Abstract
Background
Little is known regarding the effectiveness of pain protocols and guideline use in Emergency Departments (ED) in Sub-Saharan Africa. Therefore, to shed light on this research gap, this study had the following objectives: 1) to evaluate if the implementation of the Essential Pain Management (EPM) course combined with mentorship to use the World Health Organization (WHO) pain ladder-based protocol improves the quality of pain management among trauma patients at the ED of two teaching hospitals in Rwanda; and 2) to determine barriers to implementing the WHO pain ladder-based protocol among trauma patients in the same settings.
Methods
This was a pre- and post-intervention study. The intervention was 1-day essential pain management training for ED clinical staff followed by 1 week mentorship on the use of the WHO pain ladder-based protocol.
Results
We enrolled 261 patients (47.5% pre versus 52.5% post intervention), most of them were aged between 21 and 40 (60% pre versus 33% post intervention), and male (76% pre versus 73% post intervention). The quality of pain management at the ED improved as shown by the decrease of the number of patients with undocumented pain scores from 58% to 24% after the intervention (p-value > 0.001) and the increase of the number of patients with mild pain from 37% to 62% (p-value > 0.001). In addition, patients who were satisfied with the quality of pain management increased significantly from 42% before the intervention to 80% (p-value > 0.001). Barriers to the implementation of the WHO pain ladder-based protocol were identified related to staff (i.e. inadequate experience), to the hospital (i.e. poor documentation), and to patients (i.e. reluctance to report pain).
Conclusion
The implementation of the EPM course along with mentorship to use the WHO pain ladder-based protocol significantly improved the quality of pain management for trauma patients in EDs of both referral hospitals. Despite this, some barriers remain unfixed such as inadequate staff experience, poor documentation, and patient's reluctance to report pain. Appropriate interventions should be implemented to address the identified barriers and ensure adequate pain management for patients admitted at EDs in public hospitals in Rwanda.
Keywords: Pain management, Trauma, Emergency department
African relevance.
• Pain management is known to be poor in many emergency settings as healthcare providers tend to focus on life and limb saving interventions, and this is probably even more of an issue in under-resourced settings across Africa.
•This project has potential to inform the implementation of similar projects by other researchers and practitioners involved in pain management of trauma patients at emergency departments across Africa.
•We hope to encourage other African scholars to publish their work and establish future research collaborations.
Alt-text: Unlabelled box
Background
Despite the known benefits of adequate pain control, most trauma patients admitted to the emergency department (ED) do not receive required adequate analgesia [1]. Multiple studies have explored the quality of pain management among ED trauma patients and found that between 14% and 54% receive treatment for their pain [[1], [2], [3], [4], [5], [6]]. Most trauma patients also reported low satisfaction with their pain management at in the ED [1]. On top of low satisfaction, poor pain management of trauma patients leads to multiple negative consequences such as clotting complications, stress related complications, increased hospital stay, and chronic pain [7].
Numerous factors have been shown to contribute to inadequate pain management including shortage of physicians and nurses, inadequate pain training, erratic supply of analgesic medications, and lack of patient education about the side effects of pain medications [2]. In addition, most EDs in Sub Saharan Africa (SSA) lack locally relevant pain protocols and guidelines leading to poor pain management [7,8]. The use of the World Health Organization (WHO) pain ladder-based protocol and training in acute pain management have shown positive results in improving pain management in different hospital settings [[9], [10], [11]] (shown in Table 1).
Table 1.
WHO Pain Ladder-based Trauma Pain Management (8).
| Pain Assessment | Methods | Results | Action |
|---|---|---|---|
| Mild | VAS | 1-3 | paracetamol, NSAIDs, cold/hot compresses |
| Moderate | VAS | 4-6 | cold/hot compresses, tramadol, pethidine |
| Severe | VAS | 7-10 | fentanyl, morphine, ketamine |
| Reassessment | Reassess every 5 minutes if severe pain, otherwise reassess every 3 hours. Evidence of adverse effects should preclude further drug administration |
||
VAS: Visual Analogue Scale, NSAIDS: Nonsteroidal anti-inflammatory drugs
However, there are limited data regarding acute trauma pain management in the ED in Sub-Saharan Africa (SSA) [2]. At the time of publication, to our knowledge, there was no previous study that evaluated the current practice for acute pain management among trauma patients at the ED in Rwandan hospitals. Therefore, this study had the following objectives: 1) to evaluate if the implementation of the Essential Pain Management (EPM) course combined with mentorship to use the WHO pain ladder-based protocol improves the quality of pain management among trauma patients at the ED of two teaching hospitals in Rwanda; and 2) to determine barriers to implementing the WHO pain ladder-based protocol among trauma patients in the same settings.
Methods
Study design
This was a pre- and post-implementation study conducted between October 2020 and March 2021. The reporting followed the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines [12].
Setting
This study was conducted at the University Teaching Hospital of Kigali (CHUK), and the University Teaching Hospital of Butare (CHUB), in Rwanda. CHUK and CHUB represent the major Rwandan public referral hospitals, CHUK and CHUB have 24 and 22 emergency beds, as well as 500 and 300 inpatient beds, respectively. Annually, the ED at CHUK receives approximately 20,000 patients while that of CHUB admits approximately 2000 injured patients each year [13,14].
Study participants
For objective 1, this study included all adult trauma patients aged 18 years and above admitted to the CHUK or CHUB ED within 24 hours. We excluded patients with a Glasgow Coma Scale (GCS) less than 15/15 at any stage of the study and those refusing to provide informed consent. For objective 2, all ED staff (nurses and doctors) were eligible to participate in the study. No staff refused to provide his/her informed consent to participate in this study.
Study conduct
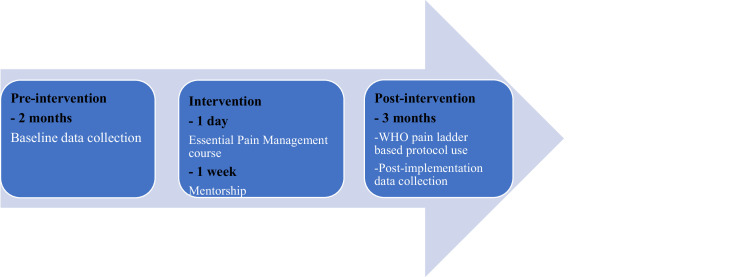
The study was conducted in three phases (Fig. 1):
Fig. 1.
WHO pain ladder-based protocol implementation timeline
Phase I: pre-intervention
The PI (JPH) trained four medical students as data collectors using one hour of demonstration of the data collection tools followed by a one-week period of mentored data collection. They collected baseline data on patients’ pain scores, use of pain assessment tools and use of pain management protocols and guidelines by ED healthcare workers, pain management documentation, and patient satisfaction with pain management. Data collection was completed over a two months period.
'The revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) was used to collect data on the quality of pain management before and after the intervention [15]. A small adaptation to the APS-POQ-R tool was made to meet the local context. For this paper, we only report the indicators identified by the implementation team as essential for adequate pain management in trauma patients in our context. These indicators include pain scores, types of pain management, patients’ satisfaction, and barriers to the implementation of the WHO pain ladder-based protocol (at staff, hospital, and patient level). The remaining data from the APS-POQ-R tool will be reported elsewhere.
Phase II: intervention
Over one week, the ED staff (nurses and doctors) of both CHUK and CHUB participated in an one day essential pain management (EPM) course (with a small modification by adding 5 scenarios for pain management in trauma and introducing the WHO pain ladder-based protocol) followed by one week mentorship (from 8:00 am until 5:00 pm during working days from Monday to Friday) on the use of the WHO pain ladder-based protocol adapted to Rwandan context and considering the evidence from the American College of Surgeons (ACS) guidelines on acute trauma pain management which are widely used both in the United States and globally [[16], [17], [18], [19]]. Printed WHO pain ladder-based protocols were included in patients’ file by the nurse during the admission process of each trauma patient during the mentorship and throughout the duration of the implementation. More than 80% of ED staff participated in the EPM course and one week mentorship except staff who were covering the ED department during the course and those ones who were in vacation during mentorship.
The WHO pain ladder protocol was chosen to be implemented based on the worldwide consensus of the value of this tool for the medical management of all pain associated with serious illness; it has the following main items: pain assessment using the Visual Analogue Scale (VAS), acute pain treatment modalities, and guidelines for reassessment (Table 1) [18].
During mentorship, the PI (JPM) with two medical students at each center reviewed the compliance of doctors and nurses with the WHO pain ladder-based protocol every two hours and provided feedback at the end of the shift or immediately if the patient was found to have severe pain during assessment. In the case of severe pain, the doctor, or the nurse responsible for the patient was encouraged to provide pain drugs as soon as possible according to the WHO pain ladder-based protocol.
As the mentorship was done during daytime excluding the weekend, it is possible that some mentorship opportunities were missed for patients who were admitted during that time. However, one week was enough time to interact with all staff at emergency department except one doctor and one nurse who were on vacation during the mentorship period.
Phase III: post intervention
After one week of intervention, the same four medical students (under supervision by the PI, JPH) collected data following same process as done during the pre-intervention phase. In addition, a second paper-based questionnaire was used to collect data from nurses and doctors on the barriers faced during the implementation of the WHO pain ladder-based protocol. A list of barriers related to staff, hospital, and patient was given with options to choose more than one barrier or add a new barrier which was not on the list.
Data collectors were the same medical students throughout the study period.
Sample size
Prior studies have shown that approximately 20% of patients in EDs received adequate pain treatment [[1], [2], [3], [4], [5], [6], [15]]. In order to detect a 20% increase in the percentage of patients with adequate pain treatment after the intervention, a sample of 162 patients (81 pre-intervention and 81 post-intervention) was required with 80% power, alpha error of 0.05, and effect size of 0.5. Given that CHUB has a lower ED patient capacity than CHUK with a ratio of almost 1:2, we planned to enroll at least 27 patients from CHUB and 54 patients from CHUK during each study period.
Data analysis
Data were entered electronically in Microsft Excel (Version 21) from paper forms by four data collectors. The PI (JPH) rechecked data entry of 10% of patients to ensure accuracy. Data were analyzed using SPSS (Version 21). Descriptive statistics were used to analyze participants’ demographic data and barriers to the use of the WHO-ladder pain protocol; number and percentages were reported as appropriate for categorical variables, no continuous variables were reported. The chi-square test was used to compare categorical variables of patients’ demographics and the quality of pain management between the two study periods with a statistical significance set at P-value < 0.05.
Ethical considerations
This study was approved by the Institutional Review Boards of the College of Medicine and Health Sciences, University of Rwanda (No 204/CMHS IRB/2019), the University Teaching Hospitals of Kigali (No. EC/CHUK/113/2019), and the University Teaching Hospitals Butare (No. CHUB/DG/SA/09.1407/2019). Informed consent was obtained from participants prior to recruitment in the study, each participant was assigned a unique study number to ensure the privacy, and data were kept in a password protected computer only accessible to the research team.
Results
Our study enrolled 261 patients (47.5% pre versus 52.5% post intervention), most of them were aged between 21 and 40 (60% pre versus 33% post intervention), male (76% pre versus 73% post intervention), and from CHUK (68.5% pre versus 66.4% post intervention). The number of patients with undocumented pain scores decreased from 58% to 24% after the intervention (p-value > 0.001) and most patients (62%) had mild pain post-intervention versus (37%) pre-intervention (p-value > 0.001). In addition, the use of morphine (41% versus 54%), paracetamol (69% versus 89%), and cold packs (5% versus 18%) increased after intervention while the use of NSAIDS was maintained (<0.001). Furthermore, patients who were very satisfied or satisfied with the quality of pain management increased significantly from 42% pre-intervention to 80% post-intervention (p-value > 0.001) (Table 2).
Table 2.
Patients’ demographics and quality of pain management at EDs of CHUK and CHUB.
| Variable | Pre-intervention N: 124 n (%) |
Post-intervention, N:137 n (%) |
P-Value |
|---|---|---|---|
|
Age (years) < 20 21- 40 41- 60 > 60 |
6 (5) 75 (60) 36 (29) 7 (6) |
32 (23.3) 45 (33) 32 (23.3) 28 (20.4) |
< 0.001 |
|
Sex male female |
94 (76) 30 (24) |
100 (73) 37 (27) |
> 0.05 |
|
Hospital CHUB CHUK |
39 (31.5) 85 (68.5) |
46 (33.6) 91 (66.4) |
> 0.05 |
|
Pain level (Scores) undocumented mild (<3) moderate (4-6) severe (7-10) |
72 (58) 46 (37) 5 (4) 1 (1) |
33 (24) 86 (62) 16 (12) 2 (1) |
< 0.001 |
|
Pain management Opioids fentanyl morphine tramadol morphine + pethidine morphine + tramadol NSAIDS diclofenac ibuprofen ibuprofen + diclofenac Other drugs paracetamol ketamine Non-pharmacological cold pack prayer talking to medical staff talking to friends and relatives |
2 (1.6) 51 (41) 3 (2) 1 (1) 0 (0) 85 (69) 29 (23) 10 (8) 85 (69) 1(1) 6 (5) 4 (3) 2 (1.6) 1 (1) |
1 (0.7) 74 (54) 3 (2) 0 (0) 2 (1.5) 47 (34) 85 (62) 3 (2) 115 (84) 2 (1.5) 24 (18) 5 (4) 20 (15) 3 (2) |
< 0.001 |
|
Level of satisfaction very satisfied satisfied neutral dissatisfied |
43 (24) 28 (18) 22 (23) 30 (35) |
81 (60) 27 (20) 26 (19) 2 (1) |
< 0.001 |
CHUK: University Teaching Hospital of Kigali, CHUB: University Teaching Hospital of Butare, NSAIDS: Nonsteroidal anti-inflammatory drugs
Different barriers to the implementation of the WHO pain ladder-based protocol have been reported by 23 ED staff mainly related to staff (i.e. inadequate experience), to the hospital (i.e. poor documentation), and to patients (i.e. reluctance to report pain). (Table 3).
Table 3.
Barriers to the implementation of the WHO pain ladder-based trauma pain protocol at EDs of CHUK and CHUB, N=23.
| Variable | Number (%) |
|---|---|
|
Respondents per hospital CHUB Doctors Nurses CHUK Doctors Nurses |
4 (17.4) 7 (30.4) 3 (13.1) 9 (39.1) |
|
Staff related barriers Inadequate experience and time constraints Inadequate experience with pain control Reluctant to use opioids Poor communication skills with patients Inadequate pain assessment |
1 (4.3) 10 (43.1) 4 (17.3) 2 (9) 2 (9) |
|
Hospital related barriers Limited staff Poor documentation Inadequate use of available pain management protocols and guidelines |
4 (17.3) 13 (56.5) 12 (52) |
|
Patients related barriers Reluctance to report pain Reluctance to take analgesics Poor communication with medical staff |
14 (60) 9 (40) 9 (40) |
CHUK: University Teaching Hospital of Kigali, CHUB: University Teaching Hospital of Butare
Discussion
The results of this study suggest that the implementation of the EPM training combined with the WHO pain ladder-based protocol decreased rates of undocumented pain scores by more than 50% and increased rates of patients with controlled or mild pain by more than 40% at 6 months post-implementation positively affecting patients’ satisfaction. The existing literature evaluating the use of guidelines for pain assessment and management have shown mixed results highlighting the importance of having robust implementation methods including availability of drugs, protocols, training of staff, and mentorship [1,[11], [12], [13]]. In addition, interventions focusing on changing organizational culture, leadership support, regular quality improvement projects as well as reporting of performance indicators, and engagement all team members (nurses, doctors, pharmacists, information technology staff, quality improvement staff, administrative staff, etc.) are essential components of a successful implementation strategy [7,8]. Furthermore, special considerations are needed in low resource settings due to unique challenges and barriers such as shortage of staff, insufficient drugs, lack of local protocols, inadequate pain training, and different beliefs and attitude towards pain among patients and healthcare providers [[20], [21], [22]].
In the context of CHUK and CHUB, the increased patient satisfaction may be explained by multiple factors. Firstly, the increase in pain score documentation may have led to timely and effective pain management, increasing the number of patients with appropriately controlled pain. In addition, more patients received morphine and paracetamol while the use of NSAIDS was maintained; this indicates that more patients were receiving multimodal pain management which is associated with adequate pain management and higher satisfaction. Our findings indicate that regular training in acute pain management and use of pain guidelines and protocols in Rwandan EDs are useful interventions with potential to sustain adequate pain management. This training may be especially impactful in environments where there is a shortage of trained emergency medicine physicians and nurses like rural district hospitals.
Despite the demonstrated improvements in the quality of pain management at CHUK and CHUB EDs, different barriers remain. These include barriers related to staff (i.e. inadequate experience), to the hospital (i.e. poor documentation), and to patients (i.e. reluctance to report pain). Similar barriers to appropriate acute pain management have been described in the literature. For example, a previous study from Rwanda found a low-level use of pain management protocols and guidelines [21]. Effective interventions should be put in place such as regular training in essential pain management, establishing a dedicated acute pain service and team, using electronic medical record to improve recording capacity, and increasing patients’ awareness about the importance of reporting pain on time and adequate pain management [[20], [21], [22]].
Reluctance to report pain observed by EDs staff is a concerning finding because it may lead to having some patients suffering from untreated pain which could be treated if reported on time. In Rwandan culture, men are supposed to be strong and are not expected to show weakness and reporting pain may be seen as a weakness, however, more studies are needed to confirm our proposed explanation. Pain awareness campaigns may be helpful in changing this situation. Previous initiatives like the zero-pain initiative had a positive impact by convening patients’ representatives, traditional healers, religious leaders, political leaders, pain experts, and other healthcare providers in one conference to share the experience about appropriate acute and chronic pain management in the context of Rwandan culture [22]. Some of the key messages shared which should be promoted using different media channels include that no one should suffer in silence without reporting their pain; pain is real, but relief is possible by speaking up; and ensuring pain management for all through education and high quality of care [22].
Limitations
Firstly, we could not eliminate observer bias; we could not control whether the ED staff changed their behavior with regards to pain management due to known ongoing evaluation of the quality of pain management at the ED. However, because the same approach was used both before and after the intervention, we believe the bias should be similar in both data collection periods. Secondly, our study was conducted in only two referral hospitals and thus the results and conclusions may not be applicable to other hospital settings.
Conclusions
The implementation of the EPM course along with mentorship to use the WHO pain ladder-based protocol significantly improved the quality of pain management for trauma patients in EDs of both referral hospitals. Despite this, some barriers remain unfixed such as inadequate staff experience, poor documentation, and patient's reluctance to report pain. Appropriate interventions should be implemented to address the identified barriers and ensure adequate pain management for patients admitted at EDs in public hospitals in Rwanda. Future research should test effective implementation strategies to implement adequate pain management protocols in low resource settings.
Dissemination of results
We will make this article accessible to all relevant stakeholders such as the ED department, hospital administration, and the ministry of health.
Authors' contributions
Authors contributed as follow to the conception or design of the work, the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: JPH 50%, ET 25%, GN 10%, and PRB, RLCA, and JDT contributed 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Funding
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zanza C., Romenskaya T., Zuliani M., Piccolella F., Bottinelli M., Caputo G., et al. Acute traumatic pain in the emergency department. Diseases. 2023;11(1):45. doi: 10.3390/diseases11010045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abu-Snieneh H.M., Alsharari A.F., Abuadas F.H., Alqahtani M.E. Effectiveness of pain management among trauma patients in the emergency department, a systematic review. Int Emerg Nurs. 2022;62 doi: 10.1016/j.ienj.2022.101158. [DOI] [PubMed] [Google Scholar]
- 3.Mura P., Serra E., Marinangeli F., Patti S., Musu M., Piras I., et al. Prospective study on prevalence, intensity, type, and therapy of acute pain in a second-level urban emergency department. J Pain Res. 2017;10:2781–2788. doi: 10.2147/JPR.S137992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fabbri A., Voza A., Riccardi A., Serra S., et al. Study and research center of the Italian society of emergency medicine (SIMEU). The pain management of trauma patients in the emergency department. J Clin Med. 2023;12(9):3289. doi: 10.3390/jcm12093289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dale J, Bjørnsen LP. Assessment of pain in a Norwegian Emergency Department. Scand J Trauma Resusc Emerg Med. 2015 Oct 29;23:86. doi: 10.1186/s13049-015-0166-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muragizi J., Guptill M., Dumitriu B.G., Henry M.B., Aluisio A.R., Nzabandora J.P. Analgesia use in trauma patients at a university teaching hospital in Kigali, Rwanda. Afr J Emerg Med. 2023;13(3):147–151. doi: 10.1016/j.afjem.2023.05.002. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raymond S. Causes and consequences of inadequate management of acute pain. Pain Med. December 2010;12(11):1859–1871. doi: 10.1111/j.1526-4637.2010.00983.x. [DOI] [PubMed] [Google Scholar]
- 8.Motov SM, Khan ANGA. Problems and barriers of pain management in the emergency department: Are we ever going to get better? J Pain Res. 2009;2:5–11. [PMC free article] [PubMed] [Google Scholar]
- 9.Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician. 2010;56(6):514–517. Jun e202-5. [PMC free article] [PubMed] [Google Scholar]
- 10.Decosterd I, Hugli O, Tamches E, et al. Oligoanalgesia in the emergency department: short-term beneficial effects of an education program on acute pain. Ann Emerg Med. 2007;50:462–471. doi: 10.1016/j.annemergmed.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 11.The European Society for Emergency Medicine (EUSEM). Guidelines for the management of acute pain in emergency situations, 2020. https://www.eusem.org/images/EUSEM_EPI_GUIDELINES_MARCH_2020.pdf, accessed on 16 June 2024.
- 12.Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986–992. doi: 10.1136/bmjqs-2015-004411. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.University Teaching Hospital of Kigali, 2024. CHUK clinical services. https://chuk.rw/clinical-services-specialties/accident-emergency-department, accessed on 20/03/2024.
- 14.University Teaching Hospital of Butare, 2024. CHUB clinical services. https://www.chub.rw/clinical-service-division/accidentemergency, accessed on 20/03/2024.
- 15.Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11(11):1172–1186. doi: 10.1016/j.jpain.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 16.Ahmadi A, Bazargan-Hejazi S, Z Heidari Zadie, Euasobhon P, Ketumarn P, Karbasfrushan A, al et. Pain management in trauma: A review study. J Inj Violence Res. 2016;8(2):89–98. doi: 10.5249/jivr.v8i2.707. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Federation Society of Anesthesiologists. Essential Pain Management (EPM) courses, 2024. https://wfsahq.org/our-work/education-training/essential-pain-management/, accessed on 16/06/2024.
- 18.American College of Surgeons (ACS). Best practices guidelines for acute pain management in trauma patients, 2019. https://www.facs.org/quality-programs/trauma/quality/best-practices-guidelines/, accessed on 20/06/2024.
- 19.Berben S, Schoonhoven L, Meijs T, Vugt V, Grunsven V., Pierre M. Prevalence and Relief of Pain in Trauma Patients in Emergency Medical Services. Clin J Pain. September 2011;27(7):587–592. doi: 10.1097/AJP.0b013e3182169036. [DOI] [PubMed] [Google Scholar]
- 20.Goucke R, Morriss W. Pain management in Low and Middle Income Countries (LMIC) just put up with it? Egypt J Anaesth. 2012;28(1):1–2. doi: 10.1016/j.egja.2011.11.005. [DOI] [Google Scholar]
- 21.Nyirigira G, Wilson RA, VanDenKerkhof EG, Goldstein DH, Twagirumugabe T, et al. Barriers and facilitators to postoperative pain management in Rwanda from the perspective of health care providers: A contextualization of the theory of planned behavior. Can J Pain. 2018 Apr 12;2(1):87–102. doi: 10.1080/24740527.2018.1451251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canadian Anesthesiologists' Society International Education Foundation (CASIEF). Dr. Livingston returns to Rwanda (3rd edition). Rwandan pain conference: from need to opportunity, 2019. https://casief.ca/announcements/dr-livingston-returns-to-rwanda-3rd-edition/, accessed on 20 August 2024.