Abstract
Omphalitis is an infection of the umbilicus that can cause inflammation to spread. Omphalitis is rare in adults; however, it can occasionally occur owing to urachal remnants. A 61-year-old male patient with abdominal pain and umbilical pus was admitted to the emergency room. Abdominal computed tomography revealed peritonitis with multiple intra-abdominal abscesses. The patient was diagnosed with peritonitis resulting from urachal cyst rupture. Laparoscopic drainage of the abscesses and excising of the umbilicus and intra-abdominal fistula tract were performed. Antibiotics were administered, and the patient was discharged uneventfully. The rarity of peritonitis caused by infection and urachal cyst rupture can make diagnosing omphalitis challenging. Therefore, in this case report and literature review, we discuss the diagnosis and treatment of complicated omphalitis, which rarely progresses to peritonitis owing to ruptured urachal cysts.
Keywords: Peritonitis, Rupture, Umbilicus, Urachal cyst
INTRODUCTION
Omphalitis is an infection of the umbilicus during which inflammation may spread and is rare in adults. Some cases have been reported in which omphalitis originated from urachus or vitelline duct remnants and foreign bodies such as piercings, lint, and toilet paper [1]. Initially, patients may experience mild symptoms such as tenderness around the umbilicus, redness, or foul-smelling discharge from the umbilicus. Untreated omphalitis can progress, which can affect the abdominal wall, and may present with systemic symptoms such as fever and general weakness, indicating a septic condition. In rare cases, infection and urachal cyst rupture can lead to acute peritonitis. However, owing to its rarity in adults, the cause of peritonitis may be misdiagnosed, leading to incorrect treatment. Furthermore, only a few cases of peritonitis caused by urachal cyst rupture have been reported. Therefore, in the present case report, we present a case of peritonitis caused by a ruptured urachal cyst accompanied by omphalitis and discuss it in the context of the existing literature.
CASE REPORT
Patient information
A 61-year-old male patient with abdominal pain and umbilical discharge that had developed a week earlier was admitted to the emergency room. He was initially treated at a local hospital. The patient had hypertension and underwent coronary stent implantation.
Clinical findings and timeline
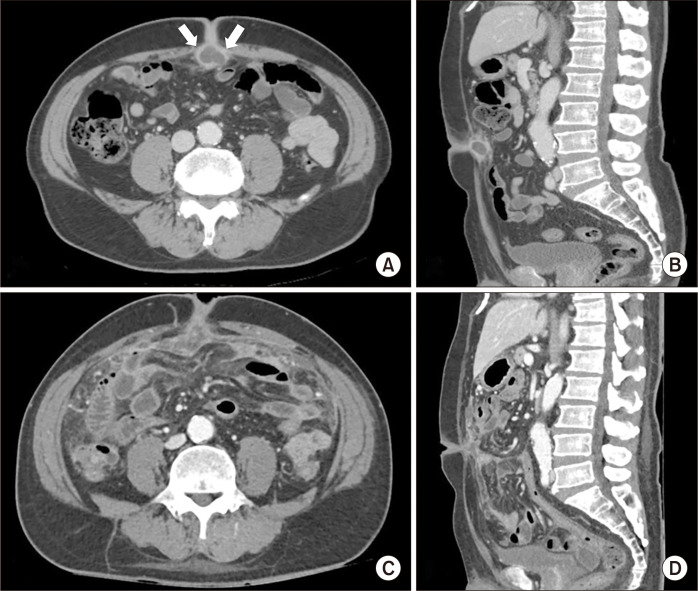
His vital signs were a blood pressure of 130/105 mmHg, a pulse rate of 107 beats/min, and a body temperature of 37.2 °C. Tenderness and rebound tenderness were observed throughout the entire abdomen. Laboratory tests indicated a white blood cell count of 15,790 cells/μL and a C-reactive protein (CRP) level of 18.14 mg/dL. Abdominal computed tomography (CT) revealed diffuse omental infiltration with peritoneal enhancement, indicating peritonitis. CT also showed multiple small omental abscesses and a cystic lesion around the umbilicus with peripheral rim enhancement (Fig. 1). A previous CT scan revealed a cystic abscess just below the umbilicus but did not indicate evidence of peritonitis. No visible communicating tract or calcification was observed along the umbilical line or bladder.
Fig. 1.
Computed tomography (CT) scans. (A, B) Images obtained at a local hospital 1 week before the visit (A, axial; B, sagittal). (C, D) Images acquired in the emergency room on the day of the visit (C, axial; D, sagittal). The images reveal multiple small abscesses in the omentum and a peripheral rim enhancement surrounding the cystic lesion near the umbilicus in the bottom panel. Compared to the bottom panel, the cystic lesion near the umbilicus (arrows) in the top panel is intact.
Diagnostic assessment
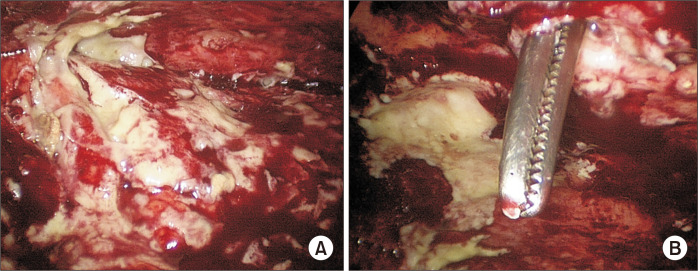
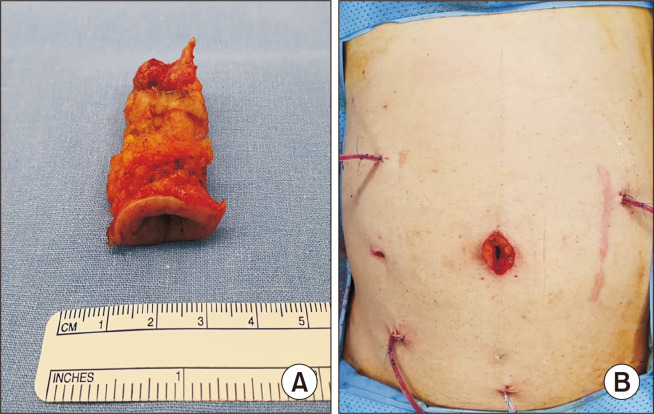
Emergency laparoscopic exploration was performed. However, severe inflammatory adhesions made it challenging to access the peritoneal space. Umbilical necrosis had occurred, creating a communication between the skin and abdominal cavity (Fig. 2). We performed adhesiolysis, abscess drainage, and umbilical removal, including the intra-abdominal fistular tract just below the umbilicus (Fig. 3). Biopsy results indicated acute suppurative inflammation with granulation. After surgery, the patient received intravenous cefotaxime and metronidazole as empirical antibiotics. The pus culture result revealed methicillin-resistant Staphylococcus aureus (MRSA).
Fig. 2.
Intraoperative findings. (A) White and yellow pus on the peritoneum and omentum. (B) Notably, umbilical necrosis was observed, creating a communication between the skin and the abdominal cavity.
Fig. 3.
Gross findings from the operating room. (A) Laparoscopic surgery was performed to remove the umbilicus, including the intra-abdominal fistular tract. (B) Multiple drains were placed to drain the abscess.
Therapeutic intervention
Teicoplanin was administered based on antibiotic susceptibility testing. The patient’s CRP level had decreased to 0.68 mg/dL, and his symptoms had improved. The patient was discharged after 30 days.
DISCUSSION
The urachus is the structure that connects the umbilicus to the bladder. The transversalis fascia covers the anterior side, whereas the peritoneum covers the posterior side. Depending on the extent of the natural closure of the urachal lumen, various urachal remnants may develop, such as urachal sinuses, patent urachus, urachal diverticula, and urachal cysts [2]. Urachal cyst infection may initially present with periumbilical symptoms, such as umbilical discharge. When a urachal cyst communicates with the bladder, urinary tract symptoms may develop, including dysuria accompanied by umbilical discharge, which can aid in the diagnosis [3]. In rare cases, the cyst can rupture, leading to peritonitis (Table 1). However, diagnosing urachal cyst rupture as the underlying cause of peritonitis can be challenging owing to the low incidence of omphalitis progressing to peritonitis or acute abdomen despite the presence of periumbilical symptoms. Furthermore, if there are no symptoms related to the umbilicus, or if the urachal remnant structure on abdominal CT is not detected, it is difficult to diagnose peritonitis due to urachal cyst rupture and it can often be misdiagnosed as acute cholecystitis, perforated appendicitis, or colon perforation [3–5]. CT imaging is valuable for differential diagnosis and establishing the relationship with surrounding structures. In our case, comparing the serial CT scan helped diagnose peritonitis caused by an infection and urachal cyst rupture, which did not communicate with the bladder. In this case, we were able to determine the intra-abdominal status before and after the occurrence of an infectious urachal cyst rupture using abdominal CT. Considering the extent and severity of inflammation is crucial when planning the treatment of omphalitis. In cases of a solitary abscess, percutaneous or incisional drainage with concomitant antibiotic therapy may be considered as first-line treatment. However, percutaneous drainage can be challenging in cases with multiple small abscesses. Therefore, antibiotics may be the preferred treatment. Subsequent surgical intervention may involve removing the umbilicus and urachal remnants to prevent recurrence [6]. In cases of peritonitis, emergency surgery may be necessary due to uncontrolled intra-abdominal infection or an unknown cause of peritonitis at the initial presentation. In most of the reviewed cases, including our case involving peritonitis caused by a ruptured urachal cyst, emergency operations were performed. Wide surgical excision, which may involve removing a portion of the bladder, may be considered when urachal remnants are connected to the urinary bladder [7]. Maruschke et al. [8] reported a case of spontaneous perforation of an infected urachal cyst that led to an extraperitoneal bladder rupture. The patient underwent a complete surgical excision of the urachal cyst along with the cuff of the bladder. The possibility of recurrence after surgery should always be considered as it is challenging to distinguish the exact structures because of the severe inflammation caused by peritonitis during surgery. Urachal remnants in adults can undergo malignant transformation. However, its disease characteristics remain unknown, and predicting this malignant transformation is challenging. Nonetheless, reports have indicated that individuals over 55 years of age, experiencing hematuria and having calcification, are more likely to have an increased risk of malignancy [9].
Table 1.
Instances of adult omphalitis resulting from urachal cyst infection progressing to peritonitis
| Study | Age (yr)/Sex | Initial symptom/urinary symptom | Abdominal examination | Preoperative diagnosis | Operative procedure | Bacteriologic features | Clinical course |
|---|---|---|---|---|---|---|---|
| Ohgaki et al. [6] | 80/female | Abdominal pain/no symptom | Diffuse tenderness | Perforated colon | Urachal cyst excision | Staphylococcus warneri | Uneventful |
| Agatstein and Stabile [5] | 31/male | Diffuse abdominal pain, fever, umbilical discharge/no symptom | Diffuse tenderness | Peritonitis | Excision of urachus and umbilicus | Prevotella melaninogenica, Peptococcus | Uneventful |
| 18/male | Umbilical pain and discharge/no symptom | Right lower quadrant tenderness | Perforated appendicitis | Urachal excision | Bacteroides, Peptococcus, Streptococcus viridans | Uneventful | |
| 25/female | Abdominal pain, fever/urinary frequency and dysuria | Periumbilical tenderness | Peritonitis | Excision | Staphylococcus epidermidis, Bacteroides asaccharolyticus, Fusobacterium nucleatum | Uneventful | |
| Horinaga et al. [7] | 68/male | Abdominal pain, fever/no symptom | Diffuse tenderness | Peritonitis | Urachal cyst excision with the dome of bladder excision | Streptococcus spp. | Death |
| Maruschke et al. [8] | 63/male | Abdominal pain and palpable mass/no symptom | Tenderness on the lower abdomen | Peritonitis | Excision of urachal cyst and the cuff of the bladder | Proteus vulgaris, Corynebacterium spp., Klebsiella pneumoniae | Uneventful |
Appropriate antibiotic treatment is crucial for clinical improvement. Microbial cultures of omphalitis yield diverse results, typically indicating a polymicrobial infection involving bacteria such as S. aureus, Streptococcus pyogenes, Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis [10]. Therefore, empirical antibiotics should be used for gram-positive and -negative bacteria. Vancomycin is recommended for cases where MRSA infection is suspected.
In conclusion, this case suggests that an infection in the urachal cyst can manifest as omphalitis and potentially develop into peritonitis. Thus, when patients present with omphalitis symptoms, urachal remnant disease should be considered in the differential diagnosis of peritonitis for early detection. When peritonitis is caused by a urachal remnant rupture, an emergency operation may be necessary. Additionally, selecting effective broad-spectrum antibiotics is essential for optimal management.
Notes
Ethics statements
This study was approved by the Institutional Review Board of Daejeon Eulji Medical Center, Eulji University (No. 2024-01-005). The patient provided informed consent for this report and for the publication of images of the patient’s body parts.
Author’s contributions
Conceptualization, Formal analysis, Methodology: MSL, MGC
Investigation: All authors
Writing–original draft: MSL, MGC
Writing–review & editing: All authors
All authors read and approved the final manuscript.
Conflict of interest
All authors have no conflicts of interest to declare.
Funding/support
None.
Data availability
The data presented in this study are available upon reasonable request to the corresponding author.
References
- 1.Rodrigues G. Umbolith: a cause of umbilical discharge and omphalitis. Infection. 2015;43:625. doi: 10.1007/s15010-015-0775-9. [DOI] [PubMed] [Google Scholar]
- 2.Schubert GE, Pavkovic MB, Bethke-Bedürftig BA. Tubular urachal remnants in adult bladders. J Urol. 1982;127:40–42. doi: 10.1016/S0022-5347(17)53595-8. [DOI] [PubMed] [Google Scholar]
- 3.Yoo KH, Lee SJ, Chang SG. Treatment of infected urachal cysts. Yonsei Med J. 2006;47:423–427. doi: 10.3349/ymj.2006.47.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohgaki M, Higuchi A, Chou H, et al. Acute peritonitis caused by intraperitoneal rupture of an infected urachal cyst: report of a case. Surg Today. 2003;33:75–77. doi: 10.1007/s005950300016. [DOI] [PubMed] [Google Scholar]
- 5.Agatstein EH, Stabile BE. Peritonitis due to intraperitoneal perforation of infected urachal cysts. Arch Surg. 1984;119:1269–1273. doi: 10.1001/archsurg.1984.01390230041009. [DOI] [PubMed] [Google Scholar]
- 6.Elkbuli A, Kinslow K, Ehrhardt JD, Jr, Hai S, McKenney M, Boneva D. Surgical management for an infected urachal cyst in an adult: case report and literature review. Int J Surg Case Rep. 2019;57:130–133. doi: 10.1016/j.ijscr.2019.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horinaga M, Masuda T, Jitsukawa S. Hinyokika Kiyo. 1998;44:505–508. doi: 10.1016/j.ijscr.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 8.Maruschke M, Kreutzer HJ, Seiter H. Bladder rupture caused by spontaneous perforation of an infected urachal cyst. Urologe A. 2003;42:834–839. doi: 10.1007/s00120-002-0290-3. [DOI] [PubMed] [Google Scholar]
- 9.Ashley RA, Inman BA, Sebo TJ, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer. 2006;107:712–720. doi: 10.1002/cncr.22060. [DOI] [PubMed] [Google Scholar]
- 10.Faridi MM, Rattan A, Ahmad SH. Omphalitis neonatorum. J Indian Med Assoc. 1993;91:283–285. [PubMed] [Google Scholar]