Summary box.
This commentary highlights various definitions of maternal and newborn health care providers used globally and demonstrates the considerable effect of a definition on study findings.
Standard definitions (eg, qualified, skilled or trained) are helpful, but the use of these terms alone might give a spurious sense of consistency, when nuanced characteristics of providers could be lacking in a specific setting.
We recommend that provider definitions should explicitly state who (designations) are involved, where (context) and when (any relevant time-specific systemic changes that could potentially impact service delivery) to complement the standard definitions.
In the global maternal and newborn health (MNH) literature, care providers have been classified in several ways, engendering the question—whether providers who care for the mother and her newborn(s) have the necessary training and skills to provide quality care. This question underscores the importance of clearly defining who provided care. A specific definition not only facilitates correct interpretation of findings but helps understand potential reasons behind successes or failures of MNH interventions. Additionally, in low- and middle-income countries (LMICs), providers who routinely attend deliveries often receive varying levels of training, even within the same classifications. This inconsistency can result in incomparable estimates of skilled birth attendance, an indicator used to reference MNH care globally.
This commentary emphasises the importance of a provider definition that is beyond the use of standard terminology like qualified, skilled or trained. We begin by reviewing the common definitions used globally, then demonstrate, using an example, the effect of definition on study findings. MNH care provider definitions should include who was involved (eg, education and training, licensing, experience and the signal function responsibilities for each provider category), where care was provided (eg, level of the facility, facility vs outreach, current national regulations for adequate contextual description) and when to describe any recent event that might have impacted the provision of care (eg, a recent training to improve and certify provider skills, a current inclusion of a new classification to provide MNH services). A definition that is relevant to national regulations and reflects on-the-ground grassroots is often selected by MNH researchers and practitioners, especially in LMICs, where chronic shortages of clinicians prevail and job classifications ranging from obstetricians to community health aides are involved in providing care.1 However, the standard definitions alone may not suitably characterise the capacities of MNH care providers, across countries. Furthermore, the delineation between skilled and unskilled providers is generally clear at either end of the scale—that is, physicians, nurses and midwives are considered skilled, while traditional birth attendants are considered unskilled.2 3 It is nebulous for those in the middle—for example, matron, a functional cadre of birth attendants in West Africa relevant to this day.
Provider definitions
Providers in high-income settings have been referred to as qualified health professionals. In 2013, the American Medical Association defined ‘a physician or other qualified healthcare professional as an individual who is qualified by education, training, licensure/regulation (when applicable) and facility privileging (when applicable) who performs a professional service within his/her scope of practice and independently reports that professional service’.4 The European Union recognises doctors of medicine, general nurses, midwives, dentists and pharmacists as qualified healthcare professionals.5 In 2017, the Organization for Economic Co-operation and Development (OECD), the Eurostat and the WHO revised the classifications of healthcare providers, implicitly incorporating ‘who’ and ‘where’.6 The comparability of healthcare settings (‘where’) across countries within the high-income category renders a basic degree of consistency that is unlikely to exist across LMIC. Thus, other definitions exist to facilitate universal comparison as well as to measure attainment of global goals.
The Sustainable Development Goal (SDG) 3.1.2 has the proportion of births attended by skilled personnel as a target. In 2018, the WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA issued a joint statement and revised the 2004 definition of skilled personnel.3 7 The revision defined skilled personnel as competent MNH professionals educated, trained and regulated to national and international standards and included midwives, nurses, obstetricians, paediatricians and anaesthetists. However, the revised definition also stated, ‘In different countries, these competencies are held by professionals with varying occupational titles’, leaving room for the inclusion of other titles not listed in the definition.3 The rationale for the 2018 revision was to provide a uniform basis across countries for robust measurement of SDG targets. A review showed that 21 different cadres, with varying lengths of training and signal function responsibilities, were grouped as skilled providers.1
A close alternative to ‘skilled provider’ is ‘trained provider’, used by the Demographic and Health Surveys (DHS) to estimate MNH indicators. These indicators are frequently used as benchmarks to assess a country's progress toward global health targets. The DHS define trained providers as doctors, nurses, midwives and matrons. The key distinction with the skilled provider is the inclusion of matrons. Matrons, esteemed for their expertise and traditional knowledge, play a pivotal role in MNH care across Africa, including Guinea, Niger, Mali, Senegal and Togo.8,12 Recent DHS across West Africa show a high but variable prevalence of matrons, ranging from 63% in Nigeria to 98% in Burkina Faso.13 This variability reflects the diverse healthcare landscapes and cultural contexts in which matrons operate.
These definitions are critical to uniformly measure international progress in MNH care. However, using only these terminologies may not sufficiently describe the ground situation in a place. We demonstrate this point using a case from Mali.
ProCCM study example
We used data from the Proactive Community Case Management (ProCCM) cluster randomised trial to illustrate the importance of a specific definition of the provider. The trial evaluated whether proactive case detection home visits by community health workers (CHWs) can improve reproductive, maternal and child health indicators at a population level, compared with services delivered only through a fixed health post. Both of these modes were supplemented with a package of services designed to remove financial, geographical and clinical barriers to care.14 The trial was conducted in Bankass Health District in Mali, between 2016 and 2020. Eligible participants were women between 15 and 49 years who were permanent residents of the study area with no plans to relocate for the duration of the trial. The primary outcome was under-5 mortality along with several secondary outcomes,14 including institutional delivery.15
In Mali, an institution was defined as a national, regional or referral hospital, dispensary, maternity home, primary health centre and private hospital or clinic.15 Following the DHS definition of a provider in Mali, we included doctors, nurses, midwives, matrons or a CHW. Our choice of provider definition was necessitated to maintain consistency with the DHS because it was the primary source of information that informed the design of the trial, including sample size; we additionally included CHWs in this group given the level of training and support they received through the intervention. A complete description of the methods and findings is presented elsewhere.15 Here, we used the same analytical methods but a modified provider definition where matrons were included in the unskilled category and doctors, nurses, midwives or CHWs were considered skilled providers. The origin of the cadre of matrons and their role have evolved over the last several decades in Mali.16 We compared institutional delivery between trial arms as well as between the baseline and the intervention period. Data were collected from annual household surveys at baseline and approximately at 12, 24 and 36 months after the start of the intervention. For the comparison between arms, we included data from the 24-month and 36-month surveys because, for deliveries reported in the 12-month survey, some period of the pregnancy likely occurred in the pre-intervention period.
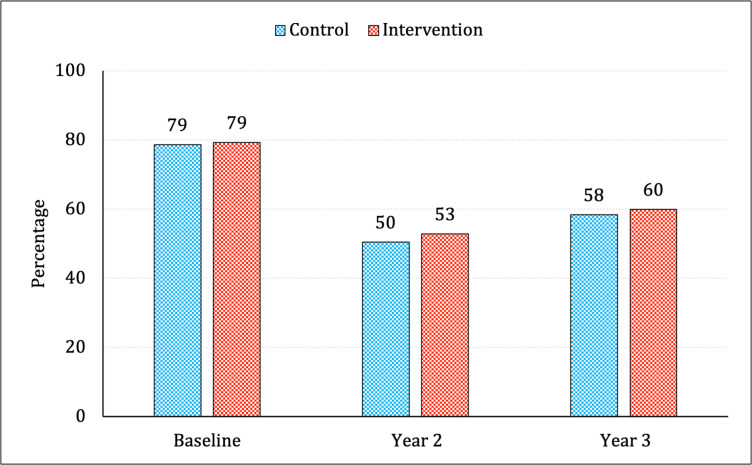
The proportions of institutional delivery with matron as a skilled provider were 59% and 57% in the intervention and control arms, which changed to 30% and 29% when matrons were considered unskilled providers, respectively (table 1). For each trial year, the proportions of institutional delivery conducted by matrons only were largely similar across the two arms, although, compared with the baseline, it decreased by about 30 and 20 percentage points in years 2 and 3, respectively (figure 1).
Table 1. Results of comparisons between: intervention with control arm; and intervention period (2020–2021) with baseline (2018), using different provider definitions.
| Institutional delivery | n/N* (%) | Risk ratio (95% CI)† | |
| Intervention vs control | Intervention | Control | |
| Published result (matron as skilled provider) | 1506/2542 (59.2) | 1421/2494 (56.9) | 1.06 (0.91 to 1.20)‡ |
| New result (matron as unskilled provider) | 752/2542 (29.6) | 727/2494 (29.2) | 1.01 (0.86 to 1.18)‡ |
| Intervention period vs baseline | Trial years 2 and 3 | Baseline | |
| Published result (matron as skilled provider) | 2927/5036 (58.1) | 2901/6668 (43.5) | 1.54 (1.41 to 1.66) |
| New pre–post (matron as unskilled provider) | 1479/5036 (29.4) | 794/6668 (11.9) | 2.46 (2.14 to 2.81) |
Counts with the outcome (n) out of the total participants (N) in the arm.
Each model included afixed effects for the year of intervention, residential distance to the nearest primary health centercentre, baseline population of the cluster, and a random intercept for thecluster.
Intention -Tto -Ttreat analysis including trial years two2 and three3 only.
Figure 1. The proportions of institutional delivery in each arm conducted by matrons at different years of the trial in Bankass, Mali, between 2016 and 2020.
We previously reported no evidence of an effect of the ProCCM intervention on institutional delivery in the last 2 years of the trial, considering the matron as a skilled provider (table 1).15 Considering the matron as an unskilled provider does not change the previous results (table 1). However, it does change the interpretation of the extent to which the ProCCM intervention affected the uptake of skilled assistance among institutional deliveries in trial years 2 and 3 compared with the baseline. During the last 2 years, the likelihood of a participant delivering in an institution with skilled assistance was 1.54 times (95% CI: 1.41 to 1.66) the likelihood of delivering in an institution at baseline, which increased to 2.46 (95% CI: 2.14 to 2.81) when matrons were considered as unskilled providers (table 1).
In Mali, the proportion of institutional deliveries conducted by matrons (who) declined during the ProCCM trial, compared with the baseline, in part, because around the time of the trial (when) Muso hired and trained a significant number of health personnel and deployed them across all (intervention and control) clusters. Consequently, institutional deliveries conducted by matrons decreased uniformly across all clusters. Thus, we did not observe a difference by trial arms but observed a big change over time (ie, between the intervention period and the baseline).
This example provides empirical evidence about the effect of provider definition on results. It is essential to understand how each type of provider is defined internationally and what is the closest match with the national definition in order to align the two. In the local context, a provider may have a designation that is misaligned with international definitions, which does not necessarily make an experienced group unskilled. However, the context (where) should be adequately explained for broader comparisons and interpretation. Currently, there are settings where providers with adequate competencies are not designated to perform EmONC signal functions because of lacking matching legislation, while in others, especially in South Asia, unskilled providers perform EmONC signal functions.1 17 Evidence also suggests that engaging CHWs can increase births with skilled assistance,18 though this cadre is not considered skilled.3
The standardised definitions of MNH providers are necessary to enable international comparisons. Despite the existence of these definitions, ambiguity exists in the global literature in terms of which provider classifications constitute these definitions in different countries. The use of standard terminology while necessary may not be sufficient by itself. It might even give a spurious sense of consistency if the underlying classifications that provide MNH care in a setting are inconsistent with the international definitions. Explicitly stating who (designations, trainings) are involved in providing care, where care was provided (context) and when (any relevant time-specific systemic changes that have the potential to impact MNH service delivery) will increase the interpretability, transparency and replicability of evidence.
Footnotes
Funding: The trial was funded with resources received by Muso through unrestricted funding as well as dedicated research funding from Child Relief International Foundation, Grand Challenges Canada (awards 1808-17345 and TTS-2002-37264), Johnson & Johnson Foundation (awards 85442 and 82844) and USAID Development Innovation Ventures (grant number 7200AA20FA00020). Child Relief International Foundation served as the nonlegal sponsor of the trial. Grant no is not applicable. The funders had no role in the design, analysis, or interpretation of the trial and its results.
Handling editor: Valery Ridde
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and The University of California, San Francisco exempted secondary analysis of the data from ethical approval. The study received ethical approval from the Ethics Committee of the Faculty of Medicine, Pharmacy and Dentistry at the University of Bamako. Informed consent from all household survey respondents was obtained prior to enrolment in the study. If the respondent was a minor, her parent’s or guardian’s consent was obtained. All methods used in the study were performed in accordance with the relevant Malian and US guidelines and regulations. Participants gave informed consent to participate in the study before taking part.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability free text: Deidentified data for the empirical case presented in this commentary can be made available on reasonable request. Please contact Maud Amon-Tanoh at Muso, mamon@musohealth.org.
Contributor Information
Rakesh Ghosh, Email: Rakesh.Ghosh@ucsf.edu.
Kassoum Kayentao, Email: kayentao@icermali.org.
Jessica Beckerman, Email: jbeckerman@musohealth.org.
Bréhima Traore, Email: btraore@musohealth.org.
Sasha Rozenshteyn, Email: sroz@umich.edu.
Ari Johnson, Email: ajohnson@musohealth.org.
Emily Treleaven, Email: treleav@umich.edu.
Jenny X Liu, Email: Jenny.Liu2@ucsf.edu.
Data availability statement
Data are available upon request.
References
- 1.Adegoke A, Utz B, Msuya SE, et al. Skilled Birth Attendants: who is who? A descriptive study of definitions and roles from nine Sub Saharan African countries. PLoS One. 2012;7:e40220. doi: 10.1371/journal.pone.0040220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Traditional birth attendants: a joint WHO/UNFPA/UNICEF statement. 1992. https://iris.who.int/bitstream/handle/10665/38994/9241561505.pdf?sequence=1 Available.
- 3.World Health Organization Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA. 2018. https://iris.who.int/bitstream/handle/10665/272818/WHO-RHR-18.14-eng.pdf Available.
- 4.Indiana State Medical Association and American Medical Association . Indiana: I.S.M. Association; 2013. What is a qualified health professional (qhp) clinical staff member?https://www.ismanet.org/pdf/education/QHP10-6-16.pdf Available. [Google Scholar]
- 5.Department of Health and Social Care United Kingdom Guidance for european economic area (eea)-qualified and swiss healthcare professionals practising in the UK. 2020. https://www.gov.uk/guidance/eea-qualified-and-swiss-healthcare-professionals-practising-in-the-uk Available.
- 6.OECD/Eurostat/World Health Organization . A system of health accounts 2011. Paris: OECD Publishing; 2017. Classification of health care providers (icha-hp) - chapter 6. [Google Scholar]
- 7.World Health Organization Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. 2004. https://www.who.int/publications/i/item/9241591692 Available.
- 8.Institut national de la statistique . Guinea demographic and health survey (EDS V) 2016-18, in INS/Guinea and ICF. Conakry, Guinea: DHS; 2019. [Google Scholar]
- 9.Institut National de la Statistique MinistËre du Plan and ICF . EnquÍte Sur Les Indicateurs Du Paludisme Au Niger 2021. Rockville, Maryland, USA: INS et ICF; 2023. [Google Scholar]
- 10.Institut national de la statistique (instat) Enquête sur les Indicateurs du Paludisme au Mali 2021. Bamako, Mali et Rockville, Maryland, USA: INSTAT, PNLP et ICF; 2022. Programme national de lutte contre le paludisme (pnlp) et icf. [Google Scholar]
- 11.Agence Nationale de la Statistique et de la Démographie (ANSD) [Sénégal], e.I . Enquête Sur Les Indicateurs Du Paludisme Au Sénégal, 2020-2021. Rockville, Maryland, USA: ANSD et ICF; 2021. [Google Scholar]
- 12.RÈpublique DÈmocratique du Congo EnquÍte DÈmographique et de SantÈ (EDS-RDC) 2013-2014. Rockville, Maryland, USA: MPSMRM, MSP, and ICF International; 2014. MinistËre du plan et suivi de la mise en úuvre de la rèvolution de la modernitè - mpsmrm/congo, ministëre de la santè publique - msp/congo, and icf international. [Google Scholar]
- 13.ICF The dhs program statcompiler. 2012. https://www.statcompiler.com/en Available.
- 14.Whidden C, Treleaven E, Liu J, et al. Proactive community case management and child survival: protocol for a cluster randomised controlled trial. BMJ Open. 2019;9:e027487. doi: 10.1136/bmjopen-2018-027487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kayentao K, Ghosh R, Guindo L, et al. Effect of community health worker home visits on antenatal care and institutional delivery: an analysis of secondary outcomes from a cluster randomised trial in Mali. BMJ Glob Health. 2023;8:e011071. doi: 10.1136/bmjgh-2022-011071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golaszewski D. Traditional Birth Attendants’ and Reproductive Expertise in Postcolonial Mali. Gend Hist. 2021;33:756–73. doi: 10.1111/1468-0424.12551. [DOI] [Google Scholar]
- 17.Utz B, Siddiqui G, Adegoke A, et al. Definitions and roles of a skilled birth attendant: a mapping exercise from four South-Asian countries. Acta Obstet Gynecol Scand. 2013;92:1063–9. doi: 10.1111/aogs.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zuñiga JA, García A, Kyololo OM, et al. Increasing utilisation of skilled attendants at birth in sub-Saharan Africa: a systematic review of interventions. Int J Nurs Stud. 2021;120:103977. doi: 10.1016/j.ijnurstu.2021.103977. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request.