Abstract
Over the past two decades, robotic surgery has seen substantial advances, with significant growth in novel platforms, particularly since 2019. As a high-volume center experienced with various robotic systems, we share our initial impressions of the new da Vinci 5 platform for robot-assisted radical prostatectomy. Key improvements include enhanced console ergonomics, more precise operative imaging, and the integration of smart commands for streamlined surgical control. Notably, force feedback instruments offer the potential for reduced tissue trauma, although further studies are needed to evaluate long-term outcomes and cost effectiveness. Our early experiences suggest that surgeons familiar with previous da Vinci models, particularly the Xi platform, will find the transition to the da Vinci 5 seamless, with minimal learning curve adjustments. Using propensity score matching, we compared perioperative outcomes for 50 da Vinci 5 RARP procedures (performed after the learning curve) with 150 da Vinci Xi cases. In our experience, optimal performance and perioperative outcomes were obtained with both models. Further studies are needed to identify any clinically significant advantages of one platform over the other.
Patient summary
We compared outcomes for patients undergoing removal of the prostate using two different surgical robots (da Vinci Xi and da Vinci 5). Optimal operative outcomes were obtained with both robots, but further studies are needed to evaluate whether one robot is clinically superior to the other.
Keywords: Robotic surgery, Radical prostatectomy, Prostate cancer
Over the past two decades, robotic surgery has experienced significant growth and the development of new technologies. Since the first clinical applications and commercial use of robotic platforms in 2000, multiple platforms have been released on the market [1]. However, it is only since 2019 that there has been significant expansion of novel platforms and new robotic surgery companies. As a high-volume center in robotic surgery, we have used all of the consecutive da Vinci models, from the first version (da Vinci Standard) to the most recent da Vinci SP, as well as several other robotic brands [2], [3], [4]. Here we share our first impressions and clinical perceptions of the new da Vinci 5 robot for robot-assisted radical prostatectomy (RARP). Our aim was to describe, as surgeons, the potential benefits of this platform in clinical routine. Details of the software or other features beyond our surgical expertise are not covered here.
We recently conducted a questionnaire-based study assessing the physical discomfort and injuries that may be experienced by surgeons during robotic surgery [5]. According to the results, the most common muscle groups affected are the neck, shoulders, and back, with many surgeons attributing their muscular fatigue and discomfort to the console ergonomics. In this context, the da Vinci 5 robot includes some modifications to the surgical console. One of the most significant updates is the improved ergonomics, which allows for a better vision angle and height adjustment. This feature enables the surgeon to operate with a fully flat neck, which can minimize the risk of neck or back injuries related to poor posture described in some studies (Fig. 1) [5] In addition, the da Vinci 5 also features a lighter hand control with a rubber cover for an improved grip. However, despite these updates, the hand control performance seems similar and the finger clutch remains the same as in previous generations. The pedals and arm adjustments are also quite similar to previous models.
Fig. 1.
Console ergonomics showing the surgeon’s back and neck curvature during operation of (A) the da Vinci Xi and (B) the da Vinci 5 surgical robot.
The updated operative imaging seems more precise with better definition. Some other updates regarding setting controls have been incorporated in the surgeon’s screen. Most of the setting changes for the energy, instruments, scope angle, force feedback, and insufflation can be performed without removing the head from the console. With this platform, the surgeon can use hand control to click on the modifications required without removing their head from the console. The aim of these new functions is to improve the surgeon’s experience and potentially improve the surgical time because the surgeon does not need to move their head from the console. However, although these smart commands could facilitate interactions with the platform, in our experience they did not significantly improve the operative time or clinical outcomes.
Significant modifications have also been made to the console, vision tower, and patient side cart, particularly for the touchscreen settings. These components of the robotic system are now smartly integrated, enabling them to execute a wide array of commands to regulate various settings, including insufflation, audio volume, capture of surgical images, cautery energy, and display of annotations on the operative field. In our experience, this unified control interface across multiple components facilitates the surgical process, giving surgeons greater autonomy and eliminating the need to depend on other team members to modify these critical settings during surgery.
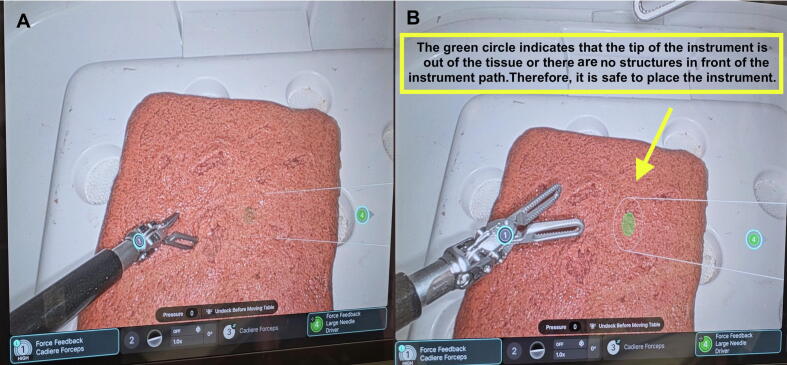
The trocar placement and docking procedures resemble those for the da Vinci Xi robot, using 8-mm trocars across all arms, a similar patient cart setup, and comparable arm articulation. We anticipate that surgical teams familiar with the Xi robot in daily practice will quickly adapt to these processes without encountering a significant learning curve. However, the system has two new security settings that identify how deep the instrument can be inserted and the location of the remote arm outside the operative view (Fig. 2). We believe that these updates benefit surgeons during the learning curve and can reduce complications related to instrument insertion and lesions outside the operative view. Table 1 summarizes the main differences between da Vinci 5 and Xi robots.
Fig. 2.
Security system for instrument placement. (A) Instrument path without a distal green dot, indicating that the instrument will hit the tissue. (B) Safe instrument path with a green dot, indicating that it is safe to place the instrument.
Table 1.
Comparison of features of the da Vinci Xi and da Vinci 5 surgical robots for radical prostatectomy
| Feature | da Vinci Xi | da Vinci 5 |
|---|---|---|
| Console ergonomics | Similar to previous generations | Improved |
| Hand commands | Similar to previous generations | Improved |
| Imaging resolution | – | Improved |
| Instruments and scope | 8 mm | 8 mm |
| Force feedback instrument | Absent | Present |
| Secure instrument placement | Absent | Present |
| Instrument position indicator | Absent | Present |
| Patient cart with four arms | Present | Present |
| Own insufflator and gas evacuation system | Absent | Present |
| Integrated console, vision tower, and patient side cart | Absent | Present |
Another notable modification is the integrated insufflation system, which comprises two separate channels situated within the robotic trocars. One trocar facilitates gas influx and the other handles smoke evacuation; both cannulas can be inserted into any of the 8-mm trocars, although we typically prefer the lateral trocars on the left and right sides. This innovative design provides a dual-flow insufflation mechanism that maintains a consistent internal pressure while simultaneously removing smoke. However, in our experience, when operating at pressures below 10 mm Hg there is a risk of abdominal wall collapse during blood suction because of the fast decrease in abdominal pressure. Consequently, at the beginning of the learning process for the insufflation system, we continued to rely on the AirSeal system to uphold low intra-abdominal pressure throughout the entire procedure. We will update our findings on clinical application of this integrated insufflation system in further studies.
A further modification is the implementation of force feedback instruments, a feature that the manufacturer claims reduces tissue traction by up to 43%. Specifically, the 8-mm instruments are equipped with integrated software that delivers force feedback when manipulating tissue, offering tactile sensation while pushing or pulling. Notably, this feedback functionality is not activated between the instrument blades during grasping, opening, or closing maneuvers. Surgeons can adjust the feedback intensity to a low, medium, or high level according to their preference and procedural requirements. On first use, particularly for prostate surgery, we observed distinct feedback effects, although ongoing clinical studies are under way to comprehensively evaluate the potential benefits in terms of surgical outcomes and patient recovery.
From April 11 to April 23, 2024, we conducted 50 consecutive RARP procedures using our established surgical technique, after excluding the first 25 cases, considered as the learning curve for the new platform [6], [7], [8]. We were able to replicate the exact steps and proficiency of our standard approach, as previously described for the Xi platform [8]. No complications or technical issues were encountered throughout the procedures. We compared these 50 cases with 150 previous RARP procedures performed with the Xi platform, selected from a cohort of 1113 (surgeries between August 2023 and May 2024) using 1:3 propensity score matching (Supplementary Table 1) [9], [10]. Our experience suggests that the learning curve for the da Vinci 5 platform involves minor adjustments and settings, rather than fundamental changes to instruments, trocar placement, pedals, or hand controls. Consequently, we believe that surgeons proficient in using the Xi platform would seamlessly transition to this updated version without significant challenges.
In conclusion, we describe the first experience with the new da Vinci 5 platform a high-volume center. After our initial contact with this surgical system, we could report optimal perioperative outcomes in patients undergoing radical prostatectomy. However, further studies are needed to describe this platform's long-term results and impacts to assess the costs of different procedures in urology and other specialties, compare outcomes of the same procedures performed on different platforms, evaluate long-term use in terms of troubleshooting, maintenance, and instrument performance, and determine the real value and associated costs of the force feedback instruments. Integrating smart commands and unified control interfaces across multiple components simplifies setup and adjustments, potentially contributing to shorter surgical times and enhanced procedural flow. The force feedback instruments also introduce a promising avenue for reducing tissue trauma and improving tactile sensation, although further research is needed to fully elucidate the clinical benefits.
Author contributions: Marcio Covas Moschovas had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Covas Moschovas, Patel.
Acquisition of data: Saikali, Gamal.
Analysis and interpretation of data: Sighinolfi.
Drafting of the manuscript: Covas Moschovas.
Critical revision of the manuscript for important intellectual content: Patel, Covas Moschovas.
Statistical analysis: None.
Obtaining funding: None.
Administrative, technical, or material support: Reddy, Rogers.
Supervision: Patel, Rocco.
Other: None.
Financial disclosures: Marcio Covas Moschovas certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Associate Editor: Roderick van den Bergh
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.euros.2024.08.014.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Gamal A., Covas Moschovas M., Jaber A.R., et al. Clinical applications of robotic surgery platforms: a comprehensive review. J Robot Surg. 2024;18:29. doi: 10.1007/s11701-023-01815-4. [DOI] [PubMed] [Google Scholar]
- 2.Covas Moschovas M., Bhat S., Rogers T., et al. da Vinci SP platform updates and modifications: the first impression of new settings. J Robot Surg. 2021;15:977–979. doi: 10.1007/s11701-021-01248-x. [DOI] [PubMed] [Google Scholar]
- 3.Covas Moschovas M., Loy D., Patel E., Sandri M., Moser D., Patel V. Comparison between intra- and postoperative outcomes of the da Vinci SP and da Vinci Xi robotic platforms in patients undergoing radical prostatectomy. J Robot Surg. 2023;17:1341–1347. doi: 10.1007/s11701-023-01563-5. [DOI] [PubMed] [Google Scholar]
- 4.Alfano C.G., Covas Moschovas M., Montagne V., et al. Implementation and outcomes of Hugo™ RAS system in robotic-assisted radical prostatectomy. Int Braz J Urol. 2023;49:211–220. doi: 10.1590/S1677-5538.IBJU.2023.9902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel E., Saikali S., Mascarenhas A., Covas Moschovas M., Patel V. Muscle fatigue and physical discomfort reported by surgeons performing robotic-assisted surgery: a multinational survey. J Robot Surg. 2023;17:2009–2018. doi: 10.1007/s11701-023-01608-9. [DOI] [PubMed] [Google Scholar]
- 6.Covas Moschovas M., Patel V. Nerve-sparing robotic-assisted radical prostatectomy: how I do it after 15.000 cases. Int Braz J Urol. 2022;48:369–370. doi: 10.1590/S1677-5538.IBJU.2022.99.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Covas Moschovas M., Patel V. Neurovascular bundle preservation in robotic-assisted radical prostatectomy: how I do it after 15.000 cases. Int Braz J Urol. 2022;48:212–219. doi: 10.1590/S1677-5538.IBJU.2022.99.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covas Moschovas M., Bhat S., Onol F.F., et al. Modified apical dissection and lateral prostatic fascia preservation improves early postoperative functional recovery in robotic-assisted laparoscopic radical prostatectomy: results from a propensity score–matched analysis. Eur Urol. 2020;78:875–884. doi: 10.1016/j.eururo.2020.05.041. [DOI] [PubMed] [Google Scholar]
- 9.Austin P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Austin P.C. Informing power and sample size calculations when using inverse probability of treatment weighting using the propensity score. Stat Med. 2021;40:6150–6163. doi: 10.1002/sim.9176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.