Abstract
Background
Chimeric antigen receptor (CAR)-T cell has revolutionary efficacy against relapsed/refractory multiple myeloma (R/R MM). However, current CAR-T cell therapy has several limitations including long vein-to-vein time and limited viability.
Methods
A 4-1BB-costimulated B-cell maturation antigen (BCMA) CAR-T integrating an independently-expressed OX40 (BCMA-BBZ-OX40) was designed and generated by a traditional manufacturing process (TraditionCART) or instant manufacturing platform (named InstanCART). The tumor-killing efficiency, differentiation, exhaustion, and expansion level were investigated in vitro and in tumor-bearing mice. An investigator-initiated clinical trial was performed in patients with R/R MM to evaluate the outcomes of both TraditionCART and InstanCART. The primary objective was safety within 1 month after CAR-T cell infusion. The secondary objective was the best overall response rate.
Results
Preclinical studies revealed that integrated OX40 conferred BCMA CAR-T cells with superior cytotoxicity and reduced exhaustion levels. InstanCART process further enhanced the proliferation and T-cell stemness of BCMA-BBZ-OX40 CAR-T cells. BCMA-BBZ-OX40 CAR-T cells were successfully administered in 22 patients with R/R MM, including 15 patients with TraditionCART and 7 patients with InstanCART. Up to 50% (11/22) patients had a high-risk cytogenetic profile and 36% (8/22) had extramedullary disease. CAR-T therapy caused grade 1–2 cytokine release syndrome in 19/22 (80%) patients, grade 1 neurotoxicity in 2/22 (9%) patients and led to ≥grade 3 adverse events including neutropenia (20/22, 91%), thrombocytopenia (15/22, 68%), anemia (12/22, 55%), creatinine increased (1/22, 5%), hepatic enzymes increased (5/22, 23%), and sepsis (1/22, 5%). The best overall response rate was 100%, and 64% (14/22) of the patients had a complete response or better. The median manufacturing time was shorter for InstanCART therapy (3 days) than for TraditionCART therapy (10 days). Expansion and duration were dramatically higher for InstanCART cells than for TraditionCART cells.
Conclusions
BCMA-BBZ-OX40 CAR-T cells were well tolerated and exhibited potent responses in patients with R/R MM. InstanCART shortened the manufacturing period compared to TraditionCART, and improved the cellular kinetics. Our results demonstrated the potency and feasibility of OX40-modified BCMA CAR-T cells using InstanCART technology for R/R MM therapy.
Trial registration number
This trial was registered at www.clinicaltrials.gov as #NCT04537442.
Keywords: Multiple Myeloma, Chimeric Antigen Receptor - CAR, Hematologic Malignancies, Immunotherapy, T cell
WHAT IS ALREADY KNOWN ON THIS TOPIC
Chimeric antigen receptor (CAR)-T cells targeting B-cell maturation antigen (BCMA) have achieved encouraging results in relapsed/refractory multiple myeloma (R/R MM), but there are still several limitations to be solved, including long vein-to-vein time, and limited persistence.
WHAT THIS STUDY ADDS
Our data support the idea that the constitutive expression of OX40 is beneficial for BCMA CAR-T-cell function. BCMA-BBZ-OX40 CAR-T cells were more persistent in vitro and in vivo, and were well tolerated in heavily pretreated patients with R/R MM. The establishment of a faster manufactured platform offers the potential to shorten the time needed before the administration of the product. Instant manufacturing platform (InstanCART) therapy had a comparable response rate compared with traditional manufacturing process therapy, even at a relatively low dose.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The InstanCART provides a treatment opportunity for rapidly progressive patients. This study provides the justification to embark on a larger, longer-duration multicenter clinical trial. Further study of OX40-modified BCMA InstanCART therapy in R/R MM is warranted.
Introduction
Chimeric antigen receptor T (CAR-T) cells targeting B-cell maturation antigen (BCMA) have shown dramatic response rates in patients with relapsed/refractory multiple myeloma (R/R MM). Despite the encouraging outcomes of CAR-T-cell therapy, how to enhance CAR-T-cell activity and viability, and reduce vein-to-vein time are still problems to be solved.1
Costimulation signaling contributes to the effector function, and persistence of T cells.2 3 In this regard, OX40 (CD134) activated by the ligand OX40L has broad effects on T-cell activation, proliferation, differentiation, and survival.4,7 At the molecular level, OX40 ligation recruits tumor necrosis factor (TNF) receptor-associated factor 2 (TRAF2), TRAF3, or TRAF5 to activate NF-κB, and induce antiapoptotic genes, including Bcl-2, and promotes the PI3K/AKT pathway to enhance cell survival and cell cycle progression.8,11 Inclusion of OX40 in CAR-T cells supports improved antigen-dependent memory formation.12 Preclinical investigation also showed that OX40-costimulated CAR-T cells outperformed both CD28 and 4-1BB CAR-T cells in cell persistence in an immunodeficient model of MM.12 13 CD19 or CD20 CAR-T cells with antigen-independent activation of OX40 have been reported to show robust amplification, and antitumor activity for treating B-cell malignancies.14 15 However, the performance of OX40 expression in CAR-T cells has never been reported in clinical trials for MM therapy.
In some cases, patients lost their eligibility for CAR-T-cell treatment due to rapid disease progression during the long vein-to-vein interval. Thus, it is critical to reduce the waiting period, especially for patients with aggressive disease. Previous studies have reported that early-harvested CAR-T cells exhibited enhanced effector function and proliferation,16 raising the feasibility of shortening the manufacturing time. Limiting the ex vivo culture time of T cells is also beneficial for maintaining the T-cell stemness that is essential for the durability of T-cell function.
Here, we constructed a BCMA CAR-T-cell with 4-1BB as the costimulatory domain, integrating an independently expressed OX40 as an armored domain (named BCMA-BBZ-OX40). An instant manufacturing platform (named InstanCART) was established, and CAR-T cells were produced within 3 days. CAR-T cells were manufactured using the InstanCART process, or traditional manufacturing process (TraditionCART). The antitumor potency, differentiation, exhaustion, and expansion levels were evaluated in vitro, and in tumor-bearing mouse models. Based on the promising preclinical data, an investigator-initiated clinical trial was conducted to further evaluate the safety, response rate, and pharmacokinetics.
Methods
Cell lines and viral vectors
The H929 and U266 cancer cell lines were purchased from the American Type Culture Collection. This H929 cell line was engineered to express firefly luciferase and green fluorescent protein (H929-LAE). The engineered H929-LAE cells were maintained in a complete medium consisting of RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS, BI), 1% penicillin and streptomycin. U266 cells were maintained in a complete medium consisting of RPMI-1640 medium supplemented with 15% FBS, BI, 1% penicillin and streptomycin. All cell lines were authenticated by short tandem repeat analysis according to supplier information.
The polymerase chain reaction products of both BCMA-BBZ-OX40 and BCMA-BBZ CAR molecules were ligated to the third-generation EF1α promoter-based lentiviral transfer plasmid pLenti6.3/V5 (Thermo Fisher, Waltham, Massachusetts, USA). Lentivirus stock was prepared by transient transfection of transfer plasmid, packaging plasmids (pLP1 and pLP2, Thermo Fisher, Waltham, Massachusetts, USA) and envelope plasmid (pLP/VSVG, Thermo Fisher, Waltham, Massachusetts, USA) into HEK293T cells using polyethyleneimine, collection of the culture medium 48 hours and 72 hours after transfection, ultrafiltration of the culture medium, and subsequent purification of the lentiviral particles using Core 700 chromatography (GE Healthcare, USA).
Generation of TraditionCART
Autologous T cells from healthy donors or patients with R/R MM were collected by leukapheresis and activated using anti-CD3 and anti-CD28 agonistic antibody-coated Dynabeads (Thermo Fisher Scientific), followed by transduction with the above lentiviral vectors for BCMA-BBZ and BCMA-BBZ-OX40 after 24 hours. Transduced T cells were expanded in cell culture using X-VIVO medium (Lonza Group, Basel, Switzerland) containing 100 U/mL interleukin-2 (IL-2). Cell counts and viability were evaluated during T-cell expansion using an automated cell counter (Thermo Fisher Scientific, USA). The transduction efficiency of CAR was assessed by flow cytometry.
Generation of InstanCART
Apheresis material from healthy donors or patients with R/R MM was passed through 30 µm nylon mesh to remove cell clumps before incubation with CD4 and CD8 MicroBeads for 15 min at 4°C (Miltenyi Biotec). Cells were washed by adding 1–2 mL of buffer per 10⁷ cells and centrifuged at 300×g for 10 min. Cell pellets were resuspended and then separated by an LS Column (Miltenyi Biotec). CD8+ and CD4+ T cells were then incubated with a suitable amount of T Cell TransAct (Miltenyi Biotec). After 24 hours, T cells were transduced with BCMA-BBZ-OX40 lentivirus and harvested 1 day later.
When generating InstanCART cells for patients, a total of 5×107 CD4/CD8 T cells were transduced with BCMA-BBZ-OX40 lentivirus at a multiplicity of infection of two and harvested 1 day later at a dose of 2×107 total T cells.
Flow cytometry
The CAR-T-cell phenotype was assessed by flow cytometry (Aurora, Cytek). Briefly, cell samples were collected, washed in phosphate-buffered saline (PBS), and stained in buffer (PBS+1% FBS) containing surface mouse-anti-human antibodies against CD3 (#300439, BioLegend), CD4 (#344644, BioLegend), CD8 (46-0087-42, Thermo), PE-labeled antibody recognizing the single-chain fragment variable (scFv) domain (from Beijing Imunopharm Technology), CD45RA (#304142, BioLegend), CD62L (#304846, BioLegend), programmed cell death protein-1 (PD-1) (#329950, BioLegend), LAG-3 (#369310, BioLegend) and OX40 (#350008, BioLegend). Data were analyzed using SpectroFlo software (Cytek).
Chronic antigen exposure model
InstanCART cells and TraditionCART cells were thawed and cultured at 1×106 cells/mL in T25 flasks with X-VIVO medium supplemented with 500 IU/mL IL-2 and 10% v/v FBS. After 24 hours, the CAR+ T cell number of TraditionCART cells was calculated using flow cytometry and 5×104 CAR+ T cells were mixed with 5×104 H929-LAE cells/well for an effector/target cell (E:T) ratio of 1:1. In the InstanCART group, the same number of total T cells as the TraditionCART cells was mixed with 5×104 H929-LAE cells regardless of CAR expression profile. Untransduced T cells were also mixed with the tumor cells. Co-cultures were maintained at a volume of 1 mL. After 2–3 days, 250 µl of the co-culture was mixed with an equal volume of fresh X-VIVO and then transferred to the new well with 5×104 H929-LAE cells. This process was repeated for 15–18 days. At the end of the assay, co-cultures were collected and analyzed for CAR+ T cell and residual tumor cells.
In vitro killing assay
To compare the cytotoxicity of CAR-T cells, CAR-T cells were serially exposed (ie, on days 1, 2, 5, and 6 after recovery) to H929-LAE tumor cells at an E:T ratio of 5:1 on day 1 and day 2 and then 10:1 on day 5 and day 6. Cell viability and proliferation were analyzed after each stimulation. After four rounds of stimulation, the residual BCMA-BBZ-OX40 CAR-T cells were mixed with U266 tumor cells. Briefly, H929 or U266 tumor cells were collected, labeled with calcein-AM (5 µg per 107 cells; Thermo Fisher Scientific), suspended in X-VIVO 15 medium (1×107 cells/mL), and added to a 48-well plate (1×105 cells/well). CAR-T cells and T cells were subsequently collected, suspended in X-VIVO 15 media, and added to the 48-well plate at different E:T ratios. After 6 hours, the plate was centrifuged, and the supernatants from each well were transferred to an ELISA plate. The fluorescence intensity (FL) of released calcein-AM in each well was detected in triplicate using a microplate reader (Varioskan LUX, Thermo Fisher Scientific; excitation, 495 nm; emission, 515 nm). For the positive control (PC), calcein-AM-labeled cell samples were lysed using 2% Triton X-100/saline. The FL of the supernatant from calcein-AM-labeled cells that were not treated with CAR-T or T cells was used as the negative control (NC). The tumor cell-killing efficiency was calculated as ((FL-NC)/(PC-NC))×100%.
Xenograft tumor model
Animal experiments were performed with 6–8 weeks-old female NPG mice (Beijing Vitalstar Biotechnology) under an approved Institutional Animal Care and Use Committee protocol. On day 0, each mouse was subcutaneously implanted with 5×106 H929-LAE tumor cells. On day 10, when the average tumor signal reached 1×104, as analyzed by live bioluminescence imaging (IVIS Spectrum, PerkinElmer, USA), the NPG mice received intravenous injection of two doses (2×106 or 5×106 CAR-T cells) of freshly recovered BCMA-BBZ TraditionCART-cells, BCMA-BBZ-OX40 TraditionCART-cells or BCMA-BBZ-OX40 InstanCART-cells. A single dose of untransduced T cells or cryopreservation medium (CM) was intravenously injected as a control. Tumor growth was monitored weekly using live bioluminescence imaging. Luciferase activity was analyzed using Living Image software V.4.5.2 (PerkinElmer). Peripheral blood was collected weekly for flow cytometric analysis of CAR-T cell levels.
Investigator-initiated clinical trial
Study design and participants
The clinical trial is a single-arm, open-label study using a non-randomized design, performed at Beijing Hospital in Beijing, China. This study was performed in accordance with the Declaration of Helsinki. Eligible patients were 18 years of age or older; had received at least two previous regimens for MM, including an immunomodulatory agent, and a proteasome inhibitor; and had disease progression after their last line of therapy according to International Myeloma Working Group (IMWG) criteria.17 Patients who had received CAR-T or BCMA-targeted treatment were excluded. Full eligibility criteria are provided in the supplemental trial protocol (see online supplemental additional file 1).
Procedures
Bridging therapy was allowed during manufacture. Lymphodepletion with 25 mg/m2 fludarabine, and 250 mg/m2 cyclophosphamide both for 3 days was given, followed by 2 days of rest. A single infusion of BCMA-BBZ-OX40 TraditionCART cells at a dose of 1×106/kg CAR+ cells, or BCMA-BBZ-OX40 InstanCART cells at a dose of 2×107 total T cells was given to each patient. Follow-up was performed from the date of CAR-T-cell infusion until the cut-off date or until the patient died. CAR-T cells and cytokines in the peripheral blood were assessed using flow cytometry analysis on days 4, 7, 14, 21, and 28 and every 12 weeks afterward.
Objectives
The primary objectives were the incidence and severity of adverse events within 1 month after CAR-T-cell infusion. Adverse events were graded using the National Cancer Institute Common Terminology Criteria for Adverse Events V.5.0. Cytokine release syndrome (CRS) and neurological toxic effects were graded using the American Society for Transplantation and Cellular Therapy consensus criteria.18 The secondary objective was the best overall response rate (ie, the percentage of patients who had a complete or partial response using IMWG criteria). Exploratory analysis included time to best response, progression-free survival (PFS), overall survival, pharmacokinetic profile, and cytokine kinetics.
Statistical analysis
Descriptive statistics are presented as the mean±SD, or medians with minimum and maximum for continuous variables, and counts and percentages for categorical variables. The baseline characteristics and adverse events of the InstanCART or TraditionCART group were compared using the independent samples t-test, Wilcoxon signed-rank test (for continuous variables), or χ2 test (for nominal variables) as appropriate. The PFS and overall survival were estimated using the Kaplan-Meier method. P values less than 0.05 were considered statistically significant. Statistical analyses were performed using Stata V.17.0 (StataCorp, College Station, Texas, USA), and SPSS V.25.0 (SPSS, Chicago, Illinois, USA).
Results
Patient characteristics
Between October 2019 and August 2023, 22 patients were enrolled and underwent apheresis. The manufacturing was successful for 100% of the patients, and all patients finished CAR-T therapy. The characteristics of the patients are shown in table 1, and online supplemental tables 1 and 2. The median age was 62.5 years (range, 45.0–78.0). Patients had received a median of three lines of previous therapies (range, 2–7), and 15 (68%) were triple-class refractory (refractory to immunomodulatory drugs, proteasome inhibitors, and anti-CD38 monoclonal antibodies). Up to 50% of patients had a high-risk cytogenetic profile, defined as the presence of del(17p), t(4;14), or t(14;16), and 36% had extramedullary disease, defined as the presence of soft-tissue plasmacytomas that result from hematogenous spread19 (detailed extramedullary disease and paraskeletal plasmacytoma is shown in online supplemental table 1). All treated patients still had measurable disease before lymphodepletion.
Table 1. Baseline characteristics.
| Total (n=22) | InstanCART group (n=7) | TraditionCART group (n=15) | P value | |
| Age, median (range) | 62.5 (45.0–78.0) | 62.0 (45.0–78.0) | 63.0 (54.0–73.0) | 0.68 |
| Male sex, no. (%) | 8 (36) | 2 (29) | 6 (40) | 0.97 |
| Immunoglobulin subtype, no. (%) | 0.44 | |||
| IgA | 11 (50) | 2 (29) | 9 (60) | |
| IgG | 6 (27) | 3 (43) | 3 (20) | |
| IgD | 1 (5) | 1 (14) | 0 | |
| Light chain only | 4 (18) | 1 (14) | 3 (20) | |
| Years since diagnosis, median (range) | 2.9 (0.8–14.7) | 3.4 (0.8–13.0) | 2.5 (1.2–14.7) | 0.96 |
| Prior lines of therapy, median (range) | 3 (2–7) | 3 (2–7) | 3 (2–7) | 0.79 |
| Triple-class refractory, no. (%) | 15 (68) | 5 (71) | 10 (67) | 1.00 |
| Previous autologous stem-cell transplantation, no. (%) | 9 (41) | 4 (57) | 5 (33) | 0.55 |
| Soft tissue plasmacytoma, no. (%) | 13 (59) | 4 (57) | 9 (60) | 1.00 |
| Extramedullary disease | 8 (36) | 3 (43) | 5 (33) | 0.96 |
| Cytogenetic risk category, no. (%) | ||||
| High risk cytogenetic profile | 11 (50) | 4 (57) | 7 (47) | 1.00 |
| Deletion 17p | 7 (32) | 1 (14) | 6 (40) | |
| t(4;14) | 6 (27) | 3 (43) | 3 (20) | |
| amp(1q) | 13 (59) | 4 (57) | 9 (60) | |
| t(11;14) | 4 (18) | 1 (14) | 3 (20) | |
| Absolute neutrophil count, no. (%) | 1.00 | |||
| ≥1.0×109/L | 19 (86) | 6 (86) | 13 (87) | |
| <1.0×109/L | 3 (14) | 1 (14) | 2 (13) | |
| Hemoglobin, no. (%) | 0.30 | |||
| ≥100 g/L | 8 (36) | 1 (14) | 7 (47) | |
| 80–<100 g/L | 9 (41) | 4 (57) | 5 (33) | |
| <80 g/L | 5 (23) | 2 (29) | 3 (20) | |
| Platelets, no. (%) | 0.80 | |||
| ≥100×109/L | 11 (50) | 4 (57) | 7 (47) | |
| 50–<100×109/L | 5 (23) | 1 (14) | 4 (27) | |
| <50×109/L | 6 (27) | 2 (29) | 4 (27) | |
| Creatinine clearance in mL/min, median (range) | 74.2 (23.7–151.1) | 84.5 (23.7–151.1) | 60.1 (33.5–124.1) | 0.18 |
| Bone marrow plasma cells burden, % (range) | 18.0 (0–95.5) | 37.0 (0–95.5) | 16.0 (1.2–14.7) | 0.21 |
| ECOG performance-status score, no. (%) | 0.21 | |||
| 0 | 6 (27) | 3 (43) | 3 (20) | |
| 1 | 7 (32) | 3 (43) | 4 (27) | |
| 2 | 3 (14) | 1.0 (14) | 2 (13) | |
| 3 | 4 (18) | 0 | 4.0 (27) | |
| 4 | 2 (9) | 0 | 2 (13) | |
| Bridging therapy, no. (%) | 10.0 (45.5) | 4.0 (57.1) | 6.0 (40.0) | 0.77 |
ECOGEastern Cooperative Oncology GroupInstanCARTinstant manufacturing platformTraditionCARTtraditional manufacturing process
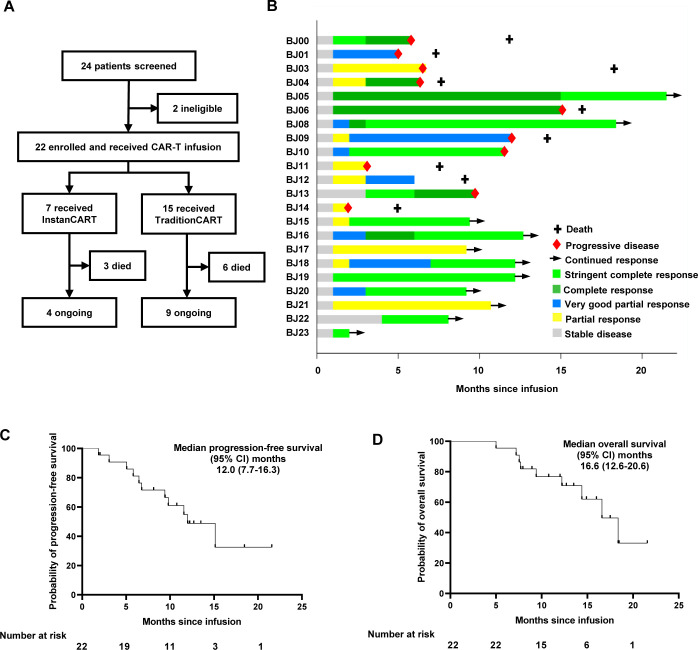
Seven (32%) patients received InstanCART infusion, and 15 (68%) patients received TraditionCART infusion (figure 1A). There were no statistically significant differences in baseline characteristics between the InstanCART group and the TraditionCART group (table 1). The median time from manufacturing initiation to the final product was 10 days (range 8–13), and the median time from manufacturing initiation to cell infusion was 17 days (range 13–42) in the TraditionCART group. In contrast, the time from manufacturing initiation to the final product was 3 days (p<0.001), and the median time from manufacturing initiation to cell infusion was 11 days (range 7–18, p=0.01) in the InstanCART group.
Figure 1. Trial profile, patient response and survival to CAR-T-cell infusion. (A) Trial profile; (B) patient response after CAR-T infusion; (C) Kaplan-Meier plot of progression-free survival; (D) Kaplan-Meier plot of overall survival. CAR-T-cell, chimeric antigen receptor T cell; InstanCART, instant manufacturing platform; TraditionCART, traditional manufacturing process.
Safety
All 22 patients had adverse events during the first month (table 2). Hematologic toxic events were the most common, ≥grade 3 hematologic adverse events including neutropenia (20 (91%) of 22 patients), anemia (12 (55%)), and thrombocytopenia (15 (68%)). Transient increases in creatinine were observed in 4 (18%) of 22 patients, 1 of whom (5%) exhibited a grade 3 increase. Transient hepatic enzyme elevation occurred in 12 (55%) patients, 5 of whom (23%) exhibited grade 3–4 elevation. Infections occurred in nine (41%) patients, including diarrhea, upper respiratory tract infection, and sepsis. One (5%) of 22 patients experienced grade 3 sepsis. CRS occurred in 19 (86%) of 22 patients, and no grade 3–4 CRS was observed. A total of 18 (82%) patients received tocilizumab, and 9 (41%) received dexamethasone. Neurological toxic effects were observed in two (9%) patients, and both were grade 1. All symptoms of CRS and neurotoxicity were reversible. TraditionCART therapy caused grade 1–2 CRS in 12 (80%) patients, and neurotoxicity in 1 (7%) patient. Meanwhile, InstanCART therapy induced grade 1–2 CRS in seven (100%) patients, and neurotoxicity in one (14%) patient. Adverse events, including CRS and neurological toxicity, were comparable between the InstanCART group and the TraditionCART group (table 2).
Table 2. Adverse events, cytokine release syndrome, and neurological toxic effects.
| Total (n=22) no. (%) | InstanCART group (n=7) no. (%) | TraditionCART group (n=15) no. (%) | ||||
| Any grade | Grade 3–4 | Any grade | Grade 3–4 | Any grade | Grade 3–4 | |
| Any adverse event* | 22 (100) | 21 (95) | 7 (100) | 7 (100) | 15 (100) | 14 (93) |
| Cytokine release syndrome | 19 (86) | 0 | 7 (100) | 0 | 12 (80) | 0 |
| Neurological toxic effect | 2 (9) | 0 | 1 (14) | 0 | 1 (7) | 0 |
| Neutropenia | 22 (100) | 20 (91) | 7 (100) | 6 (86) | 15 (100) | 14 (93) |
| Anemia | 22 (100) | 12 (55) | 7 (100) | 2 (29) | 15 (100) | 10 (67) |
| Thrombocytopenia | 22 (100) | 15 (68) | 7 (100) | 6 (86) | 12 (80) | 9 (60) |
| Creatinine increased | 4 (18) | 1 (5) | 0 | 0 | 4 (27) | 1 (7) |
| Hepatic enzymes increased | 12 (55) | 5 (23) | 4 (57) | 3 (43) | 8 (53) | 2 (13) |
| Diarrhea | 6 (27) | 0 | 3 (43) | 0 | 3 (20) | 0 |
| Upper respiratory tract infection | 2 (9) | 0 | 1 (14) | 0 | 3 (20) | 0 |
| Sepsis | 1 (5) | 1 (5) | 0 | 0 | 1 (7) | 1 (7) |
Shown are adverse events that occurred during the first 1 month month after CAR-T infusion.
CAR-Tchimeric antigen receptor T cellInstanCARTinstant manufacturing platformTraditionCARTtraditional manufacturing process
The median duration of follow-up after CAR-T infusion was 12.2 months (range, 5.0–21.6), and 11 (50%) patients acquired COVID-19 infection, including three patients with recurrent infection. COVID-19 severity was mild in eight (73%) of the patients, moderate in two (18%), and severe/critical in one (9%). Three patients developed hypoxia, and one needed mechanical ventilation. The median time to clear COVID-19 infection was 10 (range 7–50) days. One patient died of pneumothorax and respiratory failure due to COVID-19 infection.
Response and survival
The best overall response rate was 100%, and 14 (64%) of 22 patients had a complete response (2 (9%)) or stringent complete response (12 (55%)) (table 3). The best overall response rate of patients with high-risk cytogenetic and extramedullary disease was also 100%; 6 (55%) of 11 patients with high-risk cytogenetic, and 3 (38%) of 8 with extramedullary disease reached complete response or stringent complete response. Five of seven available patients reached minimal residual disease (MRD) negativity (at a sensitivity of at least one in 104 nucleated cells; limit of detection of at least 1×10-4) as assessed by eight-color flow cytometry done at the first pull of each aspirate by single tube.
Table 3. Tumor response.
| Total (n=22) | InstanCART group (n=7) | TraditionCART group (n=15) | P value | |
| Objective response, no. (%) | 22 (100) | 7 (100) | 15 (100) | 1.00 |
| Months to best response, median (range) | 2.0 (1.0–15.0) | 2.0 (1.0–3.0) | 2.0 (1.0–15.0) | 0.58 |
| Best overall response, no. (%) | 0.32 | |||
| Stringent complete response | 12 (55) | 3 (43) | 9 (60) | |
| Complete response | 2 (9) | 0 | 2 (13) | |
| Very good partial response | 3 (14) | 1 (14) | 2 (13) | |
| Partial response | 5 (23) | 3 (43) | 2 (13) | |
| Progression-free survival, months, median (95% CI) | 12.0 (7.7 to 16.3) | 9.8 (9.0 to 10.6) | 15.1 (9.5 to 20.8) | 0.10 |
| Overall survival, months, median (95% CI) | 16.6 (12.6 to 20.6) | Not reached | 16.6 (12.0 to 21.2) | 0.62 |
| Follow-up time, months, median (95% CI) | 12.2 (5.0 to 21.6) | 13.5 (5.0 to 17.5) | 12.2 (7.2 to 21.6) | 0.81 |
InstanCARTinstant manufacturing platformTraditionCARTtraditional manufacturing process
At a median follow-up of 12.2 months (range, 5.0–21.6), a total of 10 (45%) patients had disease progression, and 11 patients had ongoing responses (figure 1B). The median PFS was 12.0 months (95% CI, 7.7 to 16.3) (figure 1C). The median overall survival was 16.6 months (95% CI, 12.6 to 20.6) (figure 1D). Nine deaths occurred during the study after CAR-T infusion. Eight deaths were due to disease progression, and one death resulted from severe COVID-19 infection and pneumothorax. There were no statistically significant differences in PFS and overall survival between InstanCART group and TraditionCART group (table 3).
CAR-T cell expansion and cytokine analysis
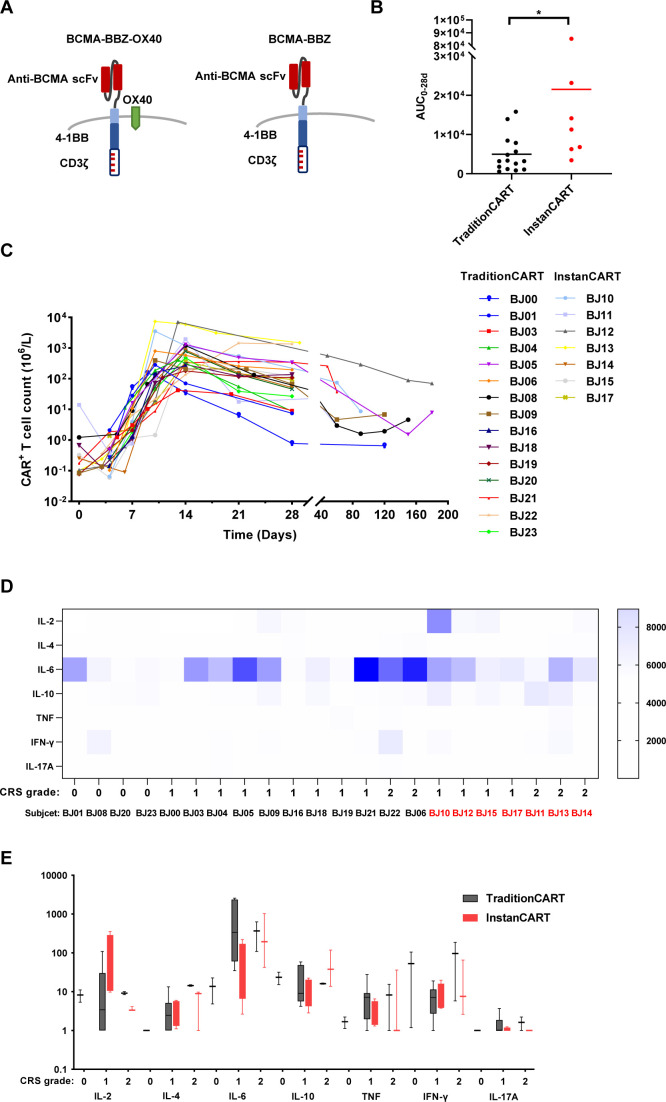
The TraditionCART and InstanCART treatments given to patients were based on a BCMA-BBZ-CAR with independently expressed OX40 using different manufacturing processes (figure 2A). The median time to peak expansion was 14 days in both the InstanCART group and the TraditionCART group. The expansion and duration of InstanCART cells (Cmax=314×107/L; AUC0–28d=2149×107/L) were dramatically higher than those of TraditionCART cells (Cmax=54×107/L, p=0.005; AUC0–28d=495×107/L, p=0.01) (figure 2B). The post-infusion kinetics of peripheral CAR-T-cell expansion and persistence are displayed in figure 2C. The kinetics of serum cytokines and CRS grade of each patient are displayed in figure 2D. Higher-grade CRS was associated with a greater fold change in the levels of these analytes from baseline level to peak level after CAR-T treatments (figure 2E).
Figure 2. CAR-T-cell expansion, persistence, and cytokine analysis in patients. (A) Schematic of BCMA-BBZ-OX40 and BCMA-BBZ CAR constructs; (B) comparison of the AUC0–28d between InstanCART and TraditionCART group. AUC0–28d, area under the curve of CAR-T cell expansion from d0 to d28; bars indicate mean of AUC0–28d of different patients, *p<0.05; (C) CAR-T-cell pharmacokinetics; (D) heatmaps indicating peak values of cytokines grouped by individual patients; (E) boxplots depicting fold changes in proinflammatory cytokine production from pre-infusion to the peak of CAR-T-cell expansion; boxplots indicate the range of the central 50% of the data, with the central line marking the median value; whiskers extend from each box to show the range of the remaining data. *p<0.05 by unpaired t-test. AUC, area under the curve; BCMA, B-cell maturation antigen; CAR-T-cell, chimeric antigen receptor T cell; CRS, cytokine release syndrome; IL, interleukin; InstanCART, instant manufacturing platform; scFv, single-chain fragment variable; TNF, tumor necrosis factor; TraditionCART, traditional manufacturing process.
Independently expressed OX40 enhanced BCMA CAR-T-cell function in vitro and in vivo
Using the second-generation BCMA-BBZ CAR as a reference, we first addressed the impact of independently expressed OX40 by generating BCMA-BBZ-OX40 CAR (figure 2A). Comparable surface CAR expression was observed on both CAR-T cells, while BCMA-BBZ-OX40 CAR-T cells showed more than 90% OX40 expression on CAR+ T cells (online supplemental figure 1A). Notably, BCMA-BBZ-OX40 CAR-T cells eradicated H929 and U266 tumor cells more potently than BCMA-BBZ CAR-T cells (online supplemental figure 1B). Furthermore, we thus examined the abundance of exhaustion-related cell surface markers PD-1 and LAG-3 in antigen-stimulated CAR-T cells. After stimulation by U266 cells for 4 days, the proportion of cells positive for PD-1 and LAG-3 was lower for both CD4+ and CD8+ BCMA-BBZ-OX40 CAR-T cells than for BCMA-BBZ CAR-T cells (online supplemental figure 1C). Furthermore, BCMA-BBZ-OX40 CAR-T cells comprised higher CD45RA+ CD62L+ T-cell subsets than BCMA-BBZ CAR-T cells after U266 stimulation (online supplemental figure 1D). The reduction in these immune checkpoint inhibitors and the low differentiation status of CAR-T cells due to OX40 expression could contribute to a higher ratio of functional T cells when stimulated with BCMA+ target cells.
To further evaluate the efficacy of the two BCMA-CAR-T cells in vivo, H929-LAE were transplanted into NPG mice, followed by a single intravenous infusion of CM, untransduced T cells, BCMA-BBZ, or BCMA-BBZ-OX40 CAR-T cells (online supplemental figure 2A). On day 89 after CAR-T-cell injection, both BCMA-CAR-T cells eliminated the H929 tumors (online supplemental figure 2B, C). We observed comparable persistence of BCMA-BBZ CAR-T cells and BCMA-BBZ-OX40 CAR-T cells in the peripheral blood of tumor-bearing mice (online supplemental figure 2D). Though not statistically significant, BCMA-BBZ-OX40 CAR-T cells prolonged the overall survival of H929 tumor-bearing mice compared with BCMA-BBZ CAR-T cells (online supplemental figure 2E). Altogether, these findings demonstrate that independently expressed OX40 confer BCMA CAR-T cells with more favorable antitumor function.
Reduction of the manufacturing time improved CAR-T-cell function in vitro and in vivo
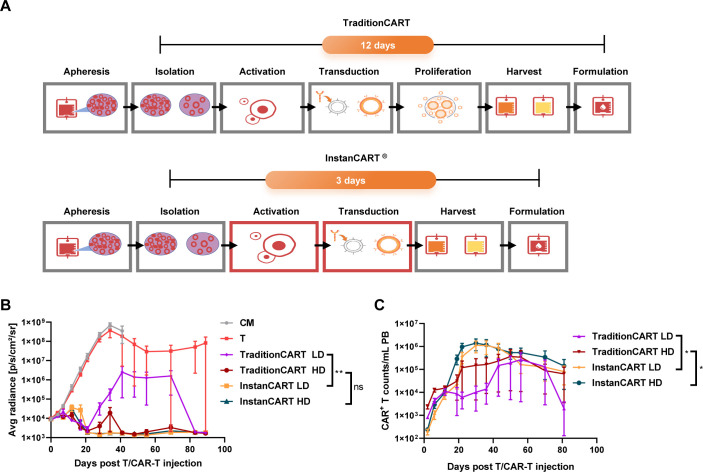
Currently, the median manufacturing time of CAR T cells is approximately 7–12 days from apheresis to final formulation. We developed a novel manufacturing process that shortens the manufacturing period to 3 days (figure 3A). The BCMA-BBZ-OX40 CAR-T cells were harvested and cryopreserved at various time points using the TraditionCART or InstanCART process. While InstanCART cells showed a relatively low viability compared with TraditionCART cells after recovery, their viability surpassed that of TraditionCART cells after a 7-day culture period (online supplemental figure 3A). Furthermore, InstanCART exhibited enhanced proliferation compared with TraditionCART (online supplemental figure 3B). InstanCART-derived cells retained more naïve and stem cell memory immunophenotypes and fewer effector immunophenotypes on day 7 after recovery (online supplemental figure 3C).
Figure 3. Reduction of the manufacturing time improved CAR-T-cell function in vitro and in vivo. (A) The general procedure for manufacturing InstanCART and TraditionCART; (B) Flux (p/s) values of tumor burden assessed by IVIS imaging; (C) CAR+ T-cell counts of CAR-T cells in the PB of mice at different time points after CAR-T treatment. LD indicated 2×106 CAR+ T cells in the TraditionCART group and 2×106 total T cells in the InstanCART group. HD indicated 5×106 CAR+ T cells in the TraditionCART group and 5×106 total T cells in the InstanCART group. *p<0.05, **p<0.01, not significant by unpaired Mann-Whitney test. CAR-T-cell, Chimeric antigen receptor T cell; CM, cryopreservation medium; InstanCART, instant manufacturing platform; PB, peripheral blood; TraditionCART, traditional manufacturing process.
To test whether the instant manufacturing process enhances the cytotoxicity of CAR-T cells, we analyzed the cytotoxic effect of TraditionCART or InstanCART cell after serially stimulated with H929-LAE cells (online supplemental figure 3D). After four stimulations with H929-LAE, both the viability and expansion of InstanCART-derived cells outperformed those of TraditionCART-derived cells (online supplemental figure 3E). Moreover, InstanCART cells comprised more cells belonging to the naïve and stem cell memory phenotype (online supplemental figure 3F). After four serial tumor cell stimulations, InstanCART cells killed more U266 cells than TraditionCART cells (online supplemental figure 3G). To determine whether shortening manufacturing time could delay CAR-T dysfunction, we deployed the chronic antigen exposure model.20 In this assay, CAR-T cells were repeatedly stimulated with H929-LAE cells (online supplemental figure 3H). Importantly, InstanCART cells show decreased tumor cells and increased CAR+ T cells, compared with TraditionCART cells (online supplemental figure 3I). The above results indicate that InstanCART cells killed BCMA+ tumor cells more effectively in vitro than TraditionCART cells.
In the NPG mouse model, mice were treated with TraditionCART cells at levels of either 2×106 (LD) or 5×106 (HD) CAR+ T cells, while they were treated with InstanCART cells at levels of either 2×106 (LD) or 5×106 (HD) total T cells. Thus, the CAR+ T-cell dose level of InstanCART cells was lower than that of TraditionCART cells. CM-treated mice exhibited a rapid increase in bioluminescent signal, necessitating euthanasia approximately 40 days after tumor inoculation. The tumor burden of the LD-InstanCART group were significantly lower than those of the TraditionCART group on day 28 and day 41 after CAR-T treatments (figure 3B). Furthermore, at both doses, InstanCART cells exhibited enhanced peripheral blood CAR-T-cell proliferative capacity compared with TraditionCART cells (figure 3C). Taken together, these experiments demonstrated that the InstanCART process was beneficial for CAR-T-cell proliferation, maintenance of stemness, and antitumor function compared with the TraditionCART process.
Discussion
In this study, we generated OX40-containing BCMA CAR-T cells, and developed a novel manufacturing process that shortened the manufacturing period to 3 days, with enhanced in vivo and in vitro antitumor capacity. These BCMA-BBZ-OX40 CAR-T cells were successfully administered to 22 patients with heavily pretreated R/R MM. The expansion and duration of InstanCART cells were higher than those of TraditionCART cells. All patients had a clinical response, and 64% of the patients had a complete response or better. No grade 3 or worse CRS or neurological toxic effects were reported.
The OX40L-OX40 signaling axis has favorable effects on T-cell activation, proliferation, low differentiation, and survival.4,7 The inclusion of OX40 in the design of CAR-T cells is thought to improve cytotoxicity and antigen-dependent memory formation.12 In this study, we independently expressed the OX40 molecule in BCMA CAR-T cells. Consistent with previous reports, we found that the tumor-killing efficiency was significantly improved, and exhaustion and effector differentiation were reduced. Since the low differentiation status indicated the maintenance of T-cell stemness, and durable function of T cells, our data support the idea that the constitutive expression of OX40 is beneficial for BCMA CAR-T-cell function.
The establishment of a faster-manufactured platform offers the potential to shorten the time needed before administration of the product. CAR-T cells are manufactured ex vivo, and the process can take as little as 7 days to as long as 6 weeks.1 21 22 Heavily pretreated patients often deteriorate rapidly, and some patients even regretfully lose eligibility.23 In the CARTITUDE-1 study, 14% of enrolled patients did not receive CAR-T infusion due to disease progression, death, or study withdrawal after apheresis.24 Thus, the potentially long time between apheresis and product manufacturing is considered one of the major obstacles in autologous anti-BCMA CAR-T-cell therapy.25 Thus, shortening the duration between apheresis and CAR-T infusion is critical for patients. Recently, novel CAR-T manufacturing processes were developed with significantly shortened ex vivo culture time and comparable potency in the clinic.26,28 In the present study, the time from manufacturing initiation to the final product by InstanCART process was as short as 3 days. InstanCAR-T cells have superior antitumor activity and proliferation capacity, even at a relatively low dose, which may offer a fast and effective solution to enhance the persistence and functionality of CAR-T cells in MM treatment.
The outcome after a single CAR-T infusion was encouraging in this study with a 100% best overall response rate, PFS of 12.0 months, and 12-month PFS of 49%. The median PFS with ide-cel was 12.1 months at the 4.50×108 dose,29 and PFS was 66% at 18 months of cilta-cel.24 A total of 13–39% of patients had extramedullary disease, and 24–35% of patients had a high-risk cytogenetic profile in the CARTITUDE-1 and KarMMa studies.24 29 Notably, the proportion of high-risk patients was higher in the present trial, as 36% of the enrolled patients had extramedullary disease and 50% of the patients had a high-risk cytogenetic profile. The presence of soft tissue plasmacytoma represents an aggressive form of MM, the Mayo Clinic reported that patients with secondary extramedullary disease treated with CAR-T therapy (n=20) achieved a median PFS of 4.9 months (3.1 months-not reached).30 The long-term efficacy of anti-BCMA CAR-T-cell therapy was worse in patients with extramedullary disease than in patients without soft tissue plasmacytoma, and with paraskeletal plasmacytoma.31,33 In our study, the median PFS of patients with extramedullary disease was 5.8 months, while the median PFS of patients without extramedullary disease was 15.1 months. Although the expansion and duration of InstanCART cells were higher than those of TraditionCART cells, treatment with the InstanCART cells did not show a superior survival outcome. The possible reason is that one patient in remission with InstanCART therapy died from COVID-19 infection. Due to the small sample size, definite conclusions about the clinical efficacy of InstanCART could not be drawn thus far.
The observed toxic effects were consistent with previous studies.24 29 34 CRS and neurotoxic effects of grade 3 or higher were not recorded. Adverse events, CRS and neurotoxic effects were comparable between patients who received InstanCART therapy and those who received TraditionCART therapy. Patients with hematological malignancies experience high mortality from COVID-19, with a longer duration of time to the first negative test.35 Half of the patients acquired COVID-19 infection, and one patient died of pneumothorax and respiratory failure due to COVID-19 infection in our study. Early antiviral treatment should be considered in this immunosuppressive population.
The present study has several limitations. First, the data were collected from a single academic center with a small sample size. In addition, a large portion of the patients could not be evaluated for MRD. Further investigations, including escalation studies, are warranted to identify the maximum tolerated dose. The clinical study is ongoing, and long-term follow-up will further inform the clinical efficacy, safety, and persistence of CAR-T cells.
Conclusions
In summary, BCMA-BBZ-OX40 CAR-T cells were more persistent in vitro and in vivo, and were well tolerated in heavily pretreated patients with R/R MM. InstanCART therapy had a shortened waiting time, and a comparable response rate compared with TraditionCART therapy. BCMA-BBZ-OX40 CAR-T cells are a potential treatment option for patients with R/R MM, and the InstanCART provides a treatment opportunity for rapidly progressive patients.
supplementary material
Footnotes
Funding: This study was supported by grant (No. BJ-2022-127) from the National High Level Hospital Clinical Research Funding, grant (No. 7232137) from the Beijing Natural Science Foundation, and grant (No. 2021-I2M-C&T-A-020) from the CAMS Innovation Fund for Medical Sciences (CIFMS). The funders had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: An independent ethics committee at Beijing Hospital approved the study protocol (2020BJYYEC-162-03). Participants gave informed consent to participate in the study before taking part.
Contributor Information
Ting Wang, Email: wangting9798@126.com.
Yazi Yang, Email: 18810560236@163.com.
Lie Ma, Email: maliehehe@126.com.
Ru Feng, Email: frbld@sina.com.
Jiangtao Li, Email: ljtxj@sina.com.
Chunli Zhang, Email: zclcontrol@sina.com.
Jiefei Bai, Email: baijf1985@126.com.
Yanping Ding, Email: dingyanping@imunopharm.com.
Guanghua Liu, Email: liuguanghua@imunopharm.com.
Fei Wu, Email: wufei@imunopharm.com.
Xinan Lu, Email: luxinan@imunopharm.com.
Shi Feng, Email: fengshi@imunopharm.com.
Zhenling Li, Email: zryyxy2013@163.com.
Ting He, Email: heting@imunopharm.com.
Jian Li, Email: lijian@pumch.cn.
Hui Liu, Email: liuhui8140@126.com.
Data availability statement
Data are available upon reasonable request.
References
- 1.Mikkilineni L, Kochenderfer JN. CAR T cell therapies for patients with multiple myeloma. Nat Rev Clin Oncol. 2021;18:71–84. doi: 10.1038/s41571-020-0427-6. [DOI] [PubMed] [Google Scholar]
- 2.Chen L, Flies DB. Molecular mechanisms of T cell co-stimulation and co-inhibition. Nat Rev Immunol. 2013;13:227–42. doi: 10.1038/nri3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Q, Vignali DAA. Co-stimulatory and Co-inhibitory Pathways in Autoimmunity. Immunity. 2016;44:1034–51. doi: 10.1016/j.immuni.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers PR, Song J, Gramaglia I, et al. OX40 promotes Bcl-xL and Bcl-2 expression and is essential for long-term survival of CD4 T cells. Immunity. 2001;15:445–55. doi: 10.1016/s1074-7613(01)00191-1. [DOI] [PubMed] [Google Scholar]
- 5.Salek-Ardakani S, Song J, Halteman BS, et al. OX40 (CD134) controls memory T helper 2 cells that drive lung inflammation. J Exp Med. 2003;198:315–24. doi: 10.1084/jem.20021937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.So T, Song J, Sugie K, et al. Signals from OX40 regulate nuclear factor of activated T cells c1 and T cell helper 2 lineage commitment. Proc Natl Acad Sci U S A. 2006;103:3740–5. doi: 10.1073/pnas.0600205103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song J, So T, Cheng M, et al. Sustained survivin expression from OX40 costimulatory signals drives T cell clonal expansion. Immunity. 2005;22:621–31. doi: 10.1016/j.immuni.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Arch RH, Thompson CB. 4-1BB and Ox40 are members of a tumor necrosis factor (TNF)-nerve growth factor receptor subfamily that bind TNF receptor-associated factors and activate nuclear factor kappaB. Mol Cell Biol. 1998;18:558–65. doi: 10.1128/MCB.18.1.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawamata S, Hori T, Imura A, et al. Activation of OX40 signal transduction pathways leads to tumor necrosis factor receptor-associated factor (TRAF) 2- and TRAF5-mediated NF-kappaB activation. J Biol Chem. 1998;273:5808–14. doi: 10.1074/jbc.273.10.5808. [DOI] [PubMed] [Google Scholar]
- 10.So T, Choi H, Croft M. OX40 complexes with phosphoinositide 3-kinase and protein kinase B (PKB) to augment TCR-dependent PKB signaling. J Immunol. 2011;186:3547–55. doi: 10.4049/jimmunol.1003156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.So T, Croft M. Regulation of PI-3-Kinase and Akt Signaling in T Lymphocytes and Other Cells by TNFR Family Molecules. Front Immunol. 2013;4:139. doi: 10.3389/fimmu.2013.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Honikel MM, Olejniczak SH. Co-Stimulatory Receptor Signaling in CAR-T Cells. Biomolecules. 2022;12:1303. doi: 10.3390/biom12091303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan J, Jia Y, Zhou M, et al. Chimeric antigen receptors containing the OX40 signalling domain enhance the persistence of T cells even under repeated stimulation with multiple myeloma target cells. J Hematol Oncol. 2022;15:39. doi: 10.1186/s13045-022-01244-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang H, Li F, Cao J, et al. A chimeric antigen receptor with antigen-independent OX40 signaling mediates potent antitumor activity. Sci Transl Med. 2021;13:eaba7308. doi: 10.1126/scitranslmed.aba7308. [DOI] [PubMed] [Google Scholar]
- 15.Wang J, Zhang X, Zhou Z, et al. A novel adoptive synthetic TCR and antigen receptor (STAR) T-Cell therapy for B-Cell acute lymphoblastic leukemia. Am J Hematol. 2022;97:992–1004. doi: 10.1002/ajh.26586. [DOI] [PubMed] [Google Scholar]
- 16.Ghassemi S, Nunez-Cruz S, O’Connor RS, et al. Reducing Ex Vivo Culture Improves the Antileukemic Activity of Chimeric Antigen Receptor (CAR) T Cells. Cancer Immunol Res. 2018;6:1100–9. doi: 10.1158/2326-6066.CIR-17-0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17:e328–46. doi: 10.1016/S1470-2045(16)30206-6. [DOI] [PubMed] [Google Scholar]
- 18.Lee DW, Santomasso BD, Locke FL, et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol Blood Marrow Transplant. 2019;25:625–38. doi: 10.1016/j.bbmt.2018.12.758. [DOI] [PubMed] [Google Scholar]
- 19.Bladé J, Beksac M, Caers J, et al. Extramedullary disease in multiple myeloma: a systematic literature review. Blood Cancer J. 2022;12:45. doi: 10.1038/s41408-022-00643-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Good CR, Aznar MA, Kuramitsu S, et al. An NK-like CAR T cell transition in CAR T cell dysfunction. Cell. 2021;184:6081–100. doi: 10.1016/j.cell.2021.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadelain M, Rivière I, Riddell S. Therapeutic T cell engineering. Nature New Biol. 2017;545:423–31. doi: 10.1038/nature22395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levine BL, Miskin J, Wonnacott K, et al. Global Manufacturing of CAR T Cell Therapy. Mol Ther Methods Clin Dev. 2017;4:92–101. doi: 10.1016/j.omtm.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parikh RH, Lonial S. Chimeric antigen receptor T-cell therapy in multiple myeloma: A comprehensive review of current data and implications for clinical practice. CA Cancer J Clin. 2023;73:275–85. doi: 10.3322/caac.21771. [DOI] [PubMed] [Google Scholar]
- 24.Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398:314–24. doi: 10.1016/S0140-6736(21)00933-8. [DOI] [PubMed] [Google Scholar]
- 25.Martino M, Canale FA, Alati C, et al. CART-Cell Therapy: Recent Advances and New Evidence in Multiple Myeloma. Cancers (Basel) 2021;13:2639. doi: 10.3390/cancers13112639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dickinson MJ, Barba P, Jäger U, et al. A Novel Autologous CAR-T Therapy, YTB323, with Preserved T-cell Stemness Shows Enhanced CAR T-cell Efficacy in Preclinical and Early Clinical Development. Cancer Discov. 2023;13:1982–97. doi: 10.1158/2159-8290.CD-22-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang J, He J, Zhang X, et al. Next-day manufacture of a novel anti-CD19 CAR-T therapy for B-cell acute lymphoblastic leukemia: first-in-human clinical study. Blood Cancer J. 2022;12:104. doi: 10.1038/s41408-022-00694-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang C, He J, Liu L, et al. Novel CD19 chimeric antigen receptor T cells manufactured next-day for acute lymphoblastic leukemia. Blood Cancer J. 2022;12:96. doi: 10.1038/s41408-022-00688-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Munshi NC, Anderson LD, Shah N, et al. Idecabtagene Vicleucel in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2021;384:705–16. doi: 10.1056/NEJMoa2024850. [DOI] [PubMed] [Google Scholar]
- 30.Zanwar S, Ho M, Lin Y, et al. Natural history, predictors of development of extramedullary disease, and treatment outcomes for patients with extramedullary multiple myeloma. Am J Hematol. 2023;98:1540–9. doi: 10.1002/ajh.27023. [DOI] [PubMed] [Google Scholar]
- 31.Li W, Liu M, Yuan T, et al. Efficacy and follow-up of humanized anti-BCMA CAR-T cell therapy in relapsed/refractory multiple myeloma patients with extramedullary-extraosseous, extramedullary-bone related, and without extramedullary disease. Hematol Oncol. 2022;40:223–32. doi: 10.1002/hon.2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Y, Sun Z, Qu X. Advances in the treatment of extramedullary disease in multiple myeloma. Transl Oncol. 2022;22:101465. doi: 10.1016/j.tranon.2022.101465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cappell KM, Kochenderfer JN. Long-term outcomes following CAR T cell therapy: what we know so far. Nat Rev Clin Oncol. 2023;20:359–71. doi: 10.1038/s41571-023-00754-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brudno JN, Kochenderfer JN. Recent advances in CAR T-cell toxicity: Mechanisms, manifestations and management. Blood Rev. 2019;34:45–55. doi: 10.1016/j.blre.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McNerney KO, Richards RM, Aguayo-Hiraldo P, et al. SARS-CoV-2 infections in pediatric and young adult recipients of chimeric antigen receptor T-cell therapy: an international registry report. J Immunother Cancer. 2023;11:e005957. doi: 10.1136/jitc-2022-005957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.