Abstract
Background
This study aimed to evaluate the effectiveness of implementing evidence-based preoperative nursing interventions in reducing postoperative infections and intensive care unit (ICU) length of stay among liver transplant recipients.
Material/Methods
A controlled study was conducted, comparing postoperative outcomes between an intervention group receiving standardized, evidence-based preoperative care and a control group receiving routine preoperative care. Patients undergoing elective liver transplantation from September 2020 to March 2021 were included and assigned to either the intervention or control group. The intervention group received preoperative interventions based on best available evidence, while the control group received standard preoperative care. The primary outcomes measured were postoperative infection rates and length of ICU stay.
Results
In the control group the overall Intensive Care Unit (ICU) length of stay was 3 days and the infection rate was 33.30%, while in the intervention group it was 3 days and 13.80% (P<0.05). There was no significant difference in the length of ICU stay between the control and the intervention groups (P>0.05). There was a significant improvement in the awareness, acceptance, and compliance of doctors and nurses.
Conclusions
Using the best evidence-based intervention for preoperative nursing of liver transplantation patients can standardize preoperative nursing behavior. Although we did not find significant differences in outcomes before and after the intervention, it is necessary to prevent postoperative infection and improve nursing compliance.
Keywords: Evidence-Based Nursing, Liver Transplantation, Postoperative Complications, Preoperative Care
Introduction
Liver transplantation surgery has become the most effective method for treating end-stage liver disease [1]. With continuing improvements in transplant technology and using novel immunosuppressive agents, the postoperative survival rate of patients receiving a liver transplant has greatly increased. Despite the progress in liver transplantation techniques, however, the incidence of infections has increased in recent years [2–5]. Research indicates that infection is the most common cause of death following liver transplantation, especially within the first year after transplant [6–8]. Despite a steady decline in infectious disease-related mortality in non-transplant settings, it remains a significant concern in the context of liver transplantations [6–8]. According to a survey conducted by the European Institute, the early postoperative infection rate in patients receiving a liver transplant ranges from 37.9% to 66.0% [9]. Among these infections, the proportion of deaths caused by infections accounts for 20.0% of the overall mortality rate [10]. Surgical site infection (SSI) definitions include superficial and deep incisional infections, and organ/organ space infections that occur within 30 days after the surgical procedure. Local signs of pain, swelling, erythema, and purulent drainage provide the most reliable information in diagnosing SSI. In addition, many patients with SSI develop fever and/or leukocytosis. Common pathogens associated with postoperative infections after liver transplantation include multidrug-resistant Pseudomonas aeruginosa, Enterococcus species, and various fungal infections [11–13]. Infections crucially affect the survival rate and quality of life of liver transplant patients.
Chinese and international studies have consistently demonstrated that providing certain preoperative interventions for liver transplant patients can effectively prevent postoperative infections [14,15]. As stated in the 2018 WHO Global Guidelines for the Prevention of Surgical Site Infection (2nd edition) [16], measures that include preoperative prophylactic antibiotic use and administration of oral or enteral nutritional formulas containing multiple nutrients to underweight patients undergoing major surgery can help prevent surgical site infections (SSIs). The CDC Guideline for the Prevention of Surgical Site Infection [17] recommends that patients use antiseptic/non-antimicrobial soap or other antimicrobial agents to shower or bathe the night before the surgery at the latest. This practice has been shown to effectively prevent postoperative SSIs and other related complications. According to the national organ procurement standards (false-positive and false-negative risks), infection risk screening should be conducted for organ donors [18,19], and donor-derived infections carried by organ transplant donors must be carefully assessed. A balance needs to be struck between the urgent need for liver transplantation and the potential infection risks associated with deceased organ donors.
Although a series of measures have been taken in our center to prevent postoperative infections, a unified standard and protocol have not yet been established, and relevant training materials in the department have not been updated in a timely manner. This study aimed to apply the best available evidence concerning preoperative interventions to prevent postoperative infections in patients receiving a liver transplant, establish standardized preoperative intervention procedures, reduce the incidence of early postoperative infections, promote recovery, and provide references for formulation of standardized processes in China [20,21].
Material and Methods
Literature Review and Evaluation
This study followed the principles of the evidence retrieval pyramid to conduct systematic research retrieval. Evidence-based resources related to preoperative interventions in liver transplant surgery patients were retrieved, including clinical practice guidelines, systematic reviews, evidence summaries, and primary research studies. The Chinese keywords used were ‘liver transplant surgery’, ‘infection’, and ‘preoperative intervention’. The English keywords used were ‘liver transplantation’, ‘infection’, and ‘preoperative intervention’. The following databases were searched: NICE, Cochrane Library, BMJ Best Practice, UptoDate, the British Transplantation Society, Medlinker, Guideline Central, PubMed, and China Biology Medicine (CBM, from January 2017 to the present, published in both Chinese and English). The inclusion criterion was patients awaiting a liver transplant. The exclusion criteria were: patients awaiting a liver transplant with severe infections, and studies published before 2017. A total of 63 papers were retrieved from NICE (1), Cochrane (23), BMJ (1), Guideline Central (2), UpToDate (26), PubMed (1), Medlinker (3), and CBM (6). After excluding 57 papers, including 20 duplicates, 11 inappropriate paper types, and 26 papers with irrelevant content, we finally included 7 papers.
Through the literature review, we identified 3 criteria for inclusion in this study. Guideline evaluation: The Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool was used, which includes 6 dimensions. The score for each dimension was calculated using the following formula:
| [ 10]. |
Based on the standardized scores obtained, the NICE guideline demonstrated strong overall quality, with the following scores for each of the 6 dimensions: scope and purpose (97%), stakeholder involvement (93.75%), development rigour (90.48%), clarity of presentation (89.58%), applicability (83.33%), and editorial independence (83.33%). The average score across all dimensions was 89.58%, indicating a high level of recommendation for the NICE guideline. The APSIC guidelines for the prevention of surgical site infection (Guideline.net) achieved scores above 90% in all 6 dimensions, with an average score of 94.65%, indicating strong recommendation. The Chinese Surgical Site Infection Prevention Guidelines (Medlinker) achieved scores above 80% in all 6 dimensions, with an average score of 88.22%, also indicating strong recommendation. In terms of system assessment, a Joanna Briggs Institute 2015 (JBI2015) evaluation [22,23] was conducted. Two team members conducted evaluations of a systematic review from PubMed and 2 expert consensus articles. Based on the results, the systematic review received 17 ‘A’ ratings and 5 ‘C’ ratings, indicating moderate overall quality. Both expert consensus articles were approved.
Identifying Evidence-Based Nursing Issues
Infection is an important factor affecting the survival rate and quality of life of patients receiving a liver transplant. Currently, routine skin preparation is performed in our department for patients receiving a liver transplant, but no routine assessment of lung function or standardized pulmonary exercise has been implemented. Guidelines are also needed for the multimodal rehabilitation of patients with post-intensive care syndrome (PICS), a variable and complex syndrome that requires an individualized multidisciplinary and multi-professional approach. The rehabilitation of PICS should include an assessment and therapy of motor, cognitive, and psychological health impairments [24]. This present study was an integrative review of the international health literature on health equity in relation to clinical practice guidelines (CPGs). Understanding how equity is discussed in the literature relative to CPGs has implications for their uptake by and utility for HCPs in their goal of providing equitable healthcare. The successful and equitable implementation of CPGs could be improved if equity were more clearly articulated within all aspects of the CPG process, including conceptualization, development, implementation, and evaluation [25]. However, the evidence suggests that routine skin preparation should be avoided, and routine assessment of lung function and pulmonary exercise should be included.
In the PIPOST framework, evidence-based issues are conceptualized as follows: 1) Population (P): patients undergoing scheduled liver transplant surgery. 2) Intervention (I): I1: skin preparation; I2: pharmacological intervention; I3: nutritional interventions; I4: pulmonary exercise for lung function improvement; I5: assessment of potential donor infection risks. 3) Professionals (P): attending physicians and nurses. 4) Outcomes (O): O1: patient-level outcomes including the incidence of postoperative infections, ICU length of stay, and the infection prevention knowledge of patients pre-transplant. O2: practitioner-level outcomes including awareness, acceptance, and adherence to evidence. O3: system-level outcomes including the enhancement of nursing protocols for preoperative infection prevention in patients receiving a liver transplant. 5) Setting (S): general surgery center with 110 beds, 40 doctors and 70 nurses performing 150 liver transplant surgeries annually. There are existing preoperative nursing protocols for liver transplant procedures, but aspects of these are outdated and not regularly updated. 6) Type of evidence (T): Clinical practice guidelines, expert consensus, and systematic reviews.
Microbiology and Diagnosis of Postoperative Infections
Postoperative infections in liver transplant patients can be caused by a wide range of microorganisms, including bacteria, viruses, and fungi. In this study, postoperative infections were diagnosed based on a combination of clinical signs and symptoms, laboratory tests, and microbiological culture results.
Bacterial infections were identified through positive cultures from blood, respiratory specimens (sputum, bronchoalveolar lavage), urine, or surgical site samples. Common bacterial pathogens included Gram-negative bacilli (eg, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa), Gram-positive cocci (eg, Staphylococcus aureus, Enterococcus species), and anaerobes (eg, Bacteroides fragilis).
Viral infections were diagnosed through serological testing or molecular assays (eg, polymerase chain reaction) for specific viruses, such as cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus (HSV), and respiratory viruses (influenza, respiratory syncytial virus).
Fungal infections, particularly invasive candidiasis and aspergillosis, were identified through positive cultures from sterile body fluids or tissue samples, in conjunction with radiological findings and clinical manifestations.
Preoperative antimicrobial prophylaxis typically involved the administration of a broad-spectrum antibiotic, such as a third-generation cephalosporin (eg, ceftriaxone) or a combination of an aminoglycoside and an anti-anaerobic agent (eg, gentamicin and metronidazole). Postoperative antimicrobial prophylaxis was guided by culture results and targeted against specific pathogens identified in each patient.
For the prevention and management of opportunistic infections, specific prophylactic and pre-emptive strategies were employed. CMV prophylaxis or pre-emptive therapy was based on regular monitoring of CMV viral load and the use of antiviral agents (eg, valganciclovir, ganciclovir) when indicated. Pneumocystis jirovecii pneumonia (PJP) prophylaxis involved the use of trimethoprim-sulfamethoxazole or alternative agents (eg, dapsone, atovaquone) in high-risk patients. HSV prophylaxis was achieved through the administration of antiviral agents (eg, acyclovir, valacyclovir) during the early post-transplant period.
Ethics approval and consent to participate: This research was reviewed and approved by the Ethics Committee of Beijing Youan Hospital Capital Medical University. The Ethics Committee archive number is LL-2023-166-K, and the approval number is [2024]003.
Clinical application of the evidence: This study adopted the standard procedure of the JBI clinical evidence practice application system, employing a non-concurrent controlled study conducted in 3 steps: a baseline quality review, clinical practice change, and a round-two quality review.
Summary of evidence and translation quality appraisal indicators: Seventeen relevant pieces of evidence related to the topic were summarised. These were independently evaluated in terms of feasibility, appropriateness, clinical significance, and effectiveness in terms of evidence application using the JBI’s FAME evaluation model [26]. In case of divergent opinions, a third researcher participated in the discussion to reach a consensus. Evidence 3: There is currently controversy surrounding the use of a glucose chlorhexidine solution for bathing, and the evidence level in this regard is low; accordingly, it was not adopted. Evidence 9: The relationship between postoperative infection and patient nutrition was assessed. Evidence 10 and 11: Control of blood glucose for patients was evaluated. These 3 evidence categories were not included due to difficulties in their clinical adoption and implementation, as well as their low recommendation levels. Finally, 13 pieces of evidence were included and discussed by the team, resulting in the formulation of 7 relevant quality appraisal indicators through thorough discussion. The corresponding review methods for each indicator were also determined (Table 1).
Table 1.
Evidence translation quality appraisal table.
| Evidence | Review indicators | Review methods |
|---|---|---|
| 1. It is a good clinical practice to give patients a bath or shower before surgery. The expert panel suggests that for this purpose, regular soap or antibacterial soap can be used (conditionally recommended, moderate quality evidence) [16] | 1. The nurse instructs liver transplant patients to shower with regular soap the day before surgery | View nursing records |
| 2. The night before (or earlier) the day of surgery, patients should take a shower or full-body bath using antibacterial/non-antibacterial soap or other antibacterial agents (conditionally recommended, moderate quality evidence) [16] | 2. Routine preparation does not include shaving for patients preparing for surgery; if excessive body hair affects surgical visibility, it can only be removed with scissors | View nursing records |
| 3. It is not recommended to remove hair from patients preparing for surgery. If necessary, only scissors should be used to remove hair. Whether it is before surgery or in the operating room, the use of razors to remove hair is strongly discouraged (strongly recommended, moderate quality evidence) [16] | 3. Prophylactic antibiotics are administered within 120 minutes prior to surgery | View nursing records |
| 4. It is recommended to prophylactically use antibiotics when necessary before surgical incision [16] | 4. Patients with low body weight, specifically a BMI below 18.5, are given oral or nasal nutrition solutions | View the record sheet |
| 5. It is recommended to administer prophylactic antibiotics within 120 minutes before surgical incision. However, consideration should also be given to the half-life of the antibiotic [16] | 5. For patients with high-risk factors prior to surgery, nurses guide them in performing pulmonary | Lung function exercise record sheet |
| 6. Underweight patients undergoing major surgery are recommended to receive oral or enteral nutrition containing a variety of nutrients to prevent surgical site infections (SSI) [15] | 6. Specific plan for pulmonary function exercises | Check the medical orders and nursing records |
| 7. ”Underweight” refers to individuals with a weight that is below healthy standards. This definition typically applies to individuals with a body mass index (BMI) below 18.5, or individuals whose weight is 15–20% below the normal range for their age and height [15] | 7. Prior to surgery, doctors use the national organ procurement standards to conduct infection risk screening for organ donors | |
| 8. One of the important components of Enhanced Recovery After Surgery (ERAS) is airway management, which, when applied in clinical practice, can reduce pulmonary complications [25] | ||
| 9. Preoperative pulmonary rehabilitation training can reduce the occurrence of postoperative complications [25] | ||
| 10. Common high-risk factors in patients prior to surgery include: Advanced age: Age ≥65 years (if combined with smoking, males aged >60 years and females aged >70 years are considered advanced age). Long-term heavy smoking (smoking history ≥400 pack-years). Tracheal colonization with bacteria. Airway hyperresponsiveness. Peak expiratory flow (PEF) <250 L/min. Marginal lung function, requiring pulmonary function exercise [25] | ||
| 11. Specific pulmonary function exercise program. | ||
| 12. Potential infections carried by organ transplant donors, known as donor-derived infections, require a careful evaluation of the potential infection risk in organ donors[25] | ||
| 13. Organ donors were screened for the risk of infection according to the national organ procurement criteria (false positive and false negative risk) (BIII) [17,18] |
Evidence 1 and 2 correspond to review index 1; evidence 3 corresponds to review index 2; evidence 4 and 5 correspond to review index 3; evidence 6 and 7 correspond to review index 4; evidence 8,9 and 10 correspond to review index 5; evidence 11 corresponds to review index 6; evidence 12 and 13 should review index 7.
Data Collection Method
Patients undergoing elective liver transplantation between 21 September 2020 and 25 March 2021 were included in the study. Inclusion criteria for the infection group were: Surgical site infections occurring near or at the incision site and/or deeper underlying tissue spaces and organs within 30 days of a surgical procedure (or up to 90 days for implanted prosthetics). The general surgery center includes the general surgery ward, a transplant center, and an ICU, with a total of 110 beds, 40 doctors and 70 nurses. More than 150 liver transplant surgeries are performed annually in Beijing Youan Hospital, averaging more than 70 cases per month. Prior to the intervention, the existing preoperative nursing protocols for liver transplant procedures were outdated and lacked comprehensiveness in certain aspects, necessitating updates and improvements. Following the standard procedures of the JBI Centre for Evidence-Based Nursing Practice Application System, a baseline review was conducted between 21 September 2020 and 20 October 2020. The length of postoperative hospital stay and the postoperative infection rate of patients receiving a liver transplant were evaluated as outcome indicators, along with the knowledge, acceptance, and implementation rates of practitioners for each evidence type, and the results before and after practice changes were compared to assess the effectiveness of the evidence application. All patients were of the same ethnicity.
The evaluation index included: the recognition level of surgeons and nurses regarding preoperative intervention measures for patients receiving a liver transplant; postoperative incidence, and days of ICU stay in patients receiving a liver transplant; and the intervention implementation rate by surgical nurses. A self-designed questionnaire was used to investigate the level of awareness about preoperative interventions in patients receiving a liver transplant and the intervention implementation rate by surgical nurses. On-site observation and a review of care records were implemented to collect postoperative incidence and ICU stay days among patients receiving a liver transplant.
The questionnaire on the recognition level of surgeons and nurses about preoperative interventions for patients receiving a liver transplant was designed by a team of healthcare professionals, based on the best available evidence and developed after 2 rounds of expert consultation. The total content validity was 0.933, and the overall Cronbach’s α coefficient of the questionnaire was 0.969. The questionnaire included 20 questions, with 5 points assigned to each question for a total score of 100 points. The higher the score, the better the indicated mastery. The nurse implementation rate questionnaire consisted of 7 items, which were used to evaluate implementation of the indicators. Each index has a corresponding score, which is calculated to evaluate the implementation rate of nurses.
Evidence-Based Practice
Planning Phase
From 1 November 2020 to 5 December 2020 (5 weeks), the project entered the planning phase. With the support of mentors from the Evidence-Based Nursing Centre, nursing department leaders, ward directors, and head nurses, the project team held a project kick-off meeting and an evidence interpretation meeting. After extensive discussions and consultations within the team, the following transformation measures were formulated:
The nursing protocols for preoperative interventions in elective patients receiving a liver transplant were revised, supplemented, and improved. The specific improvement measures are as follows: 1) A soapy water bath the day before surgery was included in the standard preoperative nursing process; 2) a preoperative nutritional evaluation process and programme was developed for nutritional intervention; 3) a unified standard was formulated, including the selection of a body hair removal instrument for skin preparation, thereby improving this instrument. The knife head was changed to a one-time replaceable blade, the size of the mesh was adjusted for hair density, and a temperature control device was included; 4) Pulmonary function was evaluated based on the patient’s medical history, smoking history, and blood gas results; and 5) a lung function intervention program and unified exercise standards were formulated in the department, and training was conducted on pulmonary function detection. Patients with preoperative risk factors were defined as follows: 1) advanced age: 65 years (male >60 years; female >70 years); 2) long-term heavy smoking (smoking history of 40 years); 3) tracheal bacteria colonization; 4) airway hyperresponsiveness; 5) PEF <250 L/min; 6) marginal previous lung function exercise (nurses guided patients for lung function exercise before surgery).
After revising and improving the evidence-based practice protocols, considering the baseline review findings regarding healthcare providers’ knowledge and compliance with preoperative interventions for patients receiving a liver transplant, a lecture on evidence interpretation was organized for doctors and nurses during a collective professional development session. The lecture aimed to interpret and provide relevant training using the evidence on low compliance rates, thereby enhancing understanding among doctors and nurses of the evidence and increasing their attention to it. The operational procedures and methods for the revised nursing measures were uploaded to the department’s WeChat group for everyone to study. Questions were addressed and/or periodic assessments were conducted after the morning shift handover to reinforce patient and family education and raise awareness. Family members were also guided on the correct exercise methods.
Implementation Phase
In this phase, the revised protocols and interventions were implemented. The specific activities included: 1) The department purchased hair dryers. Before bathing, the temperature in the ward was raised, and clean patient gowns and hair dryers were prepared to assist in drying the patients’ hair after bathing. 2) The department purchased a multifunctional weighing scale to replace its old weighing scale. It measures height and weight, calculates the BMI index directly, and sets reminder (if below or above the normal BMI value) indicators. 3) A hair removal device was also purchased for surgical site preparation. Depending on the patient’s hair density, the appropriate method of skin preparation was chosen. For patients with dense hair, the hair is first trimmed using scissors; then, the hair removal device is used for secondary skin preparation. 4) Based on the patient’s medical history, smoking history, and blood gas results, lung function was assessed, and a standardized lung function exercise protocol was developed. 5) The subjects were asked to perform 2 inhalations with their incentive spirometers in the first flow indicator condition. Inspiratory volume was measured by the peak height of the volume displacement float. The department purchased incentive spirometers and conducted unified training within the department.
Study Phase
During the study phase, the team conducted regular assessments and quality control measures to monitor compliance and identify barriers. The following activities were carried out: When a surgical procedure site is located at a hairy part of the body, hair removal is usually performed. This is related to the epidemiology of postoperative wound infection [27]. During the on-site inspection of nurses’ adherence to protocols and accurate recording in the nursing records, it was found that during the practice change phase (between 1 November 2020 and 5 December 2020), Indicator 2, which states ‘Routine surgical patients should not be prepped unless excessive body hair affects surgical visibility, in which case only scissors should be used for hair removal’, had a compliance rate of 0%. Using a fishbone diagram to analyze the reasons for this result, the following barriers were identified: 1) low acceptance by doctors due to concerns about the impact of hair on wound healing; and 2) low awareness and a lack of experience among nurses. Based on the analysis of these barriers, updated practice change measures were implemented. A hair removal device was purchased for surgical site preparation. Depending on the patient’s hair density, the appropriate method of skin preparation was selected. For patients with dense hair, the hair was first trimmed using scissors, and then the hair removal device was used for secondary skin preparation.
Act Phase
Based on the findings from the study phase, the team made adjustments and implemented additional measures to address the identified barriers and improve compliance.
Statistical Methods
After quantifying and organizing all the data, a two-person team cross-checked and entered the data into Excel. Statistical analysis was conducted using SPSS 23.0 software (IBM, Armonk, NY, USA). For continuous variables, the Shapiro-Wilk test was first used to test for normality. Data that followed a normal distribution were expressed as mean±standard deviation, and t tests were used for intergroup comparisons. Data that did not follow a normal distribution were expressed as a median (interquartile range), and the Mann-Whitney U test was used for intergroup comparisons. Categorical variables were presented as counts (%) and compared between groups using the chi-square test. All tests were two-tailed, and the significance level was set at 0.05.
Results
General Data of the Study Participants
Data was collected using questionnaire surveys, on-site observations, and by reviewing nursing records. The baseline review results before evidence application were as follows: Indicator 1, regarding showering with soap and water, had a knowledge rate of 92.4% and an execution rate of 71%. Indicator 2, regarding skin preparation, had a knowledge rate of 86% and an execution rate of 0%. Indicator 3, regarding antibiotic use, had a knowledge rate of 94.9% and an execution rate of 100%. Indicator 4, regarding BMI, had a knowledge rate of 88.6% and an execution rate of 0%. Indicator 5, regarding pulmonary function, had a knowledge rate of 63% and an execution rate of 2.5%. Indicator 6, regarding the pulmonary function exercise program, had a knowledge rate of 41% and an execution rate of 2.5%. Indicator 7, regarding the donor, had a knowledge rate of 96.2% and an execution rate of 98.7%. In the control group, the minimum postoperative ICU stay was 1 day, the maximum was 11 days, and the median was 3 days. There were 8 cases of postoperative infections and 16 cases without infections, including 4 cases of pulmonary infections, 2 cases of abdominal infections, and 1 case each of abdominal and central venous infections. The overall infection rate was 33.30%. The most common infections were pneumonia (caused by Pseudomonas aeruginosa and Klebsiella pneumoniae), followed by abdominal infections (caused by Enterococcus faecalis and Bacteroides fragilis), central line-associated bloodstream infections (caused by Staphylococcus aureus), and surgical site infections (caused by Staphylococcus aureus and Enterococcus faecalis).
The control group included 24 patients, with 23 males and 1 female. The mean age was 56 (29–65) years, BMI index was 24.97±4.10, and the mean preoperative hospital stay was 2 (1–26) days. The intervention group included 64 patients, with 52 males and 12 females. The mean age was 54 (29–67) years, BMI index was 24.08±4.02, mean preoperative hospital stay was 3 (1–33) days. In addition, we further analyzed the impact of the incidence of obesity, diabetes, and kidney disease on the 2 groups. The results showed that the rates of obesity, diabetes, and kidney disease were basically the same in the 2 groups (Table 2).
Table 2.
General data of the study subjects.
| Index | Control group (n=24) | Intervention group (n=64) | p-value |
|---|---|---|---|
| Gender (Male/Female) | 23/1 | 52/12 | 0.32* |
| Age | 56 (29, 65) | 54 (29, 67) | 0.61** |
| BMI index | 24.97±4.10 | 24.08±4.02 | 0.34*** |
| Preoperative hospitalization days | 2 (1, 26) | 3 (1, 33) | 0.18** |
| MELD score | 22 (12, 35) | 20 (8, 40) | 0.27** |
| Primary liver cancer | 11 | 25 | – |
| Drug-induced liver injury | 0 | 2 | – |
| Decompensated hepatitis B cirrhosis | 5 | 18 | – |
| Decompensated hepatitis C cirrhosis | 0 | 3 | – |
| Decompensated alcoholic cirrhosis | 1 | 9 | – |
| Liver failure | 5 | 6 | – |
| Autoimmune liver disease | 2 | 1 | – |
| Cholestatic cirrhosis | 0 | 1 | – |
| Spontaneous bacterial peritonitis (SBP) | 0 | 0 | – |
| Receive antibiotics | 5 | 8 | 0.54* |
| Diabetes | 4 | 9 | 0.76* |
| Obesity | 2 | 3 | 0.67* |
| Kidney disease | 3 | 3 | 1.00* |
p-value calculated using chi-square test;
p-value calculated using Mann-Whitney U test;
p-value calculated using t-test.
Analysis of Barrier Factors
Based on the baseline review results, an analysis of the review indicators was conducted, and a fishbone diagram was used to represent the findings. After project team discussions, the following barriers were identified: 1) Insufficient emphasis and inadequate patient education by nurses: patients and their families lacked knowledge and worried that bathing could cause a fever and affect the surgery on the following day. 2) Lack of corresponding guidelines: low room temperature in the ward environment. 3) Low nurse awareness and a lack of experience: doctors were worried that hair at the incision site could affect wound healing, resulting in poor compliance. 4) Conflict between the evidence and original guidelines: a lack of skin and follicle-friendly equipment available for skin preparation without causing damage; skin preparation scissors were used inappropriately. 5) Concerns among doctors about increased patient costs; patients found the taste of nutritional fluid unpleasant. 6) A lack of proceduralized preoperative nutritional assessment and intervention. 7) A lack of knowledge and insufficient emphasis on infection prevention after liver transplantation among doctors, nurses, and patients; families. 8) Due to the COVID-19 pandemic, lung function exercise testing was unavailable and the risk of aerosol transmission due to detection is greater; a lack of uniform standards for pulmonary function exercise was also observed.
Level of Preoperative Intervention Implementation by Surgeons and Nurses for Patients Receiving a Liver Transplant Before and After the Application of Evidence
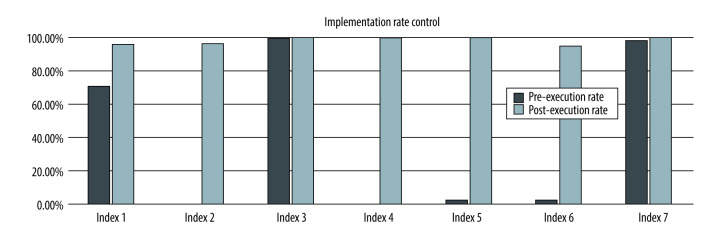
This study employed a self-designed questionnaire to investigate the implementation rate of evidence during the baseline review and after the process of promotion and practice change. Then, we studied the variables of pre- and postoperative quality control. Because the respondents represented the same group before and after the implemented changes, the groups were comparable. The results showed that the implementation level of most review indicators increased as a result of following the evidence (P<0.05) (Table 3).
Table 3.
Implementation of the best evidence before and after the application of evidence.
| Review indicators | Baseline | Application of evidence | χ2 | P-value | ||||
|---|---|---|---|---|---|---|---|---|
| Execution (cases) | Not executed (cases) | Execution rate (%) | Execution (cases) | Not executed (cases) | Execution rate (%) | |||
| Indicator1 | 56 | 23 | 71.00 | 80 | 3 | 96.30 | 320.05 | <0.01 |
| Indicator2 | 0 | 79 | 0.00 | 80 | 3 | 96.30 | 4636.85 | <0.01 |
| Indicator3 | 79 | 0 | 100.00 | 83 | 0 | 100.00 | 0.00 | <0.01 |
| Indicator4 | 0 | 79 | 0.00 | 83 | 0 | 100.00 | 5000.00 | <0.01 |
| Indicator5 | 2 | 77 | 2.50 | 83 | 0 | 100.00 | 4753.13 | <0.01 |
| Indicator6 | 2 | 77 | 2.50 | 79 | 4 | 95.00 | 4278.13 | <0.01 |
| Indicator7 | 78 | 1 | 98.70 | 83 | 0 | 100.00 | 0.845 | 0.017 |
Postoperative ICU Days and the Incidence of Postoperative Infection
In the control group, the mean postoperative ICU stay was 3 (range, 1–11) days. Twenty-three patients were transferred to regular wards for further treatment, 1 patient was discharged automatically, and there were no deaths. There were 16 cases without infection after surgery and 8 cases with an infection. Among the cases with an infection, there were 4 pulmonary infection cases, 2 abdominal infection cases, and 1 case each of abdominal and central venous infections. The overall infection rate was 33.30%.
In the intervention group, the mean postoperative ICU stay was 3 (range, 1–28) days. Among them, 58 patients were transferred to regular wards for further treatment, 3 patients died, and 3 patients were discharged automatically. There were 55 cases without infection after surgery and 9 cases with infection. Among the cases with an infection, there were 2 cases of pulmonary infection, 1 case of abdominal infection, 2 cases of abdominal and pulmonary infection, 1 case of abdominal and thoracic infection, 2 cases of wound infection, and 1 case of biliary tract infection. The overall infection rate was 14.10% (Table 4). The most common infections were pneumonia (caused by Pseudomonas aeruginosa and Haemophilus influenzae), followed by abdominal infections (caused by Escherichia coli and Enterococcus faecium), surgical site infections (caused by Staphylococcus aureus), and biliary tract infections (caused by Enterococcus faecalis).
Table 4.
Patient outcome measures.
| Control group | Intervention group | P-value | |
|---|---|---|---|
| ICU length of stay (days) | 3 (1, 11) | 3 (1, 28) | 0.714 |
| Postoperative infection rate (%) | 33.3 | 14.1 | 0.039 |
P<0.05 indicated that the difference was statistically significant.
Execution Rate of Surgical Nurses
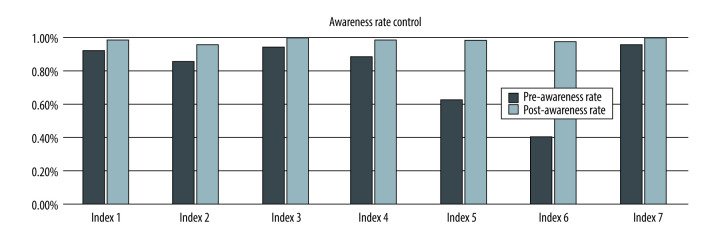
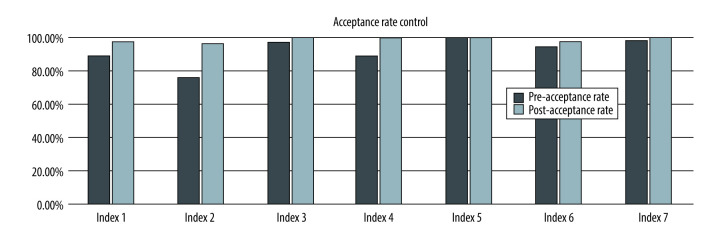
A pre-interpretation survey was conducted with a total of 79 respondents, including 8 doctors and 71 nurses. Among them, there were 42 practitioners with junior professional titles, 34 with intermediate professional titles, 2 vice directors, and 1 director. After the interpretation of evidence and clinical promotion, a post-interpretation survey was conducted with a total of 83 respondents, including 12 doctors and 71 nurses. The distribution of professional titles remained similar, with 43 practitioners having junior professional titles, 35 with intermediate professional titles, 2 vice directors, and 3 directors. By comparing the selected review indicators, the gaps between the current situation and the evidence were identified. After the interpretation of evidence and its promotion in clinical practice, there was a significant improvement in the awareness, acceptance, and implementation rates of the review indicators by doctors and nurses (Figures 1–3).
Figure 1.
The awareness rate of practitioners.
Figure 2.
Practice acceptance rate control chart.
Figure 3.
Practitioner execution rate control chart.
Clinical Factors Associated with Postoperative Infections
Several clinical factors were identified as potential risk factors for postoperative infections in the study population. These included advanced age (≥65 years), prolonged preoperative hospital stay (>7 days), high Model for End-Stage Liver Disease (MELD) score (≥25), presence of comorbidities (eg, diabetes mellitus, chronic obstructive pulmonary disease), and prolonged operative time (>6 h).
These risk factors have been associated with an increased risk of SSIs and other postoperative infections in liver transplant recipients due to factors such as impaired wound healing, immunosuppression, and prolonged exposure to potential sources of infection [28,29]. Patients with these risk factors were closely monitored for the development of postoperative infections and received targeted preventive measures, such as extended antimicrobial prophylaxis or intensified surveillance.
Safety and Adverse Events
The implementation of the evidence-based preoperative interventions was closely monitored for any potential adverse events or unintended consequences. No significant adverse events were observed in either the intervention or control group. There were no reported cases of delayed transplantation times or increased workload for nursing staff that could negatively impact patient care.
Discussion
Improving the preoperative nursing standard of patients undergoing surgical liver transplantation surgery can effectively reduce the postoperative infection rate
By reviewing the results of clinical practice, this study identified gaps in the selected review indicators, implemented changes, and improved preoperative care guidelines for patients undergoing liver transplantation. This led to the standardization and visualization of the preoperative nursing process. Regarding outcomes, there was no statistically significant difference in the length of stay in the ICU for patients before and after the practice transformation. This may be attributed to the short duration and insufficient sample size of the study. However, there was a statistically significant difference in infection rates, indicating a noticeable decrease in postoperative infection rates after the adoption of evidence-based protocols. This effectively improved the quality of patient care and enhanced outcomes.
Detailed Evidence Interpretation and Strict Quality Control Standardize the Operation Procedures of Nurses and Ensure Implementation of the Best Evidence
Through clinical practice, a comparison was made between the healthcare professionals’ awareness, acceptance, and implementation rates of evidence and the selected review indicators. This helped to identify gaps between the current situation and the evidence. As a result of interpreting the evidence and promoting its clinical application, a significant improvement was observed in healthcare professionals’ awareness, acceptance, and implementation rates concerning the review indicators. This facilitated the translation of evidence into clinical practice and enhanced the adherence of clinical staff to evidence-based practices. Importantly, the findings demonstrated a statistically significant reduction in postoperative infection rates after the implementation of the evidence-based interventions, indicating the positive impact of these practices on patient outcomes.
Evidence Application Promotes New Product Development
Evidence-based practice should consider the specific circumstances of each hospital department. However, it is important to address concerns and cognitive biases among doctors to improve their acceptance of established evidence. In this case, the low acceptance of providing preoperative skin preparation for patients with hair near the incision site may have been due to ingrained beliefs regarding the potential impact of hair on wound healing. To address this issue, a compromise solution was implemented. For patients with dense body hair, the hair was initially trimmed with scissors before using a hair removal device for skin preparation. For those with sparse and soft body hair, the hair removal device was directly used for skin preparation. To further prevent infection after liver transplantation, it would be beneficial to continue promoting the benefits of evidence-based practices and seeking opportunities for the widespread implementation and dissemination of the patented device.
Limitations
Due to limited time and a small sample size, further follow-up is required to track the impact of evidence-based nursing measures on ICU length of stay. Additionally, this was a single-center study, and multi-center research is warranted to verify our results. Moreover, the effectiveness of implementation of some review indicators remains suboptimal, even after evidence application, suggesting the need for ongoing optimization and the continuous improvement of relevant processes and systems, which will also be a focus of our future research.
Conclusions
This study strictly followed the 3 stages of evidence-based nursing for evidence translation and application to enhance preoperative nursing standards and intervention protocols for preventing postoperative infections in patients receiving a liver transplant and achieving standardized care. The positive effects of evidence-based preoperative interventions in clinical practice have been recognised and, by combining theory and practice, support has been made available for surgical healthcare professionals to update their professional knowledge, change their work philosophy, improve their work methods, ensure patient safety, and effectively reduce the rate of postoperative infections in patients receiving a liver transplant.
Abbreviations
- JBI
Joanna Briggs Institute
- ICU
Intensive Care Unit
- SSI
surgical site infections
- NICE
National Institute for Healthcare Excellence
- The AGREE II
Appraisal of Guidelines for Research and Evaluation II
- ERAS
enhanced recovery after surgery
- BMI
body mass index
- PEF
peak expiratory flow
Footnotes
Conflict of interest: None declared
Ethics Statement: The studies involving human participants were reviewed and approved by the Beijing Youan Hospital of China Capital Medical University.
Declaration of Figures’ Authenticity: All figures submitted were created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Financial support: Beijing Hospitals Authority Youth Programme, QML20211714; Beijing Hospitals Authority Youth Programme, QML20231704; Beijing You’an Hospital, Capital Medical University, 2021 Hospital Young and middle-aged Talents Incubation Project (special construction project-nursing research), No. YAKTHL2021006 and No. YAKTHL2021003; Beijing You’an Hospital, Capital Medical University, 2023 Hospital Young and middle-aged Talents Incubation Project (special construction project-nursing research), No. BJYAYY-YN2023-23
References
- 1.Zhang P, Xu P, Duan Z, et al. Effects of admission systemic inflammatory indicators on clinical outcomes in patients with vertebrobasilar artery occlusion: Insight from the PERSIST registry. J Neurointerv Surg. 2023;15(e2):e270–e76. doi: 10.1136/jnis-2022-019437. [DOI] [PubMed] [Google Scholar]
- 2.Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007;357(25):2601–14. doi: 10.1056/NEJMra064928. [DOI] [PubMed] [Google Scholar]
- 3.Idossa DW, Simonetto DA. Infectious complications and malignancies arising after liver transplantation. Anesthesiol Clin. 2017;35(3):381–93. doi: 10.1016/j.anclin.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Leibovici-Weissman Y, Anchel N, Nesher E, et al. Early post-liver transplantation infections and their effect on long-term survival. Transpl Infect Dis. 2021;23(4):e13673. doi: 10.1111/tid.13673. [DOI] [PubMed] [Google Scholar]
- 5.Esquivel CO. Liver transplantation: Where we are and where we are heading. Transplant Proc. 2010;42(2):610–12. doi: 10.1016/j.transproceed.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Washington K. Update on post-liver transplantation infections, malignancies, and surgical complications. Adv Anat Pathol. 2005;12(4):221–26. doi: 10.1097/01.pap.0000175113.55541.9c. [DOI] [PubMed] [Google Scholar]
- 7.Levesque E, Hoti E, Azoulay D, et al. Pulmonary complications after elective liver transplantation-incidence, risk factors, and outcome. Transplantation. 2012;94(5):532–38. doi: 10.1097/TP.0b013e31825c1d41. [DOI] [PubMed] [Google Scholar]
- 8.Patkowski W, Zieniewicz K, Skalski M, Krawczyk M. Correlation between selected prognostic factors and postoperative course in liver transplant recipients. Transplant Proc. 2009;41(8):3091–102. doi: 10.1016/j.transproceed.2009.09.038. [DOI] [PubMed] [Google Scholar]
- 9.Baganate F, Beal EW, Tumin D, et al. Early mortality after liver transplantation: Defining the course and the cause. Surgery. 2018;164(4):694–704. doi: 10.1016/j.surg.2018.04.039. [DOI] [PubMed] [Google Scholar]
- 10.Sun HY, Cacciarelli TV, Singh N. Identifying a targeted population at high risk for infections after liver transplantation in the MELD era. Clin Transplant. 2011;25(3):420–25. doi: 10.1111/j.1399-0012.2010.01262.x. [DOI] [PubMed] [Google Scholar]
- 11.Romero FA, Razonable RR. Infections in liver transplant recipients. World J Hepatol. 2011;3(4):83–92. doi: 10.4254/wjh.v3.i4.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HK, Park YK, Wang HJ, et al. Epidemiology and clinical features of post-transplant bloodstream infection: An analysis of 222 consecutive liver transplant recipients. Infect Chemother. 2013;45(3):315–24. doi: 10.3947/ic.2013.45.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freire MP, Soares Oshiro IC, Bonazzi PR, et al. Surgical site infections in liver transplant recipients in the model for end-stage liver disease era: An analysis of the epidemiology, risk factors, and outcomes. Liver Transpl. 2013;19(9):1011–19. doi: 10.1002/lt.23682. [DOI] [PubMed] [Google Scholar]
- 14.Yang LS, Shan LL, Saxena A, Morris DL. Liver transplantation: A systematic review of long-term quality of life. Liver Int. 2014;34(9):1298–313. doi: 10.1111/liv.12553. [DOI] [PubMed] [Google Scholar]
- 15.Chang AL, Cortez AR, Bondoc A, et al. Metabolic syndrome in liver transplantation: A preoperative and postoperative concern. Surgery. 2016;160(4):1111–17. doi: 10.1016/j.surg.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 16.De Vries FEE, Wallert ED, Solomkin JS, et al. A systematic review and meta-analysis including GRADE qualification of the risk of surgical site infections after prophylactic negative pressure wound therapy compared with conventional dressings in clean and contaminated surgery. Medicine (Baltimore) 2016;95(36):e4673. doi: 10.1097/MD.0000000000004673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Todd B. New CDC guideline for the prevention of surgical site infection. Am J Nurs. 2017;117(8):17. doi: 10.1097/01.NAJ.0000521963.77728.c0. [DOI] [PubMed] [Google Scholar]
- 18.Baddley JW, Forrest GN AST Infectious Diseases Community of Practice. Cryptococcosis in solid organ transplantation – Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13543. doi: 10.1111/ctr.13543. [DOI] [PubMed] [Google Scholar]
- 19.Camargo JF. Donor-derived infections in solid organ transplant recipients: Challenging the 30-day paradigm. Transpl Infect Dis. 2017;19(2):12665. doi: 10.1111/tid.12665. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, An B, Zhou G, et al. Study on the relieving effect of evidence-based nursing model on pain nursing of patients after liver transplantation. Minerva Med. 2021;112(5):676–77. doi: 10.23736/S0026-4806.20.06581-7. [DOI] [PubMed] [Google Scholar]
- 21.Fliedner MC. Research within the field of blood and marrow transplantation nursing: How can it contribute to higher quality of care? Int J Hematol. 2002;76(Suppl 2):289–91. doi: 10.1007/BF03165135. [DOI] [PubMed] [Google Scholar]
- 22.Lin EY, Cornman-Homonoff J, Odisio BC, Madoff DC. Applications of transcatheter embolotherapy in preparation for liver transplantation and resection. Chin Clin Oncol. 2019;8(6):59. doi: 10.21037/cco.2019.12.03. [DOI] [PubMed] [Google Scholar]
- 23.Saab S, Han SH, Martin P. Liver transplantation. Selection, listing criteria, and preoperative management. Clin Liver Dis. 2000;4(3):513–32. doi: 10.1016/s1089-3261(05)70124-0. [DOI] [PubMed] [Google Scholar]
- 24.Renner C, Jeitziner MM, Albert M, et al. Guideline on multimodal rehabilitation for patients with post-intensive care syndrome. Crit Care. 2023;27(1):301. doi: 10.1186/s13054-023-04569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McMillan Boyles C, Spoel P, et al. Representations of clinical practice guidelines and health equity in healthcare literature: An integrative review. J Nurs Scholarsh. 2023;55(2):506–20. doi: 10.1111/jnu.12847. [DOI] [PubMed] [Google Scholar]
- 26.Stevens KR. The impact of evidence-based practice in nursing and the next big ideas. Online J Issues Nurs. 2013;18(2):4. [PubMed] [Google Scholar]
- 27.Perl TM, Roy MC. Postoperative wound infections: Risk factors and role of Staphylococcus aureus nasal carriage. J Chemother. 1995;7(Suppl 3):29–35. [PubMed] [Google Scholar]
- 28.Hellinger WC, Crook JE, Heckman MG, et al. Surgical site infection after liver transplantation: Risk factors and association with graft loss or death. Transplantation. 2009;87(9):1387–93. doi: 10.1097/TP.0b013e3181a25133. [DOI] [PubMed] [Google Scholar]
- 29.Righi E. Management of bacterial and fungal infections in end stage liver disease and liver transplantation: Current options and future directions. World J Gastroenterol. 2018;24(38):4311–29. doi: 10.3748/wjg.v24.i38.4311. [DOI] [PMC free article] [PubMed] [Google Scholar]