Abstract
Given fragmentation between mental health and criminal justice systems, we tested feasibility of implementing a potential new form of pre-booking jail diversion. Our “linkage system” consists of three steps: (1) individuals with serious mental illnesses and an arrest history give special consent to be enrolled in a statewide database; (2) if an officer has an encounter with an enrolled patient and runs a routine background check, he/she receives an electronic message to call; and (3) the “Linkage Specialist” provides brief telephonic assistance to the officer. Of 206 eligible individuals, 199 (96.6%) opted in; the database received 679 hits; and the Linkage Specialist received 31 calls (and in at least three cases an arrest was likely averted). Mean number of arrests was 0.59±0.92 in the year before enrollment (38.7% arrested), and 0.48±0.83 during the 12-month intervention (30.7% arrested). Implementation is feasible, and a signal that the system might reduce incarceration was detected, encouraging development of a larger study.
Keywords: Arrest, Community mental health, Criminal justice, Incarceration, Law enforcement, Police, Pre-booking jail diversion, Serious mental illnesses
Introduction
Fragmentation between mental health and criminal justice systems is a major clinical and public health burden for the estimated >1 million adults with serious mental illnesses currently in correctional supervision (Ditton, 1999; James & Glaze, 2006), as well as the multitude of others who interface frequently with police. Unnecessary criminalization and incarceration of individuals who might best be managed with outpatient mental health services signals a lack of coordination between community mental health services and the criminal justice system (Allen, Wakeman, Cohen, & Rich, 2010; Torrey, 2012). To decrease criminalization of those with serious mental illnesses requires improving mental health communication and coordination between local police and local mental health services to reduce mental health–criminal justice fragmentation, increasing mental health training for police officers, and providing better community treatment for detainees with serious mental illnesses once released (Lamb, Weinberger, & Gross, 2004). Interventions that rapidly identify and serve persons with serious mental illnesses promise to be most responsive to the needs of a substantial portion of those who are currently populating jails and prisons (Draine, Blank Wilson, Metraux, Hadley, & Evans, 2010), and those at risk of incarceration. The Sequential Intercept Model, theorized by Munetz and Griffin (2006), reveals six specific points of intervention within mental health and criminal justice systems: (1) best clinical practices within the mental health system, which will ideally prevent criminal justice involvement; (2) law enforcement and emergency services; (3) post-arrest, such as during initial detention and hearings; (4) post-hearing (e.g., mental health courts); (5) reentry from corrections institutions to the community; and (6) community corrections (i.e., probation and parole).
Patrol officers are gatekeepers to both the criminal justice and mental health systems (Wells & Schafer, 2006), and as such commonly must make on-the-scene decisions about arresting someone versus referral to mental health services versus informal resolution, often without the expertise needed to recognize mental illnesses. Many officers value the chance to consider mental health status. Despite the psychiatric-triage role of officers, they often receive very little training on mental illnesses unless they are involved in a specialized training program, such as that offered by the Crisis Intervention Team (CIT) model (Compton et al., 2014, Watson et al., 2017). Most officers want linkages with the mental health system given how much their work involves persons with mental illnesses. Straight-forward, low-cost, highly distributable approaches are needed to enhance communication, coordination, and cooperation between officers and the mental health system. Our new police–mental health linkage system was designed to address this need.
We conducted a study to test the feasibility of a potential new form of pre-booking jail diversion. Our “linkage system” consists of three steps. First, individuals with serious mental illnesses and a prior arrest history who are receiving treatment at a community mental health agency give special consent to be enrolled in a statewide database, for a very brief disclosure of their mental health status to be provided to responding officers via the state’s criminal justice information system, and for the responding officer to talk with a mental health professional. Second, when an officer has an encounter with enrolled patients and queries their name/identifiers as part of a routine background check (or “inquiry”), the officer receives an electronic message in the inquiry output on their standard in-car laptop (or via dispatch) in the same way that other output is received, such as any standing bench warrants, sex offender status, or probation/parole status. The messages states, “THE INDIVIDUAL IS A POSSIBLE PARTICIPANT IN A MENTAL HEALTH LINKAGE SYSTEM PROJECT; PARTICIPANTS ARE ENROLLED IN A TREATMENT PROGRAM. IF CONTACT IS MADE WITH THE PARTICIPANT, CALL (Linkage Specialist’s phone number given here).” Third, the officer can, in real time, call the “Linkage Specialist” (a licensed mental health professional at the community mental health agency) to receive brief telephonic assistance, thinking through observed behaviors and potential dispositions (for a more detailed description of the Linkage System, see the Part I companion article on acceptability). The goal is for the officer on the scene to speak with a Linkage Specialist at the community mental health agency who can raise awareness of any mental health concerns and help re-connect the patient to mental health care, potentially averting unnecessary misdemeanor arrests when appropriate.
Our project was designed as a feasibility study in advance of a larger effectiveness study. It focused on all implementation processes to ensure that recruitment, enrollment into the database, and telephonic connection between officers and the Linkage Specialist all run smoothly, and to estimate important parameters that are needed to design a fully powered study, such as willingness of clinicians to refer participants, willingness of participants to be randomized, number of hits to the database, number of calls to the Linkage Specialist, and arrest rates. Feasibility studies do not formally test the outcome of interest (Arain, Campbell, Cooper, & Lancaster, 2010). The Part I companion article addresses acceptability of the linkage system via focus groups involving patients, officers, and others; the aim of this study was to assess feasibility of implementation and to answer the nine a priori questions listed in Table 1.
Table 1.
Nine Feasibility Questions Answered by the Study
| 1. After engaging outpatient referral sites and informing referring clinicians of eligibility criteria, how many patients must be referred in order to reach the target sample? What proportion of referred patients meet eligibility criteria? |
| 2. What proportion of eligible patients opt into the linkage system? |
| 3. What proportion of patients not opting into the linkage system do so because: (a) they do not want their name placed into the registry in the criminal justice information system; (b) they do not want the researchers to collect arrest data from the criminal justice information system; or (c) other reasons (to be specified)? |
| 4. Among patients enrolling into the linkage system, what proportion state that they would also be willing to enroll in the context of a hypothetical, blinded, randomized trial (such that they would not know whether or not their name had been placed into the linkage system database)? |
| 5. How many hits are received to the database during the course of the study period (specifically, 200 patients enrolled for 12 months each)? |
| 6. How many calls does the Linkage Specialist receive from police officers during the course of the study period (again, 200 patients enrolled for 12 months each)? |
| 7. Among the calls received, in what proportion does a discretionary arrest appear to have been averted? |
| 8. In what number/proportion of participants can administrative data not be accessed from the state criminal justice information center? |
| 9. Using administrative criminal justice data, what is an estimated effect size of the linkage system, when comparing patients’ arrests in the pre-intervention year and the intervention year? |
Methods
Sample and Setting
The eligibility criteria for patients with serious mental illnesses included: (1) able to speak/read English; (2) age 18–65 years; (3) clinical diagnosis of a psychotic or mood disorder (with or without comorbidities) based on referring clinician report; (4) history of at least one prior arrest within the past five years; (5) not enrolled in any other research projects; (6) free of known/suspected intellectual disability or dementia; and (7) able to give informed consent and sign the special Health Insurance Portability and Accountability Act of 1996 (HIPAA) consent document for the police–mental health linkage system and the associated research, as assessed during the in-depth, Institutional Review Board-approved consent process.
The feasibility study took place at one of Georgia’s community service boards (CSBs), which are 26 quasi-governmental mental health agencies that serve as the safety net for the provision of mental health services across the state. Established in 1994 as a public and non-profit organization, Gateway Community Service Board (dba Gateway Behavioral Health and called Gateway herein) is the largest facility specializing in care for individuals with serious mental illnesses in Georgia’s coastal region, including Savannah and Chatham County, as well as seven other coastal counties. Gateway serves more than 9,000 people annually, is certified by the Georgia Department of Behavioral Health and Developmental Disabilities, and is accredited by CARF (Commission on Accreditation of Rehabilitation Facilities). Savannah Counseling Services serves Chatham County and is a subsidiary of Gateway providing adult mental health treatment, adult day rehabilitation services, individualized supported employment, outpatient clinic, and intensive family interventions.
General Procedures
Patients were referred by Gateway clinicians to the research team. Once referred, a research assistant met with the patient, often immediately at the time of referral, to complete a screening form with the patient. If found eligible, the research assistant described the project to the patient, and for those interested, a detailed informed consent process was followed. If the patient chose to not enroll in the study, he or she was offered the chance to participate in a focus group to understand reasons they declined the linkage system. Patients were offered the same amount of monetary compensation for that focus group as those who enrolled in the study. (However, as described in the Part I companion article on acceptability, too few patients declined the linkage system to assemble a focus group.) For those choosing to enroll, once the informed consent was signed, the research assistant completed the demographics sheet and collected other basic data, and then entered the necessary demographic information into a specially designed database developed and maintained by the Georgia Crime Information Center (GCIC, which is part of the Georgia Bureau of Investigation, the state’s lead law enforcement agency). Patients were removed from the database after exactly 12 months. At that point, the GCIC provided the participant’s rap (record of arrests and prosecutions) sheet, from which information on all fingerprintable arrests in the past two years was extracted.
Statistical Analyses
Preliminary quantitative data to derive an estimate of effect size, and thus sample size to adequately power a larger study, were analyzed by comparing the number of arrests per participant in the year before and the year during linkage system involvement. We also determined the number of hits to the database that resulted in a call to the Linkage Specialist, and categorized those that led to arrest or to successful linkage with mental health services, based on interviews with the Linkage Specialist immediately after each call.
Results
From March 18th, 2014, to September 9th, 2015, 349 individuals were referred. The mean referral rate was 4.5±5.0 per week, with a minimum of 0, a maximum of 19, and a median of 3 per week. Of 349 individuals referred, 129 (37.0%) did not meet eligibility criteria. The main reasons to be screened out included not having a history of at least one arrest in the past five years (71.3%) and not having a primary psychotic or mood disorder (16.3%). Fourteen subjects declined to be screened for the study, showing hesitant behavior (e.g., not showing up for the screening appointment, asking for time to think about taking part in the study). Of the 206 eligible and interested individuals, 199 (96.6%) opted into the linkage system; three people did not consent because they did not want their name and other identifying information in the database in the criminal justice information system, and four had other reasons (e.g., individual was sure that there would never be police contact again). None of the individuals expressed concerns about researchers collecting arrest data from the criminal justice information system. Sociodemographic and clinical characteristic of the enrolled sample are shown in Table 2.
Table 2.
Sociodemographic and Clinical Characteristic of the Sample Enrolled (N=199)
| Mean | SD | |
|---|---|---|
| Age, in years | 40.0 | 11.3 |
| How long they have been receiving services, in months | 45.2 | 63.4 |
| N | % | |
| Gender, male | 108 | 54.3 |
| Race | ||
| African American | 122 | 61.3 |
| Caucasian | 71 | 35.7 |
| Other | 6 | 3.0 |
| Marital Status | ||
| Single and never married | 107 | 53.8 |
| Divorced | 46 | 23.1 |
| Married or living with a partner | 20 | 10.1 |
| Separated | 18 | 9.0 |
| Widowed | 8 | 4.0 |
| Education | ||
| Less than 7 years of school | 4 | 2.0 |
| Junior high | 19 | 9.5 |
| Some high school | 68 | 34.2 |
| Some college or trade vocational school | 46 | 23.1 |
| General education diploma | 35 | 17.6 |
| High school graduate | 22 | 11.1 |
| College graduate | 4 | 2.0 |
| Completed graduate or professional school | 1 | 0.5 |
| Has one or more children | 142 | 71.4 |
| Diagnosis (n=197) | ||
| Schizophrenia or Other Psychotic Disorder | 78 | 39.6 |
| Bipolar Disorder | 64 | 32.5 |
| Depressive Disorder | 52 | 26.4 |
| Other disorders | 3 | 1.5 |
During the study, three participants withdrew their consent to be in the linkage system and were thus removed from the database. Specifically, one withdrew because she no longer wanted to be a part of the study, having only signed up for the reimbursement; another thought that it could somehow keep her from gaining visitation rights to her boyfriend in prison (which would not have been the case); and another did not give specific reasons but believed that it could do more harm than good. Among the 199 patients enrolling into the linkage system, 184 (92.5%) reported that they would also have been willing to enroll in the context of a hypothetical, blinded, randomized, trial.
The linkage system database received a total of 679 hits during the study period, with a mean monthly rate of 27.2±13.1, a minimum of 2, and a maximum 52. The vast majority of inquiries were from law enforcement agencies (either directly from officers, or by the 911 call center on behalf of the officer), though some were from court. A driver’s license or state identification query was the main reason the system was hit, followed by wanted person, criminal history, and driver’s history (Figure 1). The month the system was hit at the highest rate was December 2014, with 39 hits for 96 participants entered in the system at that time (ratio=0.40 hits/participant). The mean of the monthly rate of hits per participant was 0.26±0.09 hits/participant.
Figure 1.
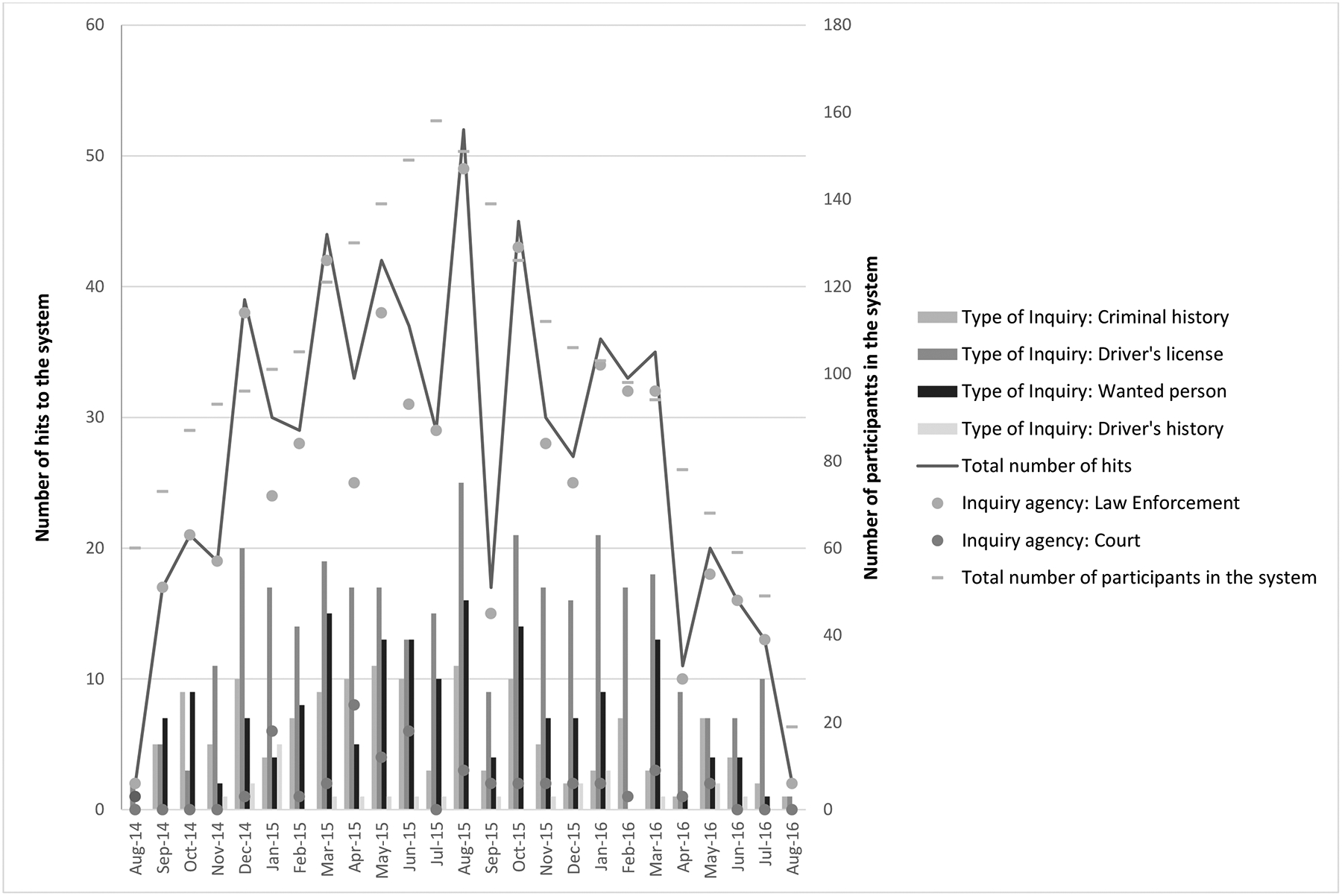
Number and Types of Hits to the Database, and Number of Enrolled Participants, during the Study Period
During the course of the study period, the Linkage Specialist received 31 calls. Among those, in at least three cases, an arrest was likely averted, in three cases an arrest was made aside from any information given by the Linkage Specialist, and in 10 cases an arrest was not being considered.
Administrative data from rap sheets were accessible for all participants. In the year before enrolling in the study, 77 (38.7%) patients had experienced at least one arrest. During the year in the linkage system 61 (30.7%) were arrested. Thirty-three (16.6%) participants were arrested both in the year prior to enrollment and during enrollment in the linkage system. The mean number of arrests across the 199 study participants was 0.59±0.92 in the year before enrollment, and 0.48±0.83 during the course of the study. This difference (paired t=1.569, df=198, p=0.118), indicates a potential effect of the intervention. The associated Cohen’s d effect size was 0.13.
Discussion
A major. ongoing problem pertaining to mental health services is the lack of coordination and communication between the mental health and criminal justice systems, resulting in individuals with serious mental illnesses commonly being arrested and incarcerated when re-connection with treatment would be more helpful. What often becomes a cycle is both expensive monetarily as well as for the livelihood and recovery of this population. One of the several models of collaboration between law enforcement and mental health is the Crisis Intervention Team (CIT) model, which is a specialized police-based program intended to enhance officers’ interactions with individuals with mental illnesses and improve the safety of all parties involved. Trained officers serve as specialized front-line responders who are better informed to redirect individuals with mental health concerns, when appropriate, to treatment services instead of the judicial system. Compton and colleagues (2008) performed a review to provide a systematic summary and critical analysis of the available research conducted on CIT; see also Watson et al., 2017. Despite the limited (though ongoing) available research, the CIT model may be an effective component in connecting individuals with mental illnesses who come to the attention of police officers with appropriate mental health services. Our linkage system is in no way intended to replace CIT, but tries to also address the aforementioned problems in order to decrease criminalization and provide appropriate services for these individuals by improving communication between police officers and mental health professionals. This tool, if proven effective, could potentially benefit both CIT-trained and non-CIT officers and does not require officers to complete the 40-hour training that is part of CIT in order for them to access potentially helpful information.
In advance of a larger effectiveness study, we have evidence for the feasibility of our new linkage system. Several authors have reviewed the features of feasibility studies, and have advised on the issues that should be addressed (Arain et al., 2010; Shanyinde, Pickering, & Weatherall, 2011). Thabane et al. (2010) reported four reasons to conduct a feasibility study.
Feasibility of processes. We looked at whether mental health providers would be willing to refer patients, and whether these patients would be willing to consent to participate. As expected, we had a high number of referrals due to the providers’ high level of engagement and interest in the linkage system. Only approximately 6% of people approached for the study did not want to participate, and only three people decided to withdraw from the study. A high percentage of participants reported being willing to participate even in the context of a hypothetical randomized, blinded trial.
Time and resource problems. We selected as our Linkage Specialist a social worker within the community mental health agency who was available 24/7, even when mental health clinics were closed, to assist the police in interactions involving someone who is diagnosed with a mental illness. The telephone number the police dialed went directly to the Linkage Specialist who could offer information and assistance in real time. The database received hits, and the police contacted the Linkage Specialist, who was then able to assist the officers by educating them, connecting them to the appropriate mental health services, and in some cases potentially facilitating the avoidance of an arrest and thus criminal charges and a possible detention.
Potential human and data management problems. During the testing of feasibility, we found no evidence of harm. Specific administrative data about arrests were available and provided for all of the participants, and data management processes were worked out in advance of a larger trial.
Scientific issues including the assessment of treatment safety, dose, response effects, and variance of the effect. We have preliminary data that arrests were diverted and some participants were reconnected with mental health services. We did not identify any safety problems.
We acknowledge several methodological limitations. First, the confined geographic area of the study could limit generalizability; a future study should be extended to a wider area, allowing assessment of the linkage system in different contexts (e.g., both rural and urban). Second, the study focused on those with serious mental illnesses, and as such, did not target other critical populations with frequent police contacts who might also benefit from such a system, including individuals with intellectual disabilities and those with dementia. Additionally, patients with mild intellectual disability in addition to a psychotic or mood disorder would have been excluded based on our eligibility criteria; yet, they may be the most vulnerable group of all, and they interact with police on a frequent basis. By excluding them from the study, we may have potentially underestimated the true effect of the intervention for the community. Future studies should consider including this group and respective legal guardians. Third, comorbid substance use undoubtedly impacts the interaction with police officers; their willingness to make use of the Linkage Specialist when interacting with acutely intoxicated individuals (and any effect on the likelihood of arrest or diversion) should be addressed in future studies. Fourth, in a future study, it might also be important to maintain a full focus on engagement of both law enforcement and Linkage Specialists due to periods in which the Linkage Specialist was not contacted on a regular base and thus could become disengaged.
Conclusion
The linkage system could benefit both the mental health community and law enforcement. It is imperative for these groups to collaborate to ensure that individuals with mental illnesses receive the services they need to advance their recovery and to minimize criminal justice entanglement. In this feasibility study, we observed a signal of the potential effectiveness of the linkage system in reducing the number of incarcerations in the year of enrollment in the system, compared to the previous year. A next step might be a controlled trial to measure the effectiveness of the linkage system in preventing incarceration and facilitating re-connection with mental health services. One might postulate that the costs would be relatively low in comparison to other forms of jail diversion (with most costs pertaining to the enrolling of patients into the statewide database, as well as supporting the work of the Linkage Specialist); this would need to be studied because scalability and uptake hinges in part on both effectiveness and cost-effectiveness.
Acknowledgements:
Research reported in this publication was supported by National Institute of Mental Health grant R34 MH099268 (“A Novel Police-Mental Health Linkage System to Promote Pre-Booking Jail Diversion”) to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Institute of Mental Health. The research team members extend their gratitude to Vernon Keenan (Georgia Bureau of Investigation); Nora Haynes (National Alliance on Mental Illness, Georgia Affiliate); David Crews, Amanda Tillman, Thomas Ward, Nina Kennedy, Chris Williams, and the many supportive clinicians and staff at Gateway Behavioral Health Services in Savannah, Georgia.
References
- Allen SA, Wakeman SE, Cohen RL, & Rich JD (2010). Physicians in US Prisons in the Era of Mass Incarceration. International journal of prisoner health, 6(3), 100–106. [PMC free article] [PubMed] [Google Scholar]
- Arain M, Campbell MJ, Cooper CL, & Lancaster GA (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol, 10, 67. doi: 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Bahora M, Watson AC, & Oliva JR (2008). A Comprehensive Review of Extant Research on Crisis Intervention Team (CIT) Programs. Journal of American Academy of Psychiatry Law, 36(1), 47–55. [PubMed] [Google Scholar]
- Compton MT, Roger Bakeman M, Broussard B, Dana Hankerson-Dyson M, Letheshia Husbands M, Shaily Krishan B, Tarianna Stewart-Hutto M, D’Orio BM, Oliva JR, Thompson NJ, & Watsonm AC (2014). The Police-Based Crisis Intervention Team (CIT) Model: I. Effects on Officers’ Knowledge, Attitudes, and Skills. Psychiatric Services, 65(4), 517–522. doi: 10.1176/appi.ps.201300107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditton PM (1999). Special report: Mental health and treatment of inmates and probationers. Washington, DC: US Department of Justice, Bureau of Justice Statistics. [Google Scholar]
- Draine J, Blank Wilson A, Metraux S, Hadley T, & Evans AC (2010). The impact of mental illness status on the length of jail detention and the legal mechanism of jail release. Psychiatric Services, 61(5), 458–462. doi: 10.1176/ps.2010.61.5.458 [DOI] [PubMed] [Google Scholar]
- James DJ, & Glaze LE (2006). Highlights mental health problems of prison and jail inmates.
- Lamb HR, Weinberger LE, & Gross BH (2004). Mentally ill persons in the criminal justice system: Some perspectives. Psychiatric Quarterly (Vol. 75, pp. 107–126). doi: 10.1023/B:PSAQ.0000019753.63627.2c [DOI] [PubMed] [Google Scholar]
- Munetz MR, & Griffin PA (2006). Use of the Sequential Intercept Model as an approach to decriminalization of people with serious mental illness. Psychiatric Services, 57(4), 544–549. doi: 10.1176/ps.2006.57.4.544 [DOI] [PubMed] [Google Scholar]
- Shanyinde M, Pickering RM, & Weatherall M (2011). Questions asked and answered in pilot and feasibility randomized controlled trials. BMC Med Res Methodol, 11(1), 117. doi: 10.1186/1471-2288-11-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, et al. (2010). A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol, 10(August 2016), 1. doi: 10.1186/1471-2288-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrey EF (2012). The Insanity Offense: How America’s Failure to Treat the Seriously Mentally Ill Endangers Its Citizens. WW Norton & Company. [Google Scholar]
- Watson et al. , 2017, under review for the current Special Issue of Behavioral Sciences & the Law.
- Wells W, & Schafer JA (2006). Officer perceptions of police responses to persons with a mental illness. Policing, 29(4), 578–601. doi: 10.1108/13639510610711556 [DOI] [Google Scholar]


