Abstract
BACKGROUND
Chondrosarcoma is typically a slow-growing tumor, and intratumoral hemorrhage is rare. Acute brainstem hemorrhage due to chondrosarcoma has rarely been reported.
OBSERVATIONS
A 77-year-old man presented with the sudden onset of headache and vomiting followed by a declining level of consciousness, progressive right hemiparesis, and left ophthalmoplegia. Magnetic resonance imaging showed pontine hemorrhage and a mass in the retroclival space compressing the brainstem. Emergency endoscopic endonasal surgery was performed. Intraoperative observation revealed that a hematoma was located in the pons and subdural space around the tumor mass, suggesting that the hematoma had likely been caused by the rupture of small vessels around the pons, not by intratumoral hemorrhage. The pathological diagnosis was chondrosarcoma. The patient recovered well and underwent radiotherapy.
LESSONS
This report describes a case of sudden neurological deterioration due to hemorrhage in a patient with chondrosarcoma of the skull base. An emergency endoscopic endonasal approach for mass reduction and hematoma removal was effective in the acute setting. This approach revealed the suspected etiology of peritumoral hemorrhage, not intratumoral hemorrhage.
Keywords: chondrosarcoma, chordoma, endoscopic endonasal approach, brainstem hemorrhage, skull base
ABBREVIATIONS: MRI = magnetic resonance imaging
Skull base chondrosarcoma is a rare primary osseous malignancy that represents only 0.2% of all intracranial tumors.1 Because chondrosarcoma arises from primitive mesenchymal cells retained after endochondral ossification or embryonal cartilage remnants in the cranial base synchondroses, it commonly develops in the fibrocartilage and invades the skull bone or displaces surrounding structures.1–3 Chondrosarcoma is typically a slow-growing tumor that progressively compresses the contents of the posterior fossa or cavernous sinus until the patient becomes symptomatic, typically exhibiting cranial neuropathies.
Chondrosarcoma is frequently compared with chordoma because of the similarity of their anatomical location of development and radiographic findings. However, chordoma progresses in a more drastic manner, and its recurrence rate after resection is relatively high.4 In contrast to chordoma, chondrosarcoma does not commonly exhibit direct invasion of the surrounding neurovascular structures.2, 5 Instead, chondrosarcoma tends to compress or displace neurovascular structures, explaining its indolent symptomatology. Acute hemorrhagic onset of chondrosarcoma is a rare occurrence when compared with chordoma.6, 7
Illustrative Case
A 77-year-old man presented with the sudden onset of headache and vomiting followed by a declining level of consciousness, progressive right hemiparesis, and left ophthalmoplegia. Head computed tomography showed pontine hemorrhage and a mass in the retroclival space, and the mass extended dorsally and compressed the pons (Fig. 1A and B). Magnetic resonance imaging (MRI) revealed a low-intensity mass on the T1-weighted image, and the mass was strongly enhanced with contrast agent (Fig. 1C and D). Because of the patient’s declining level of consciousness, we performed emergency endoscopic endonasal tumor removal for mass reduction.
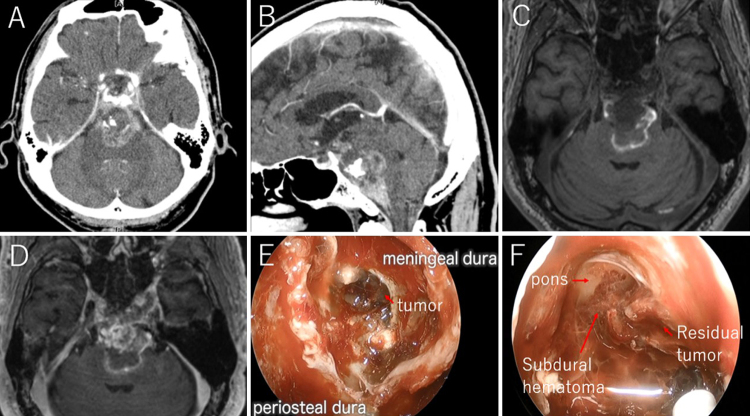
FIG. 1.
Admission axial (A) and sagittal (B) head computed tomography scans demonstrating subdural hemorrhage extending to the pons and a mass in the retroclival space. Admission MRI revealed a retroclival mass, with a T1-weighted sequence without contrast agent (C) showing a mass of low signal intensity and a T1-weighted image with contrast agent (D) showing a heterogeneously enhanced mass. Findings of endoscopic endonasal surgery (E): after drilling the clival bone, the tumor mass was found in the interdural space and extending to the pons, which caused disruption of the dura propria. No intratumoral hemorrhage was found. After partial resection of the tumor (F), residual tumor was found to penetrate the arachnoid and pia maters, resulting in hemorrhage around the subdural space.
A standard binostril approach was chosen. After drilling the clival bone, the soft tumor mass was exposed and found to reside in the interdural space and extend to the pons with disruption of the dura propria. No intratumoral hemorrhage was found intraoperatively (Fig. 1E). The tumor had a soft consistency with partial calcification. It progressed dorsally and medially, penetrating the arachnoid and pia maters and causing hemorrhage in the pons and surrounding subdural space (Fig. 1F). After subtotal removal of the tumor and decompression of the pons, a vascularized nasoseptal flap with a collagen matrix was used for skull base reconstruction.
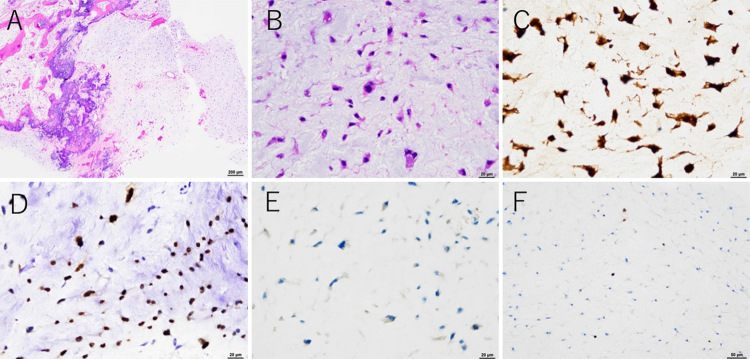
Hematoxylin and eosin staining revealed that the tumor had an abundant myxoid and cartilaginous matrix but no evidence of intratumoral hemorrhage (Fig. 2A and B). Immunohistochemistry revealed positive staining for S100 and SOX9 (Fig. 2C and D). Brachyury staining was negative (Fig. 2E), confirming that the tumor was not a chordoma. The Ki-67 labeling index was < 1% (Fig. 2F). The pathological diagnosis was grade 2 chondrosarcoma.
FIG. 2.
Hematoxylin and eosin staining showed spindle and fusiform cells with eosinophilic cytoplasm and a myxoid and cartilaginous matrix (AandB). Immunohistochemistry for S100 (C) and SOX9 (D) was positive. Brachyury staining (E) was negative. The Ki-67 labeling index was < 1% (F). Original magnification ×40 (A) and ×400 (B–F).
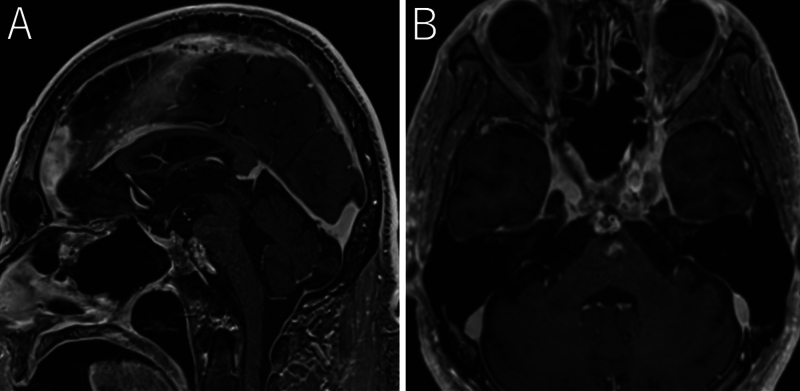
Four months after the operation, the patient had recovered well and was able to walk with minimal assistance. The left ophthalmoplegia had partially improved. MRI at 4 months postoperatively showed complete disappearance of the hematoma, and the residual mass was located in the left cavernous sinus near the basilar artery (Fig. 3A and B). The patient received radiotherapy for the residual mass.
FIG. 3.
Follow-up sagittal (A) and axial (B) T1-weighted MRI with contrast agent. The residual tumor was located only in the left cavernous sinus and around the basilar artery. The hematoma had completely disappeared.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Skull base chondrosarcoma is a rare disease entity, and its location and malignant features make it difficult for physicians to manage. The recurrence rate and prognosis of chondrosarcoma depend on the tumor histology, previous treatment, extent of tumor resection, and performance of adjuvant radiation therapy. Maximal safe resection with postoperative adjuvant radiation therapy is currently the most widely accepted management strategy to prevent recurrence and achieve good outcomes.4, 8
Chondrosarcoma and chordoma have different embryological origins. Both grow in a slow, destructive, and locally invasive manner. Chondrosarcoma tends to infiltrate the surrounding tissue, especially the bone and soft tissue, but not the vessels or nervous system.9 Because of the tumor’s location of invasion and gradual manner of progression, most patients initially exhibit nonspecific symptoms such as headaches or show few symptoms until the tumor grows so large that it compresses adjacent structures, such as cranial nerves and other neurovascular structures.5
The surgical approach to chondrosarcoma is challenging because of the tumor’s proximity to vital structures and poor accessibility. The recent advent of endoscopic endonasal surgery has facilitated aggressive resection with a manageable risk of complications; therefore, this approach is a more acceptable, more accessible, and less invasive approach than open surgery, especially in cases of clival chondrosarcoma.3, 8, 10, 11
Although several reports have described the hemorrhagic onset of chordoma, only a small number have described the hemorrhagic onset of chondrosarcoma. A few cases of hemorrhagic onset of primary intracranial chondrosarcoma have been reported in the literature (Table 1). Surgical craniotomy was performed in five patients,12–16 whereas an endoscopic approach was performed in ttwo patientsincluding our patient. (Table 1). Two patients had catastrophic outcomes due to complications, not due to tumor progression.12, 17 In most cases, tumor resection by craniotomy, not by the endoscopic approach, was chosen for the sudden onset of hemorrhage in the acute phase, and adjuvant radiotherapy was performed in most cases as well,.
TABLE 1.
Hemorrhagic cases of primary intracranial chondrosarcoma
| Authors & Year | Age (yrs) | Sex | Level of Consciousness & Manifestation on Admission | Location of Tumor | Type & Location of Hemorrhage | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Fukuchi et al., 199617 | 75 | F | Alert, blepharoptosis, diplopia | Clivus to petrous apex | ITH + PTH | Biopsy | Death |
| Ohshige et al., 200513 | 52 | F | Alert, headache, gait disturbance | Petrous bone to cerebellar hemisphere | IPH (cerebellum) | Evacuation of hematoma, partial resection (lat suboccipital approach) + RT | Survival |
| Harada et al., 200614 | 23 | M | Comatose, headache | Clivus | ITH + SAH | STR (combined subtemporal & presigmoid transpetrosal approach) + RT | Survival |
| Gallia et al., 200915 | 34 | M | Alert, headache, blurred vision | Paracavernous to suprasellar region | ITH + IVH, IPH (temporal lobe) | GTR (pterional approach) + RT | Survival |
| Jumani et al., 201012 | 21 | M | Alert but deteriorated (GCS score 14 to 8), rt paralysis, slurred speech | Parapharyngeal space to intracranial cavity | IPH (pons) | Chemo + RT (1st), GTR (craniotomy + EEA; 2nd) | Death |
| Little et al., 201316 | 46 | M | Alert, headache, blurred vision, photophobia | Prefrontal, extra-axial | ITH | STR (craniotomy) + RT | Survival |
| Present case | 77 | M | Comatose, headache, hemiparesis, ophthalmoplegia, coma | Clivus | IPH + PTH | STR (EEA) + RT | Survival |
EEA = endoscopic endonasal approach; GCS = Glasgow Coma Scale; GTR = gross-total resection; IPH = intraparenchymal hemorrhage; ITH = intratumoral hemorrhage; IVH = intraventricular hemorrhage; PTH = peritumoral hemorrhage; RT = radiotherapy; SAH = subarachnoid hemorrhage; STR = subtotal resection.
Because chondrosarcoma is commonly an avascular tumor,18, 19 intratumoral hemorrhage is quite rare. The intraoperative findings in our case showed that the location of the hemorrhage was subdural and intra-axial. The mechanism of the hemorrhage can be explained by the destruction of the periosteal and meningeal dura mater, as the tumor mass progressed dorsally and extended to the intradural space. The tumor could further invade the arachnoid and pia maters, and rupture of the surrounding vessels around the pons could result in a subdural hematoma and pontine hemorrhage (Fig. 4). MRI on admission also supported this pathophysiology as shown by a hyperintense rim surrounding the tumor on the T1-weighted image, suggesting peritumoral hemorrhage (Fig. 1C). The pathological findings were also consistent with peritumoral hemorrhage, not intratumoral hemorrhage. Close endoscopic inspection of the hemorrhagic compartment facilitated identification of the possible bleeding site. In the case of a hemorrhagic ventral/midline lesion of the brainstem without evidence of hydrocephalus or increased intracranial pressure, endoscopic surgery is considered a reasonable treatment option.
FIG. 4.
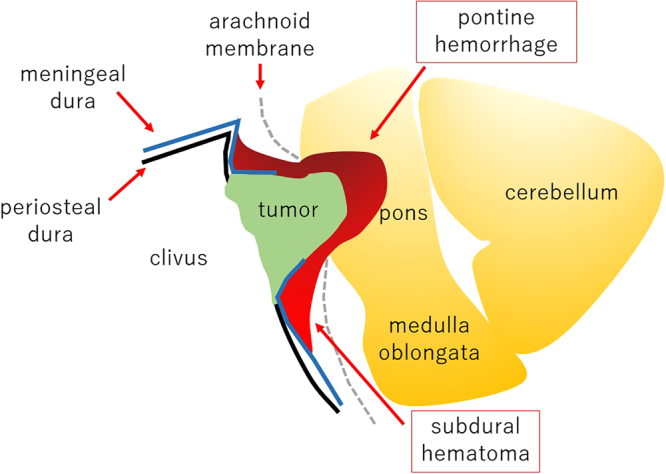
Illustration of the plausible mechanism of hemorrhage. The tumor arose from the cartilaginous matrix around the sphenopetroclival junction and progressed dorsally to the pons, with invagination and destruction of the meningeal and periosteal dura. Subdural hemorrhage and brainstem hemorrhage occurred secondary to the invasion or displacement of small vessels around the pons by the tumor.
Lessons
Chondrosarcoma grows in an indolent manner, and intratumoral hemorrhage of chondrosarcoma is extremely rare among previous reports. However, bleeding due to the disruption of vessels around the tumor can occur, as in our patient. Such bleeding can require an emergency procedure, especially if it affects the brainstem. Emergency decompression is necessary in cases of acute hemorrhage within a vital organ. In the present case, an endoscopic endonasal approach was effective for decompression and observation of the possible location of hemorrhage.
Acknowledgments
We thank Angela Morben, DVM, ELS, from Edanz for editing a draft of the manuscript.
Disclosures
Dr. Arakawa reported grants from Philips, Otsuka, Chugai, Nihon Medi-Physics, Daiichi Sankyo, Stryker, Eisai, Japan Blood Products Organization, Ono Pharmaceutical, Taiho Pharma, Sumitomo Dainippon Pharma, Astellas Pharma, Incyte Biosciences, and Servier; and personal fees from Nippon Kayaku, Novocure, UCB Japan, Ono Pharmaceutical, Brainlab, Merck, Chugai, Eisai, Daiichi Sankyo, Carl Zeiss, and Nihon Medi-Physics outside the submitted work
Author Contributions
Conception and design: Tanji, Mitani. Acquisition of data: Tanji, Mitani, Kitada, Sugimoto. Analysis and interpretation of data: Tanji, Sugimoto, Fujimoto. Drafting the article: Tanji, Mitani. Critically revising the article: Tanji, Mitani, Kitada, Sugimoto, Arakawa. Reviewed submitted version of manuscript: Mitani, Kikuchi, Arakawa. Approved the final version of the manuscript on behalf of all authors: Tanji. Statistical analysis: Tanji. Administrative/technical/material support: Tanji, Arakawa. Study supervision: Tanji, Arakawa.
Correspondence
Masahiro Tanji: Kyoto University Graduate School of Medicine, Sakyo-ku, Kyoto, Japan. tanji@kuhp.kyoto-u.ac.jp.
References
- 1.Carlson ML, O’Connell BP, Breen JT, et al. Petroclival chondrosarcoma: a multicenter review of 55 cases and new staging system. Otol Neurotol. 2016;37(7):940-950. [DOI] [PubMed] [Google Scholar]
- 2.Samii A, Gerganov V, Herold C, Gharabaghi A, Hayashi N, Samii M. Surgical treatment of skull base chondrosarcomas. Neurosurg Rev. 2009;32(1):67-75. [DOI] [PubMed] [Google Scholar]
- 3.Sbaihat A, Bacciu A, Pasanisi E, Sanna M. Skull base chondrosarcomas: surgical treatment and results. Ann Otol Rhinol Laryngol. 2013;122(12):763-770. [DOI] [PubMed] [Google Scholar]
- 4.Almefty K, Pravdenkova S, Colli BO, Al-Mefty O, Gokden M. Chordoma and chondrosarcoma: similar, but quite different, skull base tumors. Cancer. 2007;110(11):2457-2467. [DOI] [PubMed] [Google Scholar]
- 5.Ditzel Filho LFS, Prevedello DM, Dolci RL, et al. The endoscopic endonasal approach for removal of petroclival chondrosarcomas. Neurosurg Clin N Am. 2015;26(3):453-462. [DOI] [PubMed] [Google Scholar]
- 6.Vellutini Ede A, de Oliveira MF. Intradural chordoma presenting with intratumoral bleeding. J Clin Neurosci. 2016;25:139-142. [DOI] [PubMed] [Google Scholar]
- 7.Kim SK, Kim YH, Park CK, Kim MA, Park SH. Intracranial intradural chordoma presenting with intraventricular hemorrhage. Clin Neurol Neurosurg. 2012;114(8):1189-1192. [DOI] [PubMed] [Google Scholar]
- 8.Bloch OG, Jian BJ, Yang I, et al. Cranial chondrosarcoma and recurrence. Skull Base. 2010;20(3):149-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kremenevski N, Schlaffer SM, Coras R, Kinfe TM, Graillon T, Buchfelder M. Skull base chordomas and chondrosarcomas. Neuroendocrinology. 2020;110(9-10):836-847. [DOI] [PubMed] [Google Scholar]
- 10.Vaz-Guimaraes F, Fernandez-Miranda JC, Koutourousiou M, et al. Endoscopic endonasal surgery for cranial base chondrosarcomas. Oper Neurosurg. 2017;13(4):421-434. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Q, Kong F, Yan B, Ni Z, Liu H. Endoscopic endonasal surgery for clival chordoma and chondrosarcoma. Orl J Otorhinolaryngol Relat Spec. 2008;70(2):124-129. [DOI] [PubMed] [Google Scholar]
- 12.Jumani MI, Channa R, Zafar SN, Enam SA. Pontine haemorrhage due to chondrosarcoma of the skull base. J Coll Physicians Surg Pak. 2010;20(10):692-694. [DOI] [PubMed] [Google Scholar]
- 13.Ohshige H, Kasai H, Imahori T, et al. A case of petrous bone myxoid chondrosarcoma associated with cerebellar hemorrhage. Brain Tumor Pathol. 2005;22(1):41-44. [DOI] [PubMed] [Google Scholar]
- 14.Harada K, Nakahara I, Hayashi J, et al. Chondrosarcoma of the clivus presenting with intratumoral hemorrhage: case report. J Neurooncol. 2006;77(2):221-223. [DOI] [PubMed] [Google Scholar]
- 15.Gallia GL, Binder ZA, Schwarz J, Moriarity JL, Weingart JD. Skull base chondrosarcoma presenting with hemorrhage. Can J Neurol Sci. 2009;36(6):774-775. [DOI] [PubMed] [Google Scholar]
- 16.Little A, Chung C, Perez-Ordonez B, Mikulis D, Valiante TA. High-grade intracranial chondrosarcoma presenting with haemorrhage. J Clin Neurosci. 2013;20(10):1457-1460. [DOI] [PubMed] [Google Scholar]
- 17.Fukuchi M, Fushimi S, Yoneya M, et al. Chondrosarcoma of the skull base associated with fatal intratumoral hemorrhage: report of an autopsy case and review of the literature. Article in Japanese. No Shinkei Geka. 1996;24(2):175-180. [PubMed] [Google Scholar]
- 18.Berkmen YM, Blatt ES. Cranial and intracranial cartilaginous tumours. Clin Radiol. 1968;19(3):327-333. [DOI] [PubMed] [Google Scholar]
- 19.Korten AG, ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 1998;65(1):88-92. [DOI] [PMC free article] [PubMed] [Google Scholar]