Abstract
Introduction:
Foreign body aspiration (FBA) is a common, life-threatening pediatric emergency and was shown to be associated with high risk of morbidity and mortality. This systematic review and meta-analysis aimed to investigate the diagnostic value of chest computed tomography (CT) scan for identification of FBA in children.
Methods:
From inception to May 2024, a systematic search was carried out across multiple databases including Medline, Scopus, and Web of Science, considering published papers in English language. Quality assessment of the included studies was performed using seven domains of Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2).
Results:
The systematic literature search yielded 7203 articles. The pooled sensitivity and specificity of chest CT scan for identification of FBA were 0.99 (95% CI: 0.98-0.99) and 0.97 (95% CI: 0.96-0.98), respectively. The pooled positive likelihood ratio was 10.12 (95% CI: 4.59-22.20), and pooled negative likelihood ratio was 0.05 (95% CI: 0.02-0.1). Furthermore, the area under the summarized receiver operating characteristic (SROC) curve was 0.98.
Conclusion:
Our meta-analysis revealed that despite high heterogeneity, in the diagnostic characteristics of chest CT scan among studies, it has high diagnostic value in identifying FBA in suspected pediatric cases.
Key Words: Respiratory aspiration, Foreign bodies, Meta-analysis, Pediatrics, Respiratory aspiration, Tomography, X-ray computed
1. Introduction:
Foreign body aspiration (FBA) is a common, life-threatening pediatric emergency, which was shown to be associated with a high risk of morbidity and mortality in the pediatric population. Suffocation due to FBA was reported as the fourth most frequent cause of death by unintentional injury in pediatrics in the United Sates (1, 2). If there is no history pointing to aspiration, diagnosis of airway FBA in children can be considerably challenging. Early diagnosis and intervention for FBA play a pivotal role in reducing the mortality and complications. Clinical symptoms and signs of FBA are associated with different factors such as age, duration of FBA, location of foreign body in tracheobronchial tree, morphological characteristics of the foreign body, and the occupied area of the airway (3-5). Since 18-76% of children with confirmed diagnosis of FBA have negative history of aspiration, these cases may be misdiagnosed as other respiratory diseases such as bronchiectasis, pneumonia, asthma, and bronchitis (3, 4). Airway bronchoscopy as the gold standard, chest computed tomography (CT), and chest radiography are frequently used for diagnosis of FBA in children (6). Although chest radiography is used for evaluation of FBA, its main diagnostic value is for the radiopaque foreign bodies, and its accuracy for radiolucent foreign bodies is controversial (7, 8). Localization and removal of foreign bodies can be conducted by bronchoscopy, but it has some complications such as laryngeal edema, bronchial injuries, cardiac arrest, hypoxia, bronchospasm, and also complications related to anesthesia (9-12). For several years, multi-detect CT (MDCT) scan with 3D images and multiplanar reconstruction could be used to determine the location and size of foreign bodies in tracheobronchial tree, and subsequently reduce the rate of negative bronchoscopy and time of bronchoscopy (13). Many original studies have investigated the diagnostic value of chest CT for identification of FBA in pediatric populations. The reported sensitivity and specificity of previous studies demonstrated a wide range of values, indicating significant variability across different studies (6, 8, 14-26). Therefore, in this systematic review and meta-analysis, we aimed to investigate the overall diagnostic value of chest CT for identification of FBA in children.
2. Methods:
2.1 Study design and setting
We performed this diagnostic meta-analysis according to the Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies (PRISMA-DTA). From inception to May 2024, a systematic search was carried out across multiple databases including Medline, Scopus, and Web of Science, considering published papers in English language.
2.2 Search strategy
The search question was formulated based on the PECO framework:
Population: Children suspected of having FBA;
Exposure: Chest CT scan;
Comparison: Comparing with a valid gold standard such as bronchoscopy;
Outcome: Diagnostic accuracy of chest CT in identifying FBA.
This comprehensive search incorporated an array of MeSH Terms, keywords, and synonyms: [“CT” OR “Computed Tomography” OR “Multidetector Computed Tomography” OR “Computed Assisted Tomography” OR “CAT Scan” OR “Tomography” OR “Virtual Bronchoscopy”] AND [“Foreign Body” OR “Foreign Bodies” OR “Aspiration” OR “Foreign Body Aspiration” OR “Inhalation” OR “Airway Obstruction” OR “Respiratory Aspiration”] AND [“Child” OR “Children” OR “Pediatric” OR “Infant” OR “Adolescent”].
2.3 Selection criteria
Data of original studies meeting the following inclusion criteria were used: 1) studies using chest CT scan for diagnosis of FBA; 2) a valid gold standard was reported for final diagnosis of FBA; 3) true positive (TP), false positive (FP), true negative (TN), and false negative (FN) were reported or a 2×2 contingency table can be formed according to the reported data; 4) subjects were children suspected of having FBA. Exclusions pertained to duplicate studies, papers with unextractable data, case reports, cases series with less than 10 subjects, editorials, reviews, animal and cadaver studies, and conference abstracts. Systematic search and evaluating the studies with respect to the inclusion and exclusion criteria were carried out by two independent researchers and any disagreements were resolved through discussion or by consultation with a third researcher.
2.4 Data extraction
Similarly, data extraction was conducted by two independent authors, and in case of controversy, a third author determined the final data to be included in the qualitative and quantitative analyses. The data included in the literature extraction include the name of first author, publication year, study design, mean age, male/female ratio, TP, FP, TN, and FN.
2. 5 Risk of bias assessment
Quality assessment of the included studies was performed using seven domains of Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool.
2.6 Statistical analysis
Statistical analysis of diagnostic value was performed using meta-Disc software version 1.4 (Ramona Cajal Hospital, Madrid, Spain) and Stata statistical software package (Stata Corp., College Station, TX, USA) (version 17.0). Heterogeneity across the included studies was assessed using the Cochrane Q test and I-squared (I2) statistics. If P-value of Q-test was less than 0.05 or I2 was higher than 50%, the estimation of pooled variables was performed using a random-effects model. Otherwise, if P-value of Q-test was higher than 0.05 and I2 was less than 50%, the data were analyzed in a fixed-effects model. Egger’s test and funnel plot were used to investigate publication bias. We performed sensitivity analysis using leave-one-out method.
3. Results:
3.1 Study selection and characteristics
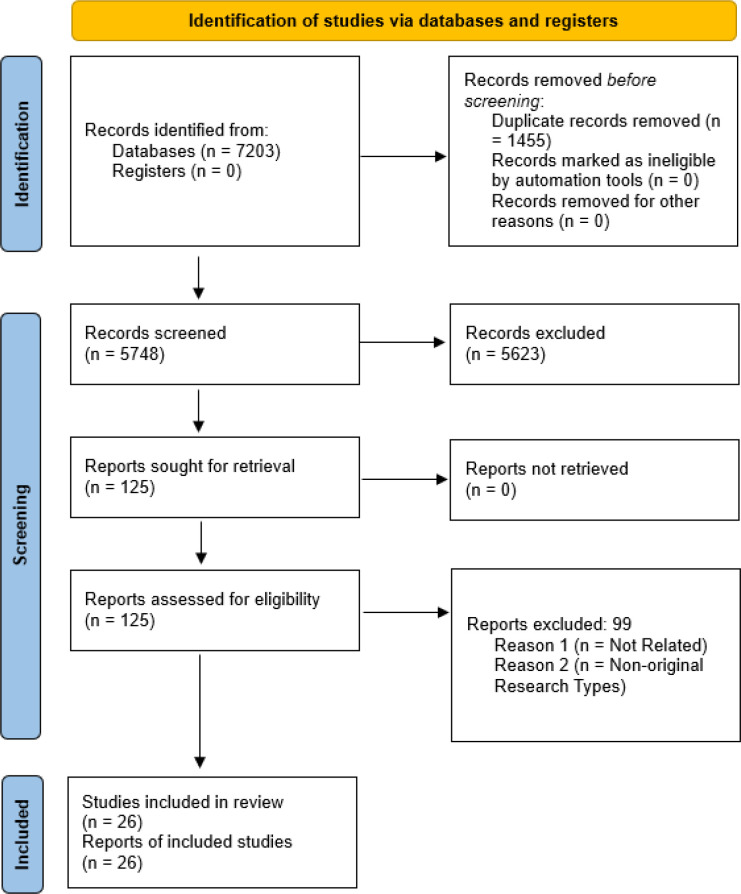
The systematic literature search yielded 7203 articles. Among them, 1455 duplicated papers were excluded, and another 5623 articles were removed through a primary process of title and abstract review. The full-text assessment of the remaining 125 papers identified 26 eligible articles with 4554 participants reporting mean ages ranging from 1.1 to 4.3 years for inclusion in our systematic review and meta-analysis. Figure 1 shows PRISMA flowchart of the literature search and selection of studies that had evaluated the accuracy of chest CT scan for the diagnosis of FBA. Among the included studies, 15 were retrospective studies, 10 were prospective studies, and one was a retrospective and prospective cross-sectional study. Table 1 summarizes the characteristics of the included studies.
Figure 1.
Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) flowchart of the literature search and selection of studies that evaluated accuracy of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA).
Table 1.
Characteristics of the included studies
| Authors | Year | Study Design | Age 1 | Sex 2 | No. 3 | TP | FP | FN | TN |
|---|---|---|---|---|---|---|---|---|---|
| Truong et al. (24) | 2023 | Retrospective | 2.74 | 1.63 | 25 | 10 | 2 | 0 | 13 |
| Shen et al. (23) | 2020 | Retrospective | 3 | 2 | 382 | 359 | 0 | 23 | 0 |
| Gordon et al. (31) | 2020 | Retrospective | NR | NR | 62 | 9 | 1 | 0 | 52 |
| Ullal et al. (25) | 2019 | Retrospective and Prospective | 2.1 | 4 | 150 | 139 | 4 | 3 | 4 |
| Arora et al. (32) | 2019 | Retrospective | 4.3 | 2.8 | 19 | 9 | 0 | 2 | 8 |
| Gibbons et al. (33) | 2019 | Retrospective | 1.8 | 1.3 | 69 | 17 | 1 | 0 | 51 |
| Ahmed et al. (34) | 2018 | Retrospective | 3.06 | 1.9 | 15 | 10 | 0 | 1 | 4 |
| Pitiot et al. (21) | 2017 | Retrospective | NR | NR | 96 | 59 | 9 | 1 | 27 |
| Friedman et al. (35) | 2016 | Retrospective | 6 | 0.8 | 20 | 4 | 0 | 0 | 16 |
| Liang et al. (20) | 2015 | Retrospective | 2 | 1.7 | 1500 | 1480 | 0 | 20 | 0 |
| Yang et al. (26) | 2015 | Retrospective | 2 | 2.2 | 1501 | 589 | 1 | 1 | 910 |
| Behera et al. (5) | 2014 | Retrospective | 2 | 2.3 | 60 | 59 | 1 | 0 | 0 |
| Abd-Elgawad et al. (36) | 2014 | Prospective | 3 | 1.6 | 21 | 16 | 1 | 1 | 3 |
| Tong et al. (8) | 2013 | Prospective | 2.4 | 1.3 | 37 | 33 | 1 | 0 | 3 |
| Hassan et al. (37) | 2013 | Prospective | 2.5 | 0.75 | 8 | 3 | 1 | 0 | 4 |
| Manach et al. (38) | 2013 | Prospective | 2.5 | 1.8 | 303 | 66 | 10 | 4 | 223 |
| Jung et al. (17) | 2011 | Retrospective | 1.5 | 1 | 10 | 10 | 0 | 0 | 0 |
| Bai et al. (39) | 2011 | Retrospective | 3.2 | 1.6 | 45 | 42 | 0 | 0 | 3 |
| Sattar et al. (22) | 2011 | Retrospective | 4 | 1.3 | 45 | 42 | 0 | 0 | 3 |
| Bhat et al. (40) | 2010 | Prospective | 3.3 | 0.5 | 20 | 12 | 1 | 1 | 6 |
| Huang et al. (16) | 2008 | Retrospective | 2.1 | 4.5 | 11 | 11 | 0 | 0 | 0 |
| Hong et al. (15) | 2008 | Prospective | 1.1 | 1.4 | 51 | 42 | 3 | 0 | 6 |
| Adaletli et al. (41) | 2007 | Prospective | 2.6 | 1.2 | 37 | 13 | 3 | 0 | 21 |
| Kocaoglu et al. (18) | 2006 | Prospective | 3.5 | 2 | 21 | 8 | 1 | 1 | 11 |
| Koşucu et al. (19) | 2004 | Prospective | 3.3 | 1.3 | 23 | 15 | 0 | 0 | 8 |
| Haliloglu et al. (14) | 2003 | Prospective | 2.4 | 0.9 | 23 | 7 | 0 | 0 | 16 |
True positive (TP), false positive (FP), true negative (TN), and false negative (FN). 1: mean age in year; 2: male/female ratio; 3: number of participants.
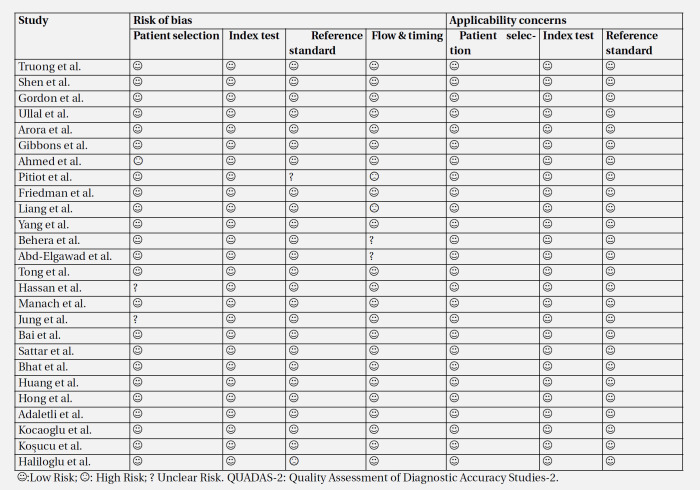
3.2 Quality assessment and publication bias
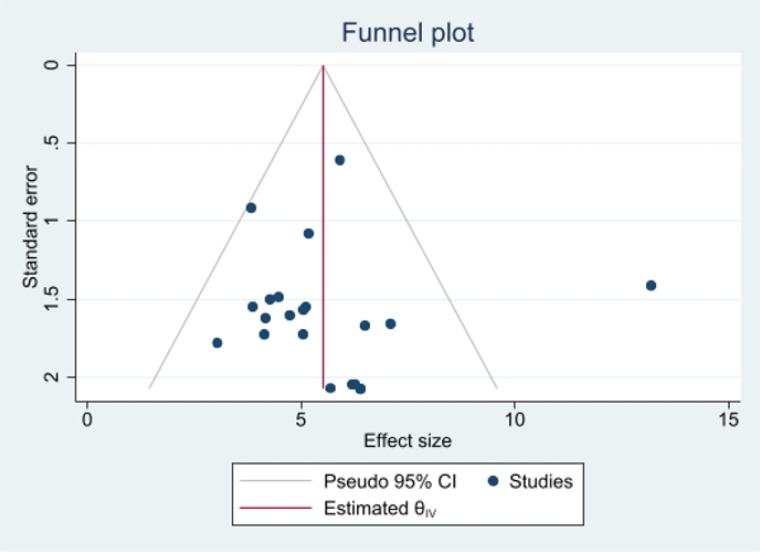
Overall, in terms of index test and applicability concerns, a low risk of bias was identified in the majority of included studies. The bias risk of two enrolled studies for flow and timing was judged as high. One study was at a high risk of bias for reference standard as the reference standard results were interpreted with knowledge of the results of the index test. The results of the QUADAS-2 regarding quality assessment of the included studies are summarized in table 2. Begg’s test and Egger’s test showed no significant publication bias (P=0.33 and P=0.85; respectively). Similarly, funnel plot revealed no publication bias (Figure 2).
Table 2.
Quality assessment of the included studies using QUADAS-2 tool
Figure 2.
Funnel plot of publication bias on the pooled diagnostic odds ratio (DOR) of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
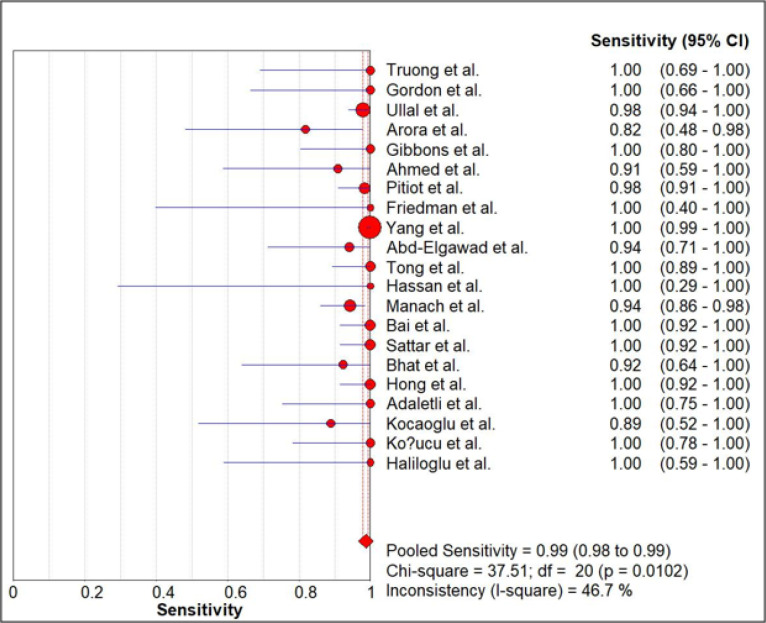
3.3 Diagnostic value of chest CT scan
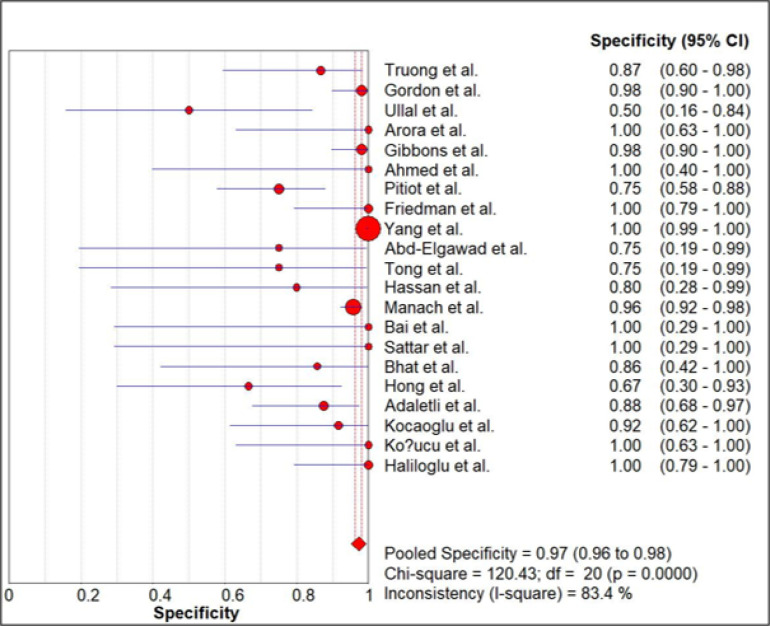
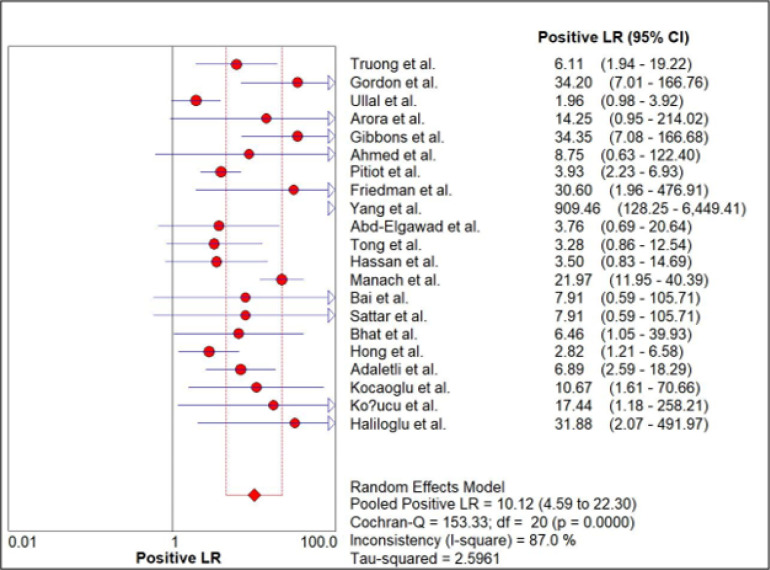
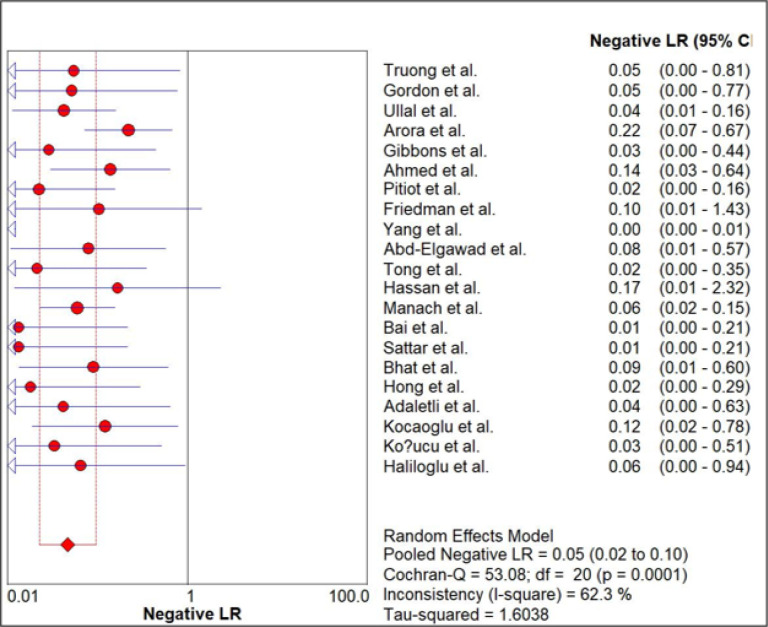
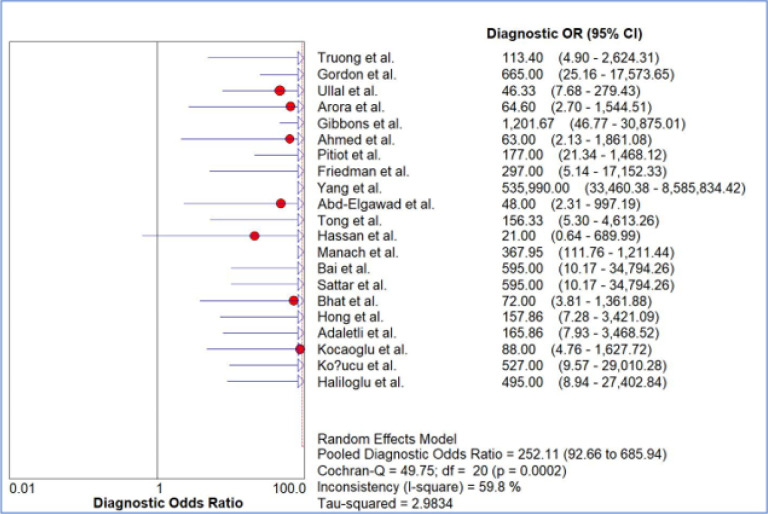
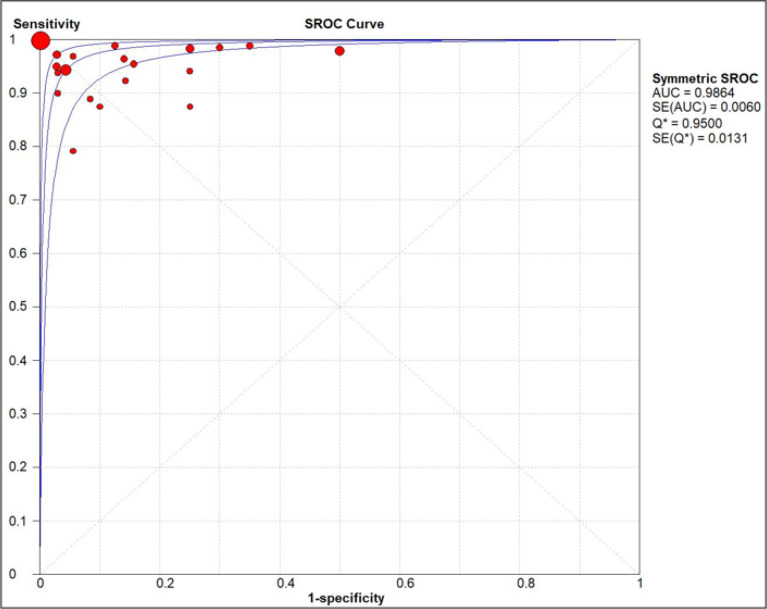
The pooled sensitivity and specificity of chest CT scan for identification of FBA in children were 0.99 (95% CI: 0.98-0.99) and 0.97 (95% CI: 0.96-0.98), respectively (Figures 3 and 4). The heterogeneity was significant in the pooled analysis of sensitivity (I2=46.7 and P=0.01) and specificity (I2=83.4 and P<0.01). The pooled positive likelihood ratio (PLR) was 10.12 (95% CI: 4.59-22.20) with significant heterogeneity (I2=87 and P<0.01), and pooled negative likelihood ratio (NLR) was 0.05 (95% CI: 0.02-0.1) with significant heterogeneity (I2=62.3 and P<0.01) (Figures 5 and 6). The pooled diagnostic odds ratio (DOR) was 252.11 (95% CI: 92.66-685.94), with significant heterogeneity (I2=59.8 and P<0.01) (Figure 7). Furthermore, the area under the summarized receiver operating characteristic (SROC)curve (AUC) was 0.98 (Figure 8).
Figure 3.
Forest plot of the pooled sensitivity of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
Figure 4.
Forest plot of the pooled specificity of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
Figure 5.
Forest plot of the pooled positive likelihood ratio (LR) of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
Figure 6.
Forest plot of the pooled negative likelihood ratio (LR) of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
Figure 7.
Forest plot of the diagnostic odds ratio (DOR) of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). CI: confidence interval.
Figure 8.
Summary receiver-operating characteristic (SROC) of computed tomography (CT) scan for the diagnosis of foreign body aspiration (FBA). AUC: area under the curve; SE: standard error.
3.4 Sensitivity analysis
Sensitivity analysis using the leave-one-out method showed that excluding each study did not significantly affect the sensitivity, specificity, or accuracy of chest CT scans for FBA. However, the study by Yang et al. (26) slightly reduced the values of sensitivity (0.98; 95% CI: 0.96-0.99), accuracy (0.97), and particularly specificity (0.93; 95%CI: 0.900-0.95).
4. Discussion:
In this systematic review and meta-analysis, we pooled the diagnostic value of chest CT scan for identification of FBA in children. Our results revealed that the sensitivity, specificity, PLR, NLR, and DOR of chest CT scan for FBA are 0.99, 0.97, 10.11, 0.05, and 252.22, respectively. The accuracy of chest CT scan for FBA was excellent (0.98).
In a similar systematic review by Tuckett et al. (6), different databases including Scopus, Web of Knowledge, Medline, and Embase were searched from 1970 to 2013. After evaluation of records with respect to eligibility criteria, the authors included 14 studies. However, they reported diagnostic values of chest CT scan from only eight studies. Their results showed that sensitivity and specificity of chest CT scan for FBA ranged between 90% to 100% and 75% to 100%, respectively. It should be noted that they did not perform meta-analysis; therefore, the pooled results of diagnostic value of chest CT scan were not indicated in their study. A recent similar meta-analysis by Azzi et al. (27) was performed using electronic databases including Web of Science, PubMed Medline, Ovid Medline, and Ovid Embase. They assessed published papers from inception of the database to January 2021. Although a rigorous search strategy was used to identify eligible papers, they found 16 studies for inclusion in the meta-analysis, which was considerably lower than the number of studies included in our meta-analysis. They found a sensitivity of 98.8 and a specificity of 96.6 for chest CT scans, respectively. Our pooled sensitivity and specificity were higher than those reported by Azzi et al., which is likely due to difference in the number of included studies, the quality of chest CT scans, variations in included subjects, and differences in inclusion and exclusion criteria of the studies.
Our meta-analysis showed that chest CT scan can effectively diagnose FBA in children, but negative effects of radiation exposure in pediatric cases and its role in cumulative received dosages of radiation over an individual’s lifetime was not noted in the results. A cohort study on 10.9 million people in Australia revealed that overall cancer incidence is 24% higher in patients with history of exposure to CT radiation than unexposed cases (28). Furthermore, it was shown that increased risk of cancer following CT scan is dose-dependent and incidence rate ratio increases by 0.16 after each further CT scan. Therefore, the high accuracy of CT scan for diagnosis of FBA must be weighed against its potential carcinogenic effects before deciding to use it for diagnosis in pediatric cases. Another point to consider is that CT scans usually require sedation in pediatric cases, which is commonly associated with respiratory complications that can affect the diagnosis of FBA, including upper airway obstruction, aspiration, cardiorespiratory depression, hypoxia, hypoventilation, and hypotension (29). Moreover, routine evaluation of suspected pediatric cases of FBA using CT scan does not seem to be cost-effective (30).
In our study, we found significant heterogeneity among the studies with respect to sensitivity, specificity, PLR, NLR, and DOR. Although the majority of included studies did not report the main variables required for meta-regression, these heterogeneities may, in part, be clarified by differences between the included studies. For instance, the dosage of radiation and the types of devices used for conducting CT scans varied among studies, potentially contributing to the observed heterogeneity. Furthermore, another possible source of heterogeneity could be the differences between studies in the use of sedation before chest CT scans. The experience level of the interpreters of CT scans and the different inclusion criteria for pediatric cases can also contribute to the heterogeneity among the included studies. In addition, variations in study design, population characteristics, and methodologies further explain the heterogeneity among the results. These factors underscore the complexity and variability inherent in the studies using CT scans for diagnosis, suggesting the need for standardized protocols in future studies to reduce such heterogeneities.
5. Limitations
Our meta-analysis was subject to several limitations. First, the diversity of inclusion criteria and characteristics of the subjects posed significant heterogeneity and challenges to extrapolating the findings to the overall population of susceptible pediatric cases of FBA. Second, some subgroups lacked the sufficient number of papers to able conduct meta-regressions, limiting the generalizability of our findings. Therefore, it is necessary to interpret the results of our study with caution.
6. Conclusion:
Our meta-analysis revealed that, despite high heterogeneity in the diagnostic value of CT scan among studies, CT scan has high diagnostic performance in identifying FBA in suspected pediatric cases. Therefore, CT scan can be used for diagnosing FBA, particularly in settings that do not have access to bronchoscopy, to improve decision-making and management of these cases.
7. Declarations:
7.1 Acknowledgement
The authors thank all those who contributed to this study.
7.2 Author contribution
All authors contributed to study design, data collection, and writing the draft of the study. All authors read and approved final version of manuscript.
7.3 Funding/support
None.
7.4 Conflict of interest
None.
7.5 Data availability
Not applicable.
7.6 Using artificial intelligence chatbots
None.
References
- 1.El Khoury P, Makhoul M, El Hadi C, Haber C, Rassi S. CT Scan in Children Suspected of Foreign Body Aspiration: A Systematic Review and Meta‐analysis. Otolaryngol Head Neck Surg. 2024;170(1):1–12. doi: 10.1002/ohn.433. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Web‐based Injury Statistics Query and Reporting System (WISQARS): leading causes of death reports, 1981−2020. 2020. [Available from: https://wisqars.cdc.gov/fatal-leading.
- 3.Kaur K, Sonkhya N, Bapna A. Foreign bodies in the tracheobronchial tree: A prospective study of fifty cases. Indian J Otolaryngol Head Neck Surg. 2002;54(1):30–4. doi: 10.1007/BF02911002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schimpl G, Weber G, Haberlik A, Höllwarth M. Foreign body aspiration in children The advantages of emergency endoscopy and foreign body removal. Anaesthesist. 1991;40(9):479–82. [PubMed] [Google Scholar]
- 5.Behera G, Tripathy N, Maru Y, Mundra R, Gupta Y, Lodha M. Role of virtual bronchoscopy in children with a vegetable foreign body in the tracheobronchial tree. J Laryngol Otol. 2014;128(12):1078–83. doi: 10.1017/S0022215114002837. [DOI] [PubMed] [Google Scholar]
- 6.Tuckett P, Cervin A. Reducing the number of rigid bronchoscopies performed in suspected foreign body aspiration cases via the use of chest computed tomography: is it safe? A literature review. J Laryngol Otol. 2015;129(S1):S1–S7. doi: 10.1017/S0022215114002862. [DOI] [PubMed] [Google Scholar]
- 7.Svedström E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol. 1989;19(8):520–2. doi: 10.1007/BF02389562. [DOI] [PubMed] [Google Scholar]
- 8.Tong B, Zhang L, Fang R, Sha Y, Chi F. 3D images based on MDCT in evaluation of patients with suspected foreign body aspiration. Eur Arch Otorhinolaryngol. 2013;270(3):1001–7. doi: 10.1007/s00405-012-2279-x. [DOI] [PubMed] [Google Scholar]
- 9.Hasdiraz L, Oguzkaya F, Bilgin M, Bicer C. Complications of bronchoscopy for foreign body removal: experience in 1035 cases. Ann Saudi Med. 2006;26(4):283–7. doi: 10.5144/0256-4947.2006.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen L-h, Zhang X, Li S-q, Liu Y-q, Zhang T-y, Wu J-z. The risk factors for hypoxemia in children younger than 5 years old undergoing rigid bronchoscopy for foreign body removal. Anesth Analg. 2009;109(4):1079–84. doi: 10.1213/ane.0b013e3181b12cb5. [DOI] [PubMed] [Google Scholar]
- 11.Brkić F, Delibegović-Dedić S, Hajdarović D. Bronchoscopic removal of foreign bodies from children in Bosnia and Herzegovina: experience with 230 patients. Int J Pediatr Otorhinolaryngol. 2001;60(3):193–6. doi: 10.1016/s0165-5876(01)00531-6. [DOI] [PubMed] [Google Scholar]
- 12.Ciftci AO, Bingöl-Koloğlu M, Şenocak ME, Tanyel FC, Büyükpamukçu N. Bronchoscopy for evaluation of foreign body aspiration in children. J Pediatr Surg. 2003;38(8):1170–6. doi: 10.1016/s0022-3468(03)00263-x. [DOI] [PubMed] [Google Scholar]
- 13.Lee EY, Restrepo R, Dillman JR, Ridge CA, Hammer MR, Boiselle PM. Imaging evaluation of pediatric trachea and bronchi: systematic review and updates. Semin Roentgenol. 2012;47(2):182–96. doi: 10.1053/j.ro.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 14.Haliloglu M, Ciftci AO, Oto A, Gumus B, Tanyel FC, Senocak ME, et al. CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration. Eur J Radiol. 2003;48(2):188–92. doi: 10.1016/S0720-048X(02)00295-4. [DOI] [PubMed] [Google Scholar]
- 15.Hong S-J, Goo HW, Roh J-L. Utility of spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol Head Neck Surg. 2008;138(5):576–80. doi: 10.1016/j.otohns.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 16.Huang H-J, Fang H-Y, Chen H-C, Wu C-Y, Cheng C-Y, Chang C-L. Three-dimensional computed tomography for detection of tracheobronchial foreign body aspiration in children. Pediatr Surg Int. 2008;24(2):157–60. doi: 10.1007/s00383-007-2088-2. [DOI] [PubMed] [Google Scholar]
- 17.Jung SY, Pae SY, Chung SM, Kim HS. Three-dimensional CT with virtual bronchoscopy: a useful modality for bronchial foreign bodies in pediatric patients. Eur Arch Otorhinolaryngol. 2012;269(1):223–8. doi: 10.1007/s00405-011-1567-1. [DOI] [PubMed] [Google Scholar]
- 18.Kocaoglu M, Bulakbasi N, Soylu K, Demirbag S, Tayfun C, Somuncu I. Thin-section axial multidetector computed tomography and multiplanar reformatted imaging of children with suspected foreign-body aspiration: is virtual bronchoscopy overemphasized? Acta Radiol. 2006;47(7):746–51. doi: 10.1080/02841850600803834. [DOI] [PubMed] [Google Scholar]
- 19.Kosucu P, Ahmetoglu A, Koramaz I, Orhan F, Özdemir Ou, Dinç H, et al. Low-dose MDCT and virtual bronchoscopy in pediatric patients with foreign body aspiration. AJR Am J Roentgenol. 2004;183(6):1771–7. doi: 10.2214/ajr.183.6.01831771. [DOI] [PubMed] [Google Scholar]
- 20.Liang J, Hu J, Chang H, Gao Y, Luo H, Wang Z, et al. Tracheobronchial foreign bodies in children–a retrospective study of 2,000 cases in Northwestern China. Ther Clin Risk Manag. 2015;11:1291–5. doi: 10.2147/TCRM.S86595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pitiot V, Grall M, Ploin D, Truy E, Khalfallah SA. The use of CT-scan in foreign body aspiration in children: a 6 years' experience. Int J Pediatr Otorhinolaryngol. 2017;102:169–73. doi: 10.1016/j.ijporl.2017.08.036. [DOI] [PubMed] [Google Scholar]
- 22.Sattar A, Ahmad I, Javed AM, Anjum S. Diagnostic accuracy of chest x-ray in tracheobronchial foreign body aspiration in paediatric patients. J Ayub Med Coll Abbottabad. 2011;23(4):103–5. [PubMed] [Google Scholar]
- 23.Shen J, Huang L, Hao C. Value of MSCT for diagnosis of tracheobronchial foreign body aspiration in children: 5-year retrospective study. Pediatr Int. 2020;62(10):1184–8. doi: 10.1111/ped.14269. [DOI] [PubMed] [Google Scholar]
- 24.Truong B, Luu K. Diagnostic clues for the identification of pediatric foreign body aspirations and consideration of novel imaging techniques. Am J Otolaryngol. 2023;44(4):103919. doi: 10.1016/j.amjoto.2023.103919. [DOI] [PubMed] [Google Scholar]
- 25.Ullal A, Mundra R, Gupta Y, Mishra S. Virtual bronchoscopy: highly sensitive time and life saving investigation in the diagnosis of foreign body aspiration—our experience. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 1):378–83. doi: 10.1007/s12070-018-1319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang C, Hua R, Xu K, Hua X, Ma P, Zheng J-N, et al. The role of 3D computed tomography (CT) imaging in the diagnosis of foreign body aspiration in children. Eur Rev Med Pharmacol Sci. 2015;19(2):265–73. [PubMed] [Google Scholar]
- 27.Azzi JL, Seo C, McInnis G, Urichuk M, Rabbani R, Rozovsky K, et al. A systematic review and meta-analysis of computed tomography in the diagnosis of pediatric foreign body aspiration. Int J Pediatr Otorhinolaryngol. 2023;165:111429. doi: 10.1016/j.ijporl.2022.111429. [DOI] [PubMed] [Google Scholar]
- 28.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:1–18. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arlachov Y, Ganatra R. Sedation/anaesthesia in paediatric radiology. Br J Radiol. 2012;85(1019):e1018–e31. doi: 10.1259/bjr/28871143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim IA, Shapiro N, Bhattacharyya N. The national cost burden of bronchial foreign body aspiration in children. Laryngoscope. 2015;125(5):1221–4. doi: 10.1002/lary.25002. [DOI] [PubMed] [Google Scholar]
- 31.Gordon L, Nowik P, Mobini Kesheh S, Lidegran M, Diaz S. Diagnosis of foreign body aspiration with ultralow-dose CT using a tin filter: a comparison study. Emerg Radiol. 2020;27(4):399–404. doi: 10.1007/s10140-020-01764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arora M, Thakker V, Thakkar N, Pitta M, Modi P, Arora S. Emergency Paediatric Airway Imaging: Should MDCT Precede Bronchoscopy in Suspicious Cases of Foreign Body Aspiration? J Clin Diagn Res. 2019;13(1):TC21–TC5. [Google Scholar]
- 33.Gibbons AT, Berazaluce AMC, Hanke RE, McNinch NL, Person A, Mehlman T, et al. Avoiding unnecessary bronchoscopy in children with suspected foreign body aspiration using computed tomography. J Pediatr Surg. 2020;55(1):176–81. doi: 10.1016/j.jpedsurg.2019.09.045. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed OG, Guillerman RP, Giannoni CM. Protocol incorporating airway CT decreases negative bronchoscopy rates for suspected foreign bodies in pediatric patients. Int J Pediatr Otorhinolaryngol. 2018;109:133–7. doi: 10.1016/j.ijporl.2018.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Friedman EM, Anthony B. A five-year analysis of airway foreign body management: toward a better understanding of negative bronchoscopies. Ann Otol Rhinol Laryngol. 2016;125(7):591–5. doi: 10.1177/0003489416637387. [DOI] [PubMed] [Google Scholar]
- 36.Abd-ElGawad EA, Ibrahim MA, Mubarak YS. Tracheobronchial foreign body aspiration in infants & children: Diagnostic utility of multidetector CT with emphasis on virtual bronchoscopy. Egypt J Radiol Nucl Med. 2014;45(4):1141–6. [Google Scholar]
- 37.Hassan MA, Youssef TA, El-Gharib M. Role of virtual bronchoscopy in foreign body inhalation in children. Egypt J Radiol Nucl Med. 2013;29:249–53. [Google Scholar]
- 38.Manach Y, Pierrot S, Couloigner V, Ayari-Khalfallah S, Nicollas R, Venail F, et al. Diagnostic performance of multidetector computed tomography for foreign body aspiration in children. Int J Pediatr Otorhinolaryngol. 2013;77(5):808–12. doi: 10.1016/j.ijporl.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 39.Bai W, Zhou X, Gao X, Shao C, Califano JA, Ha PK. Value of chest CT in the diagnosis and management of tracheobronchial foreign bodies. Pediatr Int. 2011;53(4):515–8. doi: 10.1111/j.1442-200X.2010.03299.x. [DOI] [PubMed] [Google Scholar]
- 40.Bhat K, Hegde J, Nagalotimath U, Patil G. Evaluation of computed tomography virtual bronchoscopy in paediatric tracheobronchial foreign body aspiration. J Laryngol Otol. 2010;124(8):875–9. doi: 10.1017/S0022215110000769. [DOI] [PubMed] [Google Scholar]
- 41.Adaletli I, Kurugoglu S, Ulus S, Ozer H, Elicevik M, Kantarci F, et al. Utilization of low-dose multidetector CT and virtual bronchoscopy in children with suspected foreign body aspiration. Pediatr Radiol. 2007;37(1):33–40. doi: 10.1007/s00247-006-0331-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.