Despite repeated pleas over the years, starting from the Almaty pledge of 1978 to the Sustainable Development Goals of 2030, the provision of high-quality primary healthcare (PHC) that is safe, accessible and affordable remains an elusive goal1. It is in this light that the Asthana Declaration of 2018, which calls for greater community engagement and the need to harness the services and skills of existing resources within communities, needs to be carefully examined2. Is it the case that once we take contextual factors into account, there are low-hanging solutions that could dramatically improve the quality of PHC, even though these effective strategies may, at first, face seemingly insurmountable political challenges?3
To understand whether such low-hanging solutions exist, one needs to first understand the source of the problem. An ideal PHC worker embodies a rare perfect trinity: (i) scientific (S) in approach, (ii) socially integrated (I) so as not to be considered as culturally alien or an imposition of a top-down health system; and (iii) available (A) at the affected individual’s doorstep at their time of need. However, this trinity S-I-A has proven to be difficult to fulfil; healthcare providers who are up-to-date on the latest science and the highly qualified are seldom found in rural settings or urban slums, where most of India’s population lives. Furthermore, even when these professionals are posted to such locations, the lack of complementary resources, low patient loads and cultural barriers frequently preclude their ability to provide care at the high standards that they were trained to aspire to.
The rarity of this ideal trinity has fostered an interesting new innovation, now actively implemented in several countries: The emergence of a cadre of healthcare providers called non-physician clinicians (NPCs), who are allowed to practice in a broad sense as a complement to fully trained providers. For example, as shown in Figure, across most Sub-Saharan African countries, the majority of health clinics are staffed solely by providers who are less than fully qualified doctors. The innovation here is the inversion of the S-I-A triangle: Traditionally, healthcare systems have focused on the ‘Scientific’ and given short shrift to the ‘Integrated’ and ‘Available’, but the widespread use of non-physician clinicians emphasizes the ‘I’ and the ‘A’ instead, arguing that ‘S’ can be met by integrating non-physician clinicians with formal doctors through various means.
Figure.
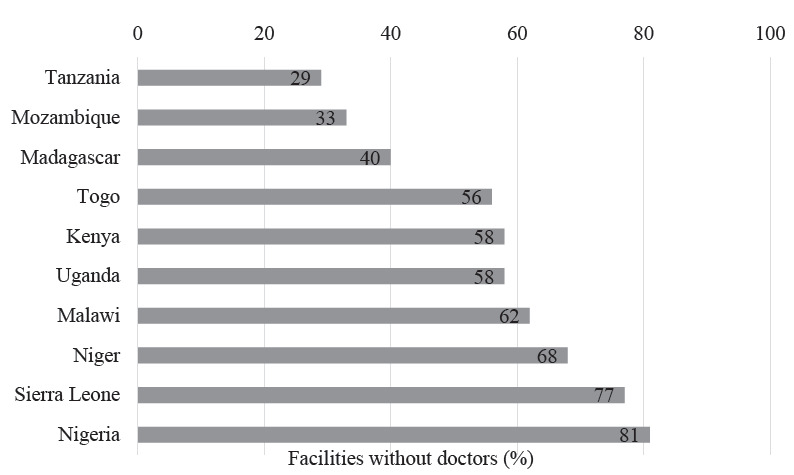
Fraction of clinics without a doctor in Sub-Saharan African countries. Note: Author’s analysis based on data from the World Bank’s Service Delivery Indicators.
The S-I-A triangle in India
To understand what inverting the S-I-A triangle means for India, three key features of the Indian health system are highlighted below.
The first feature of the health system is the large number of informal healthcare providers in virtually every Indian State. A systematic count of all types of healthcare workers in a representative sample of rural Indian villages showed that the average village in the country had 3.2 primary care providers, of whom 86 per cent were in the private sector and 68 per cent were informal providers4. Further, careful tally in three districts of Madhya Pradesh that accounted for the fact that people often visit healthcare providers outside the village uncovered that close to 80 per cent of primary care was provided by informal providers5. Subsequent studies have repeatedly come to similar conclusions in smaller samples and found that informal providers remain the dominant source of primary care even in villages with a public PHC6,7.
Who are these informal providers? These are predominantly males working in a virtually unregulated healthcare market, who have not received any scientifically rigorous training and are not accredited by a legal board8. Many took to this profession as “craftsmen,” precisely the “craft” of drug dispensing, as their source of livelihood, while doing an apprenticeship with qualified practitioners for a variable period of time9. The standard educational grades that these individuals pursued before joining this clan as a healthcare provider vary widely, and similarly variegated are their culture and operational modalities. They are aware that this professional activity is illegal, giving them a feeling of guilt, but they tend to override this and claim immunity from a moral perspective of serving people in need. Many, particularly those who work in far-flung villages and difficult-to-access locations, are the only healthcare human resource available to the population in acute distress10. This availability, a ‘candle in the dark’–type of scenario, draws them closer to the population they serve and tends to abrogate their inadequacies of scientific knowledge and training. As a group, they maintain a working relationship with formal mainstream practitioners and copy their art of prescribing, functioning as a multiplier of their prescription habits9.
The second feature of the Indian healthcare system is that the proliferation of informal healthcare providers does not decline systematically with the improvement and extension of the formal system of care. As we move from the States with lower to higher levels of human development, the share of informal providers remains the same, but their quality improves4. In fact, these quality improvements are so dramatic that the objective and scientific knowledge of how to manage key common conditions among informal providers in a State like Tamil Nadu is comparable to that of fully trained MBBS doctors in other States. Further, even though informal providers overuse antibiotics, their use of antibiotics and steroids is lower than among fully trained doctors11.
This does not imply that informal providers are of higher quality than fully trained doctors–they emphatically are not. Instead, it implies that there is such high variance in the quality of training that there are better as well as worse formally trained doctors. Furthermore, in the quality of apprenticeship of the informal doctors, interestingly, the best informal healthcare providers may be similar or even more knowledgeable than poorly trained formal providers.
The third feature of the Indian healthcare system is that, following the Bhore Committee Report of 1946, India eliminated licentiate providers and argued instead that care could only be provided by fully trained MBBS doctors12. Consequently, even though the existence and operation of informal providers are well known to those in the medical system (and obviously to the hundreds of millions of individuals who regularly use them), a veneer of untouchability prevails whenever the question of utilizing informal providers with a defined purpose arises within mainstream healthcare planning forums. A curious contradiction that has emerged is that, even as informal providers are frequently used in an opportunistic manner at the local level, these programmes have then proven impossible to integrate into systematic policy.
What does inverting the S-I-A triangle mean for India?
The Indian health system is in a state of flux with rapid change at ground level. Our mainstream public sector outreach is increasing through Ayushman Bharat Wellness Centres and an increased focus on non-communicable diseases (NCDs), tuberculosis control and countering the spiralling menace of antimicrobial resistance. This seems to be working given that a recent paper from Rajasthan showed that expanding wellness centres led to a decline in mortality for the elderly as NCDs were more likely to be detected and managed13.
The question we then pose is whether the strategic inclusion of the informal healthcare providers might add further value and help us achieve our PHC goals even as the outreach of the public sector continues apace. While this question has been posed before14, what we bring to the table is an evidence-based approach to the question, which allows for further discussion to happen on the basis of the best available scientific evidence. We draw on two examples, documenting how such evidence can be generated in the case of informal providers.
Our first example asks whether training informal providers can improve their diagnosis and management of patients. This is not a foregone conclusion, but both perceived wisdom and careful economic theorizing suggest that such training can backfire if, for instance, it falsely increases the confidence of the population in their abilities and emboldens them to practice in a manner that is not commensurate with their training. To evaluate this question, researchers studied the Liver Foundation’s pioneering multitopic training programme, which included more than 50 classes over a nine-month period15. The team first randomized informal providers into a treatment group that received the training and a control group that did not. They then sent “standardized patients” or people recruited from the local community to present the same condition to multiple providers in both treatment as well as control groups. Uniquely, the team used a “triple-blind” randomized design, whereby Liver Foundation did not know what healthcare providers would be assessed on, healthcare providers did not know who the standardized patients were and standardized patients did not know which providers were in the treatment versus control groups. This strict design, which is a first for the evaluation of any training programme worldwide, ensured that the results accurately captured the impact of the programme on outcomes, independent of any biases or teaching to the test.
This landmark study showed that the training programme significantly improved correct management among informal providers so much so that the care they now provided was similar to that provided in PHCs in the few cases that such facilities were available15. However, it was also noted that the programme was unsuccessful at decreasing the use of antibiotics or other unnecessary medications.
The results of this trial inspired the Government of West Bengal to initiate a State-wide training programme for informal healthcare providers in 2017 that is still ongoing16. For this, nursing training centres are chosen as the training hubs and nursing tutors as the trainers. The curriculum has been developed by medical academics ratified by a Government committee and is being implemented in teaching classroom sessions of 4 h each week for 24 wk. Prior to initiating the programme, Accredited Social Health Activist (ASHA) workers enumerated informal health workers across the State and from this list, 50 in each community development block are included through a lottery for the six-month training course.
Our second example asks whether the trust and acceptance of informal healthcare providers can be utilized in emergency situations. During COVID-19, it became apparent that many patients could be managed at an off-hospital site as long as there was clear communication and the possibility of rapid transfer to a hospital if needed. The Liver Foundation, in coordination with local governments, set up eight COVID Care Centres, each led by a registered MBBS doctor and staffed by a combination of informal providers and nurses. These eight COVID Care Centres admitted a total of 113 patients between May 18 and July 5, 2021, 58 per cent of whom were female with an average age of 54 yr. The assessment of these centres showed that the patients came from large catchment areas and the vast majority were normally discharged (82%). The remaining were referred (16%) or made their own arrangements (2%). Encouragingly, there were no patient deaths and out of the 13 patients that arrived with critically low SpO2 levels, eight could be stabilized at the Covid Care Centres and discharged in good condition17.
These two examples indicate two different circumstances, ranging from regular care under ‘business as usual’ situations to care under emergency conditions. In both cases, the Liver Foundation was able to leverage the available resources to improve the availability and quality of care for rural populations in difficult to reach areas, ensuring that the programme juxtaposed trained providers with available resources on the ground. While the opportunistic use of informal providers is common on the ground, the discussed approach adds value by systematically marrying ground-level implementation with the generation of the best evidence of its efficacy. Both programmes provide some grounds for optimism in the ability to use informal providers to improve primary care in areas where fully qualified doctors are hard to find. Indeed, there is similar evidence to show that informal healthcare providers also have an important role to play in public health issues that seek innovative human resource solutions, such as tuberculosis control18,19.
Conclusions
The “know-do” gap–whereby there is a large gap between the clinical practices and the knowledge of healthcare providers, is a cultural–behavioural issue that has been shown to impair the performance of trained healthcare providers in India and other countries which are within the mainstream healthcare delivery system20,21. A similar agnosia prevails in the discourse on healthcare human resource planning whenever the issue of utilization and mainstreaming of informal healthcare providers arises.
Meanwhile, tools like those arising out of telehealth and artificial intelligence are emerging as promising modalities for guiding, monitoring and regulating the clinical behaviour of health workers in remote locations. Implementation research on these issues could provide high dividends as long as the research is conducted with an open mind. Innovations always have their origins in creative opinions, but it is the evidence that makes it perfect.
Let us then choose to generate the evidence before dismissing informal healthcare providers as past relics of underdevelopment. The urgency of this moment requires nothing less.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- 1.World Health Organization Declaration of Alma-Ata. Available from: https://iris.who.int/bitstream/handle/10665/347879/WHO-EURO-1978-3938-43697-61471-eng.pdf?sequence=1, accessed on March 2, 2024.
- 2.World Health Organization and United Nations Children’s Fund Declaration of Astana: Global Conference on Primary Health Care. Available from: https://www.who.int/docs/default- source/primary-health/declaration/gcphc-declaration.pdf, accessed on March 2, 2024.
- 3.Van den Muijsenbergh M, Van Weel C. The essential role of primary care professionals in achieving health for all. Ann Fam Med. 2019;17:293–5. doi: 10.1370/afm.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das J, Daniels B, Ashok M, Shim EY, Muralidharan K. Two Indias: The structure of primary health care markets in rural Indian villages with implications for policy. Soc Sci Med. 2022;301:112799. doi: 10.1016/j.socscimed.2020.112799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Das J, Mohpal A. Socioeconomic status and quality of care in rural India: new evidence from provider and household surveys. Health Aff. 2016;35:1764–73. doi: 10.1377/hlthaff.2016.0558. [DOI] [PubMed] [Google Scholar]
- 6.Chandra S, Bhattacharya S. Unqualified Medical Practitioners: Their illegal but indispensable role in primary healthcare. Economic and Political Weekly. 2019;54:36–44. [Google Scholar]
- 7.Rao KD, Mehta A, Noonan C, Peters MA, Perry H. Voting with their feet: Primary care provider choice and its implications for public sector primary care services in India. Soc Sci Med. 2024;340:116414. doi: 10.1016/j.socscimed.2023.116414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PloS one. 2013;8:e54978. doi: 10.1371/journal.pone.0054978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gautham M, Shyamprasad KM, Singh R, Zachariah A, Singh R, Bloom G. Informal rural healthcare providers in North and South India. Health Policy Plan. 2014;29:i20–9. doi: 10.1093/heapol/czt050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George A, Iyer A. Unfree markets: socially embedded informal health providers in northern Karnataka, India. Soc Sci Med. 2013;96:297–304. doi: 10.1016/j.socscimed.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Sulis G, Daniels B, Kwan A, Gandra S, Daftary A, Das J, et al. Antibiotic overuse in the primary health care setting: A secondary data analysis of standardised patient studies from India, China and Kenya. BMJ Glob Health. 2020;5:e003393. doi: 10.1136/bmjgh-2020-003393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute of Health and Family Welfare, Government of India Report of the health survey and development committee. Available from: https://nihfw.ac.in/Doc/Reports/Bhore%20Committee%20Report%20-%20Vol%20II.pdf, accessed on March 2, 2024.
- 13.Agte P. Improving health outcomes through mid-level providers: Evidence from a large scale expansion of public primary healthcare in India. Available from: https://editorialexpress.com/cgi-bin/conference/download.cgi?db_name=NEUDC2023&paper_id=723, accessed on March 2, 2024.
- 14.Das S, Barnwal P. The need to train uncertified rural practitioners in India. J Int Med Res. 2018;46:522–5. doi: 10.1177/0300060517724948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Das J, Chowdhury A, Hussam R, Banerjee AV. The impact of training informal health care providers in India: A randomized controlled trial. Science. 2016;354:aaf7384. doi: 10.1126/science.aaf7384. [DOI] [PubMed] [Google Scholar]
- 16.Kaul R. Healthcare workers in West Bengal to undergo 9-month training. Hindustan Times. 2016. Oct 7, Available from: https://www.hindustantimes.com/india-news/healthcare-workers-in-west-bengal-to-undergo-9-month-training/story-CD6y0Lsvaxdl2CeiGR0UDI.html, accessed on November 5, 2017.
- 17.Centre for Policy Research Lessons from Covid Care Centres in West Bengal. Available from: https://cprindia.org/wp-content/uploads/2022/05/Working-Paper_Lessons-from-the-Covid-Care-Centers-in-West-Bengal_01-April-22_Revised-02.pdf, accessed on March 2, 2024.
- 18.Thapa P, Narasimhan P, Beek K, Hall JJ, Jayasuriya R, Mukherjee PS, et al. Unlocking the potential of informal healthcare providers in tuberculosis care: Insights from India. BMJ Glob Health. 2024;9:e015212. doi: 10.1136/bmjgh-2024-015212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das J, Hammer J, Leonard K. The quality of medical advice in low-income countries. J Econ Perspect. 2008;22:93–114. doi: 10.1257/jep.22.2.93. [DOI] [PubMed] [Google Scholar]
- 20.Mohanan M, Vera-Hernández M, Das V, Giardili S, Goldhaber-Fiebert JD, Rabin TL, et al. The know-do gap in quality of health care for childhood diarrhea and pneumonia in rural India. JAMA Pediatr. 2015;169:349–57. doi: 10.1001/jamapediatrics.2014.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Das J, Hammer J. Money for nothing: the dire straits of medical practice in Delhi, India. J Dev Econ. 2007;83:1–36. [Google Scholar]


