Abstract
Spinal angiolipomas are rare benign tumors composed of mature adipose cells and blood vessel walls. We report the case of a patient with a spinal epidural angiolipoma who presented with paraplegia and was treated by urgent tumor resection and decompression. The patient was a 79-year-old man who presented to our hospital with a 6-month history of numbness in both lower limbs. Plain CT showed a tumor-like lesion with a predominantly fatty component on the dorsal epidural surface at the Th2-4 level, and contrast-enhanced CT showed a relatively strongly heterogeneously enhancing lesion. Gadolinium (Gd) -enhanced MRI also showed a well-defined spindle-shaped lesion measuring 2.4 × 1.0 × 6.5 cm in size that was visualized as a heterogeneous high signal intensity on both T1- and T2-weighted images and showed strong heterogeneous enhancement on fat-saturated Gd-enhanced T1-weighted images. We performed Th1-4 laminectomy and tumor resection and the patient was discharged home, with no numbness in the lower limbs.
Keywords: Angiolipoma, Spinal angiolipoma, Spinal tumor, CT, MRI
Introduction
Spinal angiolipomas are rare benign tumors composed of mature adipose cells and blood vessel walls; they are reported to account for 0.04%-1.2% of all spinal tumors and for 2%-3% of all epidural spinal tumors [1,2]. They are more common in middle-aged women and are generally found on the dorsal surface of the thoracic epidural space. Although they are benign in nature, as they grow, they could compress the spinal cord and dural sac, causing sensory and motor deficits and localized pain, depending on their localization. Accurate preoperative imaging diagnosis of these tumors is of great clinical significance because malignant transformation of spinal angiolipoma is rare, and once removed, the neurological disorders associated with compression by the tumors were expected to be improved. In this report, we describe a case of spinal epidural angiolipoma, wherein the patient presented with paraplegia and was treated by urgent tumor resection and decompression, along with a review of the literature.
Case presentation
A 79-year-old man presented to our hospital with 6-month history of numbness in both lower limbs and a tendency to fall easily. There were no abnormal findings in the past medical history or family history, and laboratory investigations showed no abnormalities. A detailed physical examination revealed moderate symmetrical weakness in the lower limbs and sub-Th4 sensory disorder, but no bladder or rectal dysfunction. Contrast-enhanced CT and contrast-enhanced MRI were then performed. A plain CT showed a tumor-like lesion with a predominantly fatty component on the dorsal epidural surface at the Th2-4 level, and contrast-enhanced CT showed a relatively strongly heterogeneously enhancing lesion (Fig. 1). Contrast-enhanced MRI also showed a well-defined spindle-shaped mass lesion measuring 2.4 × 1.0 × 6.5 cm in size at the Th2-4 level that was visualized as a heterogeneous high signal intensity on T1-weighted and T2-weighted images, and showed strong heterogeneous enhancement on fat-saturated contrast-enhanced T1-weighted images. The tumor caused severe narrowing of the dural sac and severe spinal cord compression (Fig. 2). We treated the patient by Th1-4 laminectomy and epidural tumor resection. The tumor was diagnosed by postoperative histopathology as an epidural angiolipoma because it was composed of mature adipocytes and numerous internal capillaries, with fibrin thrombus formation observed in some capillaries (Fig. 3). The postoperative course was good, and the patient was discharged from the hospital with no numbness in the lower limbs and stable gait. No recurrence has been observed during follow-up.
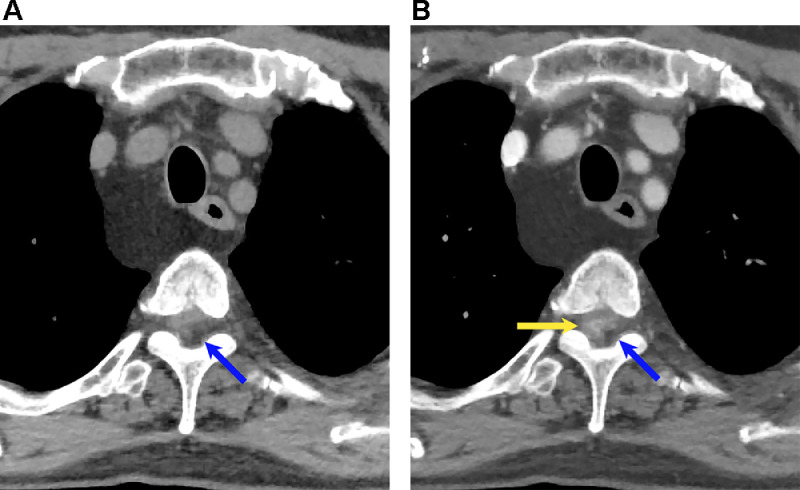
Fig. 1.
Axial CT images of the thoracic spine without enhancement (A) and with enhancement (B). These images show a heterogenous fatty tumor within the thoracic canal (blue arrow), and contrast-enhanced CT (B) shows heterogenous enhancement of the mass (yellow arrow).
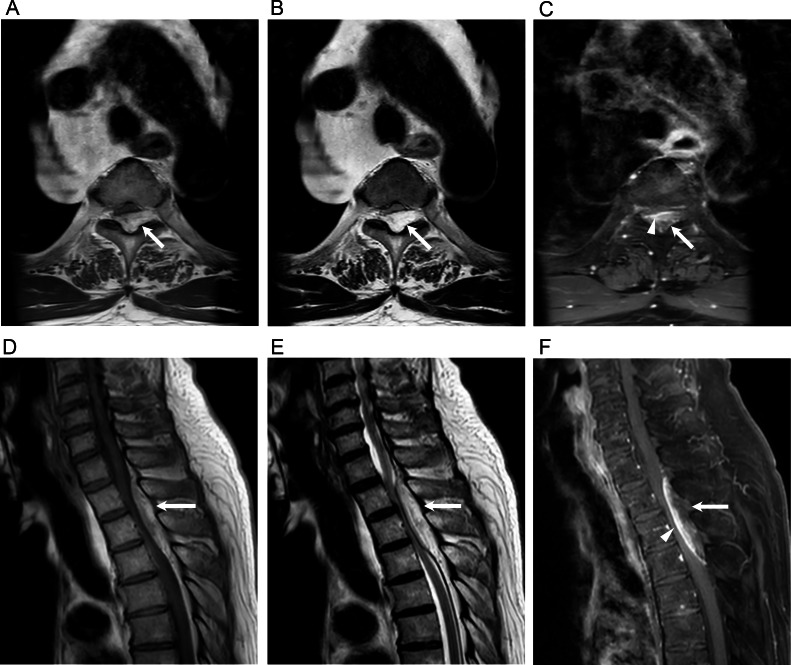
Fig. 2.
T1- (A, D), T2-weighted (B, E) and fat-saturated contrast-enhanced T1-weighted (C, F) axial and sagittal MRIs showing a heterogenous high-signal intensity on T1- and T2-weighted images (white arrow) and a heterogeneously enhancing lesion on fat-saturated contrast-enhanced T1-weighted images (arrow head).
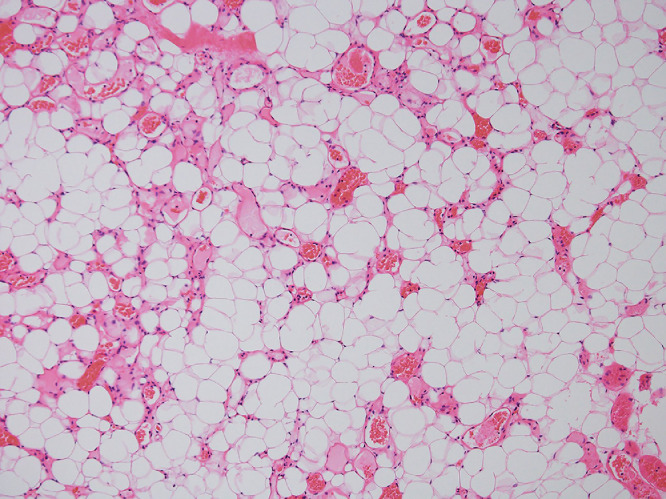
Fig. 3.
Histopathological image (hematoxylin and eosin staining, × 100) showing mature adipose tissue with numerous small blood vessels.
Discussion
Angiolipomas are tumors that are generally found in the soft tissues of the extremities, trunk, and neck. They rarely occur on the epidural surface, and epidural spinal angiolipoma was first described by Berenbruch in 1890 [3,4]. It is more common in women, although no significant difference in the incidence has been reported between the 2 sexes, and it is more common in the 40-60 years age group. When it occurs in the spine, it is most often seen in the dorsal thoracic epidural space and most commonly at the Th 5 vertebral level [5]. In the patient reported herein, the spindle-shaped lesions were detected at the Th2-4 level.
Although the factors predisposing to the development of angiolipomas have not yet been clarified, some authors suggest that they are the result of differentiation of pluripotential mesenchymal cells upon stimulation [6], while others have suggested that hormones may be involved, since angiolipomas are more common around menopause and change in size in association with hormonal changes, such as pregnancy. This patient reported herein was a male, and the relationship to hormonal balance seemed unclear. Lin et al. classified the lesions into invasive and noninvasive types, with the invasive type known to occur relatively more often on the ventral aspect of the dural sac, suggesting invasion from the vertebral venous plexus [7]. Patients usually present with neurological symptoms, such as dysesthesia and dyskinesia associated with spinal cord and dural sac compression, that could progress to paralysis of the lower limbs and vesicorectal disturbances. In terms of the neurological symptoms, sensory disturbances are known to precede motor disturbances [8]. In general, the tumors usually show slow increase in size, but rapid enlargement may occur due to intra-tumor hemorrhage, hormonal changes caused by pregnancy, weight gain, and increased circulating blood volume [8,9].
CT shows the tumor as a fat density, reflecting the abundant adipose tissue within the tumor. MRI also shows characteristic findings, such as iso-high signal intensity on T1-weighted images and high signal intensity on T2-weighted images, reflective of fatty components; the fatty components are also strongly enhanced by gadolinium (Gd), with the degree of enhancement varying depending on the ratio of the fatty and vascular components. Although they show strong enhancement, flow voids are rarely seen in these tumors. In the case presented here, both the T1- and T2-weighted images showed internally heterogeneous high signal intensities reflecting the abundant fat components, and fat-saturated contrast-enhanced T1-weighted images showed strong, internally heterogeneous enhancement.
In relation to the tumor morphology, Si et al. [10] classified tumors that are confined to the spinal canal as type I and those that extend outside the canal through the intervertebral foramen and have a dumbbell-shape as type II. Type I tumors without internal fat are defined as type IA, and Type I tumors containing fat as type IB. In past reports, the frequency of type I was high, and it is estimated that about 80%-90% of all cases are type I tumors [5,11]. Type I tumors are well-defined spindle-shaped tumors, with an average craniocaudal extent of about 2.5 vertebrae, although some large tumors exceeding 11 vertebrae have also been reported [5,12]. Lipomas and epidural hematomas can be differentiated from these tumors, because neither of these tumors show Gd-contrast enhancement. Spinal lipomas differ in that they tend to occur at a younger age, are more common at the lumbar level, and may be associated with neural tube closure disorders, such as bipartite spine. Type II tumors are important to distinguish from schwannomas, meningiomas, and other lesions that are dumbbell-shaped. Although it is often possible to distinguish these lesions from each other preoperatively based on the characteristic imaging findings, the final diagnosis requires histopathological confirmation. In this case, the tumor presented as a spindle-shaped epidural tumor with a craniocaudal extent of approximately 3 vertebral levels, was confined to the dorsal spinal canal, and the CT and MR imaging findings were relatively characteristic, which allowed preoperative diagnosis.
Surgical resection is the treatment of first choice for spinal angiolipomas. Malignant transformation is rare, and in most cases, the tumors are not adherent to the dura mater. Recurrence is rare and postoperative adjuvant therapy is generally not necessary. Even invasive spinal cord angiolipomas often have a good prognosis. Patients with spinal angiolipomas usually present with neurological symptoms, such as sensory and motor disturbances, and the postoperative course is mostly favorable. Spinal angiolipomas are rare benign tumors with a predilection for the thoracic epidural space, and contrast-enhanced MRI, which often reveals characteristic findings of spinal angiolipomas, plays a significant role in the accurate preoperative diagnosis.
Patient consent
Written informed consent for the publication of this case report was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Gelabert-González M, García-Allut A. Spinal extradural angiolipoma:report of two ases and review of the literature. Eur Spine J. 2009;18(3):324–335. doi: 10.1007/s00586-008-0858-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andaluz N, Balko G, Bui H, Zuccarello M. Angiolipomas of the central nervous system. J Neurooncol. 2000;49:219–230. doi: 10.1023/a:1006492629326. [DOI] [PubMed] [Google Scholar]
- 3.Berenbruch K. Medical Faculty Universitat Tubingen; Germany: 1890. Ein fall von multiplen angiolipomen kombiniert mit eniem angiom des ruckenmarks. Tubingen. [Google Scholar]
- 4.Fourney DR, Tong KA, Macaulay RJ, Griebel RW. Spinal angiolipoma. Can J Neurol Sci. 2001;28:82–88. doi: 10.1017/s0317167100052628. [DOI] [PubMed] [Google Scholar]
- 5.Umana GE, Visocchi M, Roca E, Passanisi M, Fricia M, Tranchina MG, et al. Thoracic spinal angiolipomas: a systematic review. J Neurol A Cent Eur Neurosurg. 2022;83:161–172. doi: 10.1055/s-0041-1739217. [DOI] [PubMed] [Google Scholar]
- 6.Ehni G, Love JG. Intraspinal lipomas: report of cases, review of the literature, and clinical and pathological study. Arch NeurPsych. 1945;53(1):1–28. doi: 10.1001/archneurpsyc.1945.02300010011001. [DOI] [Google Scholar]
- 7.Lin JJ, Lin F. Two entities in angiolipomas. A study of 459 cased of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974;34:720–727. doi: 10.1002/1097-0142(197409)34:3≤720::aid-cncr2820340331≥3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 8.Horiuchi K, Yamada T, Sakai K, Okawa A, Arai Y. Hemorrhagic sudden onset of spinal epidural angiolipoma. Case Rep Orthop. 2018;2018 doi: 10.1155/2018/5231931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsutsumi S, Nonaka Y, Abe Y, Yasumoto Y, Ito M. Spinal angiolipoma in a pregnant woman presenting with acute epidural hemorrhage. J Clin Neurosc. 2011;18(6):849–851. doi: 10.1016/j.jocn.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 10.Si Y, Wang Z, Pan Y, Lin G, Yu T. Spinal angiolipoma: etilogy, imaging findings, classification, treatment, and prognosis. Eur Spine J. 2014;23:417–425. doi: 10.1007/s00586-013-3073-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu S, Hu CH, Hu XY, Wang XM, Dai H, Fang XM, et al. MRI features of spinal epidural angiolipomas. Korean J Radiol. 2013;14(5):810–817. doi: 10.3348/kjr.2013.14.5.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garg A, Gupta V, Gaikwad S, Deol P, Mishra NK, Sharma MC, et al. Spinal angiolipoma: report of three cases and review of MRI features. Australas Radiol. Mar 2002;46(1):84–90. doi: 10.1046/j.1440-1673.2001.01001.x. [DOI] [PubMed] [Google Scholar]