodes with higher strength may have more potent influences on the network than nodes with lower strength. In the item network of kinesiophobia, TSK10 (“Simply being careful that I do not make any unnecessary movements is the safest thing I can do to prevent my pain from worsening”), TSK6 (“My accident has put my body at risk for the rest of my life”) and TSK3 (“My body is telling me I have something dangerously wrong”) had the highest strength centrality, indicating TSK10, TSK6 and TSK3 may be the central components of kinesiophobia. Previous studies mentioned that central components could predict changes in other components, may propagate intervention effects to connected components within a network and can serve as promising targets for interventions.45,46 Therefore, interventions on TSK10, TSK6, and TSK3 may propagate the effects to TSK5, TSK9, and TSK11, then spread to more components of this network, ultimately impacting the entire network. This suggests that the intervention directed at these three components of kinesiophobia could effectively prevent and reduce kinesiophobia, providing us a new perspective to develop targeted interventions for kinesiophobia among patients after TKA.47
The network displayed strong edges connecting nodes that may be clinically important for understanding the mechanism of pain catastrophizing, self-efficacy, and kinesiophobia (Figure 2). Edge PCS1 (rumination)-TSK3 (My body is telling me I have something dangerously wrong) and PCS3 (helplessness)-TSK6 (My accident has put my body at risk for the rest of my life) revealed a link between rumination, helplessness and perceived danger. Based on the fear-avoidance model, Individuals with excessive focus on pain symptoms and high awareness of being unable to control the pain perceive pain as a threat, which may result in believing that some pain-induced activities are dangerous and further lead to avoidance.21 Edge SER2 (coping self-efficacy)-TSK3 (My body is telling me I have something dangerously wrong) and SER2 (coping self-efficacy)-TSK15 (I cannot do all the things normal people do because it’s too easy for me to get injured) shows the correlations of coping self-efficacy with perceived danger and dysfunctional self. Coping self-efficacy refers to the confidence of coping with some situations in rehabilitation exercise, such as, fatigue, pain.24 Persons with lower confidence to cope with situations in rehabilitation exercises may adopt negative and avoidance strategies,48 which may perceive that situation as a threat and a decline in their own functioning.
Within the pain catastrophizing/self-efficacy-kinesiophobia network, node bridge centrality may shed light on the specific role played by different constructs of pain catastrophizing and self-efficacy in the formation and maintenance of kinesiophobia. In the pain catastrophizing and self-efficacy community, PCS1 (rumination) and SER2 (coping self-efficacy) were identified as the bridge constructs connected to kinesiophobia. These findings suggest rumination and coping self-efficacy are more closely related to kinesiophobia than other constructs of pain catastrophizing and self-efficacy. Previous studies reported that the score of the rumination dimension was higher than the other two in, suggesting rumination may be the more common characteristic of pain catastrophizing in patients after TKA.49,50 Excessive focus on pain symptoms is more likely to generate fear of pain-inducing exercise and lead to avoidance behaviors.16 Patients with low coping self-efficacy may utilize more negative coping strategies to face the stresses caused by rehabilitation exercise after TKA, which further Results in fear of exercise.26 Targeting the bridge components may lead to the deactivation of the pathway of spread and a reduction in co-occurrence.28 Thus, intervention in preventing and decreasing kinesiophobia from the perspective of pain catastrophizing and self-efficacy, which targets the two constructs, may be more effective.
Limitations
There are several Limitations in this study. First, this study conducted a cross-sectional survey. Thus, a causal link between pain catastrophizing, self-efficacy, and kinesiophobia cannot be determined. Future studies with a longitudinal design are needed to explore the causality between these components. Second, convenience sampling and single-center study setting limited the generalizability of our findings. Third, it is difficult to conduct subgroup analysis with the small sample size in this study. Further studies with a larger sample size are needed to compare the difference characteristics group network.
Future Directions and Clinical Implications
This study also has some implications for future research and clinical practice. A cross-lagged panel network analysis design was suggested to explore the causal relationship between pain catastrophizing, self-efficacy and kinesiophobia. Future research is recommended to develop interventions that target the identified three components of kinesiophobia and rumination of pain catastrophizing and coping self-efficacy, and clinical intervention trials could be conducted to validate effectiveness. Cognitive behavioral therapy is the most experienced and effective psychosocial therapy for addressing kinesiophobia among patients after TKA.51 In addition, relaxation exercise therapy and virtual reality has also been explored as effective measures for reducing kinesiophobia for TKA patients.52,53 Previous studies showed that rumination-focused cognitive-behavioral therapy and mindfulness-based therapies are useful for relieving pain-related rumination.54,55 Furthermore, we suggest that some techniques, such as performance accomplishments, verbal persuasion, vicarious learning, should be applied with a focus on coping self-efficacy.56,57
Conclusion
This study reconstructed the kinesiophobia from network perspectives, finding its unique network structures and suggesting three central components as potential targets for effective intervention. Rumination and coping self-efficacy were identified as the bridge components within connections between pain catastrophizing, self-efficacy, and kinesiophobia. These findings shed light on future studies aiming to develop theoretical understanding and interventions for relieving kinesiophobia.
Acknowledgments
We acknowledge the contributions of all the participants in this study.
Funding Statement
This study was supported by the Science and Technology Program of Baoding (grant number: 2341ZF092).
Ethics Approval and Consent to Participate
The study is approved by the Institutional Review Board of Baoding No.1 Central Hospital [Approval Number: [2022]068], and written informed consent for participants is obtained in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no relevant competing interests to disclose in this work.
References
- 1.World Health Organization. Osteoarthritis; Available from: https://www.who.int/news-room/fact-sheets/detail/osteoarthritis.Accessed June 7 2024.
- 2.Chang J, Fu M, Cao P, Ding C, Wang D. Patient-reported quality of life before and after total knee arthroplasty: a multicenter observational study. Patient Prefer Adherence. 2022;16:737–748. doi: 10.2147/PPA.S357632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991-2010. JAMA. 2012;308(12):1227–1236. doi: 10.1001/2012.jama.11153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bian YY, Cheng KY, Chang X, Weng XS. Reports and analysis of amount of Hip and knee arthroplasty in China from 2011 to 2019. Chin J Orthop. 2020;40(21):1453–1460. doi: 10.3760/cma.j.cn121113-20200320-00177 [DOI] [Google Scholar]
- 5.Bakaa N. Exercise adherence post total knee arthroplasty. McMaster Univ. 2020. [Google Scholar]
- 6.Chen H, Li S, Ruan T, Liu L, Fang L. Is it necessary to perform prehabilitation exercise for patients undergoing total knee arthroplasty: meta-analysis of randomized controlled trials. Phys Sportsmed. 2018;46(1):36–43. doi: 10.1080/00913847.2018.1403274 [DOI] [PubMed] [Google Scholar]
- 7.Sánchez Romero EA, Fernández-Carnero J, Calvo-Lobo C, Ochoa Saez V, Burgos Caballero V, Pecos-Martín D. Is a combination of exercise and dry needling effective for knee OA? Pain Med. 2020;21(2):349–363. doi: 10.1093/pm/pnz036 [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Romero EA, González-Zamorano Y, Arribas-Romano A, et al. Efficacy of manual therapy on facilitatory nociception and endogenous pain modulation in older adults with knee osteoarthritis: a case series. Appl Sci. 2021;11(4):1895. doi: 10.3390/app11041895 [DOI] [Google Scholar]
- 9.Qu QQ. The Relationship between Family Resilience, Activation and Exercise Compliance in Patients with Artificial Joint Replacement. Dalian Med Univ. 2022. [Google Scholar]
- 10.Li FY. Study on compliance and influencing factors of home rehabilitation training for patients after total knee arthroplasty in Hainan Province. Hainan Med Univ. 2021. [Google Scholar]
- 11.Zhao GY. Home-based rehabilitation adherence and its influencing factors among patients who underwent total knee arthroplasty. Shanghai Jiao Tong Univ. 2019. [Google Scholar]
- 12.Bakaa N, Chen LH, Carlesso L, Richardson J, Macedo L. Reporting of post-operative rehabilitation interventions for total knee arthroplasty: a scoping review. BMC Musculoskelet Disord. 2021;22(1):602. doi: 10.1186/s12891-021-04460-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alrawashdeh W, Eschweiler J, Migliorini F, El Mansy Y, Tingart M, Rath B. Effectiveness of total knee arthroplasty rehabilitation programmes: a systematic review and meta-analysis. J Rehabil Med. 2021;53(6):1–12. doi: 10.2340/16501977-2827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kori S. Kinesiophobia: a new view of chronic pain behaviour. Pain Manag. 1990;3:35–43. [Google Scholar]
- 15.Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019;53(9):554–559. doi: 10.1136/bjsports-2017-098673 [DOI] [PubMed] [Google Scholar]
- 16.Xu HP, Zhang YG, Liu YJ, et al. A multifactorial model of kinesiophobia in patients with knee arthroplasty. Chin J Nurs. 2021;56(10):1460–1465. doi: 10.3761/j.issn.0254-1769.2021.10.003 [DOI] [Google Scholar]
- 17.Bunzli S, Smith A, Watkins R, Schütze R, O’Sullivan P. What do people who score highly on the Tampa scale of kinesiophobia really believe? Clin J Pain. 2015;31(7):621–632. doi: 10.1097/AJP.0000000000000143 [DOI] [PubMed] [Google Scholar]
- 18.Zia S, Atta S, Ahmad MS, Murtaza F, Ahmad MZ, Hassan SZ. Relationship between kinesiophobia, fall risk and activity level among elderly females after total knee arthroplasty. J Riphah Coll Rehabili Sci. 2022;10(2):70–74. doi: 10.53389/JRCRS.2022100203 [DOI] [Google Scholar]
- 19.Sullivan M, Tanzer M, Stanish W, et al. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009;143(1–2):123–129. doi: 10.1016/j.pain.2009.02.011 [DOI] [PubMed] [Google Scholar]
- 20.Sullivan MJ, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64. doi: 10.1097/00002508-200103000-00008 [DOI] [PubMed] [Google Scholar]
- 21.Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, Karoly P. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–483. doi: 10.1097/AJP.0b013e3182385392 [DOI] [PubMed] [Google Scholar]
- 22.Londhe SB, Shah RV, Patwardhan M, Doshi AP, Londhe SS, Subhedar K. Understanding the apprehension and concern haunting patients before a total knee arthroplasty. Arthroplasty. 2021;3:14. doi: 10.1186/s42836-021-00069-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vogel M, Riediger C, Krippl M, Frommer J, Lohmann C, Illiger S. Negative affect, type D personality, quality of life, and dysfunctional outcomes of total knee arthroplasty. Pain Res Manag. 2019;2019: 6393101. doi: 10.1155/2019/6393101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waldrop D, Lightsey OR, Ethington CA, Woemmel CA, Coke AL. Self-efficacy, optimism, health competence, and recovery from orthopedic surgery. J Couns Psychol. 2001;48(2):233–238. doi: 10.1037/0022-0167.48.2.233 [DOI] [Google Scholar]
- 25.Bandura A. Self-Efficacy in Changing Societies. Cambridge University Press: 1995. [Google Scholar]
- 26.Cai L, Liu Y, Xu H, Xu Q, Wang Y, Lyu P. Incidence and risk factors of kinesiophobia after total knee arthroplasty in Zhengzhou, China: a cross-sectional study. J Arthroplasty. 2018;33(9):2858–2862. doi: 10.1016/j.arth.2018.04.028 [DOI] [PubMed] [Google Scholar]
- 27.Ding Y, Pan Y, Wang M, et al. Factors influencing kinesiophobia during the “blanking period” after radiofrequency catheter ablation in patients with atrial fibrillation by the fear-avoidance model. Int J Cardiol. 2022;363:49–55. doi: 10.1016/j.ijcard.2022.06.021 [DOI] [PubMed] [Google Scholar]
- 28.French DJ, France CR, Vigneau F, French JA, Evans RT. Fear of movement/(re) injury in chronic pain: a psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK). Pain. 2007;127(1–2):42–51. doi: 10.1016/j.pain.2006.07.016 [DOI] [PubMed] [Google Scholar]
- 29.Cui Y, Yang T, Gao H, et al. The relationship between ego depletion and work alienation in Chinese nurses: a network analysis. Front Psychol. 2022;13:15959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 31.Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2021;56(2):353–367. doi: 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- 32.Zhou Y, Gao W, Gao S, Guo X, Liu M, Cao C. Pain catastrophizing, kinesiophobia and exercise adherence in patients after total knee arthroplasty: the mediating role of exercise self-efficacy. J Pain Res. 2023;16:3993–4004. doi: 10.2147/JPR.S432106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu W. Cross-cultural adaptation of simplified Chinese version of TSK/FABQ, and its clinical application in the assessment of fear avoidance for patients with low back pain. Naval Med Univ. 2012. [Google Scholar]
- 34.Yap JC, Lau J, Chen PP, et al. Validation of the Chinese pain catastrophizing scale (HK-PCS) in patients with chronic pain. Pain Med. 2008;9(2):186–195. doi: 10.1111/j.1526-4637.2007.00307.x [DOI] [PubMed] [Google Scholar]
- 35.Pei J, Chen H, Ma T, et al. Pain catastrophizing and associated factors in preoperative total knee arthroplasty in Lanzhou, China: a cross-sectional study. BMC Musculoskelet Disord. 2022;23(1):507. doi: 10.1186/s12891-022-05435-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang HY, Xu YL, Hu SL, Zhou L, Qian Y, Qian HJ. Evaluation of the reliability and validity of Chin ese version self-efficacy for rehabilitation outcome scale. Chin J Modern Nurs. 2014;20(3):268–270. doi: 10.3760/cma.j.issn.1674-2907.2014.03.007 [DOI] [Google Scholar]
- 37.Epskamp S, Waldorp LJ, Mõttus R, Borsboom D. The gaussian graphical model in cross-sectional and time-series data. Multivariate Behav Res. 2018;53(4):453–480. doi: 10.1080/00273171.2018.1454823 [DOI] [PubMed] [Google Scholar]
- 38.Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 39.Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. 2018;23(4):617–634. doi: 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- 40.Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi: 10.1093/biostatistics/kxm045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fruchterman TM, Reingold EM, Spagnolo S. Graph drawing by force‐directed placement. Software: practice and experience. Giornale italiano di cardiologia. 1991;21(11):1129–1164. doi: 10.1002/spe.43802111021804751 [DOI] [Google Scholar]
- 42.Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med. 2018;6(1):301–328. doi: 10.1080/21642850.2018.1521283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Costantini G, Epskamp S, Borsboom D, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Pers. 2015;54:13–29. doi: 10.1016/j.jrp.2014.07.003 [DOI] [Google Scholar]
- 44.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodebaugh TL, Tonge NA, Piccirillo ML, et al. Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? J Consult Clin Psychol. 2018;86(10):831–844. doi: 10.1037/ccp0000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haslbeck J, Ryan O, Robinaugh DJ, Waldorp LJ, Borsboom D. Modeling psychopathology: from data models to formal theories. Psychol Methods. 2021;27(6):930–957. doi: 10.1037/met0000303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hofmann SG, Curtiss J, McNally RJ. A complex network perspective on clinical science. Perspect Psychol Sci. 2016;11(5):597–605. doi: 10.1177/1745691616639283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Delahaij R, Van Dam K. Coping with acute stress in the military: the influence of coping style, coping self-efficacy and appraisal emotions. Pers Individ Dif. 2017;119:13–18. doi: 10.1016/j.paid.2017.06.021 [DOI] [Google Scholar]
- 49.Pan Q. Pain catastrophizing and its influencing factors of old total knee arthroplasty patients: a longitudinal study. Zhengzhou Univ. 2022. [Google Scholar]
- 50.Li CF, He L, Huang YL, et al. Pain catastrophe and its influencing factors in patients undergoing total knee arthroplasty. J Nurs Sci. 2020;35(23):22–24+38. doi: 10.3870/j.issn.1001-4152.2020.23.022 [DOI] [Google Scholar]
- 51.Cai L, Gao H, Xu H, Wang Y, Lyu P, Liu Y. Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up. J Arthroplasty. 2018;33(3):704–710. doi: 10.1016/j.arth.2017.10.035 [DOI] [PubMed] [Google Scholar]
- 52.Gür O, Başar S. The effect of virtual reality on pain, kinesiophobia and function in total knee arthroplasty patients: a randomized controlled trial. The Knee. 2023;45:187–197. doi: 10.1016/j.knee.2023.09.012 [DOI] [PubMed] [Google Scholar]
- 53.Eymir M, Unver B, Karatosun V. Relaxation exercise therapy improves pain, muscle strength, and kinesiophobia following total knee arthroplasty in the short term: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2776–2785. doi: 10.1007/s00167-021-06657-x [DOI] [PubMed] [Google Scholar]
- 54.Soleymani A, Arani AM, Raeissadat SA, Davazdahemami MH. Rumination-Focused cognitive-behavioral therapy for chronic low back pain: a randomized controlled trial. Galen Med J. 2020;9:e1722. doi: 10.31661/gmj.v9i0.1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meints SM, Stout M, Abplanalp S, Hirsh AT. Pain-related rumination, but not magnification or helplessness, mediates race and sex differences in experimental pain. J Pain Res. 2017;18(3):332–339. doi: 10.1016/j.jpain.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 56.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191 [DOI] [PubMed] [Google Scholar]
- 57.Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2013;10(1):29. doi: 10.1186/1479-5868-10-29 [DOI] [PMC free article] [PubMed] [Google Scholar]