Abstract
Objective:
The objective of this study was to measure potential associations between surgeon sex and number of days alive and at home (DAH).
Background:
Patients treated by female surgeons appear to have lower rates of mortality, complications, readmissions, and healthcare costs when compared with male surgeons. DAH is a validated measure, shown to better capture the patient experience of postoperative recovery.
Methods:
We conducted a retrospective study of adults (≥18 years of age) undergoing common surgeries between January 01, 2007 and December 31, 2019 in Ontario, Canada. The outcome measures were the number of DAH within 30-, 90-, and 365-days. The data was summarized using descriptive statistics and adjusted using multivariable generalized estimating equations.
Results:
During the study period, 1,165,711 individuals were included, of which 61.9% (N = 721,575) were female. Those managed by a female surgeon experienced a higher mean number of DAH when compared with male surgeons at 365 days (351.7 vs. 342.1 days; P < 0.001) and at each earlier time point. This remained consistent following adjustment for covariates, with patients of female surgeons experiencing a higher number of DAH at all time points, including at 365 days (343.2 [339.5–347.1] vs. 339.4 [335.9–343.0] days). Multivariable regression modeling revealed that patients of male surgeons had a significantly lower number of DAH versus female surgeons.
Conclusions:
Patients of female surgeons experienced a higher number of DAH when compared with those treated by male surgeons at all time points. More time spent at home after surgery may in turn lower costs of care, resource utilization, and potentially improve quality of life. Further studies are needed to examine these findings across other care contexts.
Keywords: cohort study, diversity, patient outcomes, physician sex
INTRODUCTION
Physician characteristics have been associated with patient outcomes across both surgical and medical specialties.1–3 Specifically, prior studies have noted that patients receiving care from female physicians may experience lower short-term and long-term mortality, hospital readmission rates, and healthcare costs when compared with those managed by male physicians.4–9
Prior studies on this topic have generally only considered mortality, complications, and readmissions, which are valued by patients but could be undermined by other outcomes such as transfer to skilled nursing facilities as they can negatively impact quality of life.10 Days alive and at home (DAH) is a validated, composite outcome measure that has been shown to better capture the patient experience of postoperative recovery. DAH is expressed in simple terms of days and provides a useful population-level metric that can be calculated using routinely collected patient data. It integrates several clinically important endpoints, including death, nonhome discharge, hospital length-of-stay, and hospital readmission.10–12 Therefore, it has distinct advantages as it contains more information than individual binary measures while incorporating the postdischarge trajectory, which is of higher priority for patients, especially those who may be older and have more comorbidities.13,14 Prior studies have also shown its appropriate responsiveness in accounting for the severity of the acute disease, greater burden of chronic disease, lower socioeconomic status of patients, and the presence of new complications following surgery, leading to nonhome discharge.11,13
There is a paucity of evidence on the association between the number of DAH and physician characteristics such as sex. Therefore, we conducted a population-based retrospective cohort study to determine potential associations between physician sex and the number of DAH at 30-, 90-, and 365-days across patients undergoing common surgeries in Ontario, Canada.
METHODS
Study Design
Consistent with prior literature,4,5 we conducted a population-based, retrospective cohort study of adults undergoing 1 of 25 common surgeries between January 1, 2007 and December 31, 2019 in Ontario, Canada. Residents of Ontario receive insurance for physician and hospital services through a single government payer, the Ontario Health Insurance Program. We included patients undergoing 25 common elective and emergent procedures, across the spectrum of all surgical subspecialties to ensure generalizability, including both open and laparoscopic/robotic approaches. Multi-disciplinary consultation was used to select the studied procedures, ranging from low to high perioperative risk.
This study was reported according to Strengthening the Reporting of Observational Studies in Epidemiology guidelines and REporting of studies Conducted using Observational Routinely-collected health Data statement (Supplemental Table 1, http://links.lww.com/AOSO/A397).15 The study protocol was approved by the Mount Sinai Hospital Research Ethics Board (#22-0110-C).
Data Sources
We linked the Ontario Health Insurance Plan database (physician billings, laboratories, and out-of-province providers16); the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (DAD) (hospitalizations17); the CIHI National Ambulatory Care Reporting System (emergency room visits); the Registered Persons Database (demographic information17); and the Corporate Provider Database (physician characteristics). The Continuous Care Reporting System was used to capture long-term care. These datasets were linked using unique encoded identifiers and analyzed at ICES (formerly known as Institute of Clinical Evaluative Sciences).
Cohort Derivation
We identified patients who underwent 1 of the 25 index procedures for whom the treating physicians could be identified (1,322,525; Supplemental Figure 1, http://links.lww.com/AOSO/A397). We excluded patients <18 years of age (29,187), those who were not Ontario residents (340), those whose date of death preceded the date of surgery (318), and those for whom we could not reliably ascertain the treating institution (2618). We further excluded those for whom we could not determine the sex or age of the treating surgeon (48,243) or anesthesiologist (47,482), as each of these has been shown to have an association with perioperative outcomes.5,7,18 Finally, we excluded patients with multiple concomitant surgical procedures (27,802) and those with less frequent combinations of surgical specialties and procedures (e.g., urology and craniotomy; 824), as these represent uncommon situations or miscoding, which may diminish reliability and generalizability. The overall study cohort comprised 1,165,711 unique patients.
Variable
Physician sex was determined from the Corporate Provider Database, derived from physician self-reports at the time of credentialing/registration with the Ontario Ministry of Health. This dataset did not include the self-reported gender identity of surgeons.
Outcomes
The primary outcome was DAH at 30 days after surgery (DAH30). DAH reflects the number of institution-free days and is calculated for each patient at individual time points using validated sources from CIHI-DAD, registered persons database, and the Continuous Care Reporting System. In keeping with prior studies,11,19,20 DAH3010 is calculated by subtracting the number of days spent in the hospital during the index admission, subsequent hospital readmissions, and long-term care facility from 30 days. Patients who died at any location during the 30-day postoperative period were assigned a DAH30 of 0 days. The secondary outcomes included the number of DAH at 90 days (DAH90) and 365 days (DAH365) which were determined using similar calculations.
Adjustments
Patient age, sex, geographic location (local health integration networks21), geographically derived socioeconomic status, rurality, and general comorbidities (Johns Hopkins aggregate disease group and ambulatory diagnosis groups) were obtained. We also collected data on the surgeon’s sex, age, years in practice, specialty, and surgical volume. Surgical volume was determined for each surgeon and procedure by identifying the number of identical procedures the operating surgeon performed in the previous year, operationalized in quartiles. Hospital institution identifiers were used to account for facility-level variability. We defined a surgical procedure as emergent or elective using the CIHI-DAD database. All same-day surgery procedures were considered elective. The duration of surgery, in minutes, was further collected.
Statistical Analysis
Descriptive statistics were used to compare the characteristics of patients, surgeons, anesthesiologists, and hospitals according to the sex of the surgeon. Given the large sample size, as traditional statistical measures are likely to demonstrate significant differences where no clinically important difference exists, we performed between-group comparisons using standardized differences, with a clinically important difference defined as greater than 0.10.22
We used multivariable generalized estimating equations with an independent correlation structure and a negative binomial distribution with a log link to calculate both the patient-level adjusted mean number of DAH and adjusted relative risk for the number of DAH among patients undergoing the same procedures. Specifically, we adjusted for patient-, surgeon-, and hospital-level covariates (as listed above and determined a priori) and procedure year while clustering on the specific procedure fee code. Adjusted means costs were obtained with the LSMean option in proc genmod. To obtain the difference in adjusted means, the NLMeans macro was used. The unit of analysis was the patient. We assessed model assumptions including collinearity and found no violations.
We performed an additional analysis, as determined a priori, by adding the duration of surgery as a covariate among the subset of 1,100,193 (94.3%) of patients with complete data on this variable. Statistical significance was set at P < 0.05 based on a 2-tailed comparison. All analyses were performed using Enterprise Guide 6.1 (SAS Institute Inc., Cary, NC).
RESULTS
Cohort Characteristics
During the study period, we identified 1,165,711 eligible patients, of which over half were female (61.9%; 721,215). The median (interquartile range [IQR]) age of the patient cohort was 60 (47–72) years old. Across all patients, 151,054 (13.0%) were managed by a female surgeon with the others receiving care from a male surgeon, with significant differences in baseline characteristics (Supplemental Figure 1, http://links.lww.com/AOSO/A397; Supplemental Table 2, http://links.lww.com/AOSO/A397). Around a quarter of patients were cared for by a female anesthesiologist (26.7%; 311,822). The majority of cases were elective (79.9%; 931,319) and performed in community hospitals (66.3%; 772,872) in urban settings (88.5%; 1,031,075). Most cases were done by general and orthopedic surgeons (33.1%; 385,821 and 33.6%; 391,950, respectively), with an overall median (IQR) case duration of 105 (75–148) minutes (Supplemental Table 2, http://links.lww.com/AOSO/A397).
Unadjusted Days Alive and Out of Hospital at 30, 90, and 365 days
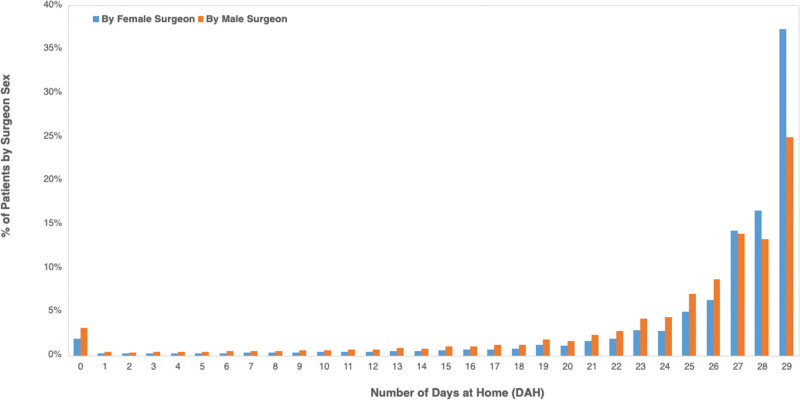
At 30 days, patients treated by female surgeons had a higher unadjusted mean number of DAH when compared with male surgeons (mean 25.6 vs 23.9 days; P < 0.001; Table 1). Similarly, patients of female surgeons had a significantly greater number of DAH at 90 and 365 days versus male surgeons (83.7 vs 80.5 days, and 351.7 vs 342.1 days, respectively; P < 0.001 for both comparisons; Table 1). The proportion of patients in each day up to DAH 30 for male and female surgeons is shown in Figure 1. Overall, most patients for both surgical groups resided within higher values of DAH of 27 days or more. However, there was a higher proportion of patients managed by female surgeons compared with male surgeons these days. At lower numbers of DAH within the distribution tail, there was a higher proportion of patients managed by male surgeons compared to female surgeons (Figure 1).
TABLE 1.
Crude Mean Number of Days Alive and at Home at 30- and 90 Days and 1 Year of Index Surgery, by Surgeon Sex
| Time Period | Measure | Male Surgeon (N = 1,014,657) | Female Surgeon (N = 151,054) | Total (N = 1,165,711) | P value |
|---|---|---|---|---|---|
| At 30 days | Mean (SD) | 23.9 (7.1) | 25.6 (6.0) | 24.1 (7.0) | <0.001 |
| Median (IQR) | 27.0 (23.0–28.0) | 28.0 (25.0–29.0) | 27.0 (23.0–29.0) | <0.001 | |
| At 90 days | Mean (SD) | 80.5 (16.4) | 83.7 (12.6) | 81.0 (16.0) | <0.001 |
| Median (IQR) | 86.0 (82.0–88.0) | 88.0 (85.0–89.0) | 87.0 (82.0–88.0) | <0.001 | |
| At 1 Year | Mean (SD) | 342.1 (61.8) | 351.7 (44.0) | 343.3 (59.9) | <0.001 |
| Median (IQR) | 360.0 (354.0–363.0) | 362.0 (358.0–364.0) | 361.0 (354.0–363.0) | <0.001 |
SD indicates standard deviation; IQR, interquartile range.
FIGURE 1.
Distribution of the patient-level number of days at home (DAH) within 30 days of index surgery, stratified by surgeon sex. For both male and female surgeons, the distribution of patients for each day up to 30 days at home is shown as a frequency (%) among the total number of patients operated on by the surgeon of that sex.
Adjusted Days Alive and Out of Hospital at 30, 90, and 365 days
When adjusted for patient, surgeon, anesthesiologist, and hospital characteristics, as determined a priori, the greater mean number of DAH persisted among patients of female versus male surgeons at all three time points (Table 2). Specifically, at 30 days, the adjusted mean (95% confidence interval [CI]) number of DAH for patients of female surgeons was 23.2 (22.7–23.6) versus 22.7 (22.2–23.2) days for those treated by male surgeons (Table 2). This significantly greater number of DAH among patients of female surgeons was also observed at 90 and 365 days versus those with male surgeons (79.9 [79.0–80.9] versus 78.8 [77.8–79.8] days, and 343.2 [339.5–347.1] versus 339.4 [335.9–343.0] days, respectively; Table 2).
TABLE 2.
Adjusted Mean Number of Days Alive and at Home at 30- and 90-Days and 1 Year of Index Surgery, by Surgeon Sex
| Time Period | Male Surgeon (N = 1,014,657) |
Female Surgeon (N = 151,054) |
Male versus Female Surgeon aRR (95% CI) | P value |
|---|---|---|---|---|
| At 30 days | 22.7 (22.2–23.2) | 23.2 (22.7–23.6) | 0.98 (0.97–0.99) | <0.001 |
| At 90 days | 78.8 (77.8–79.8) | 79.9 (79.0–80.9) | 0.99 (0.98–0.99) | <0.001 |
| At 1 year | 339.4 (335.9–343.0) | 343.2 (339.5–347.1) | 0.99 (0.98–1.00) | <0.001 |
Data presented as mean or aRR with 95% CI.
Using GEE modeling dealing with clustering based on procedure fee code (negative binomial regression with log link), adjusted for surgeon age, surgeon specialty, surgeon annual case volume, surgeon years of practice, anesthesiologist age, anesthesiologist sex, anesthesiologist annual case volume, anesthesiologist years of practice, patient age, patient sex, patient comorbidity, rurality, income quintile, LHIN, hospital status, and year of index surgery.
aRR indicates adjusted risk ratio; CI, confidence interval.
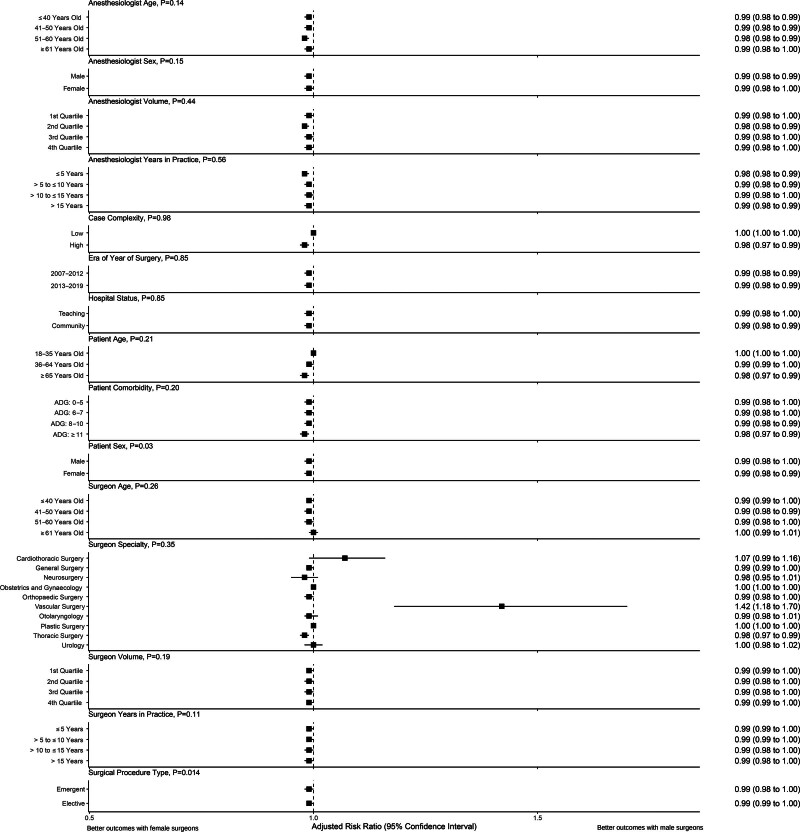
Consistent with these findings, multivariable regression modeling with adjustment for covariates revealed a significantly lower number of DAH among patients of male surgeons within 30 days (adjusted relative risk [aRR] = 0.98; 95% CI = 0.97–0.99; P < 0.001; Table 2). These observed effects remained consistent at 90 and 365 days (aRR = 0.99; 95% CI = 0.98–0.99; P < 0.001, and aRR = 0.99; 95% CI = 0.98–1.00; P < 0.001; Table 2). The findings also remained significant following adjustment for the duration of surgery (N = 1,100,193; Supplemental Table 3, http://links.lww.com/AOSO/A397). Subgroup analyses assessing for effect modification due to patient, surgeon, anesthesiologist, and procedure-related characteristics demonstrated generally consistent results (Figure 2). Of note, while there was no evidence of statistical heterogeneity between surgical specialties (P = 0.35), there was a higher number of DAH among patients of male versus female vascular surgeons (aOR = 1.42; 95% CI = 1.18–1.70; P < 0.001). This trend was also observed among cardiothoracic surgeons without reaching statistical significance (Figure 2).
FIGURE 2.
Forest plot of subgroup analyses assessing the association between surgeon sex and number of days at home (DAH) within 90 days of index surgery, stratified by anesthesiologist, surgeon, patient, and procedural characteristics. P values correspond to the observed heterogeneity. ADG indicates ambulatory diagnosis groups.
DISCUSSION
Main Findings
Across 1,165,711 adult patients undergoing common surgical procedures in Ontario, those managed by a female surgeon experienced a higher mean number of DAH when compared with individuals cared for by male surgeons. Following adjustment for covariates, patients of male surgeons had a significantly lower number of DAH versus female surgeons. A greater number of DAH reflects a larger amount of time spent away from needing medical and supportive care in the short- and long-term postoperative period which can contribute to higher quality of life for patients, as well as cost and resource savings for clinicians and healthcare institutions.
Comparison with Existing Evidence
While this study is, to the best of our knowledge, the first to measure the association between surgeon sex and the number of DAH, these findings align with prior studies that have demonstrated better clinical outcomes among patients treated by female versus male physicians. Specifically, prior studies1,2,5,9 have reported lower short-term (e.g. in-hospital or 30-day) mortality and complication rates among those treated by female physicians when compared with patients managed by male physicians. Additionally, patients of female physicians have also been shown to have lower odds of hospital readmission versus those treated by male physicians.8,23 Moreover, a study looking at longer-term outcomes noted similar findings.4 Consistent with these data, we found a higher mean number of DAH across patients of female versus male physicians at 30-, 90-, and 365 days. While these data were consistent across nearly all subgroups defined by patient, physician, and procedural characteristics, interestingly, we found that patients of male vascular surgeons having a higher number of DAH versus female vascular surgeons. However, there was no statistical evidence of heterogeneity of effect between surgical specialties. Therefore, this finding should be considered exploratory and hypothesis-generating.
Studies have also found shorter hospital length-of-stay among patients of female surgeons; however, we noted a difference in the number of DAH that does not appear to be fully explained by hospital stay alone. For instance, while Wallis et al5 reported statistically significant differences in hospital length-of-stay between patients of female versus male surgeons (adjusted relative rate 0.97; 95% CI = 0.94–0.99; P = 0.01), the estimates were similar (median [IQR] 2 [0–4] days for both cohorts). This suggests that patients may have differential postdischarge outcomes that influence the number of DAH and mortality. The mechanism behind these findings is multifactorial, with studies ongoing to better understand attributable causes. Prior studies have suggested that female surgeons may offer more evidence-based care.24,25 Therefore, this difference could be attributable to practice patterns that more closely follow postoperative care guidelines, with greater preventative care or potentially more risk-averse decision-making.26,27 Additionally, they may exhibit better communication skills and a greater willingness to work with the interprofessional team when compared with male physicians.26 This could promote shared decision-making with patients and families by enhancing their understanding and aid in improving adherence to postoperative care plans. Some studies with limited sample sizes have also reported better scores and skill acquisition among female versus male medical students.28,29 Future work on this topic across other specialties and healthcare settings should consider the use of DAH as the primary outcome given its incorporation of several patient-important measures.
DAH provides a feasible metric for assessing patients’ global and collated experiences after having surgery. At 30 days after surgery, this study revealed that patients under the care of male surgeons spend 0.5 fewer days at home compared with patients under the care of female surgeons. With consideration of our surgical cohort of approximately 1.1 million patients, if these differences were attributable to surgeon sex, this would amount to an additional 39,025 days per year that patients spend away from home needing medical and supportive care in the early postsurgery period when managed by male surgeons. With larger adjusted differences in the number of DAH at longer periods of 90 (1.1 days) and 365 days (3.8 days) following index surgery, the surgeon sex difference contributes to a respective additional 85,856 and 296,592 institutional days per year among patients managed by male surgeons within this study cohort. These data may support our earlier findings across the same study population which identified higher healthcare costs among patients treated by male surgeons (adjusted sex differences in total healthcare costs at 30 days $3115, and 1 year $24,882) that are largely driven by higher costs for inpatient and postdischarge care.30
Strengths and Limitations
This study analyzed the association between physician sex and a comprehensive outcome which captures the patient experience postoperatively, the number of DAH. This outcome has been validated across studies in the perioperative setting and was shown to better capture patient-important outcomes, including transfer to skilled nursing. We also estimated the association between surgeon sex and longer-term outcomes at 90 and 365 days following the index surgery. The inclusion of over 1.1 million patients across all surgical subspecialties, as well as both elective and emergent procedures, also improves the generalizability of the findings. We analyzed patients across all hospitals in Ontario, minimizing the risk that we would miss a subsequent admission to an institution other than the one where a patient underwent surgery.
There are important limitations to this study, mainly attributable to the observational nature of the data sources. Specifically, given the administrative datasets used, there is a risk of misclassification of characteristics and outcomes. Additionally, we captured binary biological sex and were unable to assess the gender of patients or surgeons. Furthermore, we are unable to capture other potentially important aspects of identity, including race, ethnicity, and other sociocultural factors. While we adjusted for several covariates relating to patient, surgeon, and hospital characteristics, there is a risk of residual confounding from unmeasured variables in the datasets, including qualitative differences in practice patterns and granular data regarding case complexity. While the large sample size aids in the generalizability of our findings, despite the adjustment for several covariates, further mixed-methods research is needed to determine underlying mechanisms for the observed statistical differences and better evaluate whether a clinically important difference exists. We also could not account for the potential effect of other team members (i.e. resident physicians, nurses) or intra-operative resources and equipment utilization as they are not captured in the utilized datasets. Moreover, while patients were categorized by primary surgeon sex, and we accounted for anesthesiologist characteristics, we could not assess the role of other potential surgeons and other physicians involved in the perioperative care of these individuals.
CONCLUSIONS
Patients of female surgeons experienced a higher number of DAH when compared with those treated by male surgeons, which remained consistent at 30, 90, and 365 days, following adjustment for covariates. Further studies are needed to examine these findings across other care contexts and better understand underlying mechanisms.
ACKNOWLEDGMENTS
We are indebted to the methodologic and analytic support provided by Refik Saskin, MSc, and Bo Zhang, MPH, PhD (Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada), who were compensated for their work. Dr. Zhang performed the statistical analysis based on an analytic plan designed by C.J.D.W. This study made use of deidentified data from the Institute for Clinical Evaluation Sciences Data Repository, which is managed by the Institute for Clinical Evaluative Sciences with support from its funders and partners: Canada’s Strategy for Patient-Oriented Research, Ontario Canada’s Strategy for Patient-Oriented Research Support Unit, the Canadian Institutes of Health Research, and the government of Ontario.
AUTHOR CONTRIBUTIONS
R.S., A.N.L., K.A., A.S.D., C.J.D.W., and A.J. developed the research question and methodology. K.H., R.S., A.N.L., K.A., A.S.D., C.J.D.W., and A.J. contributed to data acquisition and summarized the findings. Additional data analysis was conducted by Bo Zhang who was compensated for their work. K.H., R.S., K.A., H.S.T., A.S., N.C., F.C.W., L.G.C., A.N.L., S.R., C.R., C.M., K.A., B.B., A.S.D., A.J., C.J.D.W. interpreted the findings. K.H. wrote the first draft of the manuscript. All authors critically appraised the methodology and the findings of the study. All authors reviewed and commented on all versions of the manuscript. A.J. and C.J.D.W. provided supervision for the study.
Supplementary Material
Footnotes
Published online 19 July 2024
Angela Jerath and Christopher JD Wallis contributed equally to this work and are co-senior authors.
Disclosure: The authors declare that they have nothing to disclose.
A.J. is supported by the Women’s Heart and Brain Award, Heart and Stroke Foundation of Canada and Health Canada and a Merit Award, University of Toronto; C.J.D.W. is supported by the Hold’em for Life Early Career Professor in Cancer Research, a University limited term Named Professorship at the University of Toronto. N.C. is supported by the Sherif and Mary-Lou Hanna Chair in Surgical Oncology.
The study protocol was approved by the Mount Sinai Hospital Research Ethics Board (#22-0110-C).
Additional/raw data are available upon request from the corresponding authors (AJ & CJDW).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Tsugawa Y, Jena AB, Orav EJ, et al. Age and sex of surgeons and mortality of older surgical patients: observational study. BMJ. 2018;361:k1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallis CJD, Jerath A, Coburn N, et al. Association of surgeon-patient sex concordance with postoperative outcomes. JAMA Surg. 2022;157:146–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Etherington N, Deng M, Boet S, et al. Impact of physician’s sex/gender on processes of care, and clinical outcomes in cardiac operative care: a systematic review. BMJ Open. 2020;10:e037139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallis CJD, Jerath A, Aminoltejari K, et al. Surgeon sex and long-term postoperative outcomes among patients undergoing common surgeries. JAMA Surg. 2023;158:1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallis CJ, Ravi B, Coburn N, et al. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115:8569–8574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallis CJD, Jerath A, Kaneshwaran K, et al. Association between surgeon and anesthesiologist sex discordance and postoperative outcomes: a population-based cohort study. Ann Surg. 2022;276:81–87. [DOI] [PubMed] [Google Scholar]
- 8.Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177:206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallis CJ, Jerath A, Ikesu R, et al. Association between patient-surgeon gender concordance and mortality after surgery in the United States: retrospective observational study. BMJ. 2023;383:e075484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myles PS, Shulman MA, Heritier S, et al. Validation of days at home as an outcome measure after surgery: a prospective cohort study in Australia. BMJ Open. 2017;7:e015828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jerath A, Austin PC, Wijeysundera DN. Days alive and out of hospital: validation of a patient-centered outcome for perioperative medicine. Anesthesiology. 2019;131:84–93. [DOI] [PubMed] [Google Scholar]
- 12.McIsaac DI, Fottinger A, Sucha E, et al. Association of frailty with days alive at home after cardiac surgery: a population-based cohort study. Br J Anaesth. 2021;126:1103–1110. [DOI] [PubMed] [Google Scholar]
- 13.McIsaac DI, Talarico R, Jerath A, et al. Days alive and at home after hip fracture: a cross-sectional validation of a patient-centred outcome measure using routinely collected data. BMJ Qual Saf. 2023;32:546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tevis SE, Kennedy GD. Postoperative complications and implications on patient-centered outcomes. J Surg Res. 2013;181:106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams JI, Höher J, Lauterbach KW. Health Services Research. In: Troidl H, McKneally MF, Mulder DS, et al. , eds. Surgical Research: Basic Principles and Clinical Practice. New York, NY: Springer New York:533–554. [Google Scholar]
- 17.Schull MJ, Azimaee M, Marra M, et al. ICES: data, discovery, better health. Int J Popul Data Sci. 2020;4:1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hallet J, Jerath A, Turgeon AF, et al. Association between anesthesiologist volume and short-term outcomes in complex gastrointestinal cancer surgery. JAMA Surg. 2021;156:479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taran S, Coiffard B, Huszti E, et al. Association of days alive and at home at day 90 after intensive care unit admission with long-term survival and functional status among mechanically ventilated patients. JAMA Netw Open. 2023;6:e233265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jerath A, Austin PC, Ko DT, et al. Socioeconomic status and days alive and out of hospital after major elective noncardiac surgery: a population-based cohort study. Anesthesiology. 2020;132:713–722. [DOI] [PubMed] [Google Scholar]
- 21.Local health integration networks (operating as home and community care support services) Available at: https://www.pas.gov.on.ca/Home/Agency/647. Accessed October 31, 2023. [Google Scholar]
- 22.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat - Simul Comput. 2009;38:1228–1234. [Google Scholar]
- 23.Nakayama A, Morita H, Fujiwara T, et al. Effect of treatment by female cardiologists on short-term readmission rates of patients hospitalized with cardiovascular diseases. Circ J. 2019;83:1937–1943. [DOI] [PubMed] [Google Scholar]
- 24.Silliman RA, Demissie S, Troyan SL. The care of older women with early-stage breast cancer: what is the role of surgeon gender? Med Care. 1999;37:1057–1067. [DOI] [PubMed] [Google Scholar]
- 25.Hershman DL, Buono D, McBride RB, et al. Surgeon characteristics and receipt of adjuvant radiotherapy in women with breast cancer. J Natl Cancer Inst. 2008;100:199–206. [DOI] [PubMed] [Google Scholar]
- 26.Bertakis KD, Helms LJ, Callahan EJ, et al. The influence of gender on physician practice style. Med Care. 1995;33:407–416. [DOI] [PubMed] [Google Scholar]
- 27.Lurie N, Slater J, McGovern P, et al. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993;329:478–482. [DOI] [PubMed] [Google Scholar]
- 28.Lou Z, Yan F-H, Zhao Z-Q, et al. The sex difference in basic surgical skills learning: a comparative study. J Surg Educ. 2016;73:902–905. [DOI] [PubMed] [Google Scholar]
- 29.Chiu H-Y, Kang Y-N, Wang W-L, et al. Gender differences in the acquisition of suturing skills with the da Vinci surgical system. J Formos Med Assoc. 2020;119:462–470. [DOI] [PubMed] [Google Scholar]
- 30.Wallis CJD, Jerath A, Aminoltejari K, et al. Surgeon sex and health care costs for patients undergoing common surgical procedures. JAMA Surg. 2024;159:151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.