Abstract
Dermal allyl isothiocyanate (AITC) administration and whole-body heat stress (WBHS) are two challenge models that are used to evaluate physiological mechanisms of vasodilation and pharmacological activity in humans. Their exact vasodilatory mechanisms in humans are not fully elucidated but are likely to be nitric oxide (NO)-mediated. This study aimed to evaluate whether there is overlap in the vasodilatory pathways of dermal AITC application and WBHS by combining the challenges. In this open-label interventional study, healthy volunteers underwent dermal administration of AITC twice: under basal conditions and during WBHS. Dermal blood flow (DBF) was non-invasively measured using laser speckle contrast imaging four times, once in each of the following situations: baseline, WBHS only, AITC only, and WBHS combined with AITC. A total of 12 male volunteers, aged 18–61 years, participated in the study. Compared to baseline, following AITC application, their DBF increased by 63.43 AU (baseline: 32.55, 95% CI [17.78, 47.31] AU, AITC only: 95.97, 95% CI [81.21, 110.7] AU, p < 0.0001). During WBHS, the increase in DBF after AITC was 42.76 AU (WBHS only: 87.25, 95% CI [72.49, 102.0] AU, WBHS+AITC: 130.0, 95% CI [115.2, 144.8] AU, p < 0.0001). The combination of WBHS and AITC resulted in a lower DBF than the sum of the DBF responses to AITC and WBHS when applied separately (ED 20.67, 95% CI [−3.532, 44.88], p = 0.0916). This might point towards the presence of an interaction in the vasodilatory mechanism of AITC application and WBHS, possibly indicating overlap in their NOS-driven vasodilatory pathways.
Keywords: clinical study, vasodilatory pathways, laser speckle contrast imaging, pharmacological challenge models
Introduction
A large variety of pharmacodynamic models and human challenges are used in clinical research to unravel (patho)physiological mechanisms, mimic pathological conditions, and evaluate the pharmacological effects of newly developed medications.1–6 Two such challenges are the allyl isothiocyanate (AITC) skin challenge and whole-body heat stress (WBHS). WBHS is a technique commonly used to study mechanisms of vasodilation.7–10 It consists of passively increasing core body temperature to 38–39°C by exposing healthy volunteers to heat either with warm water suits or in a bath, which induces a dermal vasodilatory response.8,10 The recently developed AITC skin challenge is based on dermal administration of AITC, which leads to vasodilation by agonism of the transient receptor potential cation channel A1 (TRPA1).11,12 This challenge has proven to be suitable for use in early-phase clinical trials investigating TRPA1-antagonists.13 Both challenges induce dermal vasodilation, which has been demonstrated to be objectively quantifiable as (changes in) dermal blood flow (DBF) by several imaging techniques, including laser speckle contrast imaging (LSCI).14,15 The physiological pathways leading to vasodilation in these challenges are not yet fully explored.
Nitric oxide (NO) is involved in many physiological processes, such as acting as a vasodilator. Its production is catalysed by three isoforms of nitric oxide synthase (NOS): neuronal, inducible, and endothelial NOS (nNOS, iNOS, eNOS). The primary function of nNOS is the involvement in NO-related vasodilation via nitrergic nerves, synaptic signalling, and central regulation of blood pressure. iNOS plays a signalling role in immune-mediated vasodilation and shaping the immune response, while eNOS induces endothelium-dependent vasodilation.16–18 Despite the lack of knowledge about the exact vasodilatory mechanisms of the AITC challenge and WBHS, it is known that their responses are at least partly mediated by TRPA1-agonistic activity influencing the NO system.9,19,20 Hypothetically, there might be overlap in their vasodilatory mechanisms. However, data substantiating this hypothesis is lacking.
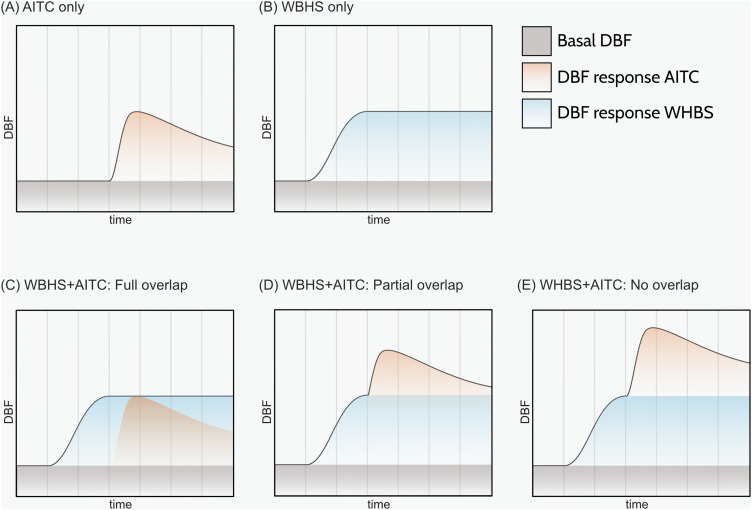
This study evaluated the vasodilatory response following a combined WBHS and AITC challenge, compared to the response to each of the challenges alone. The AITC skin challenge and WBHS were combined in the same study participants, allowing the identification of a potential overlap in their vasodilatory pathways. Theoretical outcomes comprised (1) a full overlap, resulting in no increase in skin perfusion upon an AITC challenge in a WBHS background, (2) a partial overlap, resulting in a partially additive effect of AITC, or (3) no overlap, resulting in a full additive effect of an AITC challenge in a WHBS background (Figure 1).
Figure 1.
Theoretical DBF responses to AITC, WBHS, and the combination of AITC and WBHS over time. (A) DBF after dermal administration of AITC. (B) DBF during WBHS. (C–E) DBF under the combination of AITC and WBHS. Hypotheses comprise full overlap (C), partial overlap (D), and no overlap (E) in vasodilatory mechanisms. Synergism of the DBF response by WBHS+AITC is theoretically possible, but mechanistically unlikely and therefore not included.
AITC, allyl isothiocyanate; DBF, dermal blood flow; WBHS, whole-body heat stress.
Materials and Methods
This study was conducted in accordance with the principles of the Declaration of Helsinki and the Dutch Act on Medical Research involving Human Subjects (WMO) from the 23rd of November 2021 to the 12th of January 2022 at the Center for Human Drug Research, Leiden, The Netherlands. The study, submitted at ToetsingOnline (NL79322.056.21) and prospectively registered on the 16th of November 2021 in the WHO-recognized Overview of Medical Research in The Netherlands (NL-OMON50731) registry, was approved by an independent Medical Ethics Committee (Medisch Ethische Toetsingscommissie van de Stichting Beoordeling Ethiek Biomedisch Onderzoek, Assen, The Netherlands).
Study Design and Subjects
This was an open-label interventional study. Before any study-related procedure, all subjects provided written informed consent. Healthy, non-smoking volunteers aged 18–65 years, without prior history of acute or chronic medical conditions and treatments, were eligible for participation after successfully completing a medical screening consisting of full medical history, physical examination, and laboratory testing. Only male subjects were eligible to minimize variability in DBF measurements due to known inter-sex differences in AITC responses.11,21 Subjects with a history of skin disorders, food allergies, specifically to mustard, and post-inflammatory hyperpigmentation, and subjects unable to undergo WBHS were excluded. Subjects refrained from the use of medications or illicit drugs and from vitamin, mineral, herbal, or dietary supplements from 14 days and 7 days prior to AITC administration until the end of the study, respectively. Subjects refrained from alcohol and caffeine-containing dietary products from 24 hours prior to AITC administration until the end of the study.
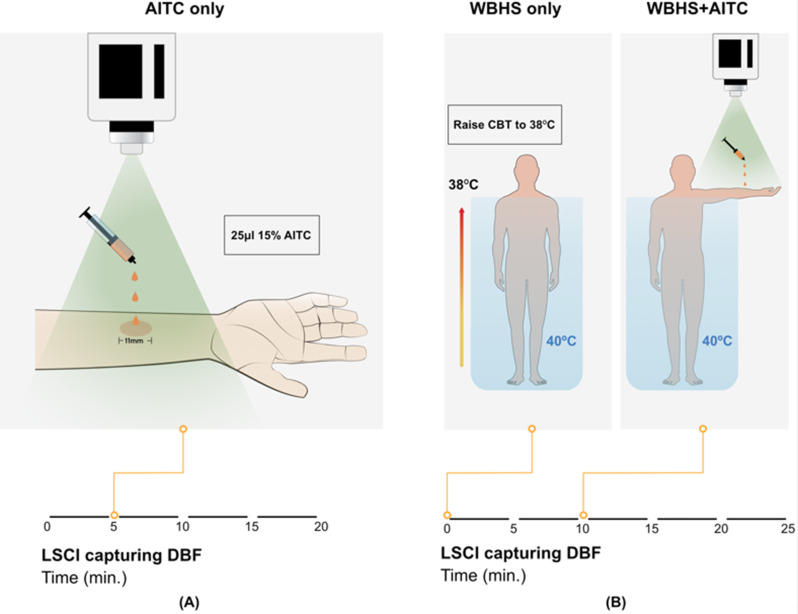
For the AITC skin challenge, GMP-grade AITC (Ofichem B.V., Ter Apel, The Netherlands), which was dissolved in mineral oil and dispensed by the Leiden University Medical Center pharmacy (Leiden, The Netherlands), was used. On two occasions, 25 µL of 15% AITC was topically applied to the skin within an 11mm O-ring: under basal conditions to one volar forearm (AITC only), and subsequently during WBHS to the contralateral volar forearm (WBHS+AITC) (Figure 2). The selected volume and concentration of AITC have previously been demonstrated to induce a robust DBF increase while having a tolerable safety profile.11
Figure 2.
Schematic representation of the study design. (A) Measurement of DBF using LSCI for a duration of 5 minutes at baseline and 15 minutes after AITC application. (B) Measurement of DBF using LSCI for a duration of 10 minutes during WBHS and 15 minutes after combination with the AITC application. In both (A) and (B), 25 µL of 15% AITC was administered within an 11mm O-ring to the volar forearm.
AITC, allyl isothiocyanate; CBT, core body temperature; DBF, dermal blood flow; min., minutes; WBHS, whole-body heat stress.
During WBHS, subjects were submerged up to their shoulders in a 40°C warm water bath (NetSpa, Rousset, France) until their core temperature reached 38°C (WBHS only and WBHS+AITC) (Figure 2). Core body temperature was measured during WBHS with an ingested capsulated thermometer (BodyCap, Hérouville Saint-Clair, France).
Vascular Endpoints
DBF, expressed in arbitrary units (AU), was measured continuously for 5 minutes before and 15 minutes after the first AITC application and for 10 minutes before and 15 minutes after the second AITC application in temperature-controlled rooms between 20 and 24°C using LSCI (PeriCam PSI NR System, Perimed AB, Järfälla, Sweden) (Figure 2). LSCI recordings of the target area on the ventral forearms were captured with the use of dedicated software (PIMSoft, Perimed AB, Järfälla, Sweden).22 The maximum DBF, measured as mean blood flow in a 30-second timeframe around the peak of perfusion, was used as the primary endpoint for the vasodilatory effects.
Statistics
All safety and statistical calculations were conducted with SAS version 9.4 for Windows or newer (SAS Institute Inc., Cary, North Carolina, United States of America). Baseline characteristics were summarized by descriptive statistics (n, mean, SD) in the case of continuous demographic variables. Qualitative demographic characteristics (eg, sex, race) were summarized by counts and percentages. DBF was evaluated at baseline, and vascular responses were evaluated after AITC only, WBHS only and WBHS+AITC within the O-ring. To further substantiate the data, a pre-specified secondary analysis was performed on skin responses that extended outside the borders of the O-ring. For this secondary response, standardized skin areas were selected based on the largest AITC-induced response in DBF among all participants. DBF is summarized per condition and graphically represented in Tukey boxplots as mean and median with minimum and maximum. DBF was analyzed with a mixed effects model with fixed factor treatment and random factor subject, and results were presented as estimated differences and estimated means, both with 95% confidence interval (95% CI). Contrasts within the model were calculated between baseline and AITC only, baseline and WBHS only, and baseline and WBHS+AITC. To estimate the difference between the combined WHBS+AITC effect and the addition of the separate WHBS only and AITC only effects, the contrast between (WHBS+AITC - baseline) and ((WHBS only - baseline)+(AITC only - baseline)) was calculated within the model.
Results
Baseline Demographics
Twelve healthy subjects, aged between 18 and 61 years, participated in the study. All included subjects were male, white, and had normal vital signs and hemoglobin levels. Baseline demographics are provided in Table 1.
Table 1.
Baseline Characteristics
| Baseline characteristics | (n=12) |
|---|---|
| Age (years) | 33.6 (16.2) |
| Sex, n (%) Male |
12 (100%) |
| Race, n (%) White |
12 (100%) |
| Ethnicity, n (%) Not Hispanic or Latino |
12 (100%) |
| Heart rate (beats per minute) | 60 (10) |
| Temperature (°C) | 36.7 (0.3) |
| Systolic blood pressure (mmHg) | 120 (11) |
| Diastolic blood pressure (mmHg) | 74 (9) |
| Respiratory rate (breaths per minute) | 14 (2) |
| BMI (kg/m2) | 24.1 (3.3) |
| Hemoglobin (mmol/L) | 9.4 (0.5) |
Abbreviations: BMI, body mass index; mmHg, millimeters of mercury.
AITC Induces a Robust Vasodilatory Response
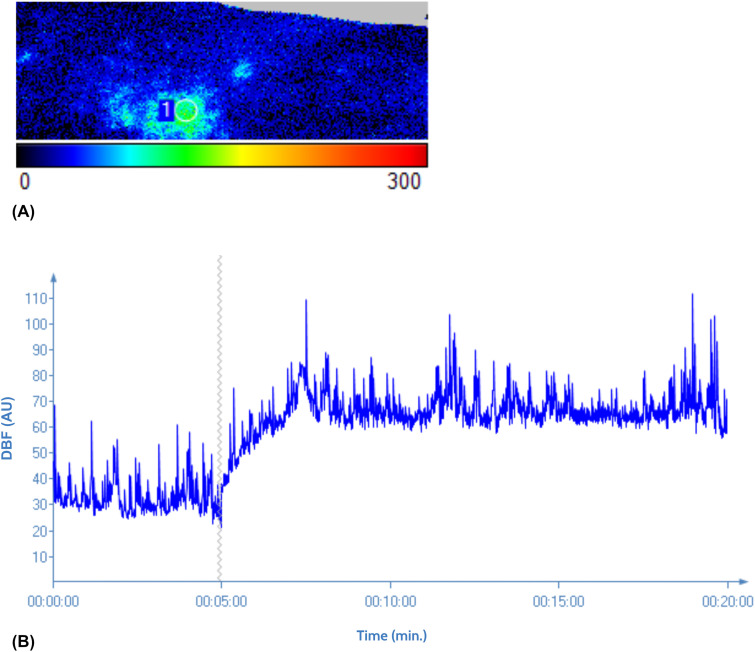
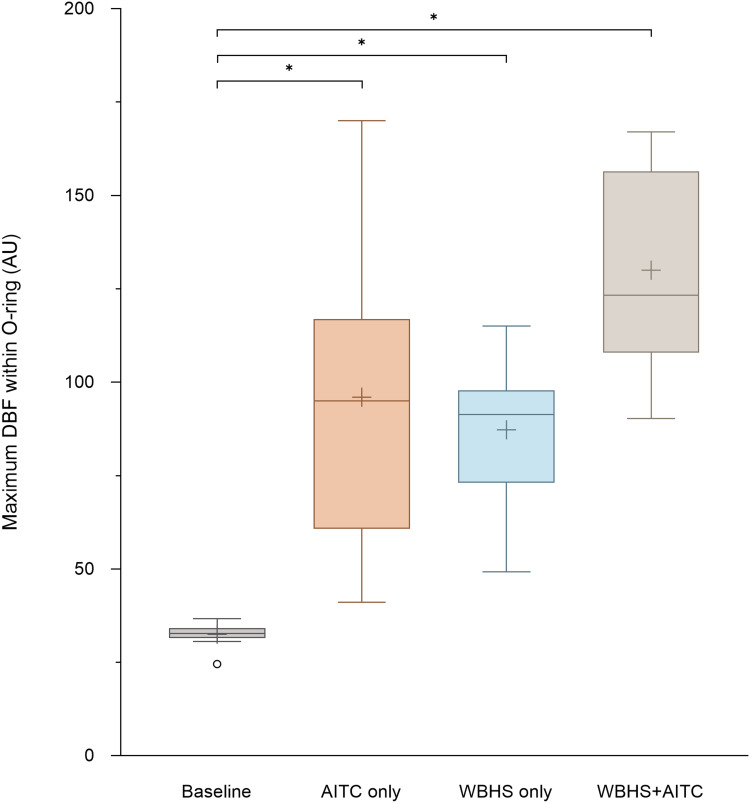
The AITC skin challenge was performed under basal conditions to characterize the AITC-mediated vasodilatory response. This dermal application of AITC induced an increase in DBF lasting for at least 15 minutes (end of measurement), with the 30-second peak occurring approximately 1-4 minutes after application. A typical curve is depicted in Figure 3. DBF within the O-ring increased significantly from 32.55 (95% CI [17.78, 47.31]) AU at baseline to a maximum of 95.97 (95% CI [81.21, 110.7]) AU, p < 0.0001 (Figure 4, Table 2).
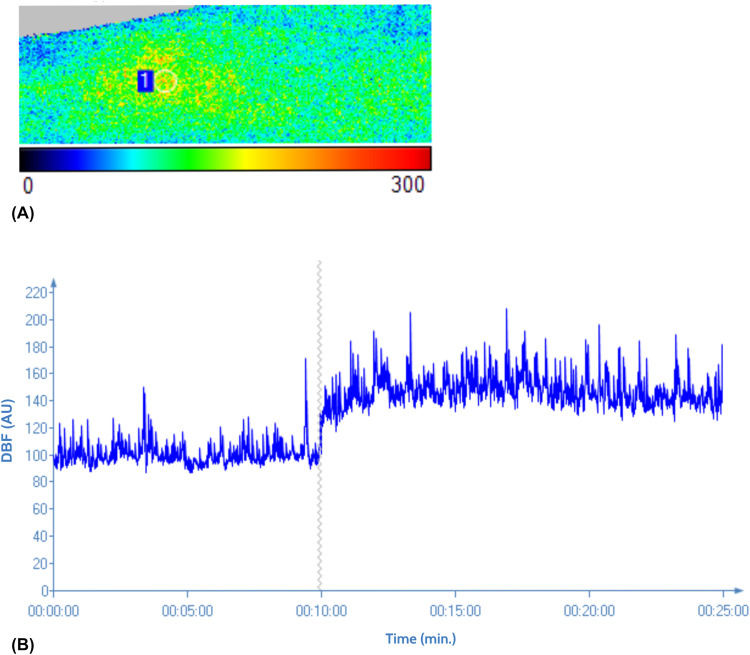
Figure 3.
Exemplary response of an individual to AITC. (A) Visual representation of DBF within the O-ring in AU after AITC administration; 1 = O-ring. (B) DBF expressed in AU at baseline and in response to AITC administration at 5 minutes, as measured by LSCI.
AITC, allyl isothiocyanate; AU, arbitrary units; DBF, dermal blood flow; LSCI, laser speckle contrast imaging; min., minutes.
Figure 4.
Tukey boxplot representing DBF within the O-ring under the studied conditions. DBF was measured using LSCI, and statistical analysis of AITC, WBHS, and WBHS+AITC compared to baseline report p-values <0.0001, as indicated with an *.
AITC, allyl isothiocyanate; AU, arbitrary units; DBF, dermal blood flow; LSCI, laser speckle contrast imaging; WBHS, whole-body heat stress.
Table 2.
DBF Responses Within the O-Ring Under the Studied Conditions
| Intervention | LSM maximum flow in AU (95% CI) | ED in AU vs Baseline (95% CI) | P-value (vs Baseline) |
|---|---|---|---|
| Baseline | 32.55 (17.78, 47.31) | - | - |
| AITC only | 95.97 (81.21, 110.7) | 63.43 (46.31, 80.54) | <0.0001 |
| WBHS only | 87.25 (72.49, 102.0) | 54.71 (37.59, 71.82) | <0.0001 |
| WBHS+AITC | 130.0 (115.2, 144.8) | 97.47 (80.35, 114.6) | <0.0001 |
Notes: DBF was measured using LSCI at baseline, after AITC administration (AITC only), during WBHS (WBHS only), and after AITC administration during WBHS (WBHS+AITC).
Abbreviations: AITC, allyl isothiocyanate; AU, arbitrary units; ED, estimated difference; LSCI, laser speckle contrast imaging; LSM, least squares means; WBHS, whole-body heat stress; 95% CI, 95% confidence interval.
Dermal Blood Flow is Augmented to a Lesser Extent by AITC Application During WBHS as Compared to AITC Application Without WBHS
The AITC skin challenge was combined with WBHS to evaluate their combined vasodilatory response. The observed peak in DBF occurred 0.5-3 minutes after the AITC application. Figure 5 illustrates a typical curve of the augmented basal flow due to WBHS and the vasodilatory response after AITC administration. The maximal DBF increased significantly from 32.55 at baseline to 87.25 (95% CI [72.49, 102.0]) AU during WBHS only (ED 54.71, 95% CI [37.59, 71.82] AU, p < 0.0001), and subsequently to a maximum of 130.0 (95% CI [115.2, 144.8]) AU after AITC challenge (ED 97.47, 95% CI [80.35, 114.6] AU, p < 0.0001) (Figure 4, Table 2). The combination of WBHS and AITC resulted in a lower DBF than theoretically possible based on the sum of the DBF responses to AITC and WBHS when applied separately (ED 20.67, 95% CI [−3.532, 44.88] AU, p = 0.0916) (Figure 4). Comparable effects were observed in the secondary analysis (Table 3).
Figure 5.
Exemplary response of an individual to AITC during WBHS. (A) Visual representation of DBF within the O-ring in AU after AITC administration during WBHS; 1 = O-ring. (B) DBF expressed in AU during WBHS and in response to AITC administration at 10 minutes, as measured by LSCI.
AITC, allyl isothiocyanate; AU, arbitrary units; DBF, dermal blood flow; LSCI, laser speckle contrast imaging; min., minutes; WBHS, whole-body heat stress.
Table 3.
DBF Under the Studied Conditions, in the Area Corresponding to the Largest AITC-Induced Vasodilatory Response Among All Subjects
| Intervention | LSM maximum flow in AU (95% CI) | ED in AU vs Baseline (95% CI) | P-value (vs Baseline) |
|---|---|---|---|
| Baseline | 28.94 (20.67–37.21) | - | - |
| AITC only | 47.08 (38.81–55.35) | 18.14 (8.90–27.37) | 0.0003 |
| WBHS only | 81.19 (72.92–89.46) | 52.25 (43.02–61.49) | <0.0001 |
| WBHS+AITC | 104.9 (96.62–113.2) | 75.94 (66.71–85.18) | <0.0001 |
Notes: DBF was measured using LSCI at baseline, after AITC administration (AITC only), during WBHS (WBHS only), and after AITC administration during WBHS (WBHS+AITC).
Abbreviations: AITC, allyl isothiocyanate; AU, arbitrary units; ED, estimated difference; LSCI, laser speckle contrast imaging; LSM, least squares means; WBHS, whole-body heat stress; 95% CI, 95% confidence interval.
Discussion
This clinical study demonstrates a robust increase in DBF, indicating vasodilation, after the topical dermal application of 15% AITC. The observations were in line with two recent papers by Joseph et al and Chan et al.11,13 Furthermore, a clear increase in skin perfusion upon WBHS was observed, with vasodilatory increases similar to those previously reported by Gemae et al and Luetkemeier et al.10,23 Our study is the first to combine AITC application and WBHS to evaluate additive effects of, and overlap in, the vasodilatory pathways of both challenges in humans. It was shown that the combination of WBHS and AITC leads to an enhanced DBF compared to each of the challenges alone, but to a lower DBF than the sum of both challenge responses, indicating a partial overlap in the underlying vasodilatory mechanisms (Figure 1D).
The observed partially additive effects of AITC on WBHS responses may indicate a partial overlap in underlying vasodilatory mechanisms between WBHS and AITC. Both challenges are known for mediating vasodilation through the NO pathway, which might explain the observations in this study. A ceiling effect in the physiological vasodilatory capacity of the dermal circulation cannot be fully excluded, for example, related to technical limitations in the detection of extreme vasodilation by LSCI. However, previous research in other pharmacological challenge models using the same recording method and analysis settings demonstrated higher DBF values (up to 110 AU higher) than in our study, suggesting that the combined effects of AITC and WBHS did not reach maximal vasodilatory capacity (data on file). Other theoretical explanations for the partial additive effect of AITC on WBHS responses are of a pharmacokinetic nature: a higher DBF during WBHS could drive more efficient local AITC absorption or clearance, thereby respectively enhancing or limiting TRPA1 stimulation and AITC-driven DBF. However, since there is no apparent faster increase after AITC application and no apparent faster resolution of the AITC-induced vasodilatory response in a WBHS background, a more efficient local AITC absorption or clearance due to heating does not seem to play a role.
Currently, limited knowledge is available about the exact contribution of specific mechanisms of vasodilation and NOS isoforms involved in both challenges in men. However, for TRPA1 agonism, NOS, specifically nNOS, has been identified as a relevant driver of downstream vasodilatory effects. For example, vasodilation induced by cinnamaldehyde (CA), another TRPA1-agonist, has been studied in mice and men. Significant reductions in DBF response to CA were observed in mice administered nitro-L-arginine methyl ester (L-NAME), a non-specific NOS inhibitor, prior to dermal application of CA. To investigate NOS isoform involvement, nNOS was selectively inhibited using S-methyl-L-thiocitrulline (SMTC), which significantly reduced CA-induced DBF. This highlights the role of nNOS in TRPA1-mediated vasodilation.24 In healthy volunteers, administration of L-NAME prior to CA infusion through dermal microdialysis significantly reduced CA-induced vasodilation.25 Furthermore, the vasodilatory mechanisms of WBHS have been studied in humans, also showing NOS involvement. Administration of L-NAME significantly lowered WBHS-driven skin perfusion.9,20 Intradermal administration of two specific nNOS-inhibitors, 7-nitroindazol (7-NI) and Nω-propyl-l-arginine (NPLA), during WBHS significantly attenuated the dermal vasodilatory response to WBHS in healthy volunteers, underlining the involvement of nNOS in the WBHS response.7,26 Based on this, we hypothesize that nNOS involvement in both challenge models specifically explains the overlap in vasodilatory response observed in our study.
The influence of other downstream activated vasodilatory mediators, such as hydrogen sulfide (H2S) through TRPA1 agonism, on the development of the vasodilatory response after TRPA1 activation by AITC cannot be ruled out.24,25,27 However, based on the presented (pre-)clinical research on TRPA1 antagonists and mechanistic reasoning, it is most likely that the direct agonistic effect of AITC on TRPA1 initiates the vasodilatory response measured in this study through NO signaling and that other vasodilatory mediators arise secondary to the AITC stimulus.9,20,24–26
Although our study does not include a WBHS-only group, specific NOS-related biomarkers, or an intervention blocking specific NOS pathways, it does provide insight into mechanistic overlap between the AITC and WBHS response, potentially aiding further characterization and application of these challenge models for the pharmacodynamic evaluation of future vascular drugs. To provide further insight into the vasodilatory mechanisms of both challenges and examine the involvement of nNOS, it would be interesting to conduct future studies that included vasodilation induced by AITC skin challenge and WBHS combined with the addition of a specific nNOS blocker, such as 7-NI. However, there are currently no facilities that produce GMP-grade 7-NI for the purpose of exploratory clinical studies.
Conclusion
In conclusion, this is the first study combining AITC and WBHS, demonstrating an enhanced skin response for the combined challenges compared to the individual challenge responses and suggesting a potential mechanistic overlap in the underlying NO-mediated vasodilatory mechanisms. Both challenges, combined or separately, are considered useful to evaluate the pharmacodynamic effects of NO-targeted drugs. An extended evaluation of the exact vasodilatory mechanisms involved in both challenges may further increase their value.
Acknowledgments
The authors thank all of CHDR’s operational staff and volunteers for their efforts that enabled us to conduct this study.
Funding Statement
This work received no external funding.
Abbreviations
7-nitroindazol (7-NI), 95% confidence interval (95% CI), allyl isothiocyanate (AITC), arbitrary units (AU), cinnamaldehyde (CA), dermal blood flow (DBF), estimated difference (ED), endothelial nitric oxide synthetase (eNOS), inducible nitric oxide synthetase (iNOS), nitro-L-arginine methyl ester (L-NAME), laser speckle contrast imaging (LSCI), least squares means (LSM), neuronal nitric oxide synthetase (nNOS), nitric oxide synthetase (NOS), Nω-propyl-l-arginine (NPLA), S-methyl-L-thiocitrulline (SMTC), transient receptor potential cation channel A1 (TRPA1), whole-body heat stress (WBHS), Dutch Act on Medical Research involving Human Subjects (WMO).
Data Sharing Statement
The authors declare that the data supporting the findings of this study are available within the paper. Reasonable requests to access the data on file referenced in the discussion can be made to the corresponding author. Individual participant data and study-specific documents are not intended to be shared.
Ethical Statement
This study was performed in line with the principles of the Declaration of Helsinki. The studies were approved by the Medical Ethics Committee “Stichting Beoordeling Ethiek Biomedisch Onderzoek” (Assen, the Netherlands). Written informed consent was obtained from all subjects prior to any study-related procedures.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.van der Kolk T, Assil S, Rijneveld R, et al. Comprehensive, multimodal characterization of an imiquimod-induced human skin inflammation model for drug development. Clin Transl Sci. 2018;11(6):607–615. doi: 10.1111/cts.12563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buters TP, Hameeteman PW, Jansen IME, et al. Intradermal lipopolysaccharide challenge as an acute in vivo inflammatory model in healthy volunteers. Br J Clin Pharmacol. 2022;88(2):680–690. doi: 10.1111/bcp.14999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Dongen MGJ, Geerts BF, Bhanot S, et al. Characterization of a standardized glucagon challenge test as a pharmacodynamic tool in pharmacological research. Hormone Metab Res. 2014;46(4):269–273. doi: 10.1055/s-0033-1363223 [DOI] [PubMed] [Google Scholar]
- 4.Vanmolkot FHM, Van Der Schueren BJEP, De Hoon JNJM. Calcitonin gene-related peptide-induced vasodilation in the human forearm is antagonized by CGRP8-37: evaluation of a human in vivo pharmacodynamic model. Clin Pharmacol Ther. 2006;79(3):263–273. doi: 10.1016/j.clpt.2005.11.005 [DOI] [PubMed] [Google Scholar]
- 5.Stephens DP, Charkoudian N, Benevento JM, Johnson JM, Louis Saumet J, Johnson JM. The influence of topical capsaicin on the local thermal control of skin blood flow in humans. Am J Physiol Regul Integr Comp Physiol. 2001;281:894–901. doi: 10.1152/ajpregu.2001.281.3.R894 [DOI] [PubMed] [Google Scholar]
- 6.Roestenberg M, Hoogerwerf MA, Ferreira DM, Mordmüller B, Yazdanbakhsh M. Experimental infection of human volunteers. Lancet Infect Dis. 2018;18(10):e312–e322. doi: 10.1016/S1473-3099(18)30177-4 [DOI] [PubMed] [Google Scholar]
- 7.Kellogg DL, Zhao JL, Wu Y. Neuronal nitric oxide synthase control mechanisms in the cutaneous vasculature of humans in vivo. J Physiol. 2008;586(3):847–857. doi: 10.1113/jphysiol.2007.144642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kellogg DL Jr, Zhao JL, Wu Y, et al. Antagonism of soluble guanylyl cyclase attenuates cutaneous vasodilation during whole body heat stress and local warming in humans. J Appl Physiol. 2011;110:1406–1413. doi: 10.1152/japplphysiol.00702.2010.-We [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong BJ. Sensory nerves and nitric oxide contribute to reflex cutaneous vasodilation in humans. Am J Physiol Regul Integr Comp Physiol. 2013;304:651–656. doi: 10.1152/ajpregu.00464.2012 [DOI] [PubMed] [Google Scholar]
- 10.Gemae MR, Akerman AP, McGarr GW, et al. Myths and methodologies: reliability of forearm cutaneous vasodilatation measured using laser-Doppler flowmetry during whole-body passive heating. Exp Physiol. 2021;106(3):634–652. doi: 10.1113/EP089073 [DOI] [PubMed] [Google Scholar]
- 11.Joseph V, Yang X, Gao SS, et al. Development of AITC-induced dermal blood flow as a translational in vivo biomarker of TRPA1 activity in human and rodent skin. Br J Clin Pharmacol. 2021;87(1):129–139. doi: 10.1111/bcp.14370 [DOI] [PubMed] [Google Scholar]
- 12.Lippe IT, Stabentheiner A, Holzer P. Participation of nitric oxide in the mustard oil-induced neurogenic inflammation of the rat paw skin. Eur J Pharmacol. 1993;232:113. doi: 10.1016/0014-2999(93)90735-z [DOI] [PubMed] [Google Scholar]
- 13.Chan P, Ding HT, Liederer BM, et al. Translational and pharmacokinetic-pharmacodynamic application for the clinical development of GDC-0334, a novel TRPA1 inhibitor. Clin Transl Sci. 2021;14(5):1945–1954. doi: 10.1111/cts.13049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guven G, Dijkstra A, Kuijper TM, et al. Comparison of laser speckle contrast imaging with laser Doppler perfusion imaging for tissue perfusion measurement. Microcirculation. 2023;30(1). doi: 10.1111/micc.12795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaseling GK, Crandall CG, Gagnon D. Skin blood flow measurements during heat stress: technical and analytical considerations. Am J Physiol Regul Integr Comp Physiol. 2019;318. doi: 10.1152/ajpregu.00177.2019.-During [DOI] [PubMed] [Google Scholar]
- 16.Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33(7):829–837. doi: 10.1093/eurheartj/ehr304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bogdan C. Nitric oxide and the immune response NO production in the immune system. Nat Immunol. 2001;2(10):907–916. doi: 10.1038/ni1001-907 [DOI] [PubMed] [Google Scholar]
- 18.Bruckdorfer R. The basics about nitric oxide. Mol Aspects Med. 2005;26(1–2):3–31. doi: 10.1016/j.mam.2004.09.002 [DOI] [PubMed] [Google Scholar]
- 19.Andrei SR, Ghosh M, Sinharoy P, Damron DS. Stimulation of TRPA1 attenuates ischemia-induced cardiomyocyte cell death through an eNOS-mediated mechanism. Channels. 2019;13(1):192–206. doi: 10.1080/19336950.2019.1623591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holowatz LA, Houghton BL, Wong BJ, et al. Nitric oxide and attenuated reflex cutaneous vasodilation in aged skin. Am J Physiol Heart Circ Physiol. 2003;284(5):53–55. doi: 10.1152/ajpheart.00871.2002 [DOI] [PubMed] [Google Scholar]
- 21.Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–58. doi: 10.1093/bja/aet127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heeman W, Steenbergen W, van Dam GM, Boerma EC. Clinical applications of laser speckle contrast imaging: a review. J Biomed Opt. 2019;24(08):1. doi: 10.1117/1.jbo.24.8.080901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luetkemeier MJ, Allen DR, Huang M, et al. Skin tattooing impairs sweating during passive whole body heating. J Appl Physiol. 2020;129:1033–1038. doi: 10.1152/japplphysiol.00427.2019 [DOI] [PubMed] [Google Scholar]
- 24.Aubdool AA, Kodji X, Abdul-Kader N, et al. TRPA1 activation leads to neurogenic vasodilatation: involvement of reactive oxygen nitrogen species in addition to CGRP and NO. Br J Pharmacol. 2016;173:2419–2433. doi: 10.1111/bph.13519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGarr GW, King KE, Cassan CJM, Janetos KMT, Fujii N, Kenny GP. Involvement of nitric oxide synthase and reactive oxygen species in TRPA1-mediated cutaneous vasodilation in young and older adults. Microvasc Res. 2023;145:104443. doi: 10.1016/j.mvr.2022.104443 [DOI] [PubMed] [Google Scholar]
- 26.Kellogg DL, Zhao JL, Wu Y. Roles of nitric oxide synthase isoforms in cutaneous vasodilation induced by local warming of the skin and whole body heat stress in humans. J Appl Physiol. 2009;107(5):1438–1444. doi: 10.1152/japplphysiol.00690.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pozsgai G, Hajna Z, Bagoly T, et al. The role of transient receptor potential ankyrin 1 (TRPA1) receptor activation in hydrogen-sulphide-induced CGRP-release and vasodilation. Eur J Pharmacol. 2012;689(1–3):56–64. doi: 10.1016/j.ejphar.2012.05.053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors declare that the data supporting the findings of this study are available within the paper. Reasonable requests to access the data on file referenced in the discussion can be made to the corresponding author. Individual participant data and study-specific documents are not intended to be shared.