Abstract
We report a case of infection with the zoonotic nematode Gongylonema sp. in a 24-year-old woman from Varna, Bulgaria. Two days before seeking medical attention, the patient had noticed a filamentous mass in her buccal mucosa that migrated when touched with the tongue. She manually removed a thread-like worm from the mucosa near her lower lip. Albendazole was prescribed for three days. The patient had no history of travelling abroad or contact with animals. To our knowledge, this is the sixth case that has been reported in the country.
Keywords: Gongylonematosis, Zoonotic disease, Helminth, Nematode
Introduction
There are more than 35 species of Gongylonema affecting a variety of mammals and birds but only G. pulchrum has been reported to infect humans (1). G. pulchrum, the gullet worm, is a nematode that invades the upper digestive tract of several mammalian species e.g. ruminants (cattle, sheep, goats), equids, pigs, rodents, bears, primates.
Intermediate hosts dung beetles develop the egg to infective third stage larvae and the infection occurs following accidental ingestion of the intermediate hosts or part of them via contaminated food or water. Ingested larvae develop into adult worms in the mucosa and submucosa of the duodenum and stomach of infected animals in around 60–80 days. After that they migrate to the esophagus and oral cavity (2). The movement of the parasites forms visible serpentine tails under the mucosa (3). Human infections are rare i.e. less than 200 cases have been reported worldwide since the worm was isolated from a child in 1850 (1).
Case report
The patient was a healthy, 24-year-old woman, living in Varna (the third largest city in Bulgaria). Two days before seeking medical attention, she had noticed a filamentous mass in her oral mucosa that she could feel with her tongue. The woman had a sensation that it migrated from the left side of the buccal mucosa to the lower lip. She touched it with the fingers to find out what it was. Manually, she removed a thread-like worm from the mucosa near to her lower lip. She brought it to the Department of Parasitology, Medical University of Plovdiv, where it was determined as female Gongylonema sp. under a light microscope.
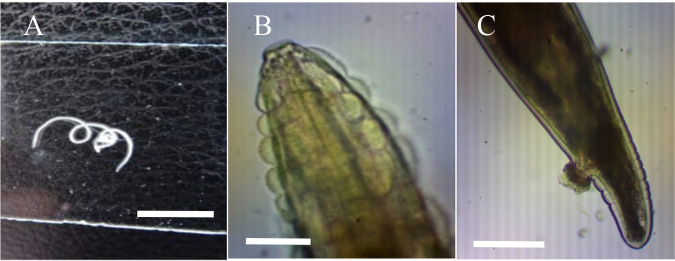
The parasite was whitish, thin and cylindrical with small part of its body partially destroyed. It was around 30 mm long and 0.12 mm wide. The anterior end was characteristic with raised cuticular bosses arranged in longitudinal rows. The worm possessed a small mouth with a funnel-shaped rim. A transverse striation of the cuticle followed the bosses anteriorly. Unfertilized eggs were observed in the uterus. The caudal end was asymmetrically bluntly conical (Fig.1).
Fig. 1:
Gongylonema sp.: A. Adult worm; B. Anterior end covered by cuticular bosses arranged in longitudinal rows; C. Caudal end (female). Scale bars: A – 10 mm, B and C – 50 μm
The patient had no other symptoms or eosinophilia in differential blood count. She was a fashion model and often ate salads, sushi and meat. She had no history of travelling abroad but she had been staying in a small village for three months before extraction of the parasite. Albendazole was prescribed for 3 days at a dose of 400 mg twice a day because of the concern that more than one helminth could have invaded the patient (4). After the removal of the parasite, the woman had no more complaints about her oral cavity.
Ethics approval
Written informed consent was obtained from the patient.
Discussion
Cases of gongylonematosis in man are rare which is associated with the mode of transmission (4). Unboiled water and unwashed vegetables contaminated with larvae can be a source of infection, but usually how the patients acquired the infection cannot be determined with certainty (5).
The disease has been reported from China, the USA, France, Slovenia, Italy, Brazil, Sri Lanka, Japan, Iran (1,6–8). Five cases have been observed in Bulgarian residents since now and all of them lived in rural areas (9).
Infected persons are young or middle-aged and their oral cavity is affected (10–12) as in the case we presented. Rarely, G. pulchrum has been found in the esophagus (8,13). The most common clinical presentation is a sensation of a foreign body in the mouth. The movement of the helminth can cause ache, numbness of tongue, difficulty in swallowing, hypersalivation, nausea, vomiting (10,14). Eosinophils can be elevated. Gongylonematosis can be misdiagnosed as oral candidiasis, delusional parasitosis or psychosis especially when the parasite cannot be seen during the examination of the oral cavity (5,14). One human case of esophageal gongylonematosis coexisting with early esophageal cancer has been reported but the authors could not conclude a strong relationship between these diseases (13). Yet G. pulchrum has not been shown to stimulate malignant tissue degeneration in humans as other species (G. neoplasticum and G. orientale) do in animals (1).
The diagnosis of gongylonematosis is made by identification of the parasite after its extraction. Morphological examination of the anterior end of the parasite shows characteristic rounded bosses of Gongylonema spp. (3). Male G. pulchrum and G. nepalensis (identified in domestic and wild ruminants in Europe) can be differentiated by the length of left spicule – it is shorter in G. nepalensis (less than 20.9% of the body length). But female parasites of both species are almost identical and on morphological grounds it is difficult to make exact differentiation (15). Therefore, in the reported case, the extracted parasite was identified as Gongylonema sp. Molecular genetic analyses are needed to determine the species (7).
Extraction of the parasite is the most effective treatment. Some patients take albendazole for three days although there is not enough evidence that it can cure patients with gongylonematosis (4).
Conclusion
Human infection with the zoonotic nematode Gongylonema sp. is a surprising clinical finding. Although rare, doctors should be aware of this disease and consider it in a differential diagnosis when the patient presents complaints related to the oral cavity even if there are no obvious risk factors for acquiring this parasite.
Footnotes
Conflict of interest
Authors state no conflict of interest.
References
- 1.Kurumanastırlı B, Yılmaz YA. Literature Review of Gongylonema pulchrum: A Rare Nematode. Turkiye Parazitol Derg. 2021;45(4):311–6. English. doi: 10.4274/tpd.galenos.2021.77486 [DOI] [PubMed] [Google Scholar]
- 2.Xiaodan L, Zhensheng W, Ying H, Hongwei L, Jianqiu J, et al. Gongylonema pulchrum infection in the human oral cavity: A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(3):e49–e53. doi: 10.1016/j.oooo.2017.11.019 [DOI] [PubMed] [Google Scholar]
- 3.Mathison BA, Pritt BS. A Systematic Overview of Zoonotic Helminth Infections in North America. Lab Med. 2018;49:e61–e93. doi: 10.1093/labmed/lmy029 [DOI] [PubMed] [Google Scholar]
- 4.Wilson ME, Lorente CA, Allen JE, Eberhard ML. Gongylonema infection of the mouth in a resident of Cambridge, Massachusetts. Clin Infect Dis. 2001;32(9):1378–80. doi: 10.1086/319991 [DOI] [PubMed] [Google Scholar]
- 5.Allen JD, Esquela-Kerscher A. Gongylonema pulchrum infection in a resident of Williamsburg, Virginia, verified by genetic analysis. Am J Trop Med Hyg. 2013;89(4):755–7. doi: 10.4269/ajtmh.13-0355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haruki K, Furuya H, Saito S, Kamiya S, Kagei N. Gongylonema infection in man: a first case of gongylonemosis in Japan. Helminthologia. 2005;42(2):63–6. [Google Scholar]
- 7.Kramar U, SkvarČ M, Logar M, et al. First case of human Gongylonema pulchrum infection in Slovenia. J Helminthol. 2019;94:e62. doi: 10.1017/S0022149X19000658 [DOI] [PubMed] [Google Scholar]
- 8.Huang Q, Wang J, Yang T, Liu Y. Multiple Gongylonema pulchrum worms in a human esophagus. Endoscopy. 2016;48:E24–25. doi: 10.1055/s-0035-1569657 [DOI] [PubMed] [Google Scholar]
- 9.Ganov V. Gongylonema pulchrum, Molin 1857. Bulgarian Clinic. 1940;XII(1–2):77 (in Bulgarian) [Google Scholar]
- 10.Pesson B, Hersant C, Biehler JF, et al. First case of human gongylonemosis in France. Parasite. 2013;20:5. doi: 10.1051/parasite/2013007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molavi GH, Massoud J, Gutierrez Y. Human Gongylonema infection in Iran. J Helminthol. 2006;80(4):425–8. doi: 10.1017/joh2006355 [DOI] [PubMed] [Google Scholar]
- 12.Ayala MA, Yencha MW. Gongylonema: a parasitic nematode of the oral cavity. Arch Otolaryngol Head Neck Surg. 2012;138(11):1082–4. doi: 10.1001/2013.jamaoto.386 [DOI] [PubMed] [Google Scholar]
- 13.Zhou Q, Wei Y, Zhai H, Li S, Xu R, et al. Comorbid early esophageal cancer and Gongylonema pulchrum infection: a case report. BMC Gastroenterol. 2021;21(1):305. doi: 10.1186/s12876-021-01873-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Libertin CR, Reza M, Peterson JH, Lewis J, Hata DJ. Human Gongylonema pulchrum Infection: Esophageal Symptoms and Need for Prolonged Albendazole Therapy. Am J Trop Med Hyg. 2017;96(4):873–5. doi: 10.4269/ajtmh.16-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varcasia A, Scala A, Zidda A, et al. First record of Gongylonema nepalensis in domestic and wild ruminants in Europe. Vet Parasitol. 2017;246:11–18. doi: 10.1016/j.vetpar.2017.08.022 [DOI] [PubMed] [Google Scholar]