Abstract
Background
The rise of global forced migration urges healthcare systems to respond to the needs of forced migrants (FM) during pregnancy and childbirth. Yet, comprehensive data on the health outcomes of pregnant FM in destination countries remain scarce. This study aimed to describe the characteristics and maternal and perinatal outcomes of pregnancy in this specific migrant population on a national scale in the Netherlands and to explore differences from other populations.
Methods
The Dutch perinatal registry was linked to national migration data to analyze pregnancy outcomes in FM (2014–2019), using non-migrants (NM) and resident migrants (RM) as reference populations. We reported outcome rates (% [95 % CI]) for a range of primary and secondary pregnancy outcomes. Primary outcomes included perinatal mortality, small for gestational age infants (SGA), preterm birth, and emergency cesarean section (CS), for which we also calculated the crude relative risk (RR [95 % CI]) of FM compared to NM and RM. In addition, we conducted binary logistic regression analyses on primary outcomes to report adjusted odds ratios (aORs [95 % CIs]) while controlling for multiple births, maternal age and parity.
Findings
Compared to the NM group, the FM group had increased risks of perinatal mortality (RR 1.50 [95 % CI 1.20–1.88]), SGA (1.65 [1.59–1.71], and emergency CS (1.19 [1.13–1.25]). Compared to RM, FM still had elevated risks of SGA (1.17 [1.13–1.22]). In contrast, the risk of preterm birth was lower in FM than in NM (0.81 [0.76–0.86]) and RM (0.83 [0.77–0.88]). These differences were confirmed in the adjusted analysis. Differences in secondary outcomes included higher rates of late antenatal care in FM (29.4 % [28.5–30.3]) than in NM (6.7 % [6.6–6.9]) and RM (15.5 % [15.1–15.9]). Rates of planned CS were similarly elevated (14.3 % [95 % CI 13.7–14.8] versus 7.·8 % [7.7–7.8] and 9.6 % [9.5–9.7]), while FM had lower rates of postpartum hemorrhage (3.9 % [3.6–4.2]) versus 6.8 % [6.8–6.9] and 5.7 % [5.6–5.9]).
Conclusion
This first Dutch registry-based study demonstrated increased risks of multiple, though not all, adverse pregnancy outcomes in forced migrants. Our results emphasize the imperative to further unravel and address migration-related disparities, dismantle structural barriers to health among forced migrants, and improve the inclusivity of data systems. Collaborative policy, clinical practice, and research efforts are essential to ensure equitable care for every individual, regardless of migration status.
Keywords: Forced migration, Refugees, Asylum seekers, Pregnancy, Childbirth, Perinatal health inequity
Introduction
The global population of refugees, asylum seekers, and others in need of international protection reached an unprecedented number of 45 million people under the mandate of the UNHCR in 2022. (UNHCR, 2023) Women* forced to cross borders due to threats to life or livelihood may be exposed to a multitude of negative health determinants, including gender-based violence, socioeconomic marginalization, and suboptimal healthcare. (Heslehurst et al., 2018) As a consequence, forced migrants face higher risks of a wide range of adverse outcomes of pregnancy and childbirth compared to other populations in destination countries. (Heslehurst et al., 2018; Gieles et al., 2019)
The Netherlands receives approximately 45,000 asylum applications annually, and several hundred women give birth while living in a reception center for asylum seekers. A recent study showed that these women face a sevenfold greater risk of perinatal mortality than other women in the same hospital. (Verschuuren et al., 2020) However, national population-based studies on maternal and perinatal health outcomes among forced migrants have not yet been conducted.
The scarcity of population-based studies in the Netherlands and internationally is partially attributable to the limited availability of data, as specific indicators of forced migration, such as asylum seeking status, are rarely recorded in clinical practice and national registries. (Eslier et al., 2023) Consequently, migrant populations are often poorly defined in research, which impedes further insights into the complex interactions between migration and pregnancy. (Villalonga-Olives et al., 2017) Moreover, subpopulations that face specific health disadvantages, such as forced migrants, remain understudied and underserved.
In response to these gaps, our study aimed to elucidate the characteristics and maternal and perinatal outcomes of forced migrant women in the Netherlands. We present a linkage method to identify these women in nationwide registry data and compare their pregnancy outcomes to those of non-migrant women, as well as a more heterogeneous population of migrants. In addition, we explore outcome variations between forced migrants with different migration characteristics. The resulting overview will be used to set the stage for future research and provide recommendations for current policy and practice.
*When referring to ‘women’ in this study, we also refer to people with a uterus who may not identify as women, such as trans men and nonbinary persons.
Methods
Study design and participants
In this retrospective registry-based cohort study, we linked individual-level birth records to routinely collected population and migration data. The study population consisted of women with a high likelihood of recent forced migration, defined as “a migratory movement in which an element of coercion exists, including threats to life and livelihood, whether arising from natural or man-made causes”. (Office EUP, 2019) We operationalized these criteria by including all asylum seekers who either arrived or obtained a residence permit as a legally recognized refugee in the Netherlands during the study period between 2014 and 2019.
To explore differences, we compared forced migrants (FM) with two reference populations: women born in the Netherlands with two native Dutch parents, referred to as non-migrants (NM), and all first-generation migrants not included in the FM population, referred to as resident migrants (RM).
The RM population comprised people with diverse migration motives, such as study or work, as well as former asylum seekers who already received a residence permit before the start of the study period (01-01-2014).
Births were eligible for inclusion if the pregnancy duration was known and above 22 weeks and if maternal age fell within the WHO reproductive range of 15–49 years. Multiple births were treated as separate records. Women giving birth more than once during the study period were included multiple times.
Data sources and linkage
We obtained birth records from the Netherlands Perinatal Registry (Perined, www.perined.nl). Perined contains maternal and perinatal data of more than 97 % of all pregnancies in the country. Birth records were linked to non-public, pseudo-anonymized microdata from Statistics Netherlands (Dutch abbreviation: CBS). We first linked to the municipal personal records database for information on maternal country of birth. To identify births in FM, we then linked Perined to the asylum migration microdata of CBS. Starting in 2014, these microdata cover monthly information on asylum seekers in reception centers, recipients of a refugee residence permit, children of these groups born in the Netherlands, and reunified family members from abroad. The microdata are provided to CBS by the Immigration and Naturalization Services, the Central Agency for the Reception of Asylum seekers, and Dutch municipalities. Linkage between registries was performed through a unique personal identification key, the Record Identification Number (RIN). The RIN is a meaningless and dimensionless number assigned by CBS as a pseudonymized version of the national citizen service number. At the time of this study, asylum seekers could request a citizen service number (Dutch abbreviation: BSN) after receiving a residence permit or after approximately six months of residence in the Netherlands. Women who did not have a BSN at the time of birth and did not receive it until the end of the study period could therefore not be included.
Data access and processing
All data sources were accessed within a data infrastructure (DIAPER; Data-InfrAstructure for ParEnts and ChildRen) managed by the National Institute for Public Health and the Environment (RIVM). (Scheefhals et al., 2023) Permission for the use of data for this study was obtained from CBS (project number 8552) and Perined (data request number 19·39). All data were handled in accordance with the EU General Data Protection Regulation and were accessed only in the secured remote-access environment of CBS.
Variables
Population characteristics
From the perinatal registry, we obtained maternal parity (categorized as none, one, two or more than two previous live births), age (mean and categorized as <20, 20–24, 25–29, 30–34 or >35 years), singleton birth (yes/no), start of care (community or hospital care), transfer from community to hospital care (no transfer/unknown, during pregnancy, during birth, postpartum or with unclear timing), and birth setting (homebirth, midwife-led hospital birth, obstetrician-led hospital birth or other/unknown).
From the municipal personal records database, we obtained maternal country of birth and categorized these into world regions as defined by the WHO, i.e., the African Region, Region of the Americas, South-East Asian Region, European Region, and West Pacific Region. The five most common countries of birth were reported separately.
From the asylum microdata, we obtained the type of FM as categorized by the immigration services (family reunification applicant or regular asylum seeker). After linkage to the perinatal registry, we derived the status of the asylum procedure during pregnancy (residence permit received prior to pregnancy, during pregnancy, or not received before birth) and the official place of residence at the time of birth (categorized as the asylum reception center, regular housing, or unknown). In addition, we calculated the number of relocations between reception centers in the period between one year prior to birth and two months postpartum (none, one, two, or more than two relocations).
Pregnancy outcomes
All pregnancy outcomes were obtained from the perinatal registry. Primary outcomes included maternal mortality (any maternal death during pregnancy or within 42 days after birth), perinatal mortality (defined as fetal or neonatal death between 22 weeks of pregnancy and seven days after birth), small for gestational age infants (SGA; birthweight below <p10 of national reference curves adjusted for gestational age and sex), preterm birth (<37 weeks of pregnancy), and emergency cesarean section (CS).
Secondary outcomes were categorized into maternal and perinatal outcomes. Secondary maternal outcomes included a late start of antenatal care (first antenatal consultation after 12 weeks of pregnancy in line with WHO recommendations), start of birth (spontaneous, induction of labor, or by planned CS), end of birth (spontaneous, instrumental, or by emergency CS), the use of intrapartum analgesics for hospital births (none, epidural analgesia from the onset of dilation, general anesthesia for CS or ‘other’), the use of general anesthesia in cases of emergency CS, postpartum hemorrhage (PPH; defined as blood loss of 1000 ml or more), and obstetric anal sphincter injury (OASI; perineal laceration grade III or IV).
Secondary perinatal outcomes included postterm birth (>42 weeks of pregnancy), low Apgar score (< seven at five minutes after birth), and admission to a neonatal intensive care unit (NICU) after birth.
Statistical analyses
All outcomes were reported as rates (proportions) with corresponding 95 % confidence intervals (95 % CI) using IBM SPSS 22. Missing values were not included in the analyses; the proportion of missing data was only reported if it was higher than 1·5 % for any variable. Since the aim of the study was to describe the maternal and perinatal health profile of FM during pregnancy and childbirth, we reported the outcome rates of NM and RM as reference populations for interpretation. To estimate the differences between FM and the reference populations, we calculated crude relative risks (RR) with 95 % CI for the primary outcomes. In addition, we conducted binary logistic regression analyses to report adjusted odds ratios (aORs) with 95 % CI, controlling for multiple births, maternal age and parity.
We performed a sensitivity analysis including only singleton births, to address the potential bias caused by the overrepresentation of mothers with multiple births among the adverse outcomes in the main analysis. In case of multiple births of the same mother in the study period, we only included the first-born in the sensitivity analysis.
In additional analyses, we explored the relevance of specific migration characteristics among FMs. Specifically, we compared rates of primary outcomes between regular asylum seekers and women registered as family reunification applicants. Furthermore, we compared women from the top five countries of birth in FM to women from the same country of birth in the RM group. For example, Syrian FM were compared to Syrian RM.
Ethical approval
The study was submitted to the Medical Ethical Committee of the Erasmus Medical Center in Rotterdam, which determined that formal ethical review was not required under the Dutch Medical Research Involving Human Subjects Act (registration number MEC-2021-0101).
Role of the funding source
This study was part of the EGALITE research project funded by The Netherlands Organization for Health Research and Development (ZonMw, grant number 54300311). The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Study populations and characteristics
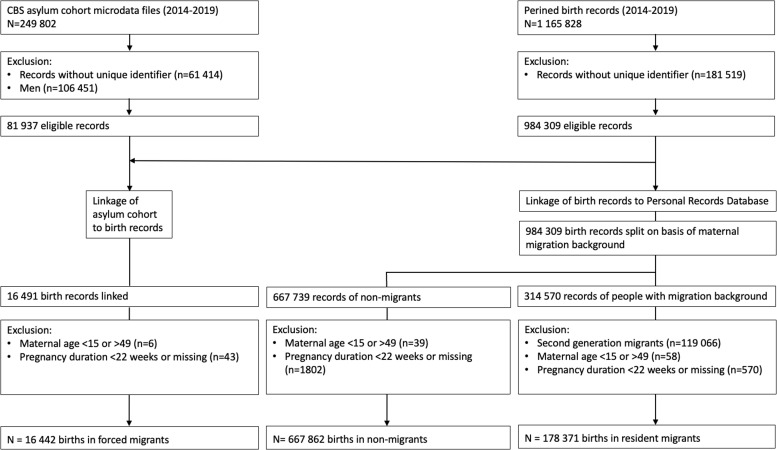
The asylum microdata contained 249,802 records of FM; 61,414 of those did not have a RIN required for linkage, and 106,451 records concerned men. Of the remaining 81,936 records, 16,491 could be linked to the perinatal registry, of which 16,442 met the inclusion criteria. These births in FM could be compared to the 667,862 births in NM and the 178,371 births in RM. Fig. 1 depicts the linkage and inclusion of all study populations.
Fig. 1.
Flow diagram of the study populations.
Table 1 presents the maternal characteristics of FM, NM, and RM, as well as the specific migration characteristics of FM. All characteristics contained less than 0.5 % missing data. Overall, FM were younger (M 28.0, SD 5.5 years) compared to NM (M 30.7, SD 4.5) and RM (31.6, SD 5.2), and FM had higher rates of teenage pregnancies (4.5 % vs. 0.7 % and 0.8 % respectively), and parity above two (19.5 % vs. 4.7 % and 10.3 % respectively). Compared to RM, FM more commonly originated from the East-Mediterranean (64.0 %, vs. 23.3 %) and the African region (31.5 % vs. 6.1 %). The five most common maternal countries of birth in FM were Syria (48.6 %), Eritrea (22.9 %), Somalia (5.5 %), Iraq (3.4 %), and Afghanistan (2.2 %). During pregnancy, FM were transferred from community midwifery care to hospital care relatively often (45.4 % of FM, vs. 37.3 % of NM and 39.6 % of RM), and mostly gave birth under supervision of an obstetric specialist in the hospital (80.4 % vs. 70.0 % and 78.6 % respectively).
Table 1.
Maternal characteristics of all study populations and migration characteristics of forced migrants.
| Forced migrants (N = 16,442) |
Non-migrants (N = 667,862) |
Resident migrants (N = 178,371) |
||
|---|---|---|---|---|
|
Age at childbirth (years) |
M (SD) | 28.0 (5.5) | 30.7 (4.5) | 31.6 (5.2) |
| <20 | 4.5 | 0.7 | 0.8 | |
| 20–24 | 24.8 | 7.4 | 8.3 | |
| 25–29 | 33.1 | 31.3 | 25.2 | |
| 30–35 | 27.0 | 46.1 | 42.3 | |
| >35 | 10.6 | 14.5 | 23.3 | |
|
Parity |
0 | 31.7 | 45.3 | 40.9 |
| 1 | 28.7 | 37.3 | 33.1 | |
| 2 | 20.2 | 12.7 | 15.7 | |
| >2 | 19.4 | 4.7 | 10.3 | |
|
World region of birth |
African Region | 31.5 | · | 6.1 |
| Region of the Americas | 0.2 | · | 14.9 | |
| South-East Asian Region | 0.7 | · | 5.6 | |
| European Region | 2.7 | 100.0 | 43.7 | |
| East-Mediterranean Region | 64.0 | · | 23.3 | |
| West-Pacific Region | 0.8 | · | 6.5 | |
|
Country of birth |
Syria | 46.9 | · | 0.6 |
| Eritrea | 22.9 | · | 0.2 | |
| Somalia | 5.5 | · | 2.7 | |
| Iraq | 3.4 | · | 2.4 | |
| Afghanistan | 2.2 | · | 2.4 | |
| Netherlands | · | 100.0 | · | |
| Other | 19·0 | · | 91.7 | |
| Multiple births | 2.4 | 3.1 | 3.0 | |
|
Start of care |
Community care | 89.4 | 89.7 | 85.4 |
| Hospital care | 10.1 | 10.0 | 14.1 | |
| Unknown/NA | 0.5 | 0.3 | 0.5 | |
|
Transfer of community to hospital care |
None/unknown | 27.7 | 37.0 | 33.1 |
| During pregnancy | 45.4 | 37.3 | 39.6 | |
| During birth | 23.9 | 22.3 | 24.5 | |
| Postpartum | 1.6 | 2.8 | 1.9 | |
| Unclear when | 1.4 | 0.6 | 0.9 | |
|
Birth setting |
Homebirth | 5·4 | 15.9 | 5.7 |
| Hospital (midwife-led) | 13.9 | 13.9 | 15.3 | |
| Hospital (obstetrician-led) | 80.4 | 70.0 | 78.6 | |
| Other/unknown | 0.2 | 0.2 | 0.3 | |
| Type of asylum applicant upon entry in the Netherlands | Regular applicant | 60.3 | NA | NA |
| Family reunification applicant | 39.9 | NA | NA | |
|
Status of residence permit |
Received before pregnancy | 68.8 | NA | NA |
| Received during pregnancy | 13.0 | NA | NA | |
| Not received before birth | 18.1 | NA | NA | |
|
Official place of residence at birth |
Asylum reception center | 15.7 | NA | NA |
| Regular housing | 82.9 | NA | NA | |
| Unclear/missing | 1.3 | NA | NA | |
|
Relocations between asylum reception centers* |
None | 54.3 | NA | NA |
| 1 relocation | 26.9 | NA | NA | |
| 2 relocations | 11.4 | NA | NA | |
| >2 relocations | 7.4 | NA | NA | |
All data are presented as proportions (%) unless otherwise indicated.
NA = Not applicable.
Sum of relocations between three months before conception and two months postpartum among women residing in asylum reception centers at the time of childbirth (n = 2 581).
Regarding migration characteristics, 60.3 % of FM were registered as regular asylum seekers, and 39.7 % were registered as family reunification applicants. Overall, most women (68.8 %) already received a residence permit as a refugee before pregnancy, 13.0 % received it during pregnancy, and 18.1 % did not have a residence permit when giving birth. Of the 15.7 % of FM who resided in an asylum reception center at the time of birth, approximately half (54.3 %) were not relocated between centers in the perinatal period (defined as one year before until two months after birth), while 26.9 % were relocated once, 11.4 % were relocated twice, and 7.4 % were relocated more than twice.
Pregnancy outcomes
Primary outcomes
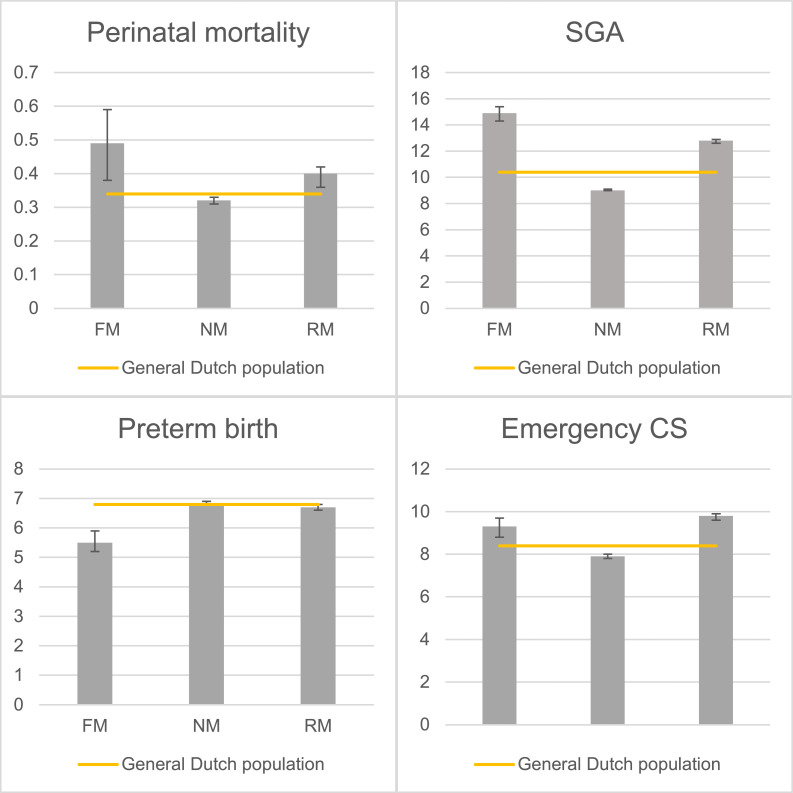
Table 2 presents the rates, crude relative risks, odds ratios and adjusted odds ratios of primary outcomes in FM compared to those in NM and RM. No maternal deaths were registered in FM in the study period (results not in table; excluded from further analysis). The crude relative risk of perinatal mortality in FM was higher than that in NM (RR 1.50 [95 % CI 1.20–1.88]. Compared to RM, the relative risk of perinatal mortality appeared higher as well, but fell marginally short of the 95% confidence confidence threshold (1.23 [0.98–1.55]). The relative risk of SGA was elevated in FM compared to NM (1.65 [1.59–1.71] and to RM (1.17 [1.13–1.22]). In contrast, the risk of preterm birth was lower in FM than in NM (0.81 [0.76–0.86]) and RM (0.83 [0.77–0.88]). Finally, the risk of emergency CS was again higher in FM than in NM (1.19 [1.13–1.25]), although not in RM (0.95 [0.91–1.00]). Fig. 2 presents the rates of primary outcomes in FM, NM and RM with the total population as a reference.
Table 2.
Rates, crude relative risks (RR), odds ratios (OR) and adjusted odds ratios (aOR) of primary outcomes in forced migrants (FM) compared to non-migrants (NM) and resident migrants (RM).
| Outcome | Group | Rate |
RR (FM vs. reference group) |
OR (FM vs. reference group) |
aOR (FM vs. reference group)* |
||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95 % CI | 95 % CI | 95 % CI | 95 % CI | |||||
|
Perinatal mortality |
FM | 0.49 | 0.38–0.59 | - | – | – | – | - | – |
| NM | 0.32 | 0.31–0.33 | 1.50 | 1.20–1.88 | 1.51 | 1.20–1.88 | 1.43 | 1.14–1.79 | |
| RM | 0.40 | 0.36–0.42 | 1.23 | 0.98–1.55 | 1.23 | 0.98–1.55 | 1.22 | 0.96–1.54 | |
|
SGA |
FM | 14.9 | 14.3–15.4 | – | – | – | – | – | – |
| NM | 9.0 | 9.0–9.1 | 1.65 | 1.59–1.71 | 1.77 | 1.69–1.85 | 1.96 | 1.87–2.05 | |
| RM | 12.8 | 12.6–12.9 | 1.17 | 1.13–1.22 | 1.20 | 1.15–1.26 | 1.30 | 1.24–1.36 | |
|
Preterm birth |
FM | 5.5 | 5.2–5.9 | – | – | – | – | – | – |
| NM | 6.8 | 6.8–6.9 | 0.81 | 0.76–0.86 | 0.80 | 0.74–0.86 | 0.84 | 0.78–0.91 | |
| RM | 6.7 | 6.6–6.8 | 0.83 | 0.77–0.88 | 0.81 | 0.76–0.87 | 0.86 | 0.80–0.92 | |
|
Emergency CS |
FM | 9.3 | 8.9–9.8 | – | – | ||||
| NM | 7.9 | 7.8–8.0 | 1.19 | 1.13–1.25 | 1.21 | 1.14–1.27 | 1.71 | 1.62–1.81 | |
| RM | 9.8 | 9.7–10.0 | 0.95 | 0.91–1.00 | 0.95 | 0.90–1.00 | 1.28 | 1.21–1.36 | |
Adjusted for multiple births, maternal age and parity
SGA = Small for gestational age infant.
CS = Cesarean section.
Fig. 2.
Bar charts of primary outcome rates (%) in forced migrants (FM), non-migrants (NM), and resident migrants (RM).
SGA: Small for gestational age infants. CS: Cesarean section. Y-axis represents rates (%), with 95 % confidence intervals represented in error bars. The reference line (general Dutch population) represents the outcome rates for all registered births in the Netherlands in the study period (2014–2019).
After adjusting for multiple births, maternal age and parity, the odds of perinatal mortality remained higher in FM than in NM (aOR 1.43 [1.14–1.79]). Compared to the reference populations, the risk of FM increased for SGA (aOR 1.96 [1.87–2.05] and 1.30 [1.24–1.36]) and emergency CS [aOR 1.71 [1.62–1.81] and 1.28 [1.21–1.36]) in the adjusted analyses. The risk of preterm birth remained lower for FM compared to NM and RM (aOR 0.84 [0.78–0.91] and 0.86 [0.80–0.92]).
Secondary outcomes
Table 3 presents the rates of secondary maternal and perinatal outcomes in FM, NM, and RM. Only the outcomes ‘start of antenatal care’ and ‘intrapartum analgesics’ contained more than 1.5 % missing data (8.4 % and 17.5 % on average, respectively).
Table 3.
Rates of secondary outcomes in forced migrants (FM), non-migrants (NM), and resident migrants (RM).
| Group |
FM |
NM |
RM |
||||
|---|---|---|---|---|---|---|---|
| % | 95 % CI | % | 95 % CI | % | 95 %CI | ||
| Maternal outcomes | |||||||
| Late start of antenatal care | 29.4 | 28.5–30.3 | 6.7 | 6.6–6.9 | 15.5 | 15.1–15.9 | |
| Mode of birth (start) | Spontaneous | 64.1 | 63.4–64.9 | 69.9 | 69·8–70.0 | 68.0 | 67.8–68.2 |
| Induction of birth | 20.2 | 19.6–20.8 | 21.8 | 21.7–21.9 | 21.8 | 21.6–22.0 | |
| Planned CS | 14.3 | 13.7–14.8 | 7.8 | 7.7–7.8 | 9.6 | 9.5–9.7 | |
| Mode of birth (end) | Spontaneous | 69.1 | 68.4–69.8 | 76.2 | 76.1–76.3 | 73.2 | 73.0–73.4 |
| Instrumental birth | 5.9 | 5.5–6.3 | 7.6 | 7.5–7.6 | 6.7 | 6.6–6.8 | |
| Emergency CS | 9.3 | 8.9–9.8 | 7.9 | 7.8–8.0 | 9.8 | 9.7–10.0 | |
| Intrapartum analgesics | None | 28.9 | 28.3–29.6 | 26.9 | 26.7–27.0 | 26.0 | 25.7–26.3 |
| Epidural anesthesia* | 17.4 | 16.8–18.0 | 18.8 | 18.7–18.9 | 22.3 | 22.1–22.5 | |
| General anesthesia | 2.2 | 2.0–2.5 | 0.8 | 0.8–0.9 | 1.2 | 1.1–1.2 | |
| Analgesics in emergency CS | General anesthesia | 11.2 | 9.7–13.0 | 6.3 | 6.1–6.5 | 6.8 | 6.5–7.2 |
| Other | 88.8 | 88.3–89.3 | 93.7 | 93.5–93.9 | 93.2 | 89.9–93.4 | |
| Postpartum hemorrhage | 3.9 | 3.6–4.2 | 6.8 | 6.8–6.9 | 5.8 | 5.7–5.9 | |
| Obstetric anal sphincter injury | 1.8 | 1.6–2.0 | 2.1 | 2.0–2.1 | 1.8 | 1.8–1.9 | |
| Perinatal outcomes | |||||||
| Postterm birth | 1.0 | 0.9–1.2 | 0.5 | 0.5–0.5 | 0.6 | 0.6–0.6 | |
| Low Apgar score | 2.6 | 2.4–2.9 | 1.7 | 1.7–1.7 | 2.1 | 2.0–2.1 | |
| NICU admissions | 3.7 | 3.4–4.0 | 3.8 | 3.7–3.8 | 4.3 | 4.2–4.4 | |
All data are reported as proportions (%, [95 % confidence intervals]).
Only the use of epidural anesthesia in labor (excluding CS) is reported.
CS = Cesarean section.
NICU = Neonatal Intensive Care Unit.
Notable differences in maternal outcomes included a higher rate of late antenatal care in FM (29.4 % [28.5–30.3]) than in NM (6.7 % [6.6–6.9]) and RM (15.5 % [15.1–15.9]). We also observed higher rates of planned CS in FM than in NM and RM (14.3 % [13.7–14.8] vs. 7.8 % [7.7–7.8] and 9.6 % [9.5–9.7]). Furthermore, the rate of hospital births without any intrapartum analgesics was higher in FM (28.9 % [28.3–29.6]) than in NM (26.9 % [26.7–27.0]) and RM (26.0 % [25.7–26.3]). In particular, the use of general anesthesia was higher in FM than in both other groups, particularly in cases of emergency CS (11.2 % [9.7–12.9] vs. 6.3 % [6.1–6.5] in NM and 6.8 % [6.5–7.2] in RM). In contrast, the incidence of PPH was notably lower in FM (3.9 % [3.6–4.2]) than in both NM (6.8 % [6.8–6.9]) and RM (5.7 % [5.6–5.9]).
Notable differences in perinatal outcomes included a higher rate of postterm births in FM than in both NM and RM (1.0 % [0.9–1.2] vs. 0.5 % [0.5–0.5] and 0.6 % [0.6–0.6]), as well as a higher rate of low Apgar scores (2.6 % [2.4–2.9] vs. 1.7 % [1.7–1.7] and 2.1 % [2.0–2.1]). The rate of NICU admissions was similar in FM compared to NM (3.7 % [3.4– 4.0 vs. 3.8 % [3.7–3.8]) and lower compared to RM (4.3 % [4.2–4.4]).
Sensitivity analyses and subanalyses
A sensitivity analysis, including only first-born singleton births in the dataset, revealed differences similar to those of the main analyses. Analyses of subgroups within the FM population revealed that in comparison to regular asylum seekers, family reunification applicants had lower rates of preterm birth (4.7 % [4.2–5.3] vs. 6.0 % [5.6–5.5]) and emergency CS (7.0 % [6.4–7.7] vs. 10.8 % [10.2–11.4]) (see supplementary material).
Comparison of perinatal mortality rates between the FM and RM groups with the same country of birth was not possible due to unreportable data resulting from low sample sizes. No differences in other primary outcomes were observed between these groups.
Discussion
This registry-based cohort study confirms that recently arrived forced migrants in the Netherlands are more likely to experience several adverse pregnancy outcomes, compared to both non-migrants and migrants with a different profile (resident migrants). In particular, compared to the reference populations, forced migrants had higher risks of multiple adverse outcomes, including perinatal mortality and small for gestational age (SGA) infants. Forced migrants also had higher risks of emergency CS than non-migrants, whereas their risk of preterm birth was lower than non-migrants and resident migrants. Rates of secondary outcomes were mostly elevated in forced migrants, including the rate of late start of antenatal care, planned cesarean sections, postterm birth and low Apgar scores, while postpartum hemorrhage rates were lower in forced migrants than in non-migrants and resident migrants.
Our nationwide findings support the evidence that women affected by forced migration face specific inequities in pregnancy and childbirth and underscore the need to address structural health barriers for this population. (Heslehurst et al., 2018; Juárez et al., 2019) (Sturrock et al., 2021; Liu et al., 2019; Gibson-Helm et al., 2015) In the Netherlands, these may include lengthy asylum procedures, limited socioeconomic opportunities, and substandard or unstable living conditions in asylum reception centers. (Bollini et al., 2009; Harakow et al., 2021) Nearly half (45.7 %) of the women in asylum reception centers at the time of birth in this study were relocated at least once in the perinatal period, which likely reduced continuity and quality of care and exacerbated maternal stress. (Tankink et al., 2021; Verschuuren et al., 2023) In addition, the high rates of late antenatal care, cesarean sections, and the use of general anesthesia in emergency cesareans may reflect barriers to seeking, accessing and receiving high-quality care. (Heslehurst et al., 2018; Esscher et al., 2014; Bozorgmehr et al., 2018; Schrot-Sanyan et al., 2021) Suboptimal care can result from women's lack of trust and information, unresolved language barriers, or a lack of culturally appropriate care, including professionals’ implicit bias or racism. (Royce et al., 2023; Koopmanschap et al., 2022; Sheikh et al., 2022) Measures to facilitate equitable care should therefore target both the conditions for a healthy pregnancy, such as safe and stable housing for asylum seekers, and care responsiveness, for instance, by advancing guidelines and professional training. (Verschuuren et al., 2023; Balaam et al., 2021)
The observed perinatal mortality rate of 0.5 % in our national forced migrant cohort contrasts with the 3.2 % rate reported in a recent study from the Netherlands' primary reception center for asylum seekers. (Verschuuren et al., 2020) This difference may be related to the added stress and limited access to healthcare faced by women arriving pregnant at the primary reception center, while our larger cohort also included women in later stages of the asylum procedure and recognized refugees. (Van Loenen et al., 2018) In addition, the primary reception center accommodates more recently arrived asylum seekers and undocumented women, who may face the highest risk of adverse outcomes. (de Jonge et al., 2011; Eslier et al., 2022) Undocumented women only have the right to stay in a reception center in the weeks around childbirth, and lack a citizen service number needed for data linkage. We thereby inadvertently excluded at least one maternal death, which was reported to us by a midwife after the study.
Other remarkable findings, such as the reduced risk of preterm birth, and lower rate of PPH in forced migrants compared to non-migrants and resident migrants also underscore the complexity of the relationship between different pregnancy outcomes and forced migration. Lower preterm birth rates have previously been reported in forced migrant populations, though remain poorly understood. (Harakow et al., 2021; Sørbye et al., 2014) Explanations for the lower preterm birth rates in forced migrants could include bias in pregnancy dating or a higher rate of early miscarriages. (Bozorgmehr et al., 2018; Khadra et al., 2022; Juárez et al., 2021) In addition, although maternal stress is associated with increased preterm birth rates in other populations, an adaptive response to the specific stress of forced migration might delay labor until the mother reaches safer circumstances, resulting in longer fetal survival under suboptimal uterine conditions. This could also explain the observed higher rates of postterm birth and SGA in forced migrants, as well as fewer preterm births.
Further research should address the heterogeneity within the forced migrant population to understand the mechanisms driving migration-related disparities. In this study, we refrained from adjusting for a wide range of individual characteristics to describe a general profile of the maternal and perinatal health status of women with a background of recent forced migration. However, variations in legal status, length of residence, and exposure to relocation policies within the forced migration population, which may also correlate with the geographic origin of women, likely influence outcome patterns. For instance, family reunification applicants, which mostly concern Syrian women in the Dutch context, generally spend less time in the asylum procedure, which might contribute to the reduced rates of preterm birth and emergency CS observed in the exploratory subanalyses.
The strengths of this study include the successful strategy of registry data linkage to identify a specific, often invisible population of migrants, in line with recent recommendations for advancing equity amidst fragmented healthcare and information systems. (Bozorgmehr et al., 2023) Other strengths of our approach include the multiyear, nationwide cohort of births and the comparison of forced migrants to multiple reference populations, including a more heterogeneous migrant population. The main limitation concerns the missing data of an unknown number of women who never received a citizen service number, as their birth records could not be linked. This likely led to an underestimation of adverse outcomes, including maternal mortality, among forced migrants in our study. This limitation reflects the inherent inequity caused by data invisibility of already marginalized populations and underscores the need for registration and ethical use of relevant migration indicators in clinical practice and perinatal databases. (Gagnon et al., 2010) The issuance of unique personal identification numbers needed for the linkage of health records to other registries should not depend on migrants’ legal status or length of residence.
In conclusion, this first Dutch national registry-based study on pregnancy outcomes in forced migrants demonstrated higher risks of several outcomes, including perinatal mortality and small for gestational age infants, compared to both non-migrants and resident migrants in the Netherlands. Our unadjusted and exploratory analyses also highlight the complexity of disparities and the need for further research to take heterogeneity in migrants’ characteristics and policy exposures into account. The relative invisibility of the most marginalized groups of migrants posed limitations to our study and calls for improved monitoring and registration of forced migrants in healthcare. Furthermore, our findings call for critical reflection and dismantling of structural health barriers among women in asylum reception centers and recognized refugees in the Netherlands. This will require a collaborative approach in policy, clinical practices, and research to ensure equitable care for every individual, irrespective of migration status, throughout their pregnancy journey.
Data sharing
The data used in this study are subject to restrictions imposed by CBS and Perined, preventing direct public sharing. However, investigators interested in accessing the data may submit a formal request to CBS and Perined, in accordance with their established procedures. Upon request, the authors are willing to provide the statistical syntax used for data linkage and analysis. Interested investigators are encouraged to contact the corresponding author.
CRediT authorship contribution statement
J.B. Tankink: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. L.C.M. Bertens: Writing – review & editing, Supervision, Methodology, Formal analysis. J.P. de Graaf: Writing – review & editing, Methodology, Conceptualization. M.E.T.C. van den Muijsenbergh: Writing – review & editing, Supervision, Investigation. J.N. Struijs: Writing – review & editing, Resources, Investigation, Data curation. B. Goodarzi: Writing – review & editing, Supervision, Investigation. A. Franx: Writing – review & editing, Investigation, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We are thankful to all the researchers and data managers at Statistics Netherlands (Dutch abbreviation: CBS) and the National Institute for Public Health and Environment (Dutch abbreviation: RIVM) who provided advice in the initial phase of the study, in particular regarding the registry linkage.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2024.100261.
Appendix. Supplementary materials
References
- Anon, , UNHCR . UNHCR Global Data Service, Statistics and Demographics Section; Copenhagen, Denmark: 2023. Global Trends: Forced Displacement in 2022. [Google Scholar]
- Balaam M.-C., Kingdon C., Haith-Cooper M. A systematic review of perinatal social support interventions for asylum-seeking and refugee women residing in Europe. J. Immigr. Minor. Health. 2021;24(3):1–18. doi: 10.1007/s10903-021-01242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollini P., Pampallona S., Wanner P., Kupelnick B. Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc. Sci. Med. 2009;68(3):452–461. doi: 10.1016/j.socscimed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Bozorgmehr K., Biddle L., Preussler S., Mueller A., Szecsenyi J. Differences in pregnancy outcomes and obstetric care between asylum seeking and resident women: a cross-sectional study in a German federal state, 2010–2016. BMC Pregnancy ChildBirth. 2018;18(1):1–8. doi: 10.1186/s12884-018-2053-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozorgmehr K., McKee M., Azzopardi-Muscat N., et al. Integration of migrant and refugee data in health information systems in Europe: advancing evidence, policy and practice. Lancet Reg. Health–Europe. 2023;34:1–16. doi: 10.1016/j.lanepe.2023.100744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jonge A., Rijnders M., Agyemang C., et al. Limited midwifery care for undocumented women in the Netherlands. J. Psychosom. Obstetr. Gynecol. 2011;32(4):182–188. doi: 10.3109/0167482X.2011.589016. [DOI] [PubMed] [Google Scholar]
- Eslier M., Azria E., Chatzistergiou K., Stewart Z., Dechartres A., Deneux-Tharaux C. Association between migration and severe maternal outcomes in high-income countries: systematic review and meta-analysis. PLoS Med. 2023;20(6) doi: 10.1371/journal.pmed.1004257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eslier M., Deneux-Tharaux C., Sauvegrain P., et al. Severe maternal morbidity among undocumented migrant women in the PreCARE prospective cohort study. BJOG: Int. J. Obstetr. Gynaecol. 2022;129(10):1762–1771. doi: 10.1111/1471-0528.17124. [DOI] [PubMed] [Google Scholar]
- Esscher A., Binder-Finnema P., Bødker B., Högberg U., Mulic-Lutvica A., Essén B. Suboptimal care and maternal mortality among foreign-born women in Sweden: maternal death audit with application of the ‘migration three delays’ model. BMC Pregnancy ChildBirth. 2014;14(1):1–11. doi: 10.1186/1471-2393-14-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon A.J., Zimbeck M., Zeitlin J. Migration and perinatal health surveillance: an international Delphi survey. Eur. J. Obstetr. Gynecol. Reproduct. Biol. 2010;149(1):37–43. doi: 10.1016/j.ejogrb.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Gibson-Helm M.E., Teede H.J., Cheng I.H., et al. Maternal health and pregnancy outcomes comparing migrant women born in humanitarian and nonhumanitarian source countries: a retrospective, observational study. Birth. 2015;42(2):116–124. doi: 10.1111/birt.12159. [DOI] [PubMed] [Google Scholar]
- Gieles N.C., Tankink J.B., van Midde M., et al. Maternal and perinatal outcomes of asylum seekers and undocumented migrants in Europe: a systematic review. Eur. J. Public Health. 2019;29(4):714–723. doi: 10.1093/eurpub/ckz042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harakow H.I., Hvidman L., Wejse C., Eiset A.H. Pregnancy complications among refugee women: a systematic review. Acta Obstet. Gynecol. Scand. 2021;100(4):649–657. doi: 10.1111/aogs.14070. [DOI] [PubMed] [Google Scholar]
- Heslehurst N., Brown H., Pemu A., Coleman H., Rankin J. Perinatal health outcomes and care among asylum seekers and refugees: a systematic review of systematic reviews. BMC Med. 2018;16(1):1–25. doi: 10.1186/s12916-018-1064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juárez S., Mussino E., Hjern A. Being a refugee or having a refugee status? Birthweight and gestational age outcomes among offspring of immigrant mothers in Sweden. Scand. J. Public Health. 2019;47(7):730–734. doi: 10.1177/1403494818777432. [DOI] [PubMed] [Google Scholar]
- Juárez S.P., Urquia M.L., Mussino E., Liu C., Qiao Y., Hjern A. Preterm disparities between foreign and Swedish born mothers depend on the method used to estimate gestational age. A Swedish population-based register study. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0247138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadra M.M., Suradi H.H., Amarin J.Z., et al. Risk factors for miscarriage in Syrian refugee women living in non-camp settings in Jordan: results from the Women ASPIRE cross-sectional study. Confl. Health. 2022;16(1):1–10. doi: 10.1186/s13031-022-00464-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmanschap I., Martin L., Gitsels-van der Wal J.T., Suurmond J. Counselling for prenatal anomaly screening to migrant women in the Netherlands: an interview study of primary care midwives’ perceived barriers with client–midwife communication. Eur. J. Midwifery. 2022;6 doi: 10.18332/ejm/147911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Ahlberg M., Hjern A., Stephansson O. Perinatal health of refugee and asylum-seeking women in Sweden 2014–17: a register-based cohort study. Eur. J. Public Health. 2019;29(6):1048–1055. doi: 10.1093/eurpub/ckz120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office EUP. European Migration Network (EMN) Glossary. 2019. https://home-affairs.ec.europa.eu/networks/european-migration-network-emn/emn-asylum-and-migration-glossary_en (accessed 1 November 2023).
- Royce C.S., Morgan H.K., Baecher-Lind L., et al. The time is now: addressing implicit bias and in obstetrics and gynecology education. Am. J. Obstet. Gynecol. 2023;228(4):369–381. doi: 10.1016/j.ajog.2022.12.016. [DOI] [PubMed] [Google Scholar]
- Scheefhals Z.T.M., de Vries E.F., Molenaar J.M., Numans M.E., Struijs J.N. Observational data for understanding maternity care and early life: experiences with a data-infrastructure for parents and children in the Netherlands. IJIC. 2023;23(4) doi: 10.5334/ijic.7012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrot-Sanyan S., Kolanska K., Haimeur Y., et al. Language barrier as a risk factor for obstetric anal sphincter injury–A case-control study. J. Gynecol. Obstet. Hum. Reprod. 2021;50(8) doi: 10.1016/j.jogoh.2021.102138. [DOI] [PubMed] [Google Scholar]
- Sheikh J., Allotey J., Kew T., et al. Effects of race and ethnicity on perinatal outcomes in high-income and upper-middle-income countries: an individual participant data meta-analysis of 2 198 655 pregnancies. The Lancet. 2022;400(10368):2049–2062. doi: 10.1016/S0140-6736(22)01191-6. [DOI] [PubMed] [Google Scholar]
- Sørbye I.K., Daltveit A.K., Sundby J., Vangen S. Preterm subtypes by immigrants’ length of residence in Norway: a population-based study. BMC Pregnancy ChildBirth. 2014;14(1):1–14. doi: 10.1186/1471-2393-14-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturrock S., Williams E., Greenough A. Antenatal and perinatal outcomes of refugees in high income countries. J. Perinat. Med. 2021;49(1):80–93. doi: 10.1515/jpm-2020-0389. [DOI] [PubMed] [Google Scholar]
- Tankink J.B., Verschuuren A.E., Postma I.R., et al. Childbirths and the prevalence of potential risk factors for adverse perinatal outcomes among asylum seekers in the netherlands: a five-year cross-sectional study. Int. J. Environ. Res. Public Health. 2021;18(24):12933. doi: 10.3390/ijerph182412933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Loenen T., Van Den Muijsenbergh M., Hofmeester M., et al. Primary care for refugees and newly arrived migrants in Europe: a qualitative study on health needs, barriers and wishes. Eur. J. Public Health. 2018;28(1):82–87. doi: 10.1093/eurpub/ckx210. [DOI] [PubMed] [Google Scholar]
- Verschuuren A., Postma I., Riksen Z., Nott R., Feijen-de Jong E., Stekelenburg J. Pregnancy outcomes in asylum seekers in the North of the Netherlands: a retrospective documentary analysis. BMC Pregnancy ChildBirth. 2020;20(1):1–10. doi: 10.1186/s12884-020-02985-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verschuuren A., Tankink J., Franx A., et al. Community midwives’ perspectives on perinatal care for asylum seekers and refugees in the Netherlands: a survey study. Birth. 2023;50(4):815–826. doi: 10.1111/birt.12727. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I., Von Steinbüchel N. Pregnancy and birth outcomes among immigrant women in the US and Europe: a systematic review. J. Immigr. Minor. Health. 2017;19:1469–1487. doi: 10.1007/s10903-016-0483-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.