Abstract
Background
Children with ADHD demand for effective intervention with minimum side effect to improve executive function (EF) and health well-being.
Method
This study used a three-arm partially-blinded randomized controlled trial to test the effects of two different kinds of 8-week game-based training programs (game-based HIIT program, GameHIIT; and game-based structured aerobic exercise program, GameSAE) on EF and other health indicators of children with ADHD, which was compared with a non-treatment control group.
Results
A total of 49 children with ADHD completed the program. Analyses of EF tests and parental survey indicated that (i) there is no significant intragroup difference among all measures between pre-/post-intervention tests for two game-based intervention groups. The only significant intergroup difference was observed in self-monitor score of parent-reported child's EF between GameSAE group and the control (large effect). Similarly, cerebral hemodynamic responses also found no significant group effect for all EF tests. However, the time effects were observed in several channels in the GameHIIT group in two EF tests (Color Words Stroop Test and Tower of London Test). No significant change of participants' overall ADHD symptoms was found in the pre-/post-tests for three groups. Nonetheless, further analyses revealed that both of two game-based training programs exhibited the significant positive effects on child's PA levels and the large effects on levels of physical fitness, when they were compared to the control.
Conclusion
By this study, a significant enhancement in physical fitness and PA levels were found in both game-based PA interventions when they were compared with control group. However, the effectiveness of game-based PA interventions on improving EF or reducing ADHD symptoms remains unclear. This implies that a larger intervention dosage or a tailored intervention design may be warranted to improve the EF of children with ADHD.
Keywords: ADHD, children, Effectiveness, Game-based, HIIT
1. Introduction
Worldwide, 5.9%–7.1 % of children are currently diagnosed with attention-deficit/hyperactivity disorder (ADHD).1,2 The most common symptoms include inattention, hyperactivity/impulsivity, or combined.3 Children with ADHD often demonstrate executive dysfunction, which is believed to be responsible for many of their commonly observed behavioral problems.1,4 Executive function (EF) is generally regarded as a high-level cognitive process, which plays an important role in many aspects of a child's development such as successful learning, intake of healthy food, academic achievement, and sports participation.5 Although different methods (e.g., medication, psychotherapy, behavior management, etc.) have been applied to treat ADHD, physical activity (PA) has been regarded as one of the most effective ways.6, 7, 8 PA has not been reported to have those severe negative side effects that are often associated with pharmacological interventions.8
In general, there is evidence showing the acute positive effects of exercise on cognitive function including EF and attention.9 As for chronic effects, several studies have found that long-term exercise may have medium to large effects on inhibition and attention in children with ADHD.10 In addition, a recent meta-analysis reported the preliminary effectiveness of structured PA on well-being of children with ADHD in terms of reduction of inattention and mental health issues, and improvement of EF and physical fitness.11 However, existing evidence gathers around mixed exercise programs with low-to moderate-intensity aerobic nature (i.e., running and stationary cycling have been the most common exercise modes); however, the effect of mixed exercise programs on improving EF or attention in children with ADHD are still inconsistent.12, 13, 14, 15
The habitual PA patterns in children are usually games or “unpredictable” sports activities such as football, basketball.16 When it is compared to structured aerobic exercise used in most of previous studies, games-based PA may provide a more attractive, acceptable, sustainable and enjoyable exercise model for young children.17 Although mixed exercise protocols have generally been used in intervention programs for children with ADHD, only a few studies involved team sport-based games as part of their exercise intervention.14,18 A 12-week table tennis exercise program was reported to have positive effects on the gross motor skills and inhibitory control in the ADHD training group, which was compared with their peers in ADHD non-training group or the healthy controls.19
Recently, high-intensity interval training (HIIT) has emerged as feasible and efficacious for increasing physical health outcomes, including the executive performance of children and adolescents.20,21 These benefits may extend to children with ADHD. One recent study found that a traditional HIIT was more effective for children with ADHD in improving motor skills, self-esteem, friends, competence, and subjective ratings of attention, than standard multimodal therapy (TRAD).22 Although a traditional HIIT program can be completed in a short period while providing physiological adaptations equivalent to those provided by longer sessions of traditional aerobic training, it generally involves shuttle runs or cycling,20,23,24 activities that many children are not likely to enjoy. This may lead to their subsequent disinterest in the program. In contrast to running or cycling, team games closely resemble the habitual physical activity patterns of children and so they may find these activities more acceptable and enjoyable.21 In previous studies, some game-based activities have been used as part of mixed exercise programs to promote the physical/mental health of children with ADHD. However, most of these game-based activities are actually low-to moderate-intensity exercise in nature. Therefore, if the demands of HIIT are embedded in team games, this may integrate the benefits of both game-based activities and HIIT.
Therefore, to inform the development of specific exercise programs targeted at children with ADHD, this study aimed to investigate the effectiveness of an 8-week game-based HIIT program (GameHIIT) on children with ADHD, which was compared with a game-based structured aerobic exercise program (GameSAE), and/or a non-treatment control group (Control). Primary outcomes of this study include EF, and the embedded mechanism related to cerebral hemodynamic responses, and secondary outcomes are the anthropometric measures, overall ADHD symptoms, PA levels, and physical fitness.
2. Method
2.1. Participants and sample size
The inclusion criteria were (1) Chinese children aged 8–13 years; (2) a clinical diagnosis of ADHD by developmental pediatricians or clinical psychologists/psychiatrists; (3) a physician/psychologist's recommendation for participation. The exclusion criteria were: (1) diagnosed with a major neurodevelopmental or psychiatric disorder (e.g., autism spectrum disorder, intellectual disability, etc.); (2) acute:/chronic diseases that may affect engagement in physical activity; and (3) a tendency to experience convulsions.
According to the sample size calculated using G*Power 3.1, to elucidate the differences in the executive function tests with a statistical power of 0.9, a conservative effect size of 0.65 was adopted based on a previous systematic review, which suggested the average effect size calculated regarding the effect of exercise on executive function in children with ADHD.25 With a two-tailed alpha level of 0.05, it was determined that 10 participants per group will provide adequate power to detect statistically significant differences. Assuming a 30 % loss in the intervention, at least 42 eligible participants should be recruited to achieve the planned sample.
Participants were recruited from 15 different parties including community organizations, professional institutes, and local schools (both regular and special schools). Informed consent was obtained from the school principal, parents, and participating children before the study began. Ethics approval was obtained from the Human Research Ethics Committee of the University.
2.2. Study design
A three-arm partially-blinded randomized controlled trial (RCT) was conducted to evaluate the effects of two different kinds of 8-week game-based training programs on the EF of children with ADHD. The protocol was registered at ClinicalTrials.gov and previously published.26 Participants were randomly assigned to the GameHIIT group, the GameSAE group, or a non-treatment control group. Participants were not blinded to treatment allocation because of the intervention nature. To avoid contamination between treatment groups, intervention deliverers were provided with a list of students in the intervention program. Only those on the list participated in the intervention. During the 8-week intervention period, participants in Control group maintained their regular PA levels. All assessments were conducted by trained research staff blinded to group allocation.
Intervention protocols of GameHIIT group. A specially designed game-based training program with HIIT in nature was delivered to the participants as an after-school activity for 8 weeks. A small-sided games (SSGs) approach in rugby were adopted in this intervention program as it was effective in developing physical and technical capabilities in children,27 and provided similar physical stimulus, regardless of the experience of the children.28 Importantly, rugby has been introduced in a large scale to primary and secondary schools in Hong Kong. There were two training sessions each week. In each training session, there were four sets of training programs separated by 3 min of passive recovery in accordance with a previous study.29 Each set of activities lasted for around 5 min; therefore, the total duration of each training session was approximately 30 min. A brief description of the proposed training program was given in Supplemental Material Table S1. A small group size (4–6 children per group) was adopted to facilitate individual supervision and adaption of the exercise program. Also, certain social, cognitive and coordinative elements related to EF were included. All the training programs were organized for participants after school hours. A qualified rugby coach was hired to implement the training program. To encourage maintenance of an appropriate level of exercise intensity, participants were fitted with heart rate monitors (Polar H7), which were connected to a central iPad application. The coach was able to view real-time HR data during training. The exercise intensity was adjusted to ensure that HR can reach the target HR zone.
Intervention protocols of GameSAE group. Participants attended a tailor-made game-based after-school exercise training program designed by the research group.30 Similar to GameHIIT, the intervention comprised 8 weeks of structured aerobic exercise (SAE) sessions, lasting 1 h on average in each session and up to twice per week. Six to eight stations of multidimensional exercises were set up for each session. Children were instructed to finish the exercises in all stations one after another in a predetermined order. The exercise program had 3 stages and each stage lasted around two to three weeks. In the first stage, the aim was to build trust to their coaches, and paired group activities were included. In the second stage, the exercise intensity was increased to promote cardiopulmonary endurance and muscular strength. In the final stage, the exercise intensity for each session was higher than that of the previous stages and there were large group activities as well.
2.3. Procedures of measurements
Pre- (T0) and post- (T1) the 8-week intervention period, several different indicators were recorded, including EF, cerebral hemodynamic response, ADHD symptoms, PA levels, and physical fitness. Trained research staff were blinded to group allocation in all assessments. To ensure the accuracy and consistency of the measurements, a measurement training session and protocol manual, including specific instructions for conducting all assessments, were provided to the research staff. A senior researcher presented during all the testing sessions. All physical assessments were conducted in a sensitive manner (e.g., weight/waist circumference were measured in a private setting), and the EF tests and questionnaires were completed under exam-like conditions. Also, participants were instructed to follow similar diets on the test days. Only distilled water was allowed before the tests in the main trials.
2.4. Primary outcomes
Executive function (EF). EF was assessed by both objective tests and parent-reported scale. The objective EF tests were conducted by using a battery of tests on an iPad, which took approximately 20 min to complete. The battery of tests included the Colour- Wisconsin Card Sorting Test (WCST), Word Stroop Test (CWST), Tower of London Test (ToLT), and Corsi Block-tapping Test (CBTT), which are classic tasks that measure cognitive flexibility, inhibition control, organization, and working memory. In the test, both reaction time and response accuracy were recorded and analyzed. This battery was also used previously by research group to investigate the effect of exercise on cognition in young people.31 The instructions for each test were provided to the participants and they were allowed to ask questions for clarification. Participants were familiarized with the testing battery seven days prior to the main trial, and each test started with 3–6 practice stimuli to re-familiarize participants with the task at hand and eliminate any potential learning effects. In the main trial, participants completed the tests individually. In addition to the four EF tests, parent-reported Behavior Rating Inventory of Executive Function (second edition, BRIEF-II32,33) was also applied in this study with good validity (Cronbach's α = 0.873 in pre-test and 0.875 in post-test). The following variables were measured including inhibit, self-monitor, total behavioral regulation index (BRI), shift, emotional control, total emotional regulation index (ERI), initiate, working memory, plan/organize, task-monitor, organization of materials, total cognitive regulation index (CRI) and global executive composite (GEC).
Cerebral hemodynamic response. Accompanied by the EF test, the cortical hemodynamic response in the prefrontal cortex was recorded using a multi-channel fNIRS (Octamon fNIRS system, Artinis, Netherland) applying two wavelengths of near-infrared light (785 and 830 nm). The device consists of eight light sources and two detectors secured onto a head cap. The device was placed over the left and right prefrontal cortex according to the guidelines provided by the manufacturer. The data were analyzed as described in the literature.34
2.5. Secondary outcomes
Anthropometry. Body height, weight, and waist and hip circumference were measured three times. All measurements followed the Anthropometry Procedures Manual of National Health and Nutrition Examination Survey (NHANES).35
ADHD symptoms. Overall ADHD symptoms were reported by parents using the Attention-Deficit/Hyperactivity-symptoms and Normal-behaviors (SWAN) rating scale.36
Physical activity (PA). Children's leisure-time PA was determined using both an accelerometer (ActiGraph, Shalimar, USA) and a validated and modified version of the Physical Activity Questionnaire for Children (PAQ-C).37 Participating children were required to wear an accelerometer on their right hip for seven days to collect objective data of PA levels. The time on and time off of wearing the accelerometer each day were recorded, and the data was used to estimate the time spent in moderate-to-vigorous PA (MVPA). Method of using accelerometers to measure the participants' PA is included in Supplemental Material Appendix S2. The PAQ-C was a 7-day parent-reported questionnaire designed to assess daily activities from moderate to vigorous range, and the score was in a continuous range from 1 (low active) to 5 (high active).
Physical fitness. Cardiovascular fitness, muscular strength and speed-agility of participants were assessed using the ALPHA fitness test battery.38 Briefly, cardiovascular fitness was assessed by the 20m shuttle run test (Beep test); muscular strength was assessed by the handgrip strength test and standing long jump test; and speed-agility was assessed by the 4 × 10m shuttle run test.
2.6. Statistical analyses
Statistical analyses were conducted with the IBM SPSS Statistic for Windows, Version 29.0.1.0 (SPSS Inc., IBM Company Armonk, NY). All data was presented as mean and standard deviation (SD), whereas significant different was perceived as p < 0.05 during data analysis. Except the data of fNIRS, intervention effects for study outcomes were firstly examined by paired t-test to investigate the difference between pre-/post-intervention tests. Subsequently, the changes between pre-/post-tests of three groups were further compared by one-way ANOVA analysis. Effect sizes (ES) was presented as partial eta squared values (η2, for total three groups) or Hedge's g (for any two groups), if any significant difference in changes between pre-/post-intervention tests was found among three groups.
In terms of fNIRS data, after excluding those participants with poor quality of signal, a total of 35 participants (13 in GameHIIT, 13 in GameSAE, and 9 in CON) were included in subsequent analysis. The raw data was exported to MATLAB (Oxysoft2matlab version 1.86) and visually inspected to understand the signal's morphology and detect noisy channels (e.g., large head motion, and sudden amplitude changes). Then, the raw data was preprocessed by some in-built preprocessing functions in the environment of Homer3 version 1.80.2 in MATLAB R2022a. The detailed preprocessing procedures were shown on Fig. 1. After this, the concentration changes of oxyhemoglobin (HbO) and deoxyhemoglobin (HbR) were obtained. Estimation of the hemodynamic response function (HRF) was completed with the General Linear Model (GLM) using NIRS-SPM toolbox.39 The △β values (changes in β value between baseline and stimulus condition obtained in each participant at each channel) were reconstructed and submitted to a two-way repeated measures ANOVA. This is to identify the potential intervention effect on cortical activation of participants during the EF test. Post-hoc test (with Bonferroni correction) was applied if the main factor was significant. Lastly, the false discovery rate (FDR) correction was applied to the significant results from the previous steps.40,41
Fig. 1.
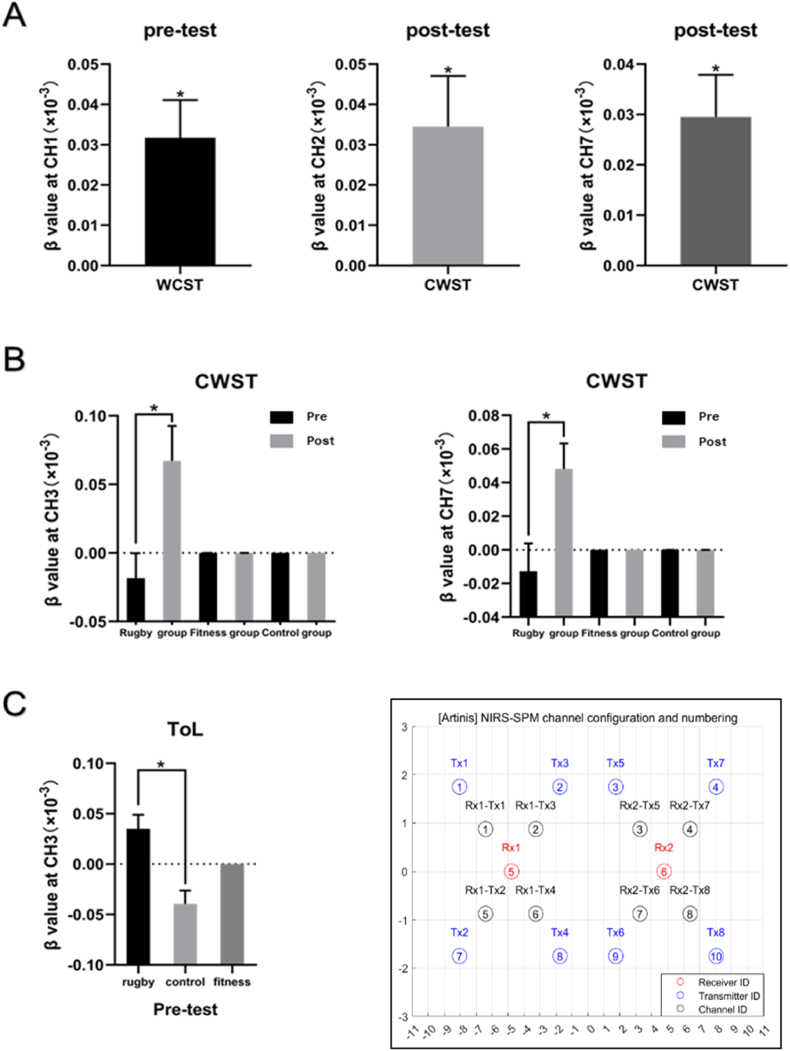
Results of brain activity.
Note. * Significant if p < 0.05. There were eight transmitter optodes and two receiver optodes, which compose of 8 channels covering the dorsolateral prefrontal cortex. The CH1, CH2, CH5 and CH6 lie in the right dorsolateral prefrontal cortex (dlPFC), while the CH3, CH4, CH7 and CH8 lie in the left dlPFC. Rugby (group) denotes GameHIIT group, and fitness (group) denotes GameSAE group.
(A) During pre-test, the brain activation of participants at CH1 while performing Wisconsin Card Sorting Test (WCST) was significantly higher than baseline. During post-test, the brain activation of participants at CH2 and CH7 while performing the Colour-Word Stroop Test (CWST) was significantly higher than baseline. (B) In the GameHIIT group, the brain activation of participants during post-test at CH3 and CH7 was significantly higher than that during pre-test, while the difference did not exist in the other groups. (C) During pre-test, the brain activation of participants in the GameHIIT group at CH3 while performing Tower of London Test (ToLT) was significantly higher than that in the control group. Error bars represent standard errors.
3. Results
3.1. Characteristics of participants
The study was implemented from January 2021 to June 2023, during which the data collection process was heavily affected by the Covid-19 pandemic. A total of 63 children with ADHD were recruited. They were randomly assigned to three groups: GameHIIT group (n = 23), GameSAE group (n = 20), and the control group (n = 20). The attrition rate of participants is 22.2 %. At last, a total of 49 children with ADHD (GameHIIT group: n = 16, GameSAE group: n = 15; Control group: n = 18) completed the programme and the post-intervention tests, whose data was enrolled in the further analyses. Among the 49 participants who provided valid data, (i) they were 10.10 ± 1.83 years old on average; (ii) 75.5 % of them were males; and (iii) regarding ADHD type, 4.1 % of them were diagnosed as having hyperactivity or impulsiveness, 24.5 % of them were affected with inattention, and other 71.4 % of them had the combined ADHD types.
3.2. Executive function and brain activity
Results of intragroup difference and intergroup difference are presented in Table 1, Table 2, respectively. Detailed results are included in Supplemental Material, whereas Table S3 presents the number of participants involved in each test, and mean and SD of study groups in each test is shown in Table S4.
Table 1.
Intragroup difference between pre-/post-intervention tests by P values of the paired t-test.
| Variables | GameHIIT | GameSAE | Control |
|---|---|---|---|
| Executive function | |||
| Parent-reported BRIEF-II | (n=14) | (n=13) | (n=18) |
| Inhibit | 0.900 | 0.673 | 0.275 |
| Self-monitor | 0.583 | 0.316 | 0.061† |
| Total Behavioral Regulation Index (BRI) | 0.864 | 0.940 | 0.105 |
| Shift | 0.671 | 0.192 | 0.595 |
| Emotional control | 0.179 | 0.616 | 0.869 |
| Total Emotional Regulation Index (ERI) | 0.425 | 0.259 | 0.784 |
| Initiate | 0.321 | 0.730 | 0.801 |
| Working memory | 0.690 | 0.522 | 0.335 |
| Plan/organize | 0.260 | 0.816 | 0.384 |
| Task-monitor | 0.283 | 1.000 | 0.231 |
| Organization of materials | 0.905 | 0.445 | 0.736 |
| Total Cognitive Regulation Index (CRI) | 0.426 | 0.874 | 0.367 |
| Global Executive Composite (GEC) | 0.753 | 0.727 | 0.287 |
| Wisconsin Card Sorting Test (WCST) | (n=11) | (n=15) | (n=15) |
| Total corrects | 0.641 | 0.320 | 0.236 |
| Percentage of corrects | 0.833 | 0.123 | 0.241 |
| Perseverative errors | 0.780 | 0.238 | 0.220 |
| Percentage of perseverative errors | 0.988 | 0.732 | 0.366 |
| Perseverative responses | 0.535 | 0.328 | 0.557 |
| Percentage of perseverative responses | 0.707 | 0.520 | 0.951 |
| Color Word Stroop Test (CWST) | (n=11) | (n=15) | (n=15) |
| Percentage of corrects | 0.514 | 0.365 | 0.624 |
| Percentage of corrects in congruent trial | 0.452 | 0.333 | 0.706 |
| Percentage of corrects in incongruent trial | 0.444 | 0.475 | 0.604 |
| Percentage of corrects in control trial | 0.919 | 0.341 | 0.715 |
| Mean reaction time | 0.820 | 0.868 | 0.652 |
| Mean reaction time in congruent trial | 0.896 | 0.125 | 0.313 |
| Mean reaction time in incongruent trial | 0.451 | 0.977 | 0.617 |
| Mean reaction time in control trial | 0.715 | 0.657 | 0.534 |
| Tower of London Test (ToLT) | (n=11) | (n=15) | (n=15) |
| Total score | 0.293 | 0.132 | 0.134 |
| Mean solution time | 0.153 | 0.397 | 0.000*** |
| Mean execution time | 0.180 | 0.414 | 0.001** |
| Mean solution time of correct solutions | 0.387 | 0.460 | 0.002** |
| Mean execution time of correct solutions | 0.144 | 0.559 | 0.002** |
| Corsi Block-tapping Test (CBTT) | (n=11) | (n=15) | (n=15) |
| Total score | 0.622 | 0.327 | 0.580 |
| Anthropometric indicators | (n = 12) | (n = 11) | (n = 17) |
| Bodyfat (%) | 0.864 | 0.101 | 0.778 |
| BMI (kg/m2) | 0.823 | 0.557 | 0.088† |
| Waist-to-hip ratio | 0.211 | 0.456 | 0.544 |
| Parent-reported ADHD symptoms by SWAN | (n = 14) | (n = 13) | (n = 18) |
| Hyperactivity/impulsiveness | 0.885 | 0.289 | 0.917 |
| Inattention | 0.090† | 0.524 | 0.553 |
| Physical fitness | (n = 12) | (n = 11) | (n = 17) |
| Left handgrip (kg) | 0.212 | 0.082† | 0.429 |
| Right handgrip (kg) | 0.313 | 0.003** | 0.811 |
| Long Jump (cm) | 0.252 | 0.048* | 0.057† |
| 4 × 10m Shuttle Run (s) | 0.028* | 0.647 | 0.243 |
| Beep test (level) | 0.637 | 0.006** | 0.666 |
| PA levels | |||
| Parent-reported PA level by PAQ | (n=14) | (n=13) | (n=12) |
| Spare time | 0.426 | 0.746 | 0.891 |
| PE class | 0.720 | 1.000 | 0.017* |
| Recess time | 0.089† | 0.071† | 0.555 |
| Lunch time | 1.000 | 0.028* | 0.104 |
| After school | 0.336 | 1.000 | 0.082† |
| Evening | 0.021* | 1.000 | 0.767 |
| Weekend | 0.055† | 0.721 | 0.491 |
| Seven days | 0.426 | 0.584 | 0.586 |
| PAQ-C | 0.037* | 0.209 | 0.447 |
| Daytime activity by accelerometer | (n=14) | (n=13) | (n=18) |
| % Sedentary | 0.116 | 0.900 | 0.785 |
| % Light | 0.007** | 0.638 | 0.617 |
| % Moderate | 0.425 | 0.399 | 0.411 |
| % MVPA per day | 0.407 | 0.399 | 0.411 |
Note. Significant different if P value < 0.05*, <0.01**, <0.001***; marginal difference if P value < 0.10†. Sample sizes of three groups in different tests are presented in parentheses. GameHIIT denotes the intervention group of a rugby-game-based high-intensity interval training. GameSAE denotes the compared group of a game-based structured aerobic exercise training. Control denotes a non-treatment group. BRIEF-II: Behavior Rating Inventory of Executive Function (version II); SWAN: Child ADHD Symptom Assessment; BMI: body-mass index; PAQ-C: Physical Activity Questionnaire for Older Children; PA: physical activity; MVPA: moderate-to-vigorous intensity physical activity; PE: physical education.
Table 2.
Intergroup difference of changes between pre-/post-intervention tests by P values of one-way ANOVA test.
| Variables | Total | GameHIIT vs. GameSAE |
GameHIIT vs. Control |
GameSAE vs. Control |
|---|---|---|---|---|
| Executive function | ||||
| Parent-reported child's executive function by BRIEF-II | ||||
| Inhibit | 0.672 | 0.695 | 0.337 | 0.650 |
| Self-monitor | 0.138 | 0.253 | 0.412 | 0.048* |
| Total Behavioral Regulation Index (BRI) | 0.441 | 0.865 | 0.321 | 0.251 |
| Shift | 0.440 | 0.270 | 0.980 | 0.254 |
| Emotional control | 0.583 | 0.314 | 0.470 | 0.716 |
| Total Emotional Regulation Index (ERI) | 0.326 | 0.144 | 0.601 | 0.295 |
| Initiate | 0.857 | 0.674 | 0.599 | 0.945 |
| Working memory | 0.495 | 0.500 | 0.629 | 0.238 |
| Plan/organize | 0.902 | 0.657 | 0.875 | 0.752 |
| Task-monitor | 0.656 | 0.506 | 0.849 | 0.374 |
| Organization of materials | 0.848 | 0.570 | 0.735 | 0.787 |
| Total Cognitive Regulation Index (CRI) | 0.877 | 0.711 | 0.916 | 0.621 |
| Global Executive Composite (GEC) | 0.889 | 0.919 | 0.649 | 0.735 |
| Wisconsin Card Sorting Test (WCST) | ||||
| Total corrects | 0.241 | 0.498 | 0.101 | 0.285 |
| Percentage of corrects | 0.699 | 0.498 | 0.985 | 0.450 |
| Perseverative errors | 0.407 | 0.581 | 0.191 | 0.404 |
| Percentage of perseverative errors | 0.816 | 0.849 | 0.701 | 0.533 |
| Perseverative responses | 0.579 | 0.966 | 0.382 | 0.366 |
| Percentage of perseverative responses | 0.928 | 0.932 | 0.722 | 0.769 |
| Color Word Stroop Test (CWST) | ||||
| Percentage of corrects | 0.910 | 0.763 | 0.670 | 0.892 |
| Percentage of corrects in congruent trial | 0.902 | 0.852 | 0.658 | 0.780 |
| Percentage of corrects in incongruent trial | 0.958 | 0.902 | 0.774 | 0.858 |
| Percentage of corrects in control trial | 0.808 | 0.527 | 0.627 | 0.872 |
| Mean reaction time | 0.972 | 0.935 | 0.818 | 0.872 |
| Mean reaction time in congruent trial | 0.666 | 0.563 | 0.819 | 0.382 |
| Mean reaction time in incongruent trial | 0.839 | 0.556 | 0.751 | 0.768 |
| Mean reaction time in control trial | 0.999 | 0.996 | 0.975 | 0.977 |
| Tower of London Test (ToLT) | ||||
| Total score | 0.951 | 0.911 | 0.761 | 0.834 |
| Mean solution time | 0.316 | 0.999 | 0.215 | 0.179 |
| Mean execution time | 0.503 | 0.772 | 0.276 | 0.382 |
| Mean solution time of correct solutions | 0.540 | 0.748 | 0.495 | 0.278 |
| Mean execution time of correct solutions | 0.690 | 0.667 | 0.394 | 0.644 |
| Corsi Block-tapping Test (CBTT) | ||||
| Total score | 0.463 | 0.289 | 0.259 | 0.940 |
| Anthropometric indicators | ||||
| Bodyfat (%) | 0.863 | 0.596 | 0.718 | 0.826 |
| BMI (kg/m2) | 0.170 | 0.665 | 0.181 | 0.080† |
| Waist-to-hip ratio | 0.299 | 0.226 | 0.145 | 0.904 |
| Parent-reported ADHD symptoms by SWAN | ||||
| Hyperactivity/impulsiveness | 0.810 | 0.534 | 0.635 | 0.847 |
| Inattention | 0.294 | 0.160 | 0.881 | 0.180 |
| Physical fitness | ||||
| Left handgrip (kg) | 0.982 | 0.900 | 0.853 | 0.963 |
| Right handgrip (kg) | 0.539 | 0.690 | 0.504 | 0.282 |
| Long Jump (cm) | 0.015* | 0.755 | 0.021* | 0.011* |
| 4 × 10m Shuttle Run (s) | 0.017* | 0.091† | 0.005** | 0.293 |
| Beep test (level) | 0.498 | 0.392 | 0.815 | 0.252 |
| PA levels | ||||
| Parent-reported PA level by PAQ | ||||
| Spare time | 0.852 | 0.660 | 0.605 | 0.931 |
| PE class | 0.216 | 0.767 | 0.166 | 0.102 |
| Recess time | 0.738 | 0.802 | 0.596 | 0.447 |
| Lunch time | 0.283 | 0.224 | 0.142 | 0.778 |
| After school | 0.396 | 0.421 | 0.554 | 0.179 |
| Evening | 0.101 | 0.089† | 0.051† | 0.765 |
| Weekend | 0.440 | 0.211 | 0.423 | 0.671 |
| Seven days | 0.573 | 0.295 | 0.642 | 0.577 |
| PAQ-C | 0.650 | 0.422 | 0.435 | 0.995 |
| Daytime activity by accelerometer | ||||
| % Sedentary | 0.642 | 0.552 | 0.362 | 0.751 |
| % Light | 0.577 | 0.437 | 0.334 | 0.843 |
| % Moderate | 0.864 | 0.904 | 0.600 | 0.698 |
| % MVPA per day | 0.862 | 0.903 | 0.597 | 0.696 |
Note. Significant different if P value < 0.05*, <0.01**, <0.001***; marginal different if P value < 0.10†. GameHIIT denotes the intervention group of a rugby-game-based high-intensity interval training. GameSAE denotes the compared group of a game-based structured aerobic exercise training. Control denotes a non-treatment group. BRIEF-II: Behavior Rating Inventory of Executive Function (version II); SWAN: Child ADHD Symptom Assessment; BMI: body-mass index; PAQ-C: Physical Activity Questionnaire for Older Children; PA: physical activity; MVPA: moderate-to-vigorous intensity physical activity; PE: physical education.
According to Table 1, Table 2, there is no significant intragroup difference among all EF measures between T0 and T1 for two game-based intervention groups (either parent-reported child's EF or objective EF tests, see Table 1). In contrary, a significant overall improvement was observed in the performance of ToLT in the Control group (all p < 0.05). Furthermore, Table 2 shows that the only significant intergroup difference was observed in self-monitor score of parent-reported child's EF measured by BRIEF-II between participants of GameSAE group and Control group (Hedge's g = 0.743, 95%CI: 0.017 to 1.458, large effect, p = 0.048), whereas self-monitor score marginally decreased in Control group between T0 and T1 (p = 0.061).
Furthermore, relationships between brain activity and two EF tests (i.e., CWST and ToLT) were found in this study (Fig. 1). Given CWST, the repeated measures ANOVA revealed a significant main effect of time at CH8 (F(1,31) = 4.877, p < 0.05, η2 = 0.136). No significant interaction effect had been observed. Pairwise comparison found significant difference at CH1(mean difference = 0.000053, p < 0.05, η2 = 0.142), CH3 (mean difference = 0.000086, p < 0.01, η2 = 0.233), and CH7 (mean difference = 0.000061, p < 0.01, η2 = 0.203) between pretest and posttest in GameHIIT group. After FDR correction, the significant effect only remained at CH3 and CH7 between pretest and posttest in GameHIIT group. Regarding ToLT, the repeated measures ANOVA revealed a significant main effect of group at CH2 (F(1,31) = 3.913, p < 0.05, η2 = 0.202), and CH3 (F(1,31) = 3.594, p < 0.05, η2 = 0.188). No significant interaction effect had been observed. Pairwise comparison found significant difference at CH2 (mean difference = −0.000040, p < 0.05, η2 = 0.202) between GameHIIT and CON, CH3 (mean difference = −0.000074, p < 0.01, η2 = 0.325) between GameHIIT and CON at pre-timepoint, CH3 (mean difference = −0.000058, p < 0.05, η2 = 0.325) between GameSAE and CON at pre-timepoint, CH7 (mean difference = −0.000060, p < 0.05, Partial η2 = 0.181) between GameHIIT and CON at post-timepoint, and CH7 (mean difference = 0.000077, p < 0.05, η2 = 0.159) between pre-timepoint and post-timepoint in GameHIIT group. After FDR correction, the only survived difference of brain activity between GameHIIT and CON was found in CH3 at the pre-timepoint. However, no significant result was found by the two-way repeated measures ANOVA for relationships between brain activity and WCST/CBTT.
3.3. Physical fitness and PA levels
Among the study outcomes, significant intragroup enhancements were revealed in levels of physical fitness and PA levels of two game-based intervention groups (p < 0.05). These include (i) levels of physical fitness, i.e., right-handgrip (GameSAE), long-jump (GameSAE), 4 × 10m shuttle run (GameHIIT), and beep test (GameSAE); (ii) parent-reported PA levels, including lunch time PA (GameSAE) and evening PA (GameHIIT); and (iii) percentage of daytime exposed to light measured by accelerometer (GameHIIT). However, unfavourable changes were found in control group regarding BMI (a marginal increase, p = 0.088), long jump test (a marginal decrease, p = 0.057), and PA levels in PE class (a significant decrease, p = 0.017). Furthermore, significant intergroup differences were observed among three groups in the long jump test [F(2,37) = 4.675, η2 = 0.202, 95%CI: 0.008 to 0.384, large effect, p = 0.015] and the 4 × 10m shuttle run test [F(2, 37) = 4.559, η2 = 0.198, 95%CI: 0.006 to 0.380, large effect, p = 0.017]. Compared to Control group, large effect was found in both game-based intervention groups by long jump test, i.e., Hedge's g = 0.790, 95%CI: 0.035 to 1.532, p = 0.021 (GameHIIT), and Hedge's g = 0.921, 95%CI: 0.136 to 1.691, p = 0.011 (GameSAE). The large effect was also observed in GameHIIT group by 4 × 10m shuttle run test when it was compared with Control group (Hedge's g = −0.981, 95%CI: 1.737 to −0.209, p = 0.005).
3.4. ADHD symptomology
Neither significant intragroup nor intergroup difference was found in overall ADHD symptoms among all three groups (all p > 0.05).
4. Discussion
According to the literature, it is evident that exercise has acute positive effects on EF and attention of children with ADHD. Previous studies found that acute aerobic exercise had a positive effect on a variety of measures in children with ADHD,10 among which a medium-to-large effects on EF were reported.42,43 Long-term exercise interventions have been mainly described as an improvement of behavioral and emotional problems.9,10 However, effect of mixed exercise programs on EF of children is inconsistent in the literature. For the current study, although the design of HIIT or SAE was combined with game-based activities, the assessment results failed to support these game-based PA interventions were significantly effective to improve EF or mitigate the overall ADHD symptoms of children with ADHD. Optimization on intervention design is further warranted in terms of sport type, intensity, or duration.44
As a non-invasive and relatively cost-effective neuroimaging technology, the fNIRS technology was adopted in the present study to explore the possible mechanisms between changes of EF and cerebral hemodynamic response to cognitive tasks. Considering the quality of data, only part of participants (n = 35) was included in the final data analysis. For the results of two-way repeated measures ANOVA, no interactive effects were observed for all fNIRS measurements which is consistent with the results of EF tests. After FDR correction, the only intergroup difference was observed in pre-test β value of CH3 during ToLT test. It was significantly higher in GameHIIT group than control group. This result is unexpected and reasons remain to clarify. In accordance, we observed the improvement in the ToLT performance in the control group but not the other two groups. For the CWST, the time effect of β value was observed in CH3 and CH7 but only in GameHIIT group. In addition, results of t-test analysis indicated a significant intragroup change in β value at CH2 and CH7 among GameHIIT participants. These results indicated the potential event-related activation of left prefrontal cortex especially left dorsolateral prefrontal cortex (dlPFC) after GameHIIT training. One previous study observed the improved brain activity in the prefrontal cortex of adolescent with ADHD after aerobic exercise.13 Our previous study also suggested that left dlPFC was partially responsible for the changes of EF after high-intensity interval exercise in healthy young adults.45 Furthermore, one recent systematic review reported the increased level of HbO in the prefrontal cortex of individuals with ADHD following pharmacotherapy.46 Therefore, a high-intensity game-based exercise may exhibit similar pharmacotherapeutic effect to a certain extent. Several recent studies have tried to adopt fNIRS technology to explore the different characteristics of ADHD47, 48, 49; however, evidence for the benefits of exercise on EF is still insufficient. Therefore, future efforts are still warranted to clarify the potential mechanisms underlying the different exercise strategies which contribute to improve the EF of children and adolescents with ADHD.
Over the past two decades, meta-analytic evidence supports the significant association between the two conditions - ADHD and obesity,50 i.e., for children, pooled crude odds ratio (cOR) = 1.20, 95 % CI: 1.05 to 1.37; for adults, cOR = 1.55, 95 % CI: 1.32 to 1.81. Regarding this, Fliers et al. (2013)51 found that children with ADHD were likely to be overweight about twice as often as their typically functioning peers; conversely, children with overweight were twice as likely to exhibit elevated rates of ADHD symptoms than their counterparts with normal weight. The similar phenomenon (Table 1), that is, a marginal increase of BMI was also observed in Control group of this study. However, participants of both game-based intervention groups had a declined trend in BMI (not significant, Table 1). To date, the casual relationship between ADHD and obesity is unclear yet by the existing evidence,52 whereas a complex bidirectional association, rather than simple unidirectional ones, is more likely to be involved.50
Furthermore, previous evidence demonstrated that children with ADHD had less engagement to PA. Mercurio et al. (2021) revealed that children diagnosed with ADHD had 21 % lower chance to engage in daily PA but an increase of being unlikely to report additional PA days than their nondiagnosed peers.53 In the current study, children of Control group had a significant decrease in PA levels during PE class but a marginal increase in the after-school time. Opposite to this, participants of game-based intervention groups showed an increased PA level in the leisure time (i.e., recess, lunch time, evening, or weekend). Particularly, GameHIIT group was reported to have a significantly increase of overall PA levels by parents and demonstrated a significantly increase of time exposed to light. This may be interpreted that GameHIIT may be efficient to improve the healthy behaviors of participants and increase their outdoor PA due to the nature of a rugby sport.
Moreover, in line with previous literature,19,54 this study indicated a significant effectiveness of game-based interventions (both GameHIIT and GameSAE) on physical fitness of children with ADHD. Results of ALPHA fitness battery suggested a significant enhancement in cardiovascular fitness, muscle strength, and speed-agility after participants completed the intervention of either GameHIIT or GameSAE. In particular, GameHIIT and GameSAE were equivalent to significantly improve the physical fitness of participants, which both significantly much improved than their peers in Control group.
4.1. Strengths and limitations of this study
There are several strengths of this study. First, this is the first RCT to investigate the effect of a game-based HIIT program on well-being of children; such intervention is especially important for children with ADHD as it involved not only physical exercise, but also social behavior and sports skills. Second, the largest developmental changes in child functioning (such as EF and motor skills) occur from early childhood, through adolescence, into adulthood. Accordingly, implementing effective interventions in the early stages of life may potentially maximize their impact. Third, the potential mechanism behind the beneficial effects of game-based exercise interventions on EF was also explored. As improvement in EF has been suggested to be related to changes in prefrontal oxygenation (e.g., higher O2Hb), a non-invasive fNIRS measurement was used in this study to monitor the cerebral hemodynamic response as participants performed the cognitive tasks. Therefore, the findings of the proposed study contributed to the literature in this research area.
This study also has limitations. First, the study period had overlapped with the lockdown of the Covid-19 pandemic for 1.5 years, which largely increased the challenges and difficulties for participant recruitment and study implementation. Although the numbers of participants eventually met the minimum of planned sample size, it is still a small size, which may limit the generalization of the study findings. Second, the originally planned 12-week intervention period was shorten to 8-week with cancelling of follow-up measurements,26 because 2/3 of study period was negatively influenced by the lockdown during the Covid-19 pandemic. As a consequence, the efficacy of interventions implemented in this study may be declined, and the reasons of participants' drop out or missing in some tests were unclear. Third, because the participants were children with ADHD, the parent-reported data was inevitable, which may be influenced by recall bias or social-desirability bias (i.e., parents were not blinded to intervention). However, partial blindness was adopted by this study to minimize the bias emerged in the assessments, that is, outcome assessors of this study were blinded to the intervention received by study participants. Fourth, an unclarified information of participants’ taking medication during the intervention may confound intervention effects. Fifth, this study assessed the immediate effect after the intervention, whereas a follow-up test for long-term intervention effect is warranted for future study. Last but not least, the energy expenditure was not directly measured in the present study which may affect the findings. Further studies are required to verify whether the energy expenditure is matched between the different exercise protocols.
5. Conclusion
In this study, an 8-week game-based HIIT program (GameHIIT) targeting on children with ADHD was evaluated by a three-arm RCT in terms of effectiveness on anthropometric indicators, PA levels, physical fitness, and EF. When it was compared with an 8-week game-based structured aerobic exercise program (GameSAE), GameHIIT showed an advanced efficiency in improving child's PA levels, or an equivalent effectiveness in enhancing the physical fitness among children with ADHD. In addition, both game-based interventions demonstrated a significant higher effect on weight management of children with ADHD than the non-treatment control group. However, the present study has no obvious evidence to support the effectiveness of game-based interventions on EF or overall ADHD symptoms of children with ADHD. Future efforts are needed to optimize the intervention design.
This study was substantially supported by General Research Fund, Research Grants Council of the Hong Kong Special Administrative Region, China (Ref. No. EdUHK 18603120).
This randomized controlled trial was registered at ClinicalTrials.gov (Identifier: NCT05308758).
Author Statement
Fenghua SUN:Conceptualization; Funding acquisition; Project administration; Resources; Supervision; Roles/Writing - original draft; and Writing - review & editing.
Yuan FANG:Data curation; Formal analysis; Methodology; Software; Roles/Writing - original draft; and Writing - review & editing.
Ying Fung HO:Project administration; Investigation; Data curation; Formal analysis.
Gary Chi-Ching CHOW:Conceptualization; Project administration; Resources; Writing - review & editing.
Yaxi YANG:Data curation; Formal analysis; Software; Visualization.
Kunyi HUANG:Formal analysis; Software; Visualization.
Clare Chung-Wah YU:Conceptualization; Resources; Writing - review & editing.
Duo Liu:Conceptualization; Resources; Writing - review & editing.
Stephen Heung-Sang WONG:Writing - review & editing.
Parco Ming-Fai SIU:Writing - review & editing.
Simon B. COOPER:Writing - review & editing.
Data availability statement
The data that support the findings of this study are available from the corresponding author (Dr. Fenghua SUN), upon reasonable request.
Ethic statement
Ethics approval was obtained from the Human Research Ethics Committee of the University (Ref. No. A2018-2019-0098).
Declaration of competing interest
All authors declared no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jesf.2024.09.001.
Contributor Information
Fenghua Sun, Email: fhsun@eduhk.hk.
Yuan Fang, Email: lunajoef@gmail.com.
Ying Fung Ho, Email: hyingfung@eduhk.hk.
Gary Chi-Ching Chow, Email: ccchow@eduhk.hk.
Yaxi Yang, Email: yassee_yang@outlook.com.
Kunyi Huang, Email: kunyihuang88@gmail.com.
Clare Chung-Wah Yu, Email: clare-chung-wah.yu@polyu.edu.hk.
Duo Liu, Email: duoliu@eduhk.hk.
Stephen Heung-Sang Wong, Email: hsswong@cuhk.edu.hk.
Parco Ming-Fai Siu, Email: pmsiu@hku.hk.
Simon B. Cooper, Email: simon.cooper@ntu.ac.uk.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Huss M., Duhan P., Gandhi P., Chen C.-W., Spannhuth C., Kumar V. Methylphenidate dose optimization for ADHD treatment: review of safety, efficacy, and clinical necessity. Neuropsychiatr Dis Treat. 2017;13:1741–1751. doi: 10.2147/NDT.S130444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nunez-Jaramillo L., Herrera-Solis A., Herrera-Morales W.V. ADHD: reviewing the causes and evaluating solutions. J Pers Med. 2021;11(3):166. doi: 10.3390/jpm11030166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolraich M.L., Hagan J.F., Jr., Allan C., et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of Attention-Deficit/Hyperactivity Disorder in children and adolescents. Pediatrics. 2019;144(4) doi: 10.1542/peds.2019-2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang X., Li R., Wong S.H.S., Sum R.K.W., Sit C.H.P. The impact of exercise interventions concerning executive functions of children and adolescents with attention-deficit/hyperactive disorder: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):1–17. doi: 10.1186/s12966-021-01135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barkley R.A., Murphy K.R., Fischer M. Guilford Press; 2008. ADHD in Adults: What the Science Says; pp. 402–406. [Google Scholar]
- 6.Cerrillo-Urbina A.J., García-Hermoso A., Sánchez-López M., Pardo-Guijarro M.J., Santos Gómez J.L., Martínez-Vizcaíno V. The effects of physical exercise in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis of randomized control trials. Child Care Health Dev. 2015;41(6):779–788. doi: 10.1111/cch.12255. [DOI] [PubMed] [Google Scholar]
- 7.Jeyanthi S., Arumugam N., Parasher R.K. Effect of physical exercises on attention, motor skill and physical fitness in children with attention deficit hyperactivity disorder: a systematic review. Atten Defic Hyperact Disord. 2019;11(2):125–137. doi: 10.1007/s12402-018-0270-0. [DOI] [PubMed] [Google Scholar]
- 8.Ng Q.X., Ho C.Y.X., Chan H.W., Yong B.Z.J., Yeo W.-S. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: a systematic review. Complement Ther Med. 2017;34:123–128. doi: 10.1016/j.ctim.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 9.Suarez-Manzano S., Ruiz-Ariza A., De La Torre-Cruz M., Martínez-López E.J. Acute and chronic effect of physical activity on cognition and behaviour in young people with ADHD: a systematic review of intervention studies. journal article. Res Dev Disabil. 2018;77:12–23. doi: 10.1016/j.ridd.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Den Heijer A.E., Groen Y., Tucha L., et al. Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review. J Neural Transm. 2017;124(Suppl 1):3–26. doi: 10.1007/s00702-016-1593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun F., Fang Y., Chan C.K.M., et al. Structured physical exercise interventions and children and adolescents with attention deficit hyperactivity disorder: a systematic review and meta-analysis. Child Care Health Dev. 2023;50(1) doi: 10.1111/cch.13150. [DOI] [PubMed] [Google Scholar]
- 12.Chang Y.-K., Hung C.-L., Huang C.-J., Hatfield B.D., Hung T.-M. Effects of an aquatic exercise program on inhibitory control in children with ADHD: a preliminary study. Arch Clin Neuropsychol. 2014;29(3):217–223. doi: 10.1093/arclin/acu003. [DOI] [PubMed] [Google Scholar]
- 13.Choi J.W., Han D.H., Kang K.D., Jung H.Y., Renshaw P.F. Aerobic exercise and attention deficit hyperactivity disorder: brain research. Med Sci Sports Exerc. 2015;47(1):33–39. doi: 10.1249/MSS.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verret C., Guay M.-C., Berthiaume C., Gardiner P., Beliveau L. A physical activity program improves behavior and cognitive functions in children with ADHD: an exploratory study. J Atten Disord. 2012;16(1):71–80. doi: 10.1177/1087054710379735. [DOI] [PubMed] [Google Scholar]
- 15.Banaschewski T., Besmens F., Zieger H., Rothenberger A. Evaluation of sensorimotor training in children with ADHD. Percept Mot Skills. 2001;92:137–149. doi: 10.2466/pms.2001.92.1.137. [DOI] [PubMed] [Google Scholar]
- 16.Nassis G.P., Papantakou K., Skenderi K., et al. Aerobic exercise training improves insulin sensitivity without changes in body weight, body fat, adiponectin, and inflammatory markers in overweight and obese girls. Metabolism. 2005;54(11):1472–1479. doi: 10.1016/j.metabol.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Cooper S.B., Dring K.J., Nevill M.E. High-intensity intermittent exercise: effect on young people's cardiometabolic health and cognition. Curr Sport Med Rep. 2016;15:245–251. doi: 10.1249/JSR.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 18.Lufi D., Parish-Plass J. Sport-based group therapy program for boys with ADHD or with other behavioral disorders. Child Fam Behav Ther. 2011;33(3):217–230. [Google Scholar]
- 19.Pan C.-Y., Tsai C.-L., Chu C.-H., Sung M.-C., Huang C.-Y., Ma W.-Y. Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: a pilot study. J Atten Disord. 2019;23(4):384–397. doi: 10.1177/1087054715569282. [DOI] [PubMed] [Google Scholar]
- 20.Costigan S.A., Eather N., Plotnikoff R.C., Taaffe D.R., Lubans D.R. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1253–1261. doi: 10.1136/bjsports-2014-094490. [DOI] [PubMed] [Google Scholar]
- 21.Logan G.R., Harris N., Duncan S., Schofield G. A review of adolescent high-intensity interval training. Sports Med. 2014;44(8):1071–1085. doi: 10.1007/s40279-014-0187-5. [DOI] [PubMed] [Google Scholar]
- 22.Meßler C.F., Holmberg H.-C., Sperlich B. Multimodal therapy involving high-intensity interval training improves the physical fitness, motor skills, social behavior, and quality of life of boys with ADHD: a randomized controlled study. J Atten Disord. 2018;22(8):806–812. doi: 10.1177/1087054716636936. [DOI] [PubMed] [Google Scholar]
- 23.Ma J.K., Le Mare L., Gurd B.J. Four minutes of in-class high-intensity interval activity improves selective attention in 9- to 11-year olds. Appl Physiol Nutr Metab. 2015;40(3):238–244. doi: 10.1139/apnm-2014-0309. [DOI] [PubMed] [Google Scholar]
- 24.Ma J.K., Le Mare L., Gurd B.J. Classroom-based high-intensity interval activity improves off-task behaviour in primary school students. Appl Physiol Nutr Metab. 2014;39(12):1332–1337. doi: 10.1139/apnm-2014-0125. [DOI] [PubMed] [Google Scholar]
- 25.Cornelius C., Fedewa A.L., Ahn S. The effect of physical activity on children with ADHD: a quantitative review of the literature. J Appl Sch Psychol. 2017;33(2):136–170. [Google Scholar]
- 26.Sun F., Chow G.C., Yu C.C., et al. Effect of game-based high-intensity interval training program on the executive function of children with ADHD: protocol of a randomized controlled trial. PLoS One. 2022;17(7) doi: 10.1371/journal.pone.0272121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrison C.B., Kilding A.E., Gill N.D., Kinugasa T. Small-sided games for young athletes: is game specificity influential? J Sports Sci. 2014;32(4):336–344. doi: 10.1080/02640414.2013.824600. [DOI] [PubMed] [Google Scholar]
- 28.Vaz L., Leite N., Joao P.V., Goncalves B., Sampaio J. Differences between experienced and novice Rugby Union players during small-sided games. Percept Mot Skills. 2012;115(2):594–604. doi: 10.2466/30.10.25.PMS.115.5.594-604. [DOI] [PubMed] [Google Scholar]
- 29.Lambrick D., Westrupp N., Kaufmann S., Stoner L., Faulkner J. The effectiveness of a high-intensity games intervention on improving indices of health in young children. J Sports Sci. 2016;34(3):190–198. doi: 10.1080/02640414.2015.1048521. [DOI] [PubMed] [Google Scholar]
- 30.Yu C.C.W., Wong S.W.L., Lo F.S.F., So R.C.H., Chan D.F.Y. Study protocol: a randomized controlled trial study on the effect of a game-based exercise training program on promoting physical fitness and mental health in children with autism spectrum disorder. BMC Psychiatr. 2018;18(1):56. doi: 10.1186/s12888-018-1635-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cooper S.B., Bandelow S., Nute M.L., Morris J.G., Nevill M.E. The effects of a mid-morning bout of exercise on adolescents' cognitive function. Ment Health Phys Act. 2012;5(2):183–190. [Google Scholar]
- 32.Hendrickson N.K., McCrimmon A.W. Test review: behavior rating inventory of executive function®, second edition (BRIEF®2) Can J Sch Psychol. 2018;34(1):73–78. by Gioia, G. A., Isquith, P. K., Guy, S. C., & Kenworthy, L. [Google Scholar]
- 33.Shum K.K., Zheng Q., Chak G.S., et al. Dimensional structure of the BRIEF2 and its relations with ADHD symptoms and task performance on executive functions in Chinese children. Child Neuropsychol. 2021;27(2):165–189. doi: 10.1080/09297049.2020.1817355. [DOI] [PubMed] [Google Scholar]
- 34.Maki A., Yamashita Y., Ito Y. Spatial and temporal analysis of human motor activity using noninvasive NIR topography. Med Phys. 1995;22(12):1997–2005. doi: 10.1118/1.597496. [DOI] [PubMed] [Google Scholar]
- 35.National Center for Health Statistics . 2020. Anthropometry Procedures Manual of National Health and Nutrition Examination Survey.https://wwwn.cdc.gov/nchs/data/nhanes/2019-2020/manuals/2020-Anthropometry-Procedures-Manual-508.pdf [Google Scholar]
- 36.Purpura D.J., Lonigan C.J. Conners' Teacher Rating Scale for preschool children: a revised, brief, age-specific measure. J Clin Child Adolesc Psychol. 2009;38(2):263–272. doi: 10.1080/15374410802698446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moore J.B., Hanes J.C.J., Barbeau P., Gutin B., Treviño R.P., Yin Z. Validation of the Physical Activity Questionnaire for older children in children of different races. Pediatr Exerc Sci. 2007;19(1):6–19. doi: 10.1123/pes.19.1.6. [DOI] [PubMed] [Google Scholar]
- 38.Ruiz J.R., Castro-Pinero J., Espana-Romero V., et al. Field-based fitness assessment in young people: the ALPHA health-related fitness test battery for children and adolescents. Br J Sports Med. 2011;45(6):518–524. doi: 10.1136/bjsm.2010.075341. [DOI] [PubMed] [Google Scholar]
- 39.Ye J.C., Tak S., Jang K.E., Jung J., Jang J. NIRS-SPM: statistical parametric mapping for near-infrared spectroscopy. Neuroimage. 2009;44(2):428–447. doi: 10.1016/j.neuroimage.2008.08.036. [DOI] [PubMed] [Google Scholar]
- 40.Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289–300. [Google Scholar]
- 41.Yekutieli D., Benjamini Y. Resampling-based false discovery rate controlling multiple test procedures for correlated test statistics. J Stat Plan Inference. 1999;82:171–196. [Google Scholar]
- 42.Chang Y.-K., Liu S., Yu H.-H., Lee Y.-H. Effect of acute exercise on executive function in children with Attention Deficit Hyperactivity Disorder. Arch Clin Neuropsychol. 2012;27(2):225–237. doi: 10.1093/arclin/acr094. [DOI] [PubMed] [Google Scholar]
- 43.Pontifex M.B., Saliba B.J., Raine L.B., Picchietti D.L., Hillman C.H. Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. J Pediatr. 2013;162(3):543–551. doi: 10.1016/j.jpeds.2012.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aranas K., Leighton J.P. Dimensions of physical activity as related to child attention-deficit/hyperactivity disorder symptoms and impairment. Clin Child Psychol Psychiatry. 2022;27(4):953–966. doi: 10.1177/13591045211058338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu Y., Sun F., Chiu M.M., Siu A.Y. Effects of high-intensity interval exercise and moderate-intensity continuous exercise on executive function of healthy young males. Physiol Behav. 2021;239 doi: 10.1016/j.physbeh.2021.113505. [DOI] [PubMed] [Google Scholar]
- 46.Poliakova E., Conrad A.L., Schieltz K.M., O'Brien M.J. Using fNIRS to evaluate ADHD medication effects on neuronal activity: a systematic literature review. Front Neuroimaging. 2023;2 doi: 10.3389/fnimg.2023.1083036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gu Y., Miao S., Han J., et al. Complexity analysis of fNIRS signals in ADHD children during working memory task. Sci Rep. 2017;7(1):829. doi: 10.1038/s41598-017-00965-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang C.M., Shin J., Kim J.I., Lim Y.B., Park S.H., Kim B.N. Classifying children with ADHD based on prefrontal functional near-infrared spectroscopy using machine learning. Clin Psychopharmacol Neurosci. 2023;21(4):693–700. doi: 10.9758/cpn.22.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dos Santos Afonso Junior A., Machado-Pinheiro W., Osorio A.A.C., et al. Association between ADHD symptoms and inhibition-related brain activity using functional near-infrared spectroscopy (fNIRS) Neurosci Lett. 2023;792 doi: 10.1016/j.neulet.2022.136962. [DOI] [PubMed] [Google Scholar]
- 50.Cortese S. The association between ADHD and obesity: intriguing, progressively more investigated, but still puzzling. Brain Sci. 2019;9(10):256. doi: 10.3390/brainsci9100256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fliers E.A., Buitelaar J.K., Maras A., et al. ADHD is a risk factor for overweight and obesity in children. J Dev Behav Pediatr. 2013;34(8):566–574. doi: 10.1097/DBP.0b013e3182a50a67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cortese S., Angriman M., Maffeis C., et al. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Crit Rev Food Sci Nutr. 2008;48(6):524–537. doi: 10.1080/10408390701540124. [DOI] [PubMed] [Google Scholar]
- 53.Mercurio L.Y., Amanullah S., Gill N., Gjelsvik A. Children with ADHD engage in less physical activity. J Atten Disord. 2021;25(8):1187–1195. doi: 10.1177/1087054719887789. [DOI] [PubMed] [Google Scholar]
- 54.Sharma V.K., Subramanian S.K., Radhakrishnan K., Rajendran R., Ravindran B.S., Arunachalam V. Comparison of structured and unstructured physical activity training on predicted VO2max and heart rate variability in adolescents - a randomized control trial. J Basic Clin Physiol Pharmacol. 2017;28(3):225–238. doi: 10.1515/jbcpp-2016-0117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author (Dr. Fenghua SUN), upon reasonable request.