Abstract
Pulmonary agenesis (PA) is a rare developmental malformation, with a frequency of approximately 1 in 10–15,000 pregnancies. Unilateral PA is often associated with other congenital anomalies, whereas bilateral PA is fatal. Prenatal diagnosis is rare and is diagnosed more frequently in the postnatal period than in the prenatal period. Is a challenge that may be difficult as it shares similar features with other more common pathologies. Ultrasound plays a crucial role in early diagnosis and management. Ultrasonographic findings for a correct prenatal diagnosis include mediastinum displacement with the absence of parenchymal or cystic tissue, decreased thoracic volume, an elevated diaphragm, cardiac axis deviation, and a hemithoracic cavity largely occupied by the heart. Cases of right PA have a worse prognosis compared to left PA, probably due to higher frequency of cardiac and great vessel abnormalities. A rare case of early prenatal ultrasound diagnosis of unilateral fetal PA, at 18 weeks of gestation, is reported.
Keywords: Fetal pulmonary malformations, lung agenesis, prenatal diagnosis, pulmonary agenesis
INTRODUCTION
Pulmonary agenesis (PA) is a rare congenital anomaly of unknown cause, characterized by complete absence of lung parenchyma, bronchi, and pulmonary vessels. In about half of the cases, it is accompanied by other malformations of skeletal, cardiovascular, and genitourinary systems. Prenatal diagnosis is rare and is diagnosed more frequently in the postnatal period than in the prenatal period.[1] Prognosis depends on the presence of other congenital malformations. Right PA is associated with a higher incidence of mediastinal displacement, tracheal compression, and great vessel distortion.[2] Early prenatal diagnosis may improve survival by allowing appropriate postnatal treatment. This is a rare and unique case of early prenatal ultrasound diagnosis of unilateral fetal PA, at 18 weeks of gestation.
CASE REPORT
A 29-year-old female patient, III gestations, II paras, 18 weeks pregnant by the date of the last menstrual period, was referred for consultation for suspected fetal thoracic anomaly with mediastinal shift on routine ultrasound evaluation. Ultrasound performed at 9 weeks found no fetal anatomical abnormalities. Pregnancy was conceived spontaneously, the patient was healthy and denied consanguinity with her partner, as well as personal history of alcohol, tobacco, and illicit drug use or family history of congenital malformations. Hematology, hepatitis, syphilis, HIV, and TORCH tests were negative. Triple serum test showed a low risk of aneuploidy.
Ultrasound evaluation at 18 weeks showed a single female fetus with normal amniotic fluid volume for gestational age. Fetal ultrasound measurements showed that all biometric measurements were below percentile 25 for gestational age. Mediastinal deviation to right with the absence of parenchymal and/or cystic tissue on the right side of the fetal thorax was observed. It was also not possible to visualize pulmonary arterial bifurcation and corresponding pulmonary veins with color Doppler. Fetal dextrocardia was also evident occupying part of the right hemithorax, with atrial septal and interventricular septal defects. The left lung was hypertrophic, accentuating mediastinum displacement toward the right hemithorax [Figure 1]. Abdominal organs were in normal position. There was no evidence of hydrops, pleural effusion, and/or cardiomegaly. The parents agreed to perform amniocentesis, the results of which showed normal karyotype (46XX).
Figure 1.
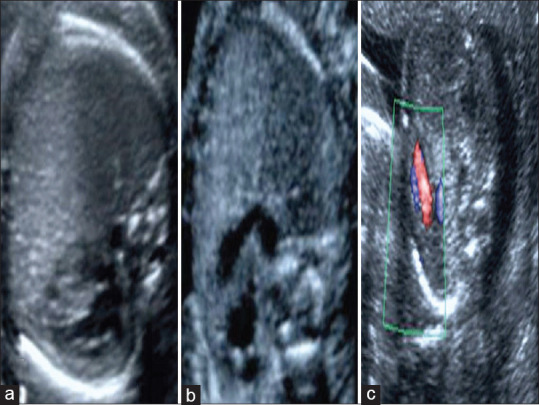
Axial image of the fetal thorax of right pulmonary agenesis. (a) Fetal heart displaced to the right side. (b) Absence of right pulmonary artery bifurcation. (c) Color Doppler ultrasound demonstrating the absence of the right pulmonary artery
The patient was referred to high-risk prenatal and genetic consultation for prenatal counseling. At the next postdiagnosis visit, the absence of fetal heart rate was determined and the patient was taken to the emergency room for cervical dilatation and uterine curettage. Detailed anatomic-pathologic examination described a female fetus of approximately 18 weeks, confirming right PA and corresponding vessels, along with dextrocardia, and hypertrophic left lung [Figure 2].
Figure 2.
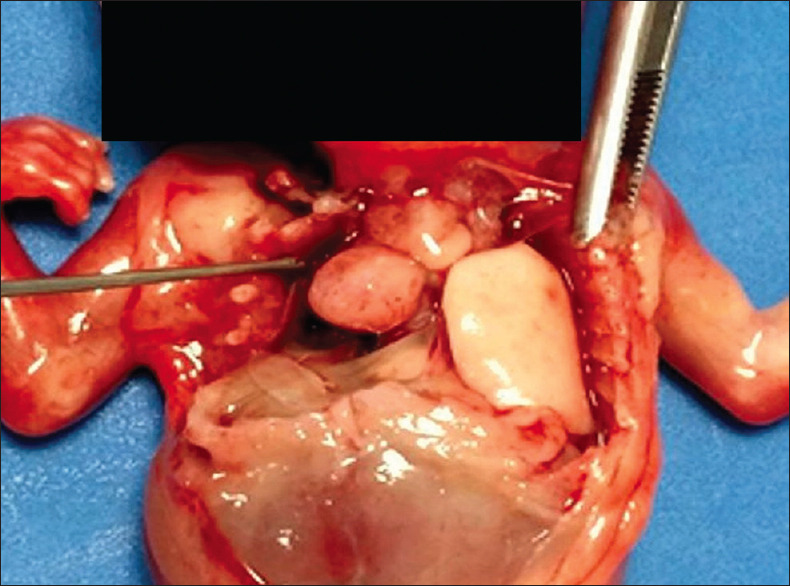
Postmortem image showing right unilateral pulmonary agenesis
DISCUSSION
Embryonic development of the respiratory system begins during the 6th week of gestation when the respiratory diverticulum appears along the foregut ventral surface. During the 7th week of gestation, it begins to branch, forming bronchial buds. Development of the respiratory tree can be divided into three main stages: pseudoglandular, canaliculus, and alveolar. As lung development progresses, airways become more canaliculate and vascularized to allow efficient gas exchange after birth.[1,2,3] Abnormalities of the respiratory tree can arise from disruption at any time. Earlier alterations lead to more severe pathologies.[1] Growth pattern is largely determined by mesoderm.[1] Defects in lung development can be classified into three major groups, according to Schneider’s classification proposed in 1909:[4] Class I – PA, with complete absence of lung tissue, bronchi, and vessels; Class II – PA, with complete absence of lung tissue but with rudimentary bronchi; and Class III – pulmonary hypoplasia, with poorly developed lung tissue and bronchi.[1,4]
Fetal PA was first reported by Depozze in 1673 as a finding from autopsy of a woman. AP congenital absence of one or both lungs was described in 1762, by Morgagni.[5,6] Is a rare condition that affects 1 in every 10–15,000 births, and may occur in isolation or in association with other malformations.[1,2,3,4,5,6,7] There are only a few reported cases of AP prenatal diagnosis in the literature. In most prenatal diagnosed cases is unilateral, the right: left ratio described is around 5:1, due to that it is possibly easier to diagnose right than left PA, especially because of greater mediastinal displacement.[2,3,4,5,7]
Exact etiology is unknown, although genetic alterations, viral infections, and folic acid and Vitamin A deficiencies have been suggested as contributing factors.[3,5,7]
Prenatal diagnosis of PA is challenging due to potential difficulties in distinguishing it from other pathologies with similar sonographic appearance.[1,2] Ultrasound findings for correct prenatal diagnosis include mediastinal displacement with the absence of parenchymal or cystic tissue, decreased thoracic volume, elevated diaphragm, deviation of cardiac axis, and hemithoracic cavity largely occupied by the heart. Color Doppler evaluation demonstrates the absence of corresponding pulmonary arterial vessels. In these cases, a complete and accurate evaluation of the rest of fetal anatomy is necessary to exclude the presence of other fetal malformations that affect postnatal prognosis.[4]
Fetal MRI overcomes ultrasound diagnostic difficulties, allowing simultaneous visualization of multiple planes and better differentiation of different types of tissue. However, it is not useful to accurately evaluate associated congenital heart disease.[1,4]
Differential diagnosis of unilateral PA includes total atelectasis, congenital cystic adenomatoid malformation, and congenital diaphragmatic hernia.[4] Total atelectasis of the right lung may be difficult based solely on displacement of the mediastinum and heart. Congenital adenomatoid cystic malformation may present multiple cystic lung lesions with heart and mediastinum displacement.[8] Fetuses with congenital diaphragmatic hernia usually present abdominal organs within the thorax, leading to displacement of the fetal heart.[8,9] Pulmonary hypoplasia may show that lung volume is asymmetrically decreased with abnormally low signal intensity.[10] Other less frequent differential diagnoses are dextrocardia or isolated dextroposition, emphysema, mediastinal teratoma, neuroblastoma, and heterotaxy syndrome.[4]
There are several important prognostic factors to consider in the management of unilateral PA as right-sided agenesis, the presence of genetic abnormalities, and other associated congenital anomalies.[1] Cases of isolated PA have an overall good prognosis and can be managed conservatively during pregnancy, with consideration of delivery at a tertiary care facility.[1] There are described cases of long-term survival, if PA is unilateral and is not associated with congenital anomalies, while bilateral agenesis is a fatal condition. Prenatal diagnosis may improve survival by allowing appropriate postnatal treatment.[4]
Few cases have been reported in literature who were treated successfully by surgical procedures such as aortopexy and diaphragmatic translocation, subclavian artery reimplantation, tracheal stenting, slide tracheoplasty, and laser ablation of fibrotic tissue at the site of tracheal stenosis.[6]
CONCLUSION
Fetal PA is a rare condition, and the diagnosis is done in the prenatal and postnatal periods. Ultrasound plays a crucial role in early prenatal diagnosis and management. The presence of mediastinal displacement, with the absence of parenchymal or cystic tissue, decreased thoracic volume, elevated diaphragm, cardiac axis deviation, a hemithoracic cavity largely occupied by the heart, and inability to locate pulmonary arteries, as presented in this case, should lead to an early ultrasound prenatal diagnosis. In these cases, complete fetal anatomic evaluation for other anomalies is essential to establish fetal prognosis. Early prenatal ultrasound diagnosis, as performed in this fetus, may aid in prenatal counseling and postdelivery care.
Ethics approval
The authors declare that the study was approved by the Committee of Ethics of the Hospital Central of Maracaibo, Venezuela, on November 29, 2022, and the procedures followed were shaped in accordance with the World Medical Association and the Declaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for the images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Author contributions
ER-V, LB-S, JCBS and CB-P designed the study, acquired, analyzed, and interpreted the data, wrote the paper, and approved the final version to be published.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Russell BC, Whitecar P, Nitsche JF. Isolated unilateral pulmonary agenesis and other fetal thoracic anomalies. Obstet Gynecol Surv. 2014;69:335–45. doi: 10.1097/OGX.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 2.Meller CH, Morris RK, Desai T, Kilby MD. Prenatal diagnosis of isolated right lung agenesis using ultrasound alone: Case study and systematic review of the literature. J Ultrasound Med. 2012;31:2017–23. doi: 10.7863/jum.2012.31.12.2017. [DOI] [PubMed] [Google Scholar]
- 3.Romero de Fasolino M, Hernández ML, Rodríguez R. Morphological aspects of lung development. In: Briceño-Pérez C, editor. Maduración Pulmonar Fetal/Fetal Lung Maturation. 1st ed. Caracas: Amolca; 2008. [Google Scholar]
- 4.Ito Y, Tanemoto T, Kato A, Tanaka K, Umehara N, Kawaguchi R, et al. Usefulness of ultrasonography and MRI for diagnosis of fetal pulmonary agenesis: Case report and review of the literature. J Med Ultrason (2001) 2013;40:157–62. doi: 10.1007/s10396-012-0410-7. [DOI] [PubMed] [Google Scholar]
- 5.Brunner S, Nissen E. Agenesis of the lung. Am Rev Respir Dis. 1963;87:103–6. doi: 10.1164/arrd.1963.87.1.103. [DOI] [PubMed] [Google Scholar]
- 6.Khurram MS, Rao SP, Vamshipriya A. Pulmonary agenesis: A case report with review of literature. Qatar Med J 2013. 2013:38–40. doi: 10.5339/qmj.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maltz DL, Nadas AS. Agenesis of the lung. Presentation of eight new cases and review of the literature. Pediatrics. 1968;42:175–88. [PubMed] [Google Scholar]
- 8.Chaturvedi A, Klionsky N, Biyyam D, Chess MA, Sultan N. Acutely presenting congenital thoracic lesions: A radiologist's handbook. Emerg Radiol. 2022;29:557–70. doi: 10.1007/s10140-022-02035-3. [DOI] [PubMed] [Google Scholar]
- 9.Strong M, Garabedian M, Pettigrew A, Barron N, Hansen W. Prenatal diagnosis of partial trisomy 16p and its association with congenital diaphragmatic hernia. Prenat Diagn. 2013;33:797–9. doi: 10.1002/pd.4108. [DOI] [PubMed] [Google Scholar]
- 10.Fujioka K, Morioka I, Nishida K, Morizane M, Tanimura K, Deguchi M, et al. Pulmonary hypoplasia caused by fetal ascites in congenital cytomegalovirus infection despite fetal therapy. Front Pediatr. 2017;5:241. doi: 10.3389/fped.2017.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]


