Abstract
Introduction and importance
Chronic subdural hematoma (CSDH) is a common neurosurgical condition, particularly in the elderly. A rare variant, calcified chronic subdural hematoma, occurs more frequently in children and young adults. The calcification mechanism involves poor circulation, absorption issues, intravascular thrombosis, and prolonged hematoma existence. Clinical symptoms resemble non calcified CSDH. Surgery is generally recommended, especially for infants, young patients, or those with progressive neurological deficit. Calcified subdural hematoma is a rare cause of epilepsy.
Case presentation
Rare case of a 49-year-old male with chronic calcified subdural hematoma (CCSDH) and increased seizures. Despite a history of epilepsy, his symptoms were poorly controlled with medication. Surgical intervention, involving craniotomy and careful removal of the calcified hematoma, led to significant improvement in symptoms and restored neurological function.
Clinical discussion
Subdural hematoma (SDH) is a blood collection between the arachnoid and dura membranes, often following minor head trauma. Chronic subdural hematoma (CSDH) can occur without recalled injury, especially in individuals with conditions like epilepsy. Our patient, with a 23-year history of poorly controlled seizures, likely had undiagnosed CSDH that calcified over time. Calcified chronic subdural hematoma (CCSDH) is typically due to regressive changes and often requires surgical intervention in young or symptomatic patients to prevent further brain damage. Our patient's postoperative recovery highlights the effectiveness of surgery for symptomatic CCSDH.
Conclusion
The case highlights the importance of considering surgical treatment for symptomatic CCSDH, especially in cases with clinical deterioration. The successful outcome aligns with existing literature, emphasizing the efficacy of surgical intervention for this uncommon condition.
Keywords: Chronic, Subdural, Hematoma, Epilepsy, Craniotomy, Trauma
Highlights
-
•
Calcified chronic subdural hematoma (CCSDH) causing increased seizures
-
•
Calcification likely due to poor circulation, absorption issues, and prolonged hematoma existence
-
•
Surgery is recommended for young or symptomatic patients, not just observation.
-
•
Surgery effectively restored the patient's neurological function, highlighting its importance in CCSDH.
-
•
Post-surgery, the patient was seizure-free with significant neurological improvement.
1. Introduction
Chronic subdural hematoma (CSDH) is a common condition in neurosurgery, particularly observed in the elderly [1,2]. Its incidence varies, ranging from 1.72 to 20.6 per 100,000 persons annually. Calcified chronic subdural hematoma, also known as an “armored brain,” is a rare variant of CSDH [3,4]. This calcification occurs more frequently in children and young adults, comprising 0.3–2.7 % of all chronic subdural hematomas [4].
The mechanism behind calcification involves poor circulation and absorption in the subdural space, coupled with intravascular thrombosis and prolonged existence of the hematoma. Clinical manifestations of calcified chronic subdural hematoma resemble those of noncalcified CSDH, encompassing symptoms such as headache, altered mentation, weakness, numbness, gait disturbance, dysphasia, seizures, memory impairment, confusion, and loss of consciousness [5]. Surgery is generally recommended for calcified chronic subdural hematoma in infants, young patients, or those with progressive neurological deficits, increased intracranial pressure, or intracerebral hematoma [6].
2. Ethical consideration
An ethical endorsement was granted from college research ethics review committee preceding the writing of this case report. Written Informed consent from patients was obtained with respect to patient's confidentiality, for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
This information was written following SCARE CRITERIA [7].
3. Case
We present the case of a 49-year-old male with a long-standing history of epilepsy, diagnosed at age 16, who experienced a significant increase in seizure episodes over an 8-month period. Despite ongoing treatment with sodium valproate and carbamazepine, his seizures were not well-controlled. He was admitted to our emergency room with complaints of right-sided hemiparesis and recurrent tonic-clonic seizures lasting for 6 h. The patient also reported fecal and urinary incontinence, with postictal periods lasting 3–5 min and seizures lasting approximately 10 min. Notably, there was eye rolling and frothing at the mouth, but no tongue biting, mouth deviation, or slurred speech. The patient had no history of trauma, and apart from epilepsy, he had no other chronic illnesses such as hypertension or diabetes. He did not consume alcohol or smoke.
On examination, the patient was conscious and alert when seizure-free, with a Glasgow Coma Score of 15. His vital signs, including blood pressure, pulse rate, and respiratory rate, were within normal limits, and he was saturating normally on room air. Central nervous system examination revealed that he was oriented to person, time, and place, with intact cranial nerves. He had power grade 3 in the right upper and lower limbs, with intact sensation, normal tone, and reflexes.
Laboratory investigations indicated normal values for the complete blood count, electrolytes and renal functions, (we do not do trough levels and free levels of antiepileptic drugs in our hospital).
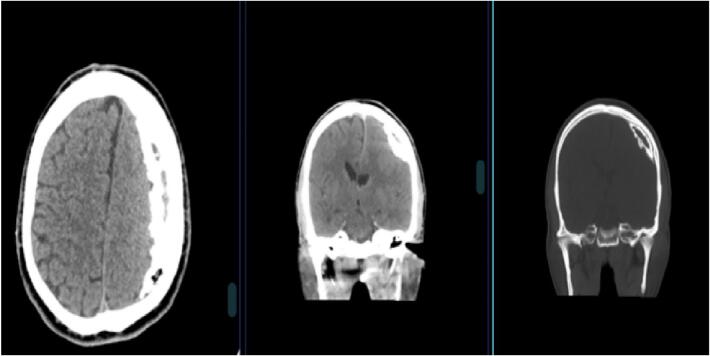
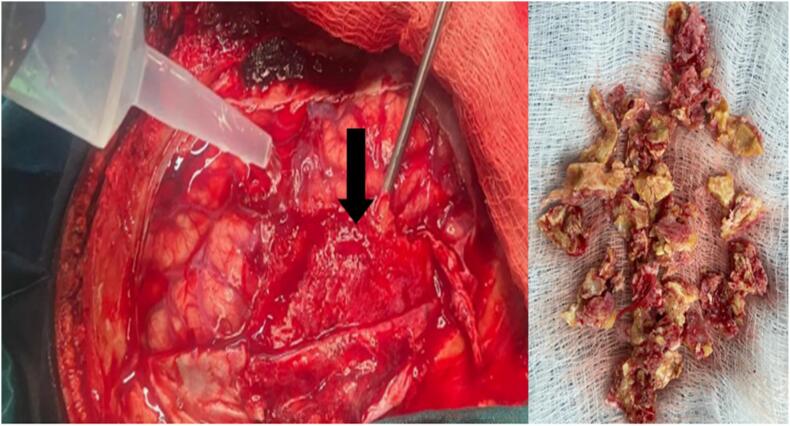
A computed tomography (CT) scan revealed a large calcified subdural hematoma in the left hemisphere (Fig. 1). Patient was prepared for surgery and a left frontoparietal craniotomy was performed, revealing an “armored dura” without an underlying hematoma. The calcified subdural hematoma, which was firmly adhered to both the dura and the brain, was carefully dissected and removed in small fragments to prevent brain damage (Fig. 2). Hemostasis was ensured, a drain was placed in the subdural space, and the bone was replaced before closing the skin in layers.
Fig. 1.
CT-scan of the brain showing a hyperdense lesion on the left frontal temporal parietal region wit same intensity as the bone.
Fig. 2.
Shows a craniotomy flap with the calcified hematoma beneath piece meal fragments of calcified hematoma.
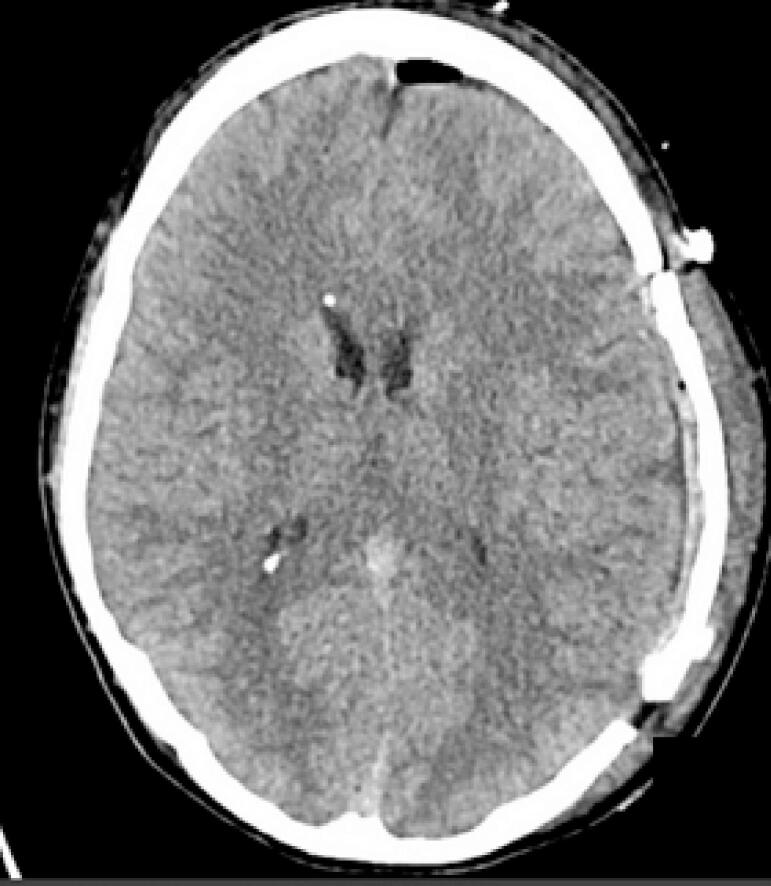
Following the surgery, the patient was prescribed prophylactic anti-convulsant. Patient was discharged home four days post, Follow-ups at the surgical clinic at 2 weeks, 3 months, showed no recurrence of the aforementioned symptoms, and the patient remained seizure-free while taking minimal doses of anticonvulsants. Subsequent CT scans after the surgery indicated ongoing improvement in brain expansion and complete resolution of the subdural hematoma, as shown in (Fig. 3).
Fig. 3.
CT-scan images post-operative showing fully brain expansion.
4. Discussion
Subdural hematoma (SDH) is a stagnant collection of blood or its breakdown products that amasses between the arachnoid and dura membranes [8]. The prevailing understanding of chronic subdural hematoma (CSDH) pathophysiology suggests that, following a mild head injury, vessels connecting the brain's surfaces tear, leading to gradual hemorrhage and hematoma formation. Although minor head trauma is frequently cited as a primary cause of CSDH, it is commonly observed in individuals who cannot recall the traumatic incident [3]. In this case, the patient doesn't remember to have a history of trauma but based on fact that he has epilepsy he may have suffered trivial trauma to the head that he doesn't recall during an episode of seizure or as a child prior the diagnosis of epilepsy.
The initial documentation of calcified chronic subdural hematoma (CCSDH) dates back to an autopsy conducted by von Rokitansky. Typically, calcification occurs over a period exceeding six months, particularly in children and young adults. The calcification in chronic subdural hematoma may result from regressive changes, such as poor absorption, calcium deposition, and tissue hyalinization, rather than an active process.
However, the exact mechanism remains undefined [8]. In certain cases, there's a history of cranial injury or childhood illness years before discovering skull abnormalities, suggesting a progressive series of physiological changes. Trauma in children, especially at a young age, may be easily overlooked [9] our patient in this case had seizures for more for more than 23 years, that started at 16 years of age and was poorly controlled which stipulates maybe he has had the hematoma and was calcifying over time. Various perspectives exist on treating calcified chronic subdural hematoma (CCSDH), with a recommendation for observation in elderly asymptomatic cases lacking acute or progressive neurological issues [10]. However, surgical intervention is advisable for infants, young patients, or those with acute or progressive neurological disorders, given the increased risk of hemorrhage, evident from vascular proliferation in the CCSDH capsule, or the presence of intracerebral hematoma to prevent further brain damage [3]. The surgical removal of CCSDH alleviates mass effect, hence tends to reduces cerebral irritation, and enhances cerebral blood flow, leading to neurological improvement post-surgery. The case patient's postoperative neurological recovery aligns with findings from previous studies, underscoring the effectiveness of surgical intervention for symptomatic CCSDH, particularly in cases of clinical deterioration [10,11].
5. Conclusion
Chronic calcified subdural hematomas are infrequent occurrences that are generally well-tolerated due to their slow progression, despite the striking radiological findings that may lack direct clinical implications. In our reported case, we successfully removed such a lesion, leading to a gradual reduction of the patient's symptoms. This restoration resulted in the patient regaining independence in his previous neurological condition.
Drawing insights from both literature cases and our own encounter, we assert that surgical intervention is essential and feasible for symptomatic patients with these hematomas, often resulting in noticeable improvements in the patient's condition.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
The ethical clearance was obtained for Kilimanjaro Chistian university ethical clearance committee, (CRERC). Kilimanjaro, united state of Tanzania with an ethical clearance number: PG 46/2023, July 20023.
Funding
None.
Author contribution
Elizabeth Ubald Wampembe: manuscript writing, patient clerkship and surgery.
Lele Mutombo Fabrice: literature search and manuscript review.
Jay Lodhia: manuscript review.
Happiness Rabiel: Critical review and final approval of the manuscript.
Guarantor
Happiness Rabiel.
Conflict of interest statement
None.
References
- 1.Holl D.C., Volovici V., Dirven C.M.F., Peul W.C., van Kooten F., Jellema K., et al. Pathophysiology and nonsurgical treatment of chronic subdural hematoma: from past to present to future. World Neurosurg. Aug 1 2018;116:402–411.e2. doi: 10.1016/j.wneu.2018.05.037. [DOI] [PubMed] [Google Scholar]
- 2.Ramachandran R., Hegde T. Chronic subdural hematomas—causes of morbidity and mortality. Surg. Neurol. Apr 1 2007;67(4):367–372. doi: 10.1016/j.surneu.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 3.Yang W, Huang J. Chronic subdural hematoma. Neurosurg Clin N Am [Internet]. Apr;28(2):205–10. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1042368016300997. [DOI] [PubMed]
- 4.Snopko P., Kolarovszki B., Opsenak R., Hanko M., Benco M. Chronic calcified subdural hematoma - case report of a rare diagnosis. 2020;164(2):209–212. doi: 10.5507/bp.2019.041. http://biomed.papers.upol.cz/doi/10.5507/bp.2019.041.html Available from: Biomed Pap [Internet] [DOI] [PubMed] [Google Scholar]
- 5.Niaz A., Nasir M.H., Niraula K., Majeed S., Neupane J., Habib Vohra A. Factors affecting the surgical outcome in extradural hematoma in Punjab Institute of Neurosciences, Lahore, Pakistan. Original Article Nepal Journal of Neuroscience. 2017;14 [Google Scholar]
- 6.Moon K.S., Lee J.K., Kim T.S., Jung S., Kim J.H., Kim S.H., et al. Contralateral acute subdural hematoma occurring after removal of calcified chronic subdural hematoma. J Clin Neurosci [Internet]. Mar 2007;14(3):283–286. doi: 10.1016/j.jocn.2005.11.016. https://linkinghub.elsevier.com/retrieve/pii/S0967586805004273 Available from: [DOI] [PubMed] [Google Scholar]
- 7.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg [Internet]. May 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. https://journals.lww.com/10.1097/JS9.0000000000000373 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beck J., Gralla J., Fung C., Ulrich C.T., Schucht P., Fichtner J., et al. Spinal cerebrospinal fluid leak as the cause of chronic subdural hematomas in nongeriatric patients. J Neurosurg [Internet]. Dec 2014;121(6):1380–1387. doi: 10.3171/2014.6.JNS14550. https://thejns.org/view/journals/j-neurosurg/121/6/article-p1380.xml Available from: [DOI] [PubMed] [Google Scholar]
- 9.Norman C.H., Dubowy J. Chronic calcified subdural hematoma. J Natl Med Assoc [Internet]. Jan 1971;63(1):3–5. http://www.ncbi.nlm.nih.gov/pubmed/5113624 Available from: [PMC free article] [PubMed] [Google Scholar]
- 10.Yan H.J., Lin K.E., Lee S.T., Tzaan W.C. Calcified chronic subdural hematoma: case report. Changgeng Yi Xue Za Zhi. 1998;21(4):521–525. [PubMed] [Google Scholar]
- 11.Oda S., Shimoda M., Hoshikawa K., Shiramizu H., Matsumae M. Organized chronic subdural haematoma with a thick calcified inner membrane successfully treated by surgery: a case report. Tokai J Exp Clin Med [Internet]. Sep 20 2010;35(3):85–88. http://www.ncbi.nlm.nih.gov/pubmed/21319032 Available from: [PubMed] [Google Scholar]