Abstract
Purpose
Despite the agreed-on efficacy and benefits of palliative radiation therapy (PRT) to alleviate end-of-life complications related to cancer progression, PRT remains an underused treatment in the hospice-care setting.3-4,6-7 Common barriers for hospice patient use of PRT include educational and economic limitations. This paper discussed these barriers and ways to eliminate them based on previously published interventions.
Methods and Materials
Literature search on PubMed; 30 articles were selected by the authors. All articles included are published after the year 2000 in peer reviewed journals.
Results
Educational barriers for medical practitioners outside radiation oncology can be addressed by creating formal education programs that reduce knowledge gaps previously identified by survey-based research studies. For radiation oncologists, continued education should focus on increasing competence and comfort with end-of-life conversations and indications for use of single-fraction radiation for patients with advanced cancer. More information on radiation oncology options should be provided to patients. As for economic barriers, rapid-access programs that use advanced level practitioners can increase PRT access by the hospice population. Also, these programs can increase use of single-fraction radiation therapy (SFX RT) in patients with a shorter projected prognosis. SFX RT is beneficial in this setting because it decreases hospice expense and is as efficacious at palliating pain in patients with advanced cancer as multiple-fraction radiation.
Conclusions
The barriers of education and economic limitations can be addressed by: expanding the PRT curriculum for all practicing physicians, improving radiation oncologist palliative care knowledge, increasing PRT resources for patients, increasing number of rapid-access radiation therapy programs, and, when indicated, encouraging use of single-fraction radiation treatment for hospice patients.
Introduction
Most hospice patients are diagnosed with a terminal cancer. Many suffer in silence struggling to eat, communicate, and breath at the end of their life. Severe pain arising from complications of metastatic cancer significantly rules these individuals’ final days; the pain of the patient extends beyond the patient, affecting both their support system and health care team.1 Palliative radiation therapy (PRT) is a well-studied, beneficial, and efficacious treatment that has been proven to control symptoms associated with terminal cancer.1, 2, 3 These symptoms include but are not limited to: bone metastasis, brain metastasis, spinal cord compression, airway obstruction, dysphagia, hemoptysis, hematuria, and bleeding associated with ulcerated tumors.2, 3, 4, 5, 6 Additionally, with treatment, there can be a significant reduction in the dosage of narcotics used to palliate the pain and improving a patient's ability to communicate coherently with their loved ones at the end of their lives.5 This modality of symptom management remains heavily underused in the hospice population.4, 5, 6, 7 Despite a positive perception of usefulness of PRT among physicians in hospice, palliative care, and general oncology, it is predicted that <3% of hospice patients7 receive PRT. With cancer continuing to be the second leading cause of death in the United States (US), combined with the fact that by 2030 20% of the total US population will be aged >65 years,8 there is a need to reassess the way advanced cancer symptoms are managed.
The goal of this narrative review was to identify barriers that can be addressed to improve access of PRT in the hospice population. Of course, it is not feasible to address all the barrier of PRT, such as improving access to palliative radiation facilities or addressing unique patient challenges. However, there are 2 barriers that are within our scope of influence: educational and economic barriers. In addition to the barriers, there have been previously published interventions to address these barriers. These interventions, along with other proposals to address the barriers, will be further examined in this narrative review.
Methods and Materials
This narrative review was conducted using the PubMed database. The research question: what barriers are contributing to the underutilization of PRT in the hospice population shaped our search terms to include: “Hospice and Palliative Radiotherapy,” “Barriers of palliative radiotherapy in hospice,” “Single vs. multi-fraction radiotherapy.” The literature search yielded a total of 276 articles.
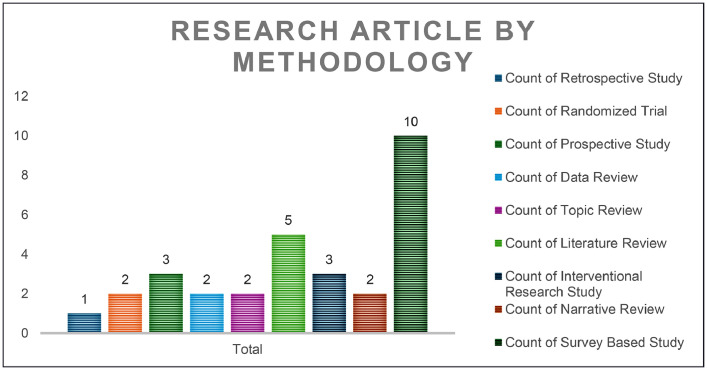
Eligibility assessment: Inclusion criteria included journal articles published between the years 2000 and 2020. Articles selected were published in peer reviewed journals. The types of articles selected were published as clinical trials, meta-analyses, randomized controlled trials, reviews, or systemic reviews. Exclusion criteria excluded studies published as abstracts, qualitative research studies, and articles that did not discuss both palliative/hospice care and PRT within the same article. A total of 25 articles were selected using the search terms and inclusion and exclusion criteria outlined above. The final 5 articles were chosen by reviewing the reference list of the 25 articles selected, if the article pertained to hospice and PRT. The final 30 articles chosen were individually reviewed by the authors. See Fig. 1 for the research methodologies included.
Figure 1.
Research article by methodology.
Educational limitations
Education for practicing physicians
A wide range of medical knowledge equips physicians with valuable skills for treating their patients effectively; from diagnosing a patient to creating a patient-centered treatment plan. A Canadian survey of family physicians assessed referral pattern to PRT. The results established a direct relationship between level of knowledge and referral pattern.9 Physicians who had been in practice for >3 years, had previous success contacting a radiation oncologist (RO), previous formal education on the subject, more patients with cancer in their practice or had previously provided palliative care were more likely to refer patients to a RO for PRT.9 The direct relationship between level of knowledge and referral pattern highlights the importance of implementing formal educational opportunities on the subject of PRT.
Additionally, formal education necessitates guidelines that help direct physicians in their clinical decisions. The underdeveloped formal guidelines for indications for referral and timeline for patient referral to PRT remains a common barrier among physicians outside the field of radiation oncology.9,10 More specifically, in a critical review on PRT at the End of Life, Jones et al,3 emphasizes the need for furthering research on prognostic models for survival, because as of now these models are highly variable. The variability in the estimate of a patient's survival can impact a physician's decision to referrer to PRT or even hospice. Although a perfect prognostic model for survival is not feasible, a more accurate model can help formulate guidelines when it comes to referring patients for PRT.5
Hospice and palliative care physicians
The opinions and attitudes of hospice professionals on use of radiation therapy is overwhelmingly positive regarding symptom control for patients with terminal cancer.7,8,11,12 However, educational barriers from minimal formal education of PRT leads to misperceptions and decreased referrals. Per a cross sectional survey of 81 of 120 hospice and palliative medicine fellowship program directors, 25% of the programs provide an optional radiation oncology rotation, 30% of the programs lack a PRT curriculum, and 14% of the programs provide <2 hours of PRT education.12 Additionally, a survey of members of the American Academy of Hospice and Palliative Medicine by McCloskey et al8 identified toxicity of radiation, delayed onset of symptom relief, lack of practice guidelines, duration of radiation treatments, concern of RO discomfort/anxiety with palliative care, and lack of multidisciplinary settings for coordination of care as educational limitations that impacted their use of PRT in a hospice setting. Livergant et al's13 literature review among hospice health professionals 62% of respondents were concerned about the occurrence of complications of PRT and insufficient knowledge on indications for referring patients for PRT.
The limited educational standards for hospice and palliative medicine fellowship programs to incorporate palliative radiation therapy into their curriculum perpetuates their lack of knowledge of PRT.12 At the University of California, a 4-hour PRT course, which included a tour of the radiation suite and introductory lecture on the topic, was developed for 5 hospice and palliative medicine fellows.14 After the completion of the course, the fellows’ perception, and knowledge of radiation oncology statistically increased; many of them said they would be more likely to refer their patients for treatment.14
The next step is to expand on the University of California PRT course14 addressing toxicity of radiation, timeline of symptom relief, and duration of radiation treatment. Exposing more hospice physicians to PRT has the potential to increase referrals of hospice patients for PRT.
Other referring physicians
Understanding pain-reduction oncology services such as radiation therapy is important for physicians in all areas of medicine; in 1 study, up to 97% of family physicians encountered 1 or more patients with a cancer diagnosis within the past month.4,9,15 Family medicine physicians’ and surgeons’ lack of knowledge contributed to 46.5% of inappropriately delayed PRT.15 Similar to hospice and palliative care physicians, the educational barriers for other referring physicians can be attributed because of a lack of formal education. Family physician perception of barriers to referral to PRT include: concern of patient age (27%-48%), functional status (53%-78%), patient life expectancy (44%-59%), cancer type or histology (55%-80%), uncertain of benefits (30%-54%), length of treatment course (31%-47%), patient's symptoms (50%), side effects or toxicity (32%-39%), and perception of inconvenience (24%-65%).13 In a Canadian family physician survey assessing family physicians’ knowledge of PRT, the physicians underestimated their knowledge of PRT; these physicians knew more about PRT than they thought.9 The physicians’ lack of confidence in their knowledge of PRT consequently impacted their referral rate. The findings from the survey found that the family physicians were able to correctly identify the minimum life expectancy for referral to PRT (<1 month) and various indications for referral including brain and bone metastasis (73%), airway obstruction (70%), dysphagia (68%), superior vena cava obstruction (54%), squamous cell carcinoma (54%), and bleeding associated with ulcerated tumors (47%).16 They incorrectly identified febrile neutropenia (41%), lymphedema (29%), and hypercalcemia (24%) as scenarios indicating need for PRT.16
The lack of knowledge of PRT in general practices should be addressed by implementing formal educational programs. The educational program can be similar to the one created by the University of California for palliative and hospice fellows,14 because there has been no prior educational program created for general practitioners. The curriculum can be expanded to address topics such as indications for referral, toxicity of radiation, timeline of symptom relief and duration of radiation treatment. As well as generally boosting these physicians’ confidence in using PRT resources. Because confidence level of a physician directly influences referral patterns, addressing this variable with an adequate understanding of PRT is an unmet research need. Developing methods that quantify a physician's knowledge of the subject through a test could provide positive feedback for the physician, further encouraging the use of PRT in the future.
RO physicians
Educational barriers for ROs are slightly different from the limitations outlined above. ROs would benefit from educational opportunities that expand their knowledge of caring for hospice patients at the end of their life. Fine-tuning communication skills and expanding treatment regimens of single-fraction radiation (SFR) and hypofractionated treatment will help address these educational limitations. Also, participating in palliative care rounds for shared patients between the 2 specialties can increase collaboration and continuity of care.
Currently, there are no standards for incorporating basic palliative care knowledge into radiation oncology residency programs, resulting in undue emotional burden.7,8,17,18 A survey of members of the National Hospice and Palliative Care Organization found that more than half the respondents felt that the ROs were not sufficiently trained in palliative care.7 The McCloskey et al8 survey of the American Society of Therapeutic Radiation Oncology, American Society of Clinical Oncology, and American Academy of Hospice and Palliative Medicine members found that many physicians feel uncomfortable and anxious when managing pain and providing symptom management. Many attributed this to a lack of education regarding palliative medicine.8,17,19 Training on how to engage patients in end-of-life conversations is of utmost importance.19 Parker et al,17 found that among 162 ROs, there were 120 consultations where PRT was recommended 86% of the time with 46% of these consultations involving a high-palliative care burden. Four domains of palliative care were identified as highly relevant to care: physical symptoms (91%), care coordination (70%), goals of care (59%), and psychosocial issues (52%).17 Providing palliative care knowledge to ROs could increase the services offered by ROs, because the physicians will be more willing to treat this population of patients. Also, it could help to alleviate the emotional burden that comes with caring for this vulnerable patient population.17,18 There are a few communication tools used by general oncologists and hospice physicians that can easily be incorporated into practice, such as the SPIKES 6-step protocol for breaking bad news and/or NURSE protocol for responding to patients’ emotions. These skills are easily accessible to all physicians online.
In addition to using the SPIKES or NURSE protocol, hospice and palliative care physicians can create a training course emphasizing communication skills emphasizing the 4 domains of palliative care identified as highly relevant by ROs (physical symptoms, care coordination, goals of care, and psychosocial issues). To our knowledge, there is no previous formal education program created by hospice and palliative care physicians for ROs. A weekend long seminar course combining RO and palliative/hospice physicians might be mutually beneficial, enabling both specialties to learn from each other and increase collaboration.
ROs could also provide refresher courses on utilization of SFR regimens and hypofractionated therapy during annual national conferences. Jones et al,3 provides a comprehensive list of suggestion for therapeutic use of PRT for various clinical scenarios at the end of life (bone metastases, malignant epidural spinal cord compression, brain metastases, and locally advanced non-small cell lung cancer). Further research in this area of radiation oncology could establish treatment guidelines for the hospice population. These protocols will help increase accessibility for radiation oncology physicians by allowing them to make evidence-based treatment decisions when treating this vulnerable population.
Medical students
Medical students would also benefit from formal PRT education. There has been only 1 literature review regarding the training of medical students in radiation oncology, and there is no data on the exact number of medical schools that offer curriculum on PRT. Although knowledge on radiation oncology improves from first year to fourth year (especially if the medical student has the opportunity to rotate with a RO), knowledge remains limited among medical students with persistent gaps in their understanding.20 At the Technical University of Munich, a 5-series seminar, each class 45 minutes each, exposed medical students to the technical aspect of radiation oncology.21 The topics included radiation biology, radiation therapy process and linear accelerator, and treatment planning, as well as a demonstration of the linear acceleration.21 The seminar was well received, but the participants were not followed limiting the conclusions on the impact of such a seminar on clinical practice.21
The 5-series seminar21 could be condensed into a 1- or 2-part lecture series and focus on the basics of radiation oncology and different uses for the modality. The series can address not only curative radiation therapy but also PRT. As outlined above, based on knowledge gaps among practicing physicians, the course can address the topics of indications for referral, toxicity of radiation, symptom-relief timeline, and duration of radiation treatment. The seminar should provide basic radiation oncology information for the eventual general practitioner. Also, data should be collected on how these courses influence referral pattern when the student is practicing medicine.
Education for patients
Patients' knowledge and understanding of their prognosis is key to helping them formulate goals of care. Because prognosis is limited by the physician's ability to adequately predict life expectancy, a patient's decision can be heavily skewed by this prediction. Providers should help guide their patients when discussing their prognosis, palliation of symptoms, and options for treatment. The treatment(s) chosen should align with the patient's values and help them achieve their objectives during the limited time they have remaining.3 Having difficult end-of-life conversations with their provider over several follow-up appointments would allow the most benefit for the patient.22
Patient hesitancy remains 1 of the main barriers for utilization of PRT on the consumer level.11 Family physicians found patient wishes (72%) as a barrier for referral to PRT.9 Among hospice professionals, patient reluctance (84%) and family reluctance (51%) were identified as barriers to referral to PRT.11 A contributing factor to patient and family reluctance could include lack of knowledge of PRT and/or negative perception of radiation in general. Online resources are easily accessible and commonly used by patients to help guide their decision.23 Up to 77% of Americans search for online health information using search engines, such as Google.23 A research study included 100 online palliative care and oncology educational articles, accessed via Google, and the articles were scored using 9 readability assessments.23 The results found that these articles were at a mean 12.1 grade reading level.23 Zero articles were written below the recommended seventh grade reading level.23 One way to address patient hesitancy is creating online patient educational resources that meet the national health literacy recommendation. This can help patients and their caregivers better understand their options for treatment as well as address general misconceptions surrounding radiation.
Ways to address this barrier include having radiation oncologists create accessible reading materials, using shared decision-making tools, and referrals to palliative/hospice care. One example provided in, “Empowering patients in decision-making in radiation oncology, we can do better,” included a consultation appointment where the patient with prostate cancer meets with a RO and a surgeon before deciding the course of treatment.22 Also, they referred any patient with a prognosis <6 months to palliative care; this helped the patients further establish the goal of treatment best suited for them.22 Ultimately, the patient is at the center of the health care model and therefore should be given the opportunity to be a part of their healing process.
Economic limitations
Waiting time: decreased with dedicated radiation therapy programs
Rapid-access radiation therapy programs are essential to help streamline the process for PRT. A literature review on rapid-access radiation therapy programs summarizes these programs as helpful in expediting the referral process.24 A defining feature of many of these programs is a team, also referred to as an advanced practice radiation therapist model, comprised of an advance practice physician, an attending physician, and a resident physician.25 By having a dedicated advanced practitioner consult with inpatients in need of PRT significantly reduces the waiting time.25 PRT wait times are often because of external factors that cannot be controlled such as department waiting lists or waiting for restaging, medical test or laboratory test results, and chemotherapy schedules. However, having an advanced practice radiation therapist significantly reduces the wait time when a patient is referred for PRT,25 and many of the patients will receive a same-day consultation and treatment. Although the external factors are hard to control, implementing a more streamlined system could alleviate the wait time unrelated to external factors. The problem of increased wait time seems to be most applicable for patients in the outpatient setting.24,26 Patients in hospitals are more likely to have a same-day consultation for symptoms, especially if it is urgent. However, this is limited by the location of the practice and if there is a radiation therapy department on site.24,26
Single versus multiple-fraction radiation therapy
Despite the reluctance of providing SFR therapy, single-fraction therapy should be considered as standard palliative treatment for patients with painful bone metastases because of the decreased cost and more convenient schedule for patients.3,27, 28, 29 Per Livergant et al13 the most common dosage of radiation used for patients in the last 30 days of life was 30 Gy in 10 fractions. Although use of SFR radiation therapy (SFX RT) courses ranged from 0% to 59%, in the US the reported rate was 8% to 9.4% compared to Canada's 19% to 59%. A major impact of implementing a rapid-access radiation therapy program was an increase in utilization of short-course radiation therapy. For example, at the Palliative Radiation Oncology Consult (PROC) service at Mount Sinai Hospital in New York, the absolute rate of SFX RT courses increased by 14.3% post-PROC.29 Similarly, within the first 10 months of starting the Inpatient Palliative Radiation Oncology Service at Vanderbilt, the utilization of SFX RT increased from 30% to 70%.24 It is also notable that with the implementation of these programs the median hospital length of stay decreased; the PROC service found median hospital length of stay decreased from 26.5 days to 21 days29; and the Inpatient Palliative Radiation Oncology Service found a medial hospital length of stay decrease from 21 days to 9 days.24 Schuster et al27 reported an 18-month program streamlined model that allowed 4 hospice patients to be successfully treated with SFX RT; the conclusion noted that, absent the program, the hospice providers would not have referred hospice patients for PRT.27 These programs’ models seem to be correlated with an increased utilization of SFX RT compared with those that do not have a dedicated rapid-access radiation therapy program. Future research in this area should further explore the rate of utilization of SFX RT courses versus multiple-fraction radiation therapy courses in the hospice-care population, in both in- and outpatient settings, without a dedicated rapid-access radiation therapy program.
The estimated quality adjusted life years and societal costs are both favored by the single-fraction treatment schedule.28 Per Van den Hout et. al,28 the estimated cost of radiation therapy including retreatments and nonmedical costs for a single-fraction schedule was $873 lower than for a multiple-fraction schedule. Additionally, Konski et. al4 compares the cost and quality adjusted life months between pain medication, SFR, multiple-fraction radiation treatment, and chemotherapy for bone metastasis in patients with prostate cancer. The SFR therapy mean cost was the most cost-effective palliative treatment, with a cost-effective ratio of $6857/quality adjusted life year and quality adjusted life months of 6.1 compared with multiple-fraction therapy, chemotherapy, and pain medication with quality adjusted life months reported at 6.25, 4.93, and 5.75 respectively.4 Chemotherapy had the highest mean total cost and lowest effectiveness.4
Reimbursement models for providing end-of-life care
For patients in hospice that could benefit from PRT, reimbursement for treatment is a significant barrier.7,27,30 Often patients must either postpone their enrollment in hospice so that they can receive palliative radiation treatment or unenroll in hospice care to obtain PRT.27 This is because of the limiting hospice reimbursement plan from Medicare which has a median per diem reimbursement rate of $114 to $150 per day, per patient.7,27 Per Lutz et. al7 the mean cost for a single fraction of radiation is $630; therefore, a common 10-fraction course could range from $1508 to $2221. According to a Jarosek et al30 data review on use of PRT in hospice, of the 953 hospices (89% of all freestanding hospice programs in the year 2002), one fifth of the programs (227 total hospice programs: 162 not-for-profit and 65 for-profit) reported radiation cost; multiple logistic regression results found that large size, not-for profit status, and percent of stays <7 days were significantly associated with providing radiation services.30 The for-profit hospice programs are half as likely to provide PRT compared with not-for-profit hospice programs because of the Medicare reimbursement model.30 In the hospice-care setting, because the length of stay for the patients in hospice can be short, therefore there is less money available to provide the option for PRT in for-profit hospice settings.27 Qualitative research has suggested that hospices will not accept patients who require high-cost services such as palliative radiation.27 A Clinic offering Affordable Radiation Therapy conducted an 18-month program that increased access to PRT for hospice patients. Eight patients were referred, and 4 patients were successfully treated with a single-fraction dose of 8 Gy.27 The model included 1 4-hour visit after they were referred.27 The referral process was a single-page form faxed to the RO.27 The hospice facilities were all within 50 miles of a radiation oncology facility.27 This program helped to streamline the process by empowering hospice nurses and directors to facilitate the referral process.27 It is suggested that the hospice reimbursement schedule should be amended, and additional financial benefits should be offered to agencies that use PRT.27 In addition to dedicated palliative care programs that offer rapid access to SFR and concurrent care plans could help alleviate the financial barriers.30 A concurrent care plan would allow a patient to remain enrolled in hospice in addition to receiving any necessary medical treatments for their disease, such as PRT.
Discussion
With the potential to benefit 397,000 patients per year, overcoming these complex obstacles is critical and will require a concerted effort within the medical community.27
Improving opportunity for education
Further implementing education programs and creating curriculum for medical professionals around guidelines for referring patients for PRT would be greatly beneficial. Discussing difficult end-of-life conversations and other basic palliative care planning will help ROs feel more confident in their abilities to work with this vulnerable population of patients. In terms of benefiting the patient, access to resources that are at or below the seventh grade reading level could help patients better understand the various oncology services available. See Table 1 for summary.
Table 1.
Educational limitations of palliative radiation therapy
| Medical professionals | Suggested intervention(s) | Goal of intervention |
|---|---|---|
| Radiation oncologists | Course on utilization of single-fraction radiation and hypofractionated therapy | Increase radiation oncologists’ confidence providing single-fraction radiation therapy |
| Course that focuses on communication skills relating to the 4 domains of palliative care (physical symptoms, care coordination, goals of care, and psychosocial issues) | Improve radiation oncologists’ confidence communicating with hospice patients and their caregivers | |
| Creating educational resources on palliative radiation therapy that meet the national health literacy recommendation | Improve communication between radiation oncologist and patient | |
| Hospice and palliative care physicians | Formal didactic course that addresses the indications for, toxicity of, timeline of symptom relief, and duration of treatment of palliative radiation therapy | Increase referrals of hospice patients for radiation oncology |
| General physician | Formal didactic course that addresses the indications for, toxicity of, timeline of symptom relief, and duration of treatment of palliative radiation therapy | Increase referrals of hospice patients for radiation oncology |
| Medical students | Formal didactic course that addresses the indications for, toxicity of, timeline of symptom relief, and duration of treatment of palliative radiation therapy | Increase knowledge of future physicians in the efforts to increase awareness of palliative radiation therapy |
How to make PRT affordable
Navigating the economics part of the barrier is difficult. However, the continued implementation and overall general body of knowledge of these benefits could help overcome the economic barriers. Rapid-access programs that streamline the referral process for inpatients and outpatients could help decrease the administrative costs and wait times. Also, finding ways to decrease the cost and burden of PRT for the patients could also contribute to making this treatment for affordable. For example, accepting single-dose radiation fraction as a cost-effective palliative care treatment, especially for hospice patients, and awareness of concurrent medical care for hospice patients. Finally, on the systemic level, advocating for a more robust hospice reimbursement schedule and reimbursing physicians for their time for providing this vulnerable population with basic palliative care could further incentivize PRT. See Table 2 for summary.
Table 2.
Economic limitations of palliative radiation therapy
| Intervention | Outcome |
|---|---|
| Dedicated rapid-access radiation therapy program that use advance practice practitioners | Decrease the time between referral for palliative radiation therapy consultation and treatment by streamlining referral process |
| Including single-fraction radiation therapy as a standard palliative treatment for patients with bone metastasis | Increase acceptance of single-fraction radiation therapy and decrease financial cost of therapy |
| Supporting use of concurrent care plans | Allows patients to receive palliative radiation therapy while also in hospice to combat the restricting per diem reimbursement model used by hospice |
Conclusions
With the aging population, and the advances in health care that have allowed people to live longer with terminal cancers, the utilization of PRT should continue to increase. Also, as the prognostic models improve in accuracy, the referral guidelines for PRT should become more accessible for physicians across all areas of medicine. Improving PRT referral patterns within the hospice population will take a concerted effort from all areas of medicine. Education on the principles of radiation therapy needs to be championed by ROs to increase knowledge among family physicians, Hospice and palliaive medicine physicians, residents, and medical students. Also, ROs need to create resources for patients and their families that meet the recommended literacy level. Finally, in terms of educational barriers, it is imperative that ROs be equipped with the knowledge and tools to address palliative care concerns pertaining to end of life. It is the mission of hospice care to provide “any services documented as reasonable and necessary for the palliation and management of patient's terminal illness,”27 which includes PRT. Therefore, the reimbursement schedule expenses should be expanded to include single-dose or hypofractionated doses of RT when indicated. It is unfortunate that the current reimbursement model prevents hospice patients from obtaining an appropriate level of end-of-life care. Future research should focus on the impact of implementing these educational and economic interventions to increase PRT referral and use of SFX RT versus multiple-fraction radiation therapy in the hospice-care setting.
Disclosures
Sana D. Karam receives funding from the NIDCR/NCI (R01 DE028528-01; R01 DE028282-01; R01 CA284561-01; 1 P50 CA261605-01) and clinical trial funding from AstraZeneca, Genentech, and Ionis, all of which are unrelated to this work. Sana D. Karam reports grant funding from Roche and Amgen unrelated to this project. The other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.McDonald R, Chow E, Rowbottom L, et al. Quality of life after palliative radiotherapy in bone metastases: A literature review. J Bone Oncol. 2015;4:24–31. doi: 10.1016/j.jbo.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spencer K, Velikova G, Henry A, Westhoff P, Pter Hall, van der Linden YM. Net pain relief after palliative radiation therapy for painful bone metastases: A useful measure to reflect response duration? A further analysis of the Dutch Bone Metastasis study. Int J Radiat Oncol Biol Phys. 2019;105:559–566. doi: 10.1016/j.ijrobp.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones JA, Lutz ST, Chow E, Johnstone PA. Palliative radiotherapy at the end of life: A critical review. CA Cancer J Clin. 2014;64:295–310. doi: 10.3322/caac.21242. [DOI] [PubMed] [Google Scholar]
- 4.Konski A. Radiotherapy is a cost-effective palliative treatment for patients with bone metastasis from prostate cancer. Int J Radiat Oncol Biol Phys. 2004;60:1373–1378. doi: 10.1016/j.ijrobp.2004.05.053. [DOI] [PubMed] [Google Scholar]
- 5.Wu JSY, Kerba M, Wong RKS, Mckimmon E, Eigl B, Hagen NA. Patterns of practice in palliative radiotherapy for painful bone metastases: impact of a regional rapid access clinic on access to care. Int J Radiat Oncol Biol Phys. 2010;78:533–538. doi: 10.1016/j.ijrobp.2009.07.1716. [DOI] [PubMed] [Google Scholar]
- 6.Park KR, Lee CG, Tseng YD, et al. Palliative radiation therapy in the last 30 days of life: A systematic review. Radiother Oncol. 2017;125:193–199. doi: 10.1016/j.radonc.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Lutz S, Spence C, Chow E, Janjan N, Connor S. Survey on use of palliative radiotherapy in hospice care. J Clin Oncol. 2004;22:3581–3586. doi: 10.1200/JCO.2004.11.151. [DOI] [PubMed] [Google Scholar]
- 8.McCloskey SA, Tao ML, Rose CM, Fink A, Amadeo AM. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J. 2007;13:130–137. doi: 10.1097/PPO.0b013e31804675d4. [DOI] [PubMed] [Google Scholar]
- 9.Samant RS, Fitzgibbon E, Meng J, Graham ID. Barriers to palliative radiotherapy referral: A Canadian perspective. Acta Oncol. 2007;46:659–663. doi: 10.1080/02841860600979005. [DOI] [PubMed] [Google Scholar]
- 10.Grewal AS, Jones J, Lin A. Palliative radiation therapy for head and neck cancers. Int J Radiat Oncol Biol Phys. 2019;105:254–266. doi: 10.1016/j.ijrobp.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 11.Vargas A, Torres C, Küller-Bosch A, Villena B. Palliative care physicians and palliative radiotherapy, knowledge and barriers for referring: A cross-sectional study. J Pain Symptom Manage. 2020;60:1193–1199.e3. doi: 10.1016/j.jpainsymman.2020.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Martin EJ, Jones JA. Palliative radiotherapy education in hospice and palliative medicine fellowship: A national needs assessment. J Clin Oncol. 2018;36 87-87. [Google Scholar]
- 13.Livergant J, Howard M, Klein J. Barriers to referral for palliative radiotherapy by physicians: A systematic review. Clin Oncol (R Coll Radiol) 2019;31:e75–e84. doi: 10.1016/j.clon.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Martin EJ, Nalawade VV, Murphy JD, Jones JA. Incorporating palliative radiotherapy education into hospice and palliative medicine fellowship training: a feasibility study. Ann Palliat Med. 2019;8:436–441. doi: 10.21037/apm.2019.04.02. [DOI] [PubMed] [Google Scholar]
- 15.Parker SM, Wei RL, Jones JA, Mattes MD. A targeted needs assessment to improve referral patterns for palliative radiation therapy. Ann Palliat Med. 2019;8:516–522. doi: 10.21037/apm.2019.08.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fairchild A, Ghosh S, Baker J. Patterns of referral and knowledge of palliative radiotherapy in Alberta. Can Fam Physician. 2012;58:e113–e122. [PMC free article] [PubMed] [Google Scholar]
- 17.Parker GM, LeBaron VT, Krishnan M, et al. Burden of palliative care issues encountered by radiation oncologists caring for patients with advanced cancer. Pract Radiat Oncol. 2017;7:e517–e524. doi: 10.1016/j.prro.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Ioannides PJ, Wei RL. Radiation oncology resident education in palliative care. Ann Palliat Med. 2019;8:305–311. doi: 10.21037/apm.2019.01.07. [DOI] [PubMed] [Google Scholar]
- 19.Wei RL, Mattes MD, Yu J, et al. Attitudes of radiation oncologists toward palliative and supportive care in the United States: Report on national membership survey by the American Society for Radiation Oncology (ASTRO) Pract Radiat Oncol. 2017;7:113–119. doi: 10.1016/j.prro.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zaorsky NG, Shaikh T, Handorf E, et al. What are medical students in the United States learning about radiation oncology? Results of a multi-institutional survey. Int J Radiat Oncol Biol Phys. 2016;94:235–242. doi: 10.1016/j.ijrobp.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dapper H, Wijnen-Meijer M, Rathfelder S, et al. Radiation oncology as part of medical education-current status and possible digital future prospects. Strahlenther Onkol. 2021;197:528–536. doi: 10.1007/s00066-020-01712-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leech M, Katz MS, Kazmierska J, McCrossin J, Turner S. Empowering patients in decision-making in radiation oncology - can we do better? Mol Oncol. 2020;14:1442–1460. doi: 10.1002/1878-0261.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prabhu AV, Crihalmeanu T, Hansberry DR, et al. Online palliative care and oncology patient education resources through Google: Do they meet national health literacy recommendations? Pract Radiat Oncol. 2017;7:306–310. doi: 10.1016/j.prro.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 24.Dennis K, Harris G, Kamel R, et al. Rapid access palliative radiotherapy programmes. Clin Oncol. 2020;32:704–712. doi: 10.1016/j.clon.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Job M, Holt T, Bernard A. Reducing radiotherapy waiting times for palliative patients: The role of the Advanced Practice Radiation Therapist. J Med Radiat Sci. 2017;64:274–280. doi: 10.1002/jmrs.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gutt R, Malhotra S, Hagan MP, et al. Palliative radiotherapy within the Veterans Health Administration: Barriers to referral and timeliness of treatment. Int J Radiat Oncol Biol Phys. 2020:108. doi: 10.1200/OP.20.00981. [DOI] [PubMed] [Google Scholar]
- 27.Schuster JM, Smith TJ, Coyne PJ, Lutz S, Anscher MS, Moghanaki D. Clinic offering affordable radiation therapy to increase access to care for patients enrolled in hospice. J Oncol Pract. 2014;10:e390–e395. doi: 10.1200/JOP.2014.001505. [DOI] [PubMed] [Google Scholar]
- 28.van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: Cost-utility analysis based on a randomized trial. J Natl Cancer Inst. 2003;95:222–229. doi: 10.1093/jnci/95.3.222. [DOI] [PubMed] [Google Scholar]
- 29.Stavas MJ, Pagan JD, Varma S, Li B, Kachnic LA. Building a palliative radiation oncology program: From bedside to B.E.D. Pract Radiat Oncol. 2017;7:203–208. doi: 10.1016/j.prro.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Jarosek SL, Virnig BA, Feldman R. Palliative radiotherapy in Medicare-certified freestanding hospices. J Pain Symptom Manage. 2009;37:780–787. doi: 10.1016/j.jpainsymman.2008.05.003. [DOI] [PubMed] [Google Scholar]