Abstract
In a global pandemic, the coronavirus has brought new challenges to reproductive and sexual health. This systematic review has been conducted with the aim of investigating a) the transmission of coronavirus disease 2019 (COVID-19) through female-to-male sexual secretions and vice versa, b) vertical transmission to the fetus, c) transmission to the newborn through the birth canal, and d) transmission through breast milk. In this review study, to find related articles, databases were searched using English and Persian keywords from the beginning of 2019 to the end of 2023. Based on the entry and exit criteria and the qualitative evaluation of the studies based on the STROBE criterion, the final studies were summarized. According to the initial search, 5970 articles were reviewed. After removing duplicate articles and the inappropriateness of the title, the abstract of the article was not related to the objectives of the project, there was no relevant study, and retrospective studies were excluded. Finally, 120 articles were selected as final articles. The general results show that transmission of the virus through the vagina to the blood of the fetus causing septicemia, vertical transmission from the mother to the fetus, transmission through the water bag, genital secretions, and ejaculate fluid are considered rare and ruled out. Transmission through rectal secretions during anal or oral sex requires more extensive studies. It is not possible to transmit the virus through breast milk. The long-term reproductive impact of COVID-19 on the reproductive systems of women and men is unclear.
Keywords: Birth canal, COVID-19, sexual health, sexual secretions, transmission, women
Introduction
The spread of the coronavirus disease 2019 (COVID-19) and deaths in more than 160 countries caused the declaration of an epidemic around the world.[1,2,3,4,5] Restrictions on access to family planning services, reduction in sexual relationships in the form of group sex relationships, reduction in sexual relationships among transsexuals, and the educational and communication gap between healthcare services and mother and child were the most important concerns during the COVID-19 era.[6] In different methods of sexual intercourse, having anal, oral, or combined sexual intercourse can cause the transmission of the virus during marital intercourse.[7,8,9] Rubin ES et al. 2020 shows that COVID-19 can be detected in the vulva;[10] however, it confirms the evidence of vaginal transmission of the virus and the role of the sexual route in the transmission of the disease.[11] The transmission of the virus in saliva and the rectum through oral and anal sex has also been reported during sexual intercourse.[12] In connection with the transmission of the virus from mother to baby, Ashraf et al.[13] (2020) raised the possibility of vertical transmission from mother to baby. Schwartz et al.[14] (2020) confirmed the presence of the coronavirus in vaginal secretions. Then, contradictory studies were reported about transmission from vaginal secretions.[15,16,17] Currently, the status of transmission of this virus through the reproductive system is still controversy regarding perinatal outcomes in infants, but vertical transmission of COVID-19 during vaginal delivery has been confirmed. Therefore, the possibility of contamination of the nasopharynx of the baby, possible infection of the baby, an increase in the rate of cesarean section, a lowering of the decision threshold for cesarean section,[18,19] an increase in the maternal and fetal outcomes of cesarean section, prematurity of the baby, and the need for neonate intensive care (NICU) admission and significant radiographic signs of the baby’s lungs can be expected.[20] Increasing the financial burden of treatment, increasing the duration of hospitalization,[3,19] and increasing perinatal complications (such as preeclampsia) are among the long-term consequences of COVID-19 transmission during pregnancy and childbirth.[19] The increase in the number of screening requests for sexually transmitted diseases and the increase in the number of questions about sexual transmission related to COVID-19 are among the most important issues related to the presence of the virus in vaginal fluid.[20,21,22,23] Considering the possibility of the spread of new strains of the virus in the future, the unpredictable pathogenic behavior of the virus, the performance of the health system in dealing with COVID-19, and the sixth position among the 15 determined and leveled ranks,[24] the researchers decided to consider a complete compilation of reliable information in this field in the continuation of the systematic review process.
Materials and Methods
The aim of this study was to investigate a) the transmission of COVID-19 through female-to-male sexual secretions and vice versa, b) vertical transmission to the fetus, c) transmission to the newborn through the birth canal, and d) transmission through breast milk. This article was put on the agenda as a review and in a systematic way. A systematic search of previous research in a purposeful and focused manner on a specific topic that is mentioned above is performed. In this regard, the combination and evaluation of research are performed using specific and predetermined criteria, which ultimately lead to the presentation of results. The method of searching in this study is performed using keywords related to the subject in several specific and valid databases. In such studies, quality filters are also applied in the selection of previous research studies. Also, sampling strategies, type of the study, study period, and their limitations are examined. The statistical population of this study includes published scientific articles that refer to the issue of transmission of COVID-19 through female-to-male sexual secretions and vice versa, vertical transmission to the fetus, transmission to the newborn through the birth canal, and transmission through breast milk. Protocol: This review study was conducted after approval by the research council and obtaining the ethical code approved by Islamic Azad University (ir.iau.ps.rec. 1400.199). This study was completed based on the protocols registered on the PROSPERO website with the code 251736, according to the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) format, and using the The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist. Search strategy: In this study, the following databases were used to find related studies in line with the goals of the project: Cochrane, IranMedx, Scientific Information Database (SID), PubMed, Google Scholar, Scopus, ScienceDirect, UpToDate, and Web of Science. Studies were reviewed from the beginning of the coronavirus epidemic 2019 until 2023 and based on the inclusion and exclusion criteria. The English keywords included sexual transmission, sexual, oral sex, rectal sex, Sexual Behavior, Sexual Partners, hetrosexual, Sexual Abstinence, Sexual Health, Sexual Maturation, Vagina, Vaginal Smears, Vaginal Discharge Vaginal, normal vaginal delivary, covid-19, corona virus, sars-covid-2, cesarean section, infant, baby, fetus, newborns, placenta, fetomaternal, transmition, breastfeeding, neonate intensive care (NICU), which were investigated by combining AND and OR. Selection of studies: The selection of studies was put on the agenda based on inclusion and exclusion criteria and relevance. The studies in Persian and English and the format of a full article were finally reviewed. Also, the list of sources used in all published articles in this field was checked. Study selection criteria are as follows: 1. studies that are in English and Farsi and have a full article format; 2. studies that have been conducted on sexual contact (heterosexual, oral sex, and rectal sex) transmission through semen and vaginal secretions; 3. studies that mention transmission through oral and anal sex; and 4. articles in the form of case reports and original research studies that have been refereed. Study exclusion criteria are as follows: 1. studies that do not get the corresponding points according to the checklists related to the meta-analysis of descriptive studies; 2. studies that are related to the infection of people with multiple partners; 3. texts presented in the form of letters to the head secretary, short articles, and articles presented in congresses and conferences. Excavating Information: According to the initial search, 5970 articles were reviewed, and after removing duplicate articles, 1018 articles were reviewed. Among them, 603 articles were removed due to the inappropriateness of the title. Then, 415 articles were analyzed. Twenty articles were excluded because the abstract of the article was not related to the objectives of the project, and 275 articles were excluded because they were not relevant. Finally, 120 articles were selected as final articles and entered the quality review stage [Figure A]. Checking the quality of studies: The information about the articles was prepared based on the checklist form and extracted and entered into Excel. To prevent bias, all the steps of extracting and checking the sources were performed by two authors independently of each other, and if the sources were rejected, the relevant reason was mentioned. In case of disagreement between two researchers, the review of the article was performed by a third person. In all stages of searching and using references, ethical principles were observed. Then, to obtain the data from the articles, data extraction worksheets were designed and adjusted in the form of eight indicators, and based on coding, each of the worksheets was completed by the researchers. The investigated indicators in each paper were article title, first author, type of the study, investigated variable, year of publication, demographic information related to each title, quality of the study, and final conclusion of the study. The quality of the studies was evaluated according to the checklist of descriptive studies in STROBE epidemiology. The revised checklist consists of 11 items, and a maximum of one point is assigned for each methodological element. The total quality score is finally 22. Scores of 16–22 are high quality, 15–8 are average quality, and less than 8 means low quality studies.[25] In this research, studies that had poor quality were deleted. After reviewing and comparing the worksheets specific to each of the extracted articles, the obtained data were compiled and the final description and analysis were performed based on the objectives of the project.
Figure A.
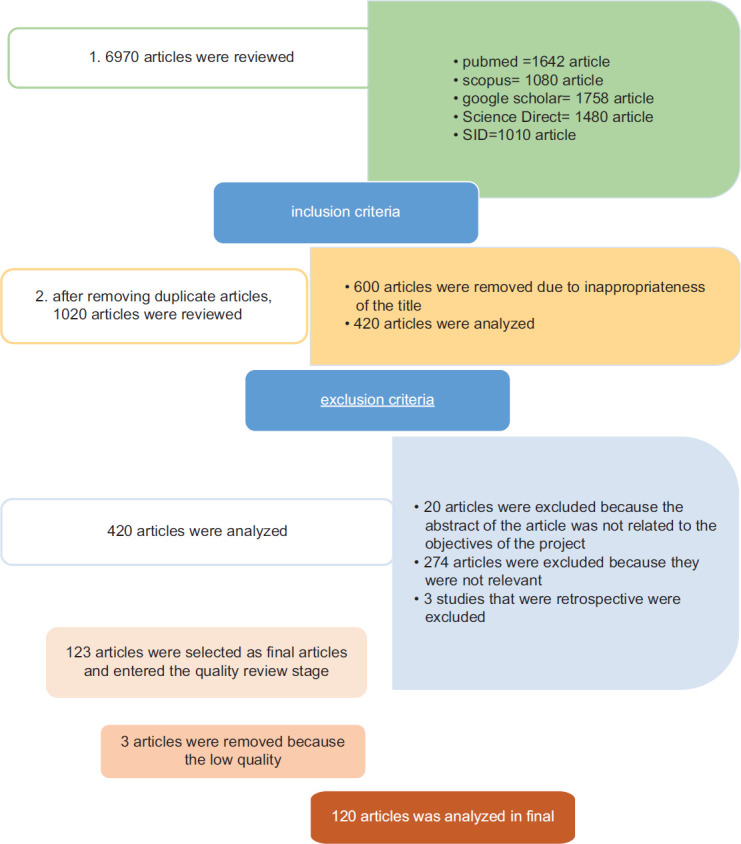
Study algorithm
Result
The following practical findings were presented in a classified manner with separate thematic axes. The aim of this study was to investigate a) the transmission of COVID-19 through female-to-male sexual secretions and vice versa, b) vertical transmission to the fetus, c) transmission to the newborn through the birth canal, and d) transmission through breast milk.
Discussion
Later studies related to the possibility of vertical transmission from mother to fetus were reported, some in favor and some in opposition. The COVID-19 pandemic has affected all aspects of reproductive and sexual health. The current review was conducted with a systematic review of 120 articles. Various studies related to the transmission of the virus through genital secretions concluded that droplets, contact, aerosol, and fecal–oral transmission are the main ways of transmitting the infection of COVID-19, and this initial finding was confirmed in all the primary articles.[135,136] In the future, due to the progress of the disease at a high speed and similar distribution in all parts of the world, the ability to detect COVID-19 in the lower genital tract of women will be noticed.[10,15,16,17,31,34,137] According to Tables 1 and 2 In this part, the researcher categorized and emphasized a the transmission of COVID-19 through female-to-male sexual secretions and vice versa. Other studies were designed in response to the transmission of COVID-19, among which the study of Rubin (2020) reported a pregnant woman infected with the virus who had vulvovaginal lesions and raised the possibility of transmission through these lesions.[10] In opposition to the above findings, other studies show that the SARS coronavirus 2 has been associated with oral and genital ulcers and describes a potential reactive dermatologic manifestation of COVID-19, but the transmission of the virus through an ulcer is not mentioned.[138,139] Later, sexual contact was proposed as a way to transmit Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and researchers sought to confirm or disconfirm the issue.[75] Kotlyar (2021) showed in their research that the rectal swap test is positive even after the nasopharynx is negative. This possibility has been raised in other studies as well.[140,141,142,143] In relation to the possibility of virus transmission through men’s semen, most of the studies showed the absence of virus transmission through ejaculate,[43,44,47,49,51,54] but Li (2020) showed in their study that there were positive results of SARS-CoV-2 in the semen of six patients (15.8%).[42] In this regard, Machado (2021) also found the virus in the semen of 6.66% of patients.[53] Some studies point to the short-term and long-term effects of COVID-19 on the male reproductive system, such as the effect of COVID-19 on the amount of male sex hormone secretions that were discussed in the study by Ling Ma et al. (2021).[46] Oligospermia, azoospermia, and sperm quality disorders have also been shown in Gacci et al. (2021).[52] Groner et al.[48] (2020) consider the effect of this virus on the reproductive system and reproductive health of men to be probable and suggest the need for more research. In favor of the result of this research, Nori and Salman (2023) reported that COVID-19 has a direct hematogenic spread to the testis and triggers the immunological response, which decreases sperm motility and counts[144] and changes the hormonal level, and the formation of antisperm antibodies is reported.[145,146] The other findings of this research are vaginal secretions that do not transmit the virus, but rectal secretions can be considered a route of transmission, which requires more extensive studies. Sexual contacts such as oral–anal contact play a role in the transmission of COVID-19. In favor of the above finding, even in Carosso A et al, (2020), the risk of virus transmission in feces during childbirth was mentioned.[68] Some of this result of the search is in favor and some is in opposition to each of the research aims. In this part, the researcher categorized and emphasized b) vertical transmission to the fetus. This research finding showed in Fornari’s[147] study (2020) that some children born to mothers infected with COVID-19 at the end of pregnancy and near the time of delivery tested positive for COVID-19, but there was no transmission. This issue has been confirmed in the studies of Yuan J et al. (2021) and Najafi, T. F et al. (2021).[148,149] Special attention is still being paid to the fact that women are not infected with COVID-19 at the time of trying to get pregnant and are not to be infected in the first trimester of pregnancy.[150] This is opposed to De Luca’s[151] (2023) study that mentions the possibility of transmission of COVID-19 via pregnancy. Although Goulioumis A et al.[152] (2022) have reported that the intrauterine infection remains controversial, anyway the expression of the ACE2 receptor on the placenta, the detection of IgM antibodies, and the COVID-19 genome in fetuses make the vertical transmission tenable. However, this article based on Hu X et al. (2020) showed in their findings that the vertical transmission of SARS-CoV-2 infection from mothers infected with COVID-19 in the last days of pregnancy is possible, but it is relatively low, and one baby of seven was infected (14.3%).[81] The findings of Sukhikh G et al.[95] (2021) showed that PCR and immunohistochemical analysis of placental tissue, umbilical cord blood, and child’s blood jointly showed vertical transmission of SARS-CoV-2 from mother to fetus. In connection with the possibility of vertical transmission of COVID-19, the review of 27 articles shows the absence of vertical transmission of this virus through the birth canal and amniotic sac from mother to fetus and newborn.[2,62,63,66,67,68,69,70,71,73,75,76,77,78,83,84,87,88,89,92,93,98,99,102,106,109] In favor of the above finding, Kim YK and Kim EH et al.[153] (2023) showed that vertical transmission in pregnancy (every trimester) is rare. This finding is consistent with that of Muhidin S et al.[154] (2020), who reported that although the rate of cesarean delivery, preterm delivery, simultaneous multi-organ involvement in the pregnant mother, and the chance of hospitalization in the intensive care unit increased, no vertical transmission from mother to baby was reported. However, in this research, Zamaniyan M et al.[114] (2023) showed that the high risk of maternal and neonatal outcomes of COVID-19 during pregnancy and the high probability of vertical transmission were seen. This report is consistent with the study by Melo GCd, and Araújo KCGMd[74] (2020) that showed that of 432 newborns born to mothers infected with COVID-19, 10 cases had positive results for primary SARS-CoV-2. Also, some reports indicated the vertical transmission of SARS-CoV-2 to newborns. The other studies, such as Alzamora MC et al. (2020), reported a severe case of COVID-19 that was delivered by cesarean section, the baby was immediately separated, and the baby’s PCR test was positive.[80] Some of this result in this search are in favor and some are in opposition to each of the research aims. In this part, the researcher had categorized and emphasized c) transmission to the newborn through the birth canal. Zimmermann P and Curtis N[79] (2020), by reviewing 11 articles and examining 333 babies, completely reject the possibility of virus transmission from vaginal secretions to the baby’s blood causing septicemia. In vaginal secretions, COVID-19 has rarely been seen. In the study by Wu et al.[17] in 2020, during further tests and investigations of mothers with COVID-19 and their babies, transmission to the baby through secretions of the birth canal was ruled out. In this regard, studies were conducted on the possible effect of elective cesarean delivery on reducing transmission through birth canal secretions and improving neonatal outcomes, but the elective cesarean section was not recommended in patients with COVID-19.[106] In the same way as this research finding, Yanting Wu et al.[155] (2020) suggested that vaginal delivery can be safe, and it does not seem that virus contamination happens through the vaginal secretion. Some of this result of the search is in favor and some is in opposition to each of the research aims. In this part, the researcher had categorized and emphasized d) transmission through breast milk.[81,147] Transmission through breast milk was investigated, and no transmission was seen. It seems that the nursing mother infected with COVID-19 infects the baby through her respiratory droplets, rather than the virus being transmitted through breast milk.[116,120,121,122,123,125,126,127,128] However, vaccination during the breastfeeding period cannot cause serious complications for the baby.[156,157] However, inter-departmental transfer of pregnant mothers or transferring them to other related departments for continuing care is associated with an increase in the possibility of contact between pregnant mothers, nursing mothers, and babies with the virus. Therefore, it is recommended to consider this issue in midwifery care.[154,158,159,160,161,162] The results of this study are in line with the results of Koç and Dilli[163] (2022) who highly advise breastfeeding while using proper infection control methods. The most important limitation of the plan was not having sufficient information or studies in the field of all aspects of the transmission of COVID-19 due to its emerging nature. Another limitation of this study was not mentioning the detailed research information in the selected articles. Cohort studies in this field did not exist at the beginning of the researchers’ work, and if they existed, they would have provided the possibility of more powerful arguments. The information obtained from the articles is generally retrospective in nature, and the researchers hope that this research will pave the way for future research in the field of emerging diseases.
Table 1.
Frequency distribution of articles according to the topic and objectives of the study
| Row | Purpose | Abundance | Percentage | |
|---|---|---|---|---|
| 1 | The relationship between the transmission of COVID-19 through vaginal secretions | 23 | 19.16 | |
| 2 | Correlation between transmission of COVID-19 through ejaculate | 19 | 15.83 | |
| 3 | The relationship between vertical transmission of COVID-19 around and around childbirth through the birth canal | 57 | 47.5 | |
| 4 | Transmission of COVID-19 through genital secretions and umbilical cord blood | 0 | 0/0 | |
| 5 | Transmission of COVID-19 through vaginal secretions to the baby’s blood | 1 | 0.83 | |
| 6 | Transmission of COVID-19 through breast milk | 20 | 16.66 | |
| 7 | Total | 120 articles | 100/0 | |
|
Type of study | ||||
|
The reviewed articles have been published between 2019 and 2023
| ||||
| 10 prospective studies | 5 observational studies | |||
| 7 retrospective studies | 26 review studies | |||
| 3 systematic review studies and meta-analysis | 9 experimental studies | |||
| 2 clinical trials | 18 case report studies and 4 case series | |||
| 2 case–control studies | 12 cross-sectional studies | |||
| 3 case reports and reviews | 7 cohort studies | |||
| 1 narrative review | 15 systematic review studies | |||
|
Quality of studies | ||||
| 11 studies had excellent quality | 109 studies had average quality | Studies that had poor quality are deleted | ||
Table 2.
Determining all of the types of transmission of COVID-19
Conclusion
The results of this systematic review study, which was conducted with the aim of investigating the mode of transmission of COVID-19 through sexual secretions and the birth canal, showed that COVID-19 is not transmitted through vaginal secretions or ejaculate, but rectal secretions can be considered a route of transmission, which requires more extensive studies. Oral–anal sexual relations have played a vague role in the transmission of COVID-19 and have been reported in the form of uncertainty. Reproductive outcomes, including male sex hormone secretion disorders, oligospermia and azoospermia, and sperm quality, have been mentioned in studies. However, the viral attack on women’s reproductive system and other direct and indirect effects on men’s reproductive system in the long term are unclear and require a more comprehensive investigation. It is not possible to transfer COVID-19 from vaginal secretions to the baby’s blood and cause septicemia, vertical transmission, transmission through the birth canal and water sac, and transmission through the flow of breast milk, but there is a need for a more comprehensive investigation regarding the risk of transmission through contaminated feces to the baby during the delivery process. The most important limitations of the study were not having enough information or studies on all aspects of the transmission of COVID-19, not mentioning detailed research information in the selected articles, and lack of cohort studies on the aspects investigated by the researchers. According to the results of the research, it is necessary to put all-round investigations in the field of possible ways of disease transmission and public education about definite ways of transmission on the agenda of healthcare workers.
Financial support and sponsorship
The research budget is provided from the income of Islamic Azad University—Maybod Branch.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The Research Council of Islamic Azad University—Maybod Branch—as the financial sponsor of the research (project code: 162432738, ethical code: IR.IAU.REC.1400.199) and the respected officials of the research field of Islamic Azad University—Yazd Branch—are hereby thanked for their special cooperation in obtaining the code of ethics.
References
- 1.Lu C-W, Liu X-F, Jia Z-F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet (London, England) 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. doi: 10.1016/S0140-6736 (20) 30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020;395:809–15. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14:779–88. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tahmineh F. Letter to the Editor: Sexual and Reproductive Health Rights and Challenges of Covid 19 Diagnosis. Medical Ethics [Internet] 2021;15:0–0. Available from: https://sid.ir/paper/1019421/en . [Google Scholar]
- 5.Hamzehgardeshi Z, Yazdani F, Rezaei M, Kiani Z. COVID-19 as a threat to sexual and reproductive health. Iran J Public Health. 2020;49(Suppl 1):136. doi: 10.18502/ijph.v49iS1.3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolarinwa OA, Ahinkorah BO, Seidu A-A, Ameyaw EK, Saeed BQ, Hagan JE, Jr, et al. Mapping evidence of impacts of COVID-19 outbreak on sexual and reproductive health: A scoping review. Healthcare. 2021;9:436. doi: 10.3390/healthcare9040436. doi: 10.3390/healthcare9040436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ding S, Liang TJ. Is SARS-CoV-2 also an enteric pathogen with potential fecal–oral transmission? A COVID-19 virological and clinical review. Gastroenterology. 2020;159:53–61. doi: 10.1053/j.gastro.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabello F, Sánchez F, Farré JM, Montejo AL. Consensus on recommendations for safe sexual activity during the COVID-19 coronavirus pandemic. J Clin Med. 2020;9:2297. doi: 10.3390/jcm9072297. doi: 10.3390/jcm9072297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blackwell CW. Reducing sexually associated transmission of COVID-19 in men who have sex with men. J Am Assoc Nurse Pract. 2021;33:1050–4. doi: 10.1097/JXX.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 10.Rubin ES, Sansone SA, Hirshberg A, Clement EG, Srinivas SK. Detection of COVID-19 in a vulvar lesion. Am J Perinatol. 2020;37:1183. doi: 10.1055/s-0040-1713665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gagneur A, Dirson E, Audebert S, Vallet S, Legrand-Quillien M, Laurent Y, et al. Materno-fetal transmission of human coronaviruses: A prospective pilot study. Eur J Clin Microbiol Infect Dis. 2008;27:863–6. doi: 10.1007/s10096-008-0505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patrì A, Gallo L, Guarino M, Fabbrocini G. Sexual transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A new possible route of infection? J Am Acad Dermatol. 2020;82:e227. doi: 10.1016/j.jaad.2020.03.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashraf MA, Keshavarz P, Hosseinpour P, Erfani A, Roshanshad A, Pourdast A, et al. Coronavirus disease 2019 (COVID-19): A systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020;21:157–68. [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz A, Yogev Y, Zilberman A, Alpern S, Many A, Yousovich R, et al. Detection of SARS-CoV-2 in Vaginal Swabs of Women with Acute SARS-CoV-2 Infection. Available from SSRN: https://ssrn.com/abstract=3671438. or http://dx.doi.org/10.2139/ssrn.3671438. [DOI] [PMC free article] [PubMed]
- 15.Cui P, Chen Z, Wang T, Dai J, Zhang J, Ding T, et al. Clinical features and sexual transmission potential of SARS-CoV-2 infected female patients: A descriptive study in Wuhan, China. MedRxiv. 2020 doi: 10.1101/2020.02.26.20028225. [Google Scholar]
- 16.Aslan MM, Yuvacı HU, Köse O, Toptan H, Akdemir N, Köroğlu M, et al. SARS-CoV-2 is not present in the vaginal fluid of pregnant women with COVID-19, The Journal of Maternal-Fetal & Neonatal Medicine. 2020 doi: 10.1080/14767058.2020.1793318. DOI: 10.1080/14767058.2020.1793318. [DOI] [PubMed] [Google Scholar]
- 17.Wu Y, Liu C, Dong L, Zhang C, Chen Y, Liu J, et al. Coronavirus disease 2019 among pregnant Chinese women: Case series data on the safety of vaginal birth and breastfeeding. BJOG. 2020;127:1109–15. doi: 10.1111/1471-0528.16276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaterian N, Abdi F. Is cesarean section a safe delivery method to prevent mother to child transmission of SARS-CoV-2? Tehran Univ Med J TUMS Publications. 2020;78:337–8. [Google Scholar]
- 19.Mor N. New Delhi: Ministry of Health and Family Welfare; 2020. Resources for primary care providers to meet patients needs during the COVID-19 epidemic. [Google Scholar]
- 20.Tamimi H, Tahmasebi R, Darabi AH, Noroozi A. The predictive role of vaccine literacy and vaccine hesitancy on acceptance of COVID-19 vaccination. ISMJ. 2021;24:597–609. [Google Scholar]
- 21.Hashem NM, Abdelnour SA, Alhimaidi AR, Swelum AA. Potential impacts of COVID-19 on reproductive health: Scientific findings and social dimension. Saudi Journal of Biological Sciences. 2021;28:1702–12. doi: 10.1016/j.sjbs.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saghafipour A. What are the barriers to Covid-19 vaccination coverage?(Commentary) Payesh (Health Monitor) 2022;21:321–3. [Google Scholar]
- 23.Mosadeghrad AH. Promote COVID-19 vaccination uptake: A letter to editor. Tehran Univ Med J TUMS Publications. 2022;80:159–60. [Google Scholar]
- 24.Sadrmomtaz N, Khedmati M, Babaei A. Evaluation of the performance of world countries’ health systems in the face of Covid-19 in respect of vaccination role. Depiction Health. 2022;13:33–47. [Google Scholar]
- 25.Aitken RJ. COVID-19 and human spermatozoa—Potential risks for infertility and sexual transmission? Andrology. 2021;9:48–52. doi: 10.1111/andr.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tatu A, Nadasdy T, Nwabudike L. Observations about sexual and other routes of SARS-CoV-2 (COVID-19) transmission and its prevention. Clin Exp Dermatol. 2020;45:761–2. doi: 10.1111/ced.14274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qiu L, Liu X, Xiao M, Xie J, Cao W, Liu Z, et al. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis. 2020;71:813–7. doi: 10.1093/cid/ciaa375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohseni AH, Taghinezhad-S S, Xu Z, Fu X. Body fluids may contribute to human-to-human transmission of severe acute respiratory syndrome coronavirus 2: Evidence and practical experience. Chin Med. 2020;15:1–4. doi: 10.1186/s13020-020-00337-7. doi: 10.1186/s13020-020-00337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cui P, Chen Z, Wang T, Dai J, Zhang J, Ding T, et al. Severe acute respiratory syndrome coronavirus 2 detection in the female lower genital tract. Am J Obstet Gynecol. 2020;223:131–4. doi: 10.1016/j.ajog.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmad MF, Mahakkanukrauh P, Das S. The detection of SARS-CoV-2 virus in the vaginal fluid of females with severe COVID-19 infection: Scientific facts. Clin Infect Dis. 2022;74:2262–3. doi: 10.1093/cid/ciaa1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lowe B, Bopp B. COVID-19 vaginal delivery–a case report. Aust N Z J Obstet Gynaecol. 2020;60:465–6. doi: 10.1111/ajo.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carosso AR, Cosma S, Benedetto C. Vaginal delivery in COVID-19 pregnant women: Anorectum as a potential alternative route of SARS-CoV-2 transmission. Am J Obstet Gynecol. 2020;223:612. doi: 10.1016/j.ajog.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khoiwal K, Kalita D, Shankar R, Kumari R, Dhundi D, Bahadur A, et al. Identification of SARS-CoV-2 in the vaginal fluid and cervical exfoliated cells of women with active COVID-19 infection: A pilot study. Int J Gynecol Obstet. 2021;153:551–3. doi: 10.1002/ijgo.13671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuvacı HU, Aslan MM, Köse O, Akdemir N, Toptan H, Cevrioğlu AS, et al. Evaluation of the presence of SARS-COV-2 in the vaginal fluid of reproductive-aged women. Ginekologia Polska. 2021;92:406–9. doi: 10.5603/GP.a2021.0018. [DOI] [PubMed] [Google Scholar]
- 35.Barber E, Kovo M, Leytes S, Sagiv R, Weiner E, Schwartz O, et al. Evaluation of SARS-CoV-2 in the vaginal secretions of women with COVID-19: A prospective study. J Clin Med. 2021;10:2735. doi: 10.3390/jcm10122735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agarwal M, Basumatary S, Bhusan D, Pati BK. Detection of severe acute respiratory syndrome corona virus 2 in cervico-vaginal secretion of COVID-19-affected female: A prospective observational study from India. SAGE Open Med. 2021;9:20503121211022993. doi: 10.1177/20503121211022993. doi: 10.1177/20503121211022993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atarod Z, Zamaniyan M, Moosazadeh M, Valadan R, Soleimanirad SM, Gordani N. Investigation of vaginal and rectal swabs of women infected with COVID-19 in two hospitals covered by Mazandaran University of Medical Sciences, 2020. J Obstet Gynaecol. 2022;42:2225–9. doi: 10.1080/01443615.2022.2036966. [DOI] [PubMed] [Google Scholar]
- 38.Erdem D, Kayaaslan B, Cakir EY, Dinc B, Asilturk D, Kirca F, et al. Investigation of SARS-CoV-2 using RT-PCR in vaginal swab samples of female patients with a diagnosis of severe COVID-19. Taiwan J Obstet Gynecol. 2023;62:270–4. doi: 10.1016/j.tjog.2022.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta P, Choudhary A, Srigyan D, Malhotra N. SARS-CoV-2 is not detectable in cervicovaginal secretions from women with active COVID-19 infection-a pilot study. JBRA Assist Reprod. 2023;27:1–3. doi: 10.5935/1518-0557.20210103. doi: 10.5935/1518-0557.20210103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khoiwal K, Kalita D, Kumari R, Dhundi D, Shankar R, Kumari R, et al. Presence of SARS-CoV-2 in the lower genital tract of women with active COVID-19 infection: A prospective study. Int J Gynaecol Obst. 2022;157:744–7. doi: 10.1002/ijgo.14153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Cillo PEC, Lafraia FM, de Souza Bonetti TC, Saldanha MG, Reis N, Sartori MGF, et al. Cross-Sectional study confirms absence of viral RNA in vaginal secretion of SARS-COV-2 infected women. AJOG Glob Rep. 2023;3:100200. doi: 10.1016/j.xagr.2023.100200. doi: 10.1016/j.xagr. 2023.100200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li D, Jin M, Bao P, Zhao W, Zhang S. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open. 2020;3:e208292. doi: 10.1001/jamanetworkopen.2020.8292. doi: 10.1001/jamanetworkopen. 2020.8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Song C, Wang Y, Li W, Hu B, Chen G, Xia P, et al. Absence of 2019 novel coronavirus in semen and testes of COVID-19 patients. Biol Reprod. 2020;103:4–6. doi: 10.1093/biolre/ioaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pan F, Xiao X, Guo J, Song Y, Li H, Patel DP, et al. No evidence of severe acute respiratory syndrome–coronavirus 2 in semen of males recovering from coronavirus disease 2019. Fertil Steril. 2020;113:1135–9. doi: 10.1016/j.fertnstert.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo L, Zhao S, Li W, Wang Y, Li L, Jiang S, et al. Absence of SARS-CoV-2 in semen of a COVID-19 patient cohort. Andrology. 2021;9:42–7. doi: 10.1111/andr.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma L, Xie W, Li D, Shi L, Ye G, Mao Y, et al. Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients. J Med Virol. 2021;93:456–62. doi: 10.1002/jmv.26259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruan Y, Hu B, Liu Z, Liu K, Jiang H, Li H, et al. No detection of SARS-CoV-2 from urine, expressed prostatic secretions, and semen in 74 recovered COVID-19 male patients: A perspective and urogenital evaluation. Andrology. 2021;9:99–106. doi: 10.1111/andr.12939. [DOI] [PubMed] [Google Scholar]
- 48.Gröner MF, Carvalho RCd, Camillo J, Ferreira PRA, Fraietta R. Effects of Covid-19 on male reproductive system. Int Braz J Urol. 2020;47:185–90. doi: 10.1590/S1677-5538.IBJU.2021.99.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Holtmann N, Edimiris P, Andree M, Doehmen C, Baston-Buest D, Adams O, et al. Assessment of SARS-CoV-2 in human semen—A cohort study. Fertil Steril. 2020;114:233–8. doi: 10.1016/j.fertnstert.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paoli D, Pallotti F, Turriziani O, Mazzuti L, Antonelli G, Lenzi A, et al. SARS-CoV-2 presence in seminal fluid: Myth or reality. Andrology. 2021;9:23–6. doi: 10.1111/andr.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kayaaslan B, Korukluoglu G, Hasanoglu I, Kalem AK, Eser F, Akinci E, et al. Investigation of SARS-CoV-2 in semen of patients in the acute stage of COVID-19 infection. Urol Int. 2020;104:678–83. doi: 10.1159/000510531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gacci M, Coppi M, Baldi E, Sebastianelli A, Zaccaro C, Morselli S, et al. Semen impairment and occurrence of SARS-CoV-2 virus in semen after recovery from COVID-19. Hum Reprod. 2021;36:1520–9. doi: 10.1093/humrep/deab026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Machado B, Barcelos Barra G, Scherzer N, Massey J, dos Santos Luz H, Henrique Jacomo R, et al. Presence of SARS-CoV-2 RNA in semen—cohort study in the United States COVID-19 positive patients. Infect Dis Rep. 2021;13:96–101. doi: 10.3390/idr13010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Temiz MZ, Dincer MM, Hacibey I, Yazar RO, Celik C, Kucuk SH, et al. Investigation of SARS-CoV-2 in semen samples and the effects of COVID-19 on male sexual health by using semen analysis and serum male hormone profile: A cross-sectional, pilot study. Andrologia. 2021;53:e13912. doi: 10.1111/and.13912. doi: 10.1111/and. 13912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gupta P, Choudhary A, Gopal G, Kumar R, Kumar A, Tiwari P, et al. Detection of SARS-CoV2 virus using the real-time reverse transcriptase polymerase chain reaction in semen and seminal plasma from men with active COVID-19 infection–A pilot study. Indian J Urol. 2021;37:331–4. doi: 10.4103/iju.iju_117_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang C, Zhou S-F, Gao L-D, Li S-K, Cheng Y, Zhou W-J, et al. Risks associated with cryopreserved semen in a human sperm bank during and after the COVID-19 pandemic. Reprod BioMed Online. 2021;42:589–94. doi: 10.1016/j.rbmo.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pavone C, Giammanco GM, Cascino AP, Baiamonte D, Pinelli M, Cangelosi E, et al. Assessment of SARS-CoV-2 RNA shedding in semen of 36 males with symptomatic, asymptomatic, and convalescent infection during the first and second wave of COVID-19 pandemic in Italy. Asian J Androl. 2022;24:135–8. doi: 10.4103/aja2021103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Delaroche L, Bertine M, Oger P, Descamps D, Damond F, Genauzeau E, et al. Evaluation of SARS-CoV-2 in semen, seminal plasma, and spermatozoa pellet of COVID-19 patients in the acute stage of infection. PLoS One. 2021;16:e0260187. doi: 10.1371/journal.pone.0260187. doi: 10.1371/journal.pone. 0260187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Donders GG, Bosmans E, Reumers J, Donders F, Jonckheere J, Salembier G, et al. Sperm quality and absence of SARS-CoV-2 RNA in semen after COVID-19 infection: A prospective, observational study and validation of the SpermCOVID test. Fertil Steril. 2022;117:287–96. doi: 10.1016/j.fertnstert.2021.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Huang Z, Do DV, Beh D, Lee CK, Yan B, Foo R, et al. Effects of acute severe acute respiratory syndrome coronavirus 2 infection on male hormone profile, ACE2 and TMPRSS2 expression, and potential for transmission of severe acute respiratory syndrome coronavirus 2 in semen of Asian men. F S Sci. 2022;3:29–34. doi: 10.1016/j.xfss.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dong L, Tian J, He S, Zhu C, Wang J, Liu C, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846–8. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu W, Wang Q, Zhang Q, Chen L, Chen J, Zhang B, et al. Coronavirus disease 2019 (COVID-19) during pregnancy: A case series. 2020 [Google Scholar]
- 63.Elshafeey F, Magdi R, Hindi N, Elshebiny M, Farrag N, Mahdy S, et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int J Gynecol Obstet. 2020;150:47–52. doi: 10.1002/ijgo.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rozycki HJ, Kotecha S. Covid-19 in pregnant women and babies: What pediatricians need to know. Paediatr Respir Rev. 2020;35:31–7. doi: 10.1016/j.prrv.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Trippella G, Ciarcià M, Ferrari M, Buzzatti C, Maccora I, Azzari C, et al. COVID-19 in pregnant women and neonates: A systematic review of the literature with quality assessment of the studies. Pathogens. 2020;9:485. doi: 10.3390/pathogens9060485. doi: 10.3390/pathogens9060485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: Maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020;144:799–805. doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 67.Mullins E, Evans D, Viner R, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: Rapid review. Ultrasound Obstet Gynecol. 2020;55:586–92. doi: 10.1002/uog.22014. [DOI] [PubMed] [Google Scholar]
- 68.Carosso A, Cosma S, Serafini P, Benedetto C, Mahmood T. How to reduce the potential risk of vertical transmission of SARS-CoV-2 during vaginal delivery? Eur J Obstet Gynecol Reprod Biol. 2020;250:246–9. doi: 10.1016/j.ejogrb.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, et al. Infants born to mothers with a new coronavirus (COVID-19) Front Pediatr. 2020;8:104. doi: 10.3389/fped.2020.00104. doi: 10.3389/fped. 2020.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, et al. Maternal and neonatal outcomes of pregnant women with coronavirus disease 2019 (COVID-19) pneumonia: A case-control study. Clin Infect Dis. 2020;71:2035–41. doi: 10.1093/cid/ciaa352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cao D, Chen M, Peng M, Yin H, Sun G. Vaginal delivery in women with COVID-19: Report of two cases. BMC Pregnancy Childbirth. 2020;20:1–6. doi: 10.1186/s12884-020-03281-4. doi: 10.1186/s12884-020-03281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwartz DA, Graham AL. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12:194. doi: 10.3390/v12020194. doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Duran P, Berman S, Niermeyer S, Jaenisch T, Forster T, Gomez Ponce de Leon R, et al. COVID-19 and newborn health: Systematic review. Rev Panam Salud Pública. 2020;44:e54. doi: 10.26633/RPSP.2020.54. doi: 10.26633/RPSP. 2020.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Melo GCd, Araújo KCGMd. COVID-19 infection in pregnant women, preterm delivery, birth weight, and vertical transmission: A systematic review and meta-analysis. Cad Saude Publica. 2020;36:e00087320. doi: 10.1590/0102-311x00087320. doi: 10.1590/0102-311×00087320. [DOI] [PubMed] [Google Scholar]
- 75.Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: Systematic review. Ultrasound Obstet Gynecol. 2020;56:15–27. doi: 10.1002/uog.22088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ahmed FT, Jabbar S. Neonatal outcomes and vertical transmission in Covid-19 infected pregnant women; a systematic review. J Glob Trends Pharm Sci. 2020;11:8589–95. [Google Scholar]
- 77.Pettirosso E, Giles M, Cole S, Rees M. COVID-19 and pregnancy: A review of clinical characteristics, obstetric outcomes and vertical transmission. Aust N Z J Obstet Gynaecol. 2020;60:640–59. doi: 10.1111/ajo.13204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marim F, Karadogan D, Eyuboglu TS, Emiralioglu N, Gurkan CG, Toreyin ZN, et al. Lessons learned so far from the pandemic: A review on pregnants and neonates with COVID-19. Eurasian J Med. 2020;52:202. doi: 10.5152/eurasianjmed.2020.20118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zimmermann P, Curtis N. COVID-19 in children, pregnancy and neonates: A review of epidemiologic and clinical features. Pediatr Infect Dis J. 2020;39:469–77. doi: 10.1097/INF.0000000000002700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020;37:861–5. doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hu X, Gao J, Luo X, Feng L, Liu W, Chen J, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vertical transmission in neonates born to mothers with coronavirus disease 2019 (COVID-19) pneumonia. Obstet Gynecol. 2020;136:65–7. doi: 10.1097/AOG.0000000000003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sheth S, Shah N, Bhandari V. Outcomes in COVID-19 positive neonates and possibility of viral vertical transmission: A narrative review. Am J Perinatol. 2020;37:1208–16. doi: 10.1055/s-0040-1714719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dumitriu D, Emeruwa UN, Hanft E, Liao GV, Ludwig E, Walzer L, et al. Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York City. JAMA Pediatr. 2021;175:157–67. doi: 10.1001/jamapediatrics.2020.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Joma M, Fovet C-M, Seddiki N, Gressens P, Laforge M. COVID-19 and pregnancy: Vertical transmission and inflammation impact on newborns. Vaccines. 2021;9:391. doi: 10.3390/vaccines9040391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.He Z, Fang Y, Zuo Q, Huang X, Lei Y, Ren X, et al. Vertical transmission and kidney damage in newborns whose mothers had coronavirus disease 2019 during pregnancy. Int J Antimicrob Agents. 2021;57:106260. doi: 10.1016/j.ijantimicag.2020.106260. doi: 10.1016/j.ijantimicag. 2020.106260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Farhadi R, Mehrpisheh S, Ghaffari V, Haghshenas M, Ebadi A. Clinical course, radiological findings and late outcome in preterm infant with suspected vertical transmission born to a mother with severe COVID-19 pneumonia: A case report. J Med Case Rep. 2021;15:1–5. doi: 10.1186/s13256-021-02835-0. doi: 10.1186/s13256-021-02835-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Palalioglu RM, Mahammadaliyeva A, Erbiyik HI, Muhcu M. COVID-19 in third trimester may not be as scary as you think, it can be innocent: Evaluating vertical transmission from a COVID-19 positive asymptomatic pregnant woman with early membrane rupture. J Obstet Gynaecol Res. 2021;47:838–42. doi: 10.1111/jog.14584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jing H, Ackerman IV WE, Zhao G, El Helou Y, Buhimschi CS, Buhimschi IA. Connecting the dots on vertical transmission of SARS-CoV-2 using protein-protein interaction network analysis–potential roles of placental ACE2 and ENDOU. Placenta. 2021;104:16–9. doi: 10.1016/j.placenta.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kumari K, Yadav R, Mittra S, Kumar A, Singh J, Bajpai PK, et al. Pregnancy consequences and vertical transmission potential of SARS-CoV-2 infection: Seeking answers from a preliminary observation. J Reprod Infertil. 2021;22:144. doi: 10.18502/jri.v22i2.5804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Douglass KM, Strobel KM, Richley M, Mok T, de St Maurice A, Fajardo V, et al. Maternal-neonatal dyad outcomes of maternal COVID-19 requiring extracorporeal membrane support: A case series. Am J Perinatol. 2021;38:82–7. doi: 10.1055/s-0040-1718694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rabiei M, Soori T, Abiri A, Farsi Z, Shizarpour A, Pirjani R. Maternal and fetal effects of COVID-19 virus on a complicated triplet pregnancy: A case report. J Med Case Rep. 2021;15:1–4. doi: 10.1186/s13256-020-02643-y. doi: 10.1186/s13256-020-02643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Abdelazim IA, AbuFaza M, Al-Munaifi S. COVID-19 positive woman presented with preterm labor: Case report. Gynecol Obstet Reprod Med. 2021;27:294–6. [Google Scholar]
- 93.Pereira PCADA, Rodrigues DND, Rodrigues AMDS, Ferreira TM, Coelho BM, Do Nascimento MD, et al. Preventive measures against COVID-19 in pregnancy and neonates. J Young Pharm. 2021;13:31. [Google Scholar]
- 94.Oncel MY, Akın IM, Kanburoglu MK, Tayman C, Coskun S, Narter F, et al. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with COVID-19 by Turkish Neonatal Society. Eur J Pediatr. 2021;180:733–42. doi: 10.1007/s00431-020-03767-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sukhikh G, Petrova U, Prikhodko A, Starodubtseva N, Chingin K, Chen H, et al. Vertical transmission of SARS-CoV-2 in second trimester associated with severe neonatal pathology. Viruses. 2021;13:447. doi: 10.3390/v13030447. doi: 10.3390/v13030447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Goh XL, Low YF, Ng CH, Amin Z, Ng YPM. Incidence of SARS-CoV-2 vertical transmission: A meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2021;106:112–3. doi: 10.1136/archdischild-2020-319791. [DOI] [PubMed] [Google Scholar]
- 97.Thapa B, Acharya S, Karki S. Vertical transmission of COVID-19: A case report and review of literature. J Nepal Health Res Counc. 2021;19:203–5. doi: 10.33314/jnhrc.v19i1.3312. [DOI] [PubMed] [Google Scholar]
- 98.Elósegui JH, García AC, Risquez AF, Quintana MB, Montes JE. Does the maternal-fetal transmission of SARS-CoV-2 occur during pregnancy? Revista Clínica Española (English Edition) 2021;221:93–6. doi: 10.1016/j.rceng.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Paramanathan S, Kyng K, Laursen A, Jensen L, Grejs A, Jain D. COVID-19 with severe acute respiratory distress in a pregnant woman leading to preterm caesarean section: A case report. Case Rep Womens Health. 2021;30:e00304. doi: 10.1016/j.crwh.2021.e00304. doi: 10.1016/j.crwh. 2021.e00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tolu LB, Ezeh A, Feyissa GT. Vertical transmission of severe acute respiratory syndrome coronavirus 2: A scoping review. PloS One. 2021;16:e0250196. doi: 10.1371/journal.pone.0250196. doi: 10.1371/journal.pone. 0250196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Carbayo-Jiménez T, Carrasco-Colom J, Epalza C, Folgueira D, Pérez-Rivilla A, Barbero-Casado P, et al. Severe acute respiratory syndrome coronavirus 2 vertical transmission from an asymptomatic mother. Pediatr Infect Dis J. 2021;40:e115–7. doi: 10.1097/INF.0000000000003028. [DOI] [PubMed] [Google Scholar]
- 102.Xiong X, Wei H, Zhang Z, Chang J, Ma X, Gao X, et al. Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19. J Med Virol. 2020;92:1657–9. doi: 10.1002/jmv.25857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sheikhahmadi S, Behzadi S, Zakaryaei F. Evaluating vertical transmission of COVID-19 from mothers to neonates: An iranian case series of 8 patients. Arch Iran Med. 2021;24:405–8. doi: 10.34172/aim.2021.58. [DOI] [PubMed] [Google Scholar]
- 104.Al Asadi J, Mousa SM. Intrauterine vertical transmission of COVID-19 during pregnancy: A systematic review. The Medical Journal of Basrah University. 2021;39:7–20. [Google Scholar]
- 105.Sharma R, Seth S, Sharma R, Yadav S, Mishra P, Mukhopadhyay S. Perinatal outcome and possible vertical transmission of coronavirus disease 2019: Experience from North India. Clin Exp Pediatr. 2021;64:239. doi: 10.3345/cep.2020.01704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cai J, Tang M, Gao Y, Zhang H, Yang Y, Zhang D, et al. Cesarean section or vaginal delivery to prevent possible vertical transmission from a pregnant mother confirmed with COVID-19 to a neonate: A systematic review. Front Med. 2021;8:634949. doi: 10.3389/fmed.2021.634949. doi: 10.3389/fmed. 2021.634949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mendoza-Hernández M, Huerta-Niño de Rivera I, Yoldi-Negrete M, Saviñon-Tejeda P, Franco-Cendejas R, López-Jácome LE, et al. Probable case of vertical transmission of SARS-CoV-2 in a newborn in Mexico. Neonatology. 2021;118:364–7. doi: 10.1159/000514710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Maeda MdFY, Brizot MdL, Gibelli MABC, Ibidi SM, Carvalho WBd, Hoshida MS, et al. Vertical transmission of SARS-CoV2 during pregnancy: A high-risk cohort. Prenatal Diagn. 2021;41:998–1008. doi: 10.1002/pd.5980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chaichian S, Mehdizadehkashi A, Mirgaloybayat S, Hashemi N, Farzaneh F, Derakhshan R, et al. Maternal and fetal outcomes of pregnant women infected with coronavirus based on tracking the results of 90-days data in Hazrat-E-Rasoul Akram Hospital, Iran University of Medical Sciences. Bull Emerg Trauma. 2021;9:145. doi: 10.30476/BEAT.2021.90434.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sinaci S, Ocal DF, Seven B, Anuk AT, Besimoglu B, Keven MC, et al. Vertical transmission of SARS-CoV-2: A prospective cross-sectional study from a tertiary center. J Med Virol. 2021;93:5864–72. doi: 10.1002/jmv.27128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lopian M, Kashani-Ligumsky L, Czeiger S, Cohen R, Schindler Y, Lubin D, et al. Safety of vaginal delivery in women infected with COVID-19. Pediatr Neonatol. 2021;62:90–6. doi: 10.1016/j.pedneo.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gupta V, Yadav Y, Sharma R, Mishra M, Ambedkar D, Gupta V, et al. Maternal and perinatal outcomes of hospitalized COVID-19 positive pregnant women. Cureus. 2022;14:e21817. doi: 10.7759/cureus.21817. doi: 10.7759/cureus. 21817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Akyıldız D, Çamur Z. Comparison of early postnatal clinical outcomes of newborns born to pregnant women with COVID-19: A case–control study. J Matern Fetal Neonatal Med. 2022;35:8673–80. doi: 10.1080/14767058.2021.1998440. [DOI] [PubMed] [Google Scholar]
- 114.Zamaniyan M, Rahmani Z, Ghasemian R, Karimi Z, Arab R-K, Ebadi A, et al. Maternal and neonatal outcomes in pregnant women with COVID-19 admitted to Imam Khomeini Hospital of Sari, Iran, 2019-2020. Arch Clin Infect Dis. 2023;18:e119394. doi: 10.5812/archcid-119394. [Google Scholar]
- 115.Sunuwar N, Jaishi PP, Twayana AR, Neupane PK, Neupane SK. A retrospective study of COVID during pregnancy and the outcome of vaginal delivery. Ann Med Surg. 2022;84:104880. doi: 10.1016/j.amsu.2022.104880. doi: 10.1016/j.amsu. 2022.104880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Florea RM, Sultana CM. COVID-19 and breastfeeding: Can SARS-CoV-2 be spread through lactation? Discoveries. 2021;9:e132. doi: 10.15190/d.2021.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ceulemans M, Cuppers B, de Vries L, Allegaert K, Duvekot J, van Puijenbroek EP. COVID-19 during pregnancy and lactation: What do we already know? Ned Tijdschr Geneeskd. 2021;164:D5036. [PubMed] [Google Scholar]
- 118.Gao X, Wang S, Zeng W, Chen S, Wu J, Lin X, et al. Clinical and immunologic features among COVID-19–affected mother–infant pairs: Antibodies to SARS-CoV-2 detected in breast milk. New Microbes New Infect. 2020;37:100752. doi: 10.1016/j.nmni.2020.100752. doi: 10.1016/j.nmni. 2020.100752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Centeno-Tablante E, Medina-Rivera M, Finkelstein JL, Rayco-Solon P, Garcia-Casal MN, Rogers L, et al. Transmission of SARS-CoV-2 through breast milk and breastfeeding: A living systematic review. Ann N Y Acad Sci. 2021;1484:32–54. doi: 10.1111/nyas.14477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pérez-Bermejo M, Peris-Ochando B, Murillo-Llorente MT. COVID-19: Relationship and Impact on Breastfeeding—A systematic review. Nutrients. 2021;13:2972. doi: 10.3390/nu13092972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bäuerl C, Randazzo W, Sánchez G, Selma-Royo M, Verdevio EG, Martínez L, et al. SARS-CoV-2 RNA and antibody detection in breast milk from a prospective multicentre study in Spain. Arch Dis Child Fetal Neonatal Ed. 2022;107:216–21. doi: 10.1136/archdischild-2021-322463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Aiman U, Sholehah M, Husein MG. Risk transmission through breastfeeding and antibody in COVID-19 mother. Gaceta Sanitaria. 2021;35:S524–9. doi: 10.1016/j.gaceta.2021.07.029. doi: 10.1016/j.gaceta. 2021.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vassilopoulou E, Feketea G, Koumbi L, Mesiari C, Berghea EC, Konstantinou GN. Breastfeeding and COVID-19: From nutrition to immunity. Front Immunol. 2021;12:661806. doi: 10.3389/fimmu.2021.661806. doi: 10.3389/fimmu. 2021.661806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ng YPM, Low YF, Goh XL, Fok D, Amin Z. Breastfeeding in COVID-19: A pragmatic approach. Am J Perinatol. 2020;37:1377–84. doi: 10.1055/s-0040-1716506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Low JM, Low YW, Zhong Y, Lee CYC, Chan M, Ng NBH, et al. Titres and neutralising capacity of SARS-CoV-2-specific antibodies in human milk: A systematic review. Arch Dis Child Fetal Neonatal Ed. 2022;107:174–80. doi: 10.1136/archdischild-2021-322156. [DOI] [PubMed] [Google Scholar]
- 126.Hethyshi R. Breast feeding in suspected or confirmed cases of COVID 19–a new perspective. J Obstet Gynecol India. 2020;70:267–71. doi: 10.1007/s13224-020-01336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Forti A, et al. Breastfeeding mothers with COVID-19 infection: A case series. Int Breastfeed J. 2020;15:1–8. doi: 10.1186/s13006-020-00314-8. doi: 10.1186/s13006-020-00314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lackey KA, Pace RM, Williams JE, Bode L, Donovan SM, Järvinen KM, et al. SARS-CoV-2 and human milk: What is the evidence? Matern Child Nutr. 2020;16:e13032. doi: 10.1111/mcn.13032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lou F, Qin H, He S, Li M, An X, Song L, et al. The benefits of breastfeeding still outweigh the risks of COVID-19 transmission. Front Med. 2021:1451. doi: 10.3389/fmed.2021.703950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lubbe W, Botha E, Niela-Vilen H, Reimers P. Breastfeeding during the COVID-19 pandemic–a literature review for clinical practice. Int Breastfeed J. 2020;15:1–9. doi: 10.1186/s13006-020-00319-3. doi: 10.3389/fmed. 2021.703950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fry HL, Levin O, Kholina K, Bianco JL, Gallant J, Chan K, et al. Infant feeding experiences and concerns among caregivers early in the COVID-19 State of Emergency in Nova Scotia, Canada. Matern Child Nutr. 2021;17:e13154. doi: 10.1111/mcn.13154. doi: 10.1111/mcn. 13154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Al-Kuraishy HM, Al-Gareeb AI, Atanu FO, El-Zamkan MA, Diab HM, Ahmed AS, et al. Maternal transmission of SARS-CoV-2: safety of breastfeeding in infants born to infected mothers. Frontiers in Pediatrics. 2021;9:738263. doi: 10.3389/fped.2021.738263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kunjumon B, Wachtel EV, Lumba R, Quan M, Remon J, Louie M, et al. Breast milk and breastfeeding of infants born to SARS-CoV-2 positive mothers: A prospective observational cohort study. Am J Perinatol. 2021;38:1209–16. doi: 10.1055/s-0041-1731451. [DOI] [PubMed] [Google Scholar]
- 134.Mishra G, Dwivedi R, Jain A. Risk of transmission of COVID-19 to newborns in COVID-19 positive mothers-A case series. J Cardiovasc Dis Res. 2022;13:716–24. [Google Scholar]
- 135.Kasraeian M, Zare M, Vafaei H, Asadi N, Faraji A, Bazrafshan K, et al. COVID-19 pneumonia and pregnancy; a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2022;35:1652–9. doi: 10.1080/14767058.2020.1763952. [DOI] [PubMed] [Google Scholar]
- 136.Mehta OP, Bhandari P, Raut A, Kacimi SEO, Huy NT. Coronavirus disease (COVID-19): Comprehensive review of clinical presentation. Front Public Health. 2021;8:582932. doi: 10.3389/fpubh.2020.582932. doi: 10.3389/fpubh. 2020.582932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Naz S, Rahat T, Memon FN. Vertical transmission of SARS-CoV-2 from COVID-19 infected pregnant women: A review on intrauterine transmission. Fetal Pediatr Pathol. 2021;40:80–92. doi: 10.1080/15513815.2020.1865491. [DOI] [PubMed] [Google Scholar]
- 138.Tammaro A, Kulakowska KA, Cantisani C, Parisella FR, Scarabello A, Adebanjo GAR. Female genital mucosal lesions associated with COVID-19 vaccination: A brief review of the literature. J Eur Acad Dermatol Venereol. 2023;37:e143–6. doi: 10.1111/jdv.18711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Falkenhain-López D, Agud-Dios M, Ortiz-Romero P, Sánchez-Velázquez A. COVID-19-related acute genital ulcers. J Eur Acad Dermatol Venereol. 2020;34:e655–6. doi: 10.1111/jdv.16740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kotlyar AM, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, Tal O, et al. Vertical transmission of coronavirus disease 2019: A systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:35–53. doi: 10.1016/j.ajog.2020.07.049. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ryan GA, Purandare NC, McAuliffe FM, Hod M, Purandare CN. Clinical update on COVID-19 in pregnancy: A review article. J Obstet Gynaecol Res. 2020;46:1235–45. doi: 10.1111/jog.14321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Heidary Z, Gargari OK, Fathi H, Zaki-Dizaji M, Ghaemi M, Rashidi BH. Maternal and neonatal complications, outcomes and possibility of vertical transmission in iranian women with COVID-19. Arch Iran Med. 2021;24:713–21. doi: 10.34172/aim.2021.104. [DOI] [PubMed] [Google Scholar]
- 143.Lessler J. An overlooked role for fecal transmission of SARS-CoV-2? Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Nori W, Salman DA. Seminal fluid changes in the COVID-19 era: During infection and Post-vaccination. Gynecology and Obstetrics Clinical Medicine. 2023;3:88–93. doi: 10.1016/j.gocm.2023.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Available from: https://dergipark.org.tr/en/pub/eurj/ issue/24881/1193573 . Des 2020.
- 146.Tristão LS, Bresler R, Modesto VA, Fernandes RdC, Bernardo WM. Urological complications of COVID-19: A systematic review. Int Braz J Urol. 2023;49:24–40. doi: 10.1590/S1677-5538.IBJU.2022.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Fornari F. Vertical transmission of Covid-19-A systematic review. J Pediatr Perinatol Child Health. 2020;4:7–13. [Google Scholar]
- 148.Yuan J, Qian H, Cao S, Dong B, Yan X, Luo S, et al. Is there possibility of vertical transmission of COVID-19: A systematic review. Transl Pediatr. 2021;10:423. doi: 10.21037/tp-20-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Najafi TF, Dashti S, Bahri N. Vertical transmission of covid-19: A systematic review. Archives of Pediatric Infectious Diseases, 2021:9. [Google Scholar]
- 150.Manigandan S, Wu M-T, Ponnusamy VK, Raghavendra VB, Pugazhendhi A, Brindhadevi K. A systematic review on recent trends in transmission, diagnosis, prevention and imaging features of COVID-19. Process Biochem. 2020;98:233–40. doi: 10.1016/j.procbio.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.De Luca D, Vauloup-Fellous C, Benachi A, Vivanti A. Transmission of SARS-CoV-2 from mother to fetus or neonate: What to know and what to do? Semin Fetal Neonatal Med. 2023;28:101429. doi: 10.1016/j.siny.2023.101429. doi: 10.1016/j.siny. 2023.101429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Goulioumis A, Angelopoulou M, Kourelis K, Mourtzouchos K, Tsiakou M, Asimakopoulos A. Hearing screening test in neonates born to COVID-19–positive mothers. European Journal of Pediatrics. 2023;182:1077–81. doi: 10.1007/s00431-022-04770-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kim YK, Kim EH. Pregnancy and COVID-19: Past, present and future. Obstet Gynecol Sci. 2023;66:149–60. doi: 10.5468/ogs.23001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Muhidin S, Moghadam ZB, Vizheh M. Analysis of maternal coronavirus infections and neonates born to mothers with 2019-nCoV; a systematic review. Arch Acad Emerg Med. 2020;8:e49. [PMC free article] [PubMed] [Google Scholar]
- 155.Wu Y, Liu C, Dong L, Zhang C, Chen Y, Liu J, et al. Viral shedding of COVID-19 in pregnant women. SSRN. 2020 doi: 10.2139/ssrn. 3562059. [Google Scholar]
- 156.Sokou R, Konstantinidi A, Boutsikou T, Iliodromiti Z, Iacovidou N. Breastfeeding in the era of COVID-19. A narrative review. J Obstet Gynaecol. 2022;42:539–45. doi: 10.1080/01443615.2021.1929112. [DOI] [PubMed] [Google Scholar]
- 157.Jakuszko K, Kościelska-Kasprzak K, Żabińska M, Bartoszek D, Poznański P, Rukasz D, et al. Immune response to vaccination against COVID-19 in breastfeeding health workers. Vaccines. 2021;9:663. doi: 10.3390/vaccines9060663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Krishnamurthy G, Sahni R, Leone T, Kim F, Brooks MC, Villaraza-Morales S, et al. Care of the COVID-19 exposed complex newborn infant. Semin Perinatol. 2020;44:151282. doi: 10.1016/j.semperi.2020.151282. doi: 10.1016/j.semperi. 2020.151282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Singh V, Trigunait P, Majumdar S, Ganeshan R, Sahu R. Managing pregnancy in COVID-19 pandemic: A review article. Journal of family medicine and primary care. 2020;9:5468–73. doi: 10.4103/jfmpc.jfmpc_950_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kimani RW, Maina R, Shumba C, Shaibu S. Maternal and newborn care during the COVID-19 pandemic in Kenya: Re-contextualising the community midwifery model. Hum Resour Health. 2020;18:1–5. doi: 10.1186/s12960-020-00518-3. doi: 10.1186/s12960-020-00518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bhatt H. Should COVID-19 mother breastfeed her newborn child? A literature review on the safety of breastfeeding for pregnant women with COVID-19. Curr Nutr Rep. 2021;10:71–5. doi: 10.1007/s13668-020-00343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Jorgensen SC, Burry L, Tabbara N. Role of maternal COVID-19 vaccination in providing immunological protection to the newborn. Pharmacotherapy. 2022;42:58–70. doi: 10.1002/phar.2649. [DOI] [PubMed] [Google Scholar]
- 163.Koç E, Dilli D. How does COVID-19 affect maternal and neonatal outcomes? J Perinat Med. 2023;51:277–83. doi: 10.1515/jpm-2022-0509. [DOI] [PubMed] [Google Scholar]



