Abstract
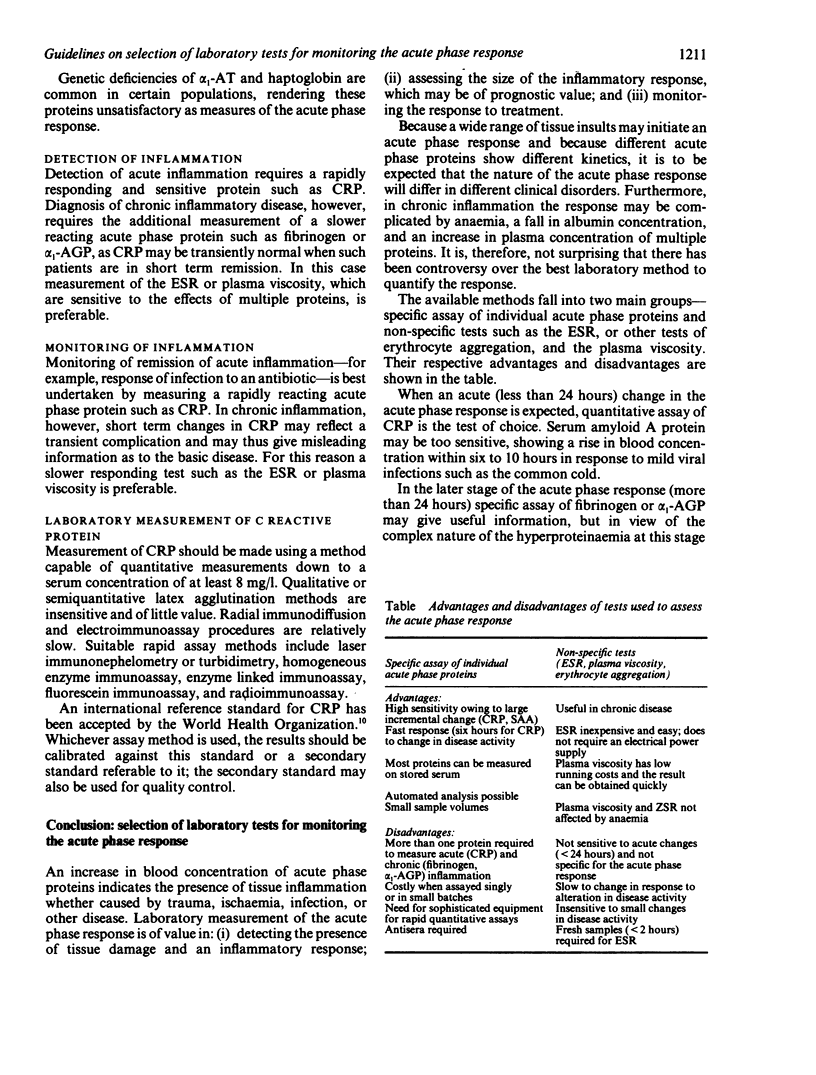
These guidelines refer to laboratory tests for monitoring changes in acute phase proteins in patients with an inflammatory response to tissue damage. Quantitative measurements of acute phase proteins are a valuable indicator of the presence, extent, and response of inflammation to treatment. When short term (less than 24 hours) changes in the inflammatory response are expected, quantitative assay of C reactive protein is the test of choice. The hyperproteinaemia that develops in response to a longer term (more than 24 hours) inflammatory response is complex and may vary from one disease to another. A test that is sensitive to the combined effect of several plasma proteins is therefore indicated, and appropriate tests include the erythrocyte sedimentation rate and plasma viscosity--the latter having several advantages. Tests for monitoring short term and long term changes in acute phase proteins are complementary and should be used for different clinical purposes; no one test is ideal for all clinical situations. A quality control programme is an essential component of laboratory tests for monitoring the acute phase response.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bull B. S., Brecher G. An evaluation of the relative merits of the Wintrobe and Westergren sedimentation methods, including hematocrit correction. Am J Clin Pathol. 1974 Oct;62(4):502–510. doi: 10.1093/ajcp/62.4.502. [DOI] [PubMed] [Google Scholar]
- Bull B. S. Clinical and laboratory implications of present ESR methodology. Clin Lab Haematol. 1981;3(4):283–298. [PubMed] [Google Scholar]
- Moseley D. L., Bull B. S. A comparison of the Wintrobe, the Westergren and the ZSR erythrocyte sedimentation rate (ESR) methods to a candidate reference method. Clin Lab Haematol. 1982;4(2):169–178. [PubMed] [Google Scholar]


