Abstract
Study Design
Retrospective cohort study.
Objectives
In patients undergoing adult spinal deformity (ASD) surgery we sought to: 1) report preoperative and postoperative lumbosacral fractional (LSF) curve and maximum coronal Cobb angles and 2) determine their impact on radiographic, clinical, and patient-reported outcomes (PROs).
Methods
A single-institution cohort study was undertaken. The LSF curve was the cobb angle between the sacrum and most tilted lower lumbar vertebra. Coronal/sagittal vertical axis (CVA/SVA) were collected. Patients were compared between 4 groups: 1) Neutral Alignment (NA); 2) coronal malalignment only (CM); 3) Sagittal malalignment only (SM); and 4) Combined-Coronal-Sagittal-Malalignment (CCSM). Outcomes including postoperative CM, postoperative coronal vertical axis, complications, readmissions, reoperation, and PROs.
Results
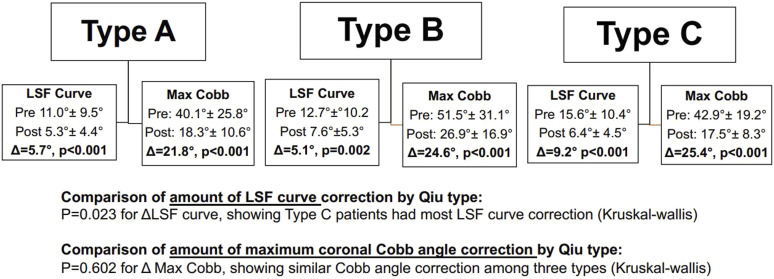
A total of 243 patients underwent ASD surgery with mean total instrumented levels of 13.5. Mean LSF curve was 12.1±9.9°(0.2-62.3) and mean max Cobb angle was 43.0±26.5° (0.0-134.3). The largest mean LSF curves were seen in patients with CM (14.6°) and CCSM (13.1°) compared to NA (12.1°) and SM (9.5°) (p=0.100). A higher LSF curve was seen in patients with fusion to the sacrum and instrumentation to the pelvis (p=0.009), and a higher LSF curve was associated with more TLIFs (p=0.031). Postoperatively, more TLIFs were associated with greater amount of LSF curve correction (p<0.001). Comparing the LSF and the max Cob angle among Qiu types, the highest mean max Cobb angle was in Qiu Type B patients (p=0.025), whereas the highest mean LSF curve was in Qiu Type C patients (p=0.037). Moreover, 82.7% of patients had a LSF curve opposite the max Cobb angle. The LSF curve was larger than the max Cobb angle in 22/243 (9.1%) patients, and most of these 22 patients were Qiu Type A (59.1%). Regarding correction, the max Cobb angle achieved more correction than the LSF curve, judged by the percent improved from preop (54.5% Cobb vs. 46.5% LSF, p=0.025) in patients with max cobb>20° and LSF curve >5°. The LSF curve underwent greater correction in Qiu Type C patients (9.2°) compared to Type A (5.7°) and Type B (5.1°) (p=0.023); however, the max Cobb angle was similarly corrected among Qiu Types: Type A 21.8°, Type B 24.6°, and Type C 25.4° (p=0.602). Minimal differences were seen comparing the preop/postop/change in LSF curve and max Cobb angle regarding postop CM, postop CVA, complications, readmissions, reoperation, and PROs.
Conclusions
The LSF curve was highest in patients with CM, CCSM, and Qiu Type C curves. Most patients had a LSF curve opposite the max Cobb angle. The max Cobb angle was more often corrected than the LSF curve. The LSF curve underwent greater correction among Qiu Type C patients, whereas the max Cobb angle was similarly corrected among all Qiu Types. No clear trend was seen regarding postoperative complications and PROs between the LSF curve and max Cobb angle.
Keywords: adult spinal deformity, lumbosacral curve, max cobb angle, patient-reported outcome, vertical axis
Introduction
When evaluating coronal alignment in adult spinal deformity (ASD) patients, both regional and global measurements must be scrutinized closely. Globally, the C7 coronal vertical axis (CVA) is the preferred measurement. Regionally, close inspection of all coronal Cobb angles, especially the lumbosacral fractional (LSF) curve is necessary. Given that postoperative coronal malalignment (CM) can lead to inferior patient-reported outcomes (PROs) and revision surgery,1-4 a keen understanding how regional coronal Cobb angles, the LSF curve, and CVA coexist is warranted.1,5-7
Though assessment of the LSF curve is integral to understanding coronal alignment, especially in ASD patients fused to the sacrum, few reports have quantified its importance.5,8,9 Prior studies have shown that the LSF curve may be more difficult to correct in Qiu Type C curves, where the CVA is to the side of the major curve convexity.9,10 A synergistic understanding of how the LSF curve correction depends on the maximum coronal Cobb angle is lacking.
In a surgical ASD population, the current objectives were to: (1) report preoperative and postoperative LSF curve and maximum coronal Cobb angles, (2) describe associations between the LSF curve and perioperative variables, and (3) determine how both the LSF curve and maximum coronal Cobb angle impact radiographic, clinical, and patient-reported outcomes (PROs).
Methods
Study Design
A retrospective cohort study was undertaken based on prospectively collected data from a single institution center consisting of 2 spine deformity surgeons. Following institutional review board approval, data was collected on all patients undergoing ASD surgery between 06/01/2015-12/31/2018. Informed consent was obtained from all patients.
Patient Population
Preoperative enrollment criteria were similar to prior studies of ASD patients.11,12 The inclusion criteria were: adults age >18 years undergoing ≥6 level fusion with at least 1 of the following radiographic criteria (Cobb angle>30 , sagittal vertical axis>5 cm, coronal vertical axis (CVA) >3 cm, pelvic tilt (PT) of >25 , or thoracic kyphosis (TK) > 60 ).
Clinical and Radiographic Data Collection
Demographic and perioperative variables were collected from the electronic medical record and included diagnosis, revision, total instrumented levels (TIL), and 3 column osteotomy (3CO). Radiographically, to measure global alignment, both the C7-coronal vertical axis (CVA) and sagittal vertical axis (SVA) were continuous variables measured in centimeters (cm), both taken from the center of the C7 body. 13 Additional radiographic variables included: L4 tilt, L5 tilt, pelvic obliquity (angle of line passing between superior iliac crest and horizontal), and leg length discrepancy (difference in height from femoral head to tibial plafond). The Qiu classification was used to assess directionality, 1 which categorized CM into 3 groups based on a value of 3 cm as follows: Type A: CVA <3 cm; Type B: CVA >3 cm and C7PL shifted to the concave side of the curve; and Type C: CVA >3 cm and C7PL shifted to the convex side of the curve. 1 Lastly, patients were divided into the following 4 groups based on preoperative alignment: 1) Neutral alignment (NA): CVA<3 cm and SVA>5 cm; 2) CM only: CVA≥3 cm and SVA<5 cm; CM only without sagittal malalignment (SM); 3) SM only: SVA≥5 cm and CVA<3 cm; CM; 4) Combined coronal and sagittal malalignment (CCSM): both CVA≥3 cm and SVA≥5 cm.
Primary Exposures: Lumbosacral Fractional Curve and Maximum Coronal Cobb Angle
The LSF curve was defined as the angle between the sacrum and distal lumbar spine, either L3/4/5 depending on the most tilted lower lumbar vertebra, according to prior studies. 14 The maximum coronal Cobb angle – hereafter referred to as the max Cobb angle – was the largest coronal curve between the following 4 regions: proximal thoracic (PT), main thoracic (MT), or thoracolumbar/lumbar (TL/L). Even if the LSF curve was larger than the PT, MT, or TL/L curves, the max Cobb angle did not include the LSF curve.
Primary Outcomes: Radiographic, Clinical, and Patient Reported Outcomes
All primary outcomes were separated into 3 domains. 1) Radiographic outcomes included the evaluation of CM measured as both a binary (CVA ≥3) and a continuous (absolute value) variable. In addition, the amount of preoperative to immediate postoperative correction regarding the LSF and max coronal Cobb angles were collected, both as a distance and percent correction. 2) Clinical outcomes consisted of major complication, 15 readmission, and reoperation. 3) PROs were based on the Oswestry Disability Index (ODI) version 2.1a,16,17 analyzed as a mean value and percent achieving minimum clinically important difference (MCID).
Statistical Analysis
Descriptive statistics were used to summarize patient demographics and radiographic data. Categorical data was presented as frequencies and percentages, whereas continuous data was presented with mean, standard deviations (SD), and medians. Pearson’s correlation was used to evaluate the relationship between the LSF curve, max Cobb angle, and other radiographic variables. Strength of correlation was classified accordingly: 0-.3 negligible, .3-.5 low, .5-.7 moderate, .7-.9 high, .9-1.0 very high. Wilcoxon-rank-sum tests were used to assess differences between 2 groups for continuous data (mean PRO values), whereas Chi-squared proportion tests were used for count data. Kruskal-Wallis testing and one-way analysis of variance (ANOVA) were used to assess continuous variables between 3 groups. MCID threshold values were set in accordance with prior studies: −18 for ODI.18-22 Logistic and linear univariate and multivariate regression were used for potential association with outcomes. Statistical significance was set at an alpha level of P < .05. All statistical analyses were performed in STATA version 14 (StataCorp LP, College Station, Texas).
Results
Demographics and Perioperative Variables
A total of 243 patients underwent ASD surgery with a mean age of 49.3 years; 33% were male with a mean BMI of 25.5 (Table 1). Half of all patients had AdIS, and the remaining 50% had various forms of revision and/or degenerative scoliosis. The population represented a complex cohort, given the 62% revision surgery rate, mean total instrumented levels (TIL) of 13.5 ± 3.9, mean operative time of 471.0 ± 133.9 minutes, and estimated blood loss (EBL) of 1315.8 ± 786.6cc. Mean preoperative CVA (cm) was 2.9 ± 2.7, ranging from .1-19.7. Mean preoperative SVA (cm) was 3.7 ± 6.8, ranging from -8.8-26.1. Mean PO was 2.3° ± 2.4°, ranging from 0-22.1°. Global alignment of all patients was: N 115 (47.3%), CM 48 (19.8%), SM 38 (15.6%), and CCSM 42 (17.6%). Qiu type was: Type A (153; 63%), Type B (53; 22%), and Type C (37, 15%). Of the 243 patients, 175 (72%) had 2-year follow-up. Major complications were seen in 41 (17%) patients, readmissions occurred in 38 (16%), and reoperation was required in 34 (14%).
Table 1.
Demographics, Operative Variables, and Outcome Variables.
| Variable | Value N = 243 |
|---|---|
| Age, mean ± SD | 49.3 ± 18.3 |
| Female, n (%) | 163 (67%) |
| ASA, n (%) | |
| 1/2/3 | 25/150/68 |
| BMI, mean ± SD | 25.5 ± 5.7 |
| Depression, n (%) | 48 (20%) |
| Diagnosis, n (%) | |
| Adult idiopathic scoliosis (AdIS) | 121 (50%) |
| Degenerative and other | 122 (50%) |
| Revision, n (%) | 150 (62%) |
| Preop C7-CVA (cm), mean ± SD (range) | 2.9 ± 2.7 (.1-19.7) |
| Preop SVA (cm), mean ± SD (range) | 3.7 ± 6.8 (-8.8-26.1) |
| Max cobb (°), mean ± SD (range) | 43.0 ± 26.5 (.0-134.3) |
| Lumbosacral fractional curve (°), mean ± SD | 12.1 ± 9.9 (.2-62.3) |
| Pelvic obliquity (°), mean ± SD | 2.3 ± 2.4 (0-22.1) |
| Total instrumented levels, mean ± SD | 13.5 ± 3.9 |
| Three-column osteotomy, n (%) | 35 (14%) |
| Operative time (min), mean ± SD | 471.0 ± 133.9 |
| EBL (cc), mean ± SD | 1315.8 ± 786.6 |
| Length of stay, mean ± SD | 8.0 ± 7.9 |
| Major complication, n (%) | 41 (17%) |
| Readmission, n (%) | 38 (16%) |
| Reoperation, n (%) | 34 (14%) |
Lumbosacral Fractional Curve
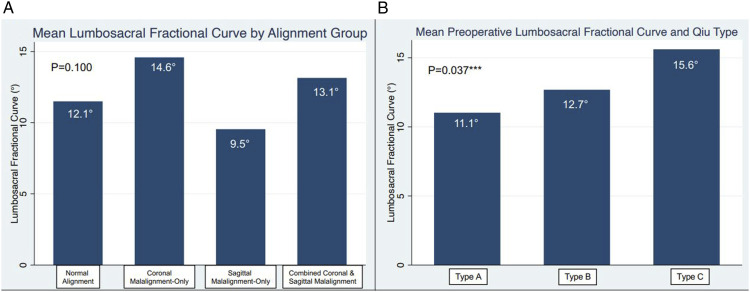
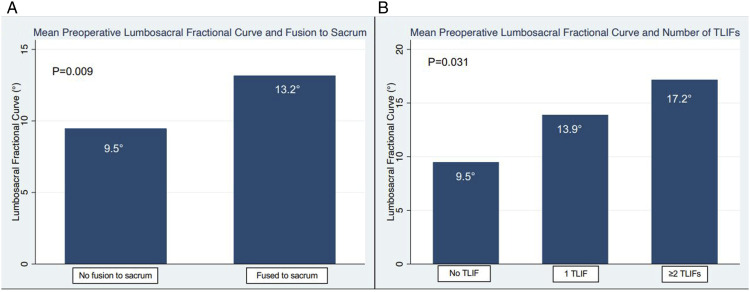
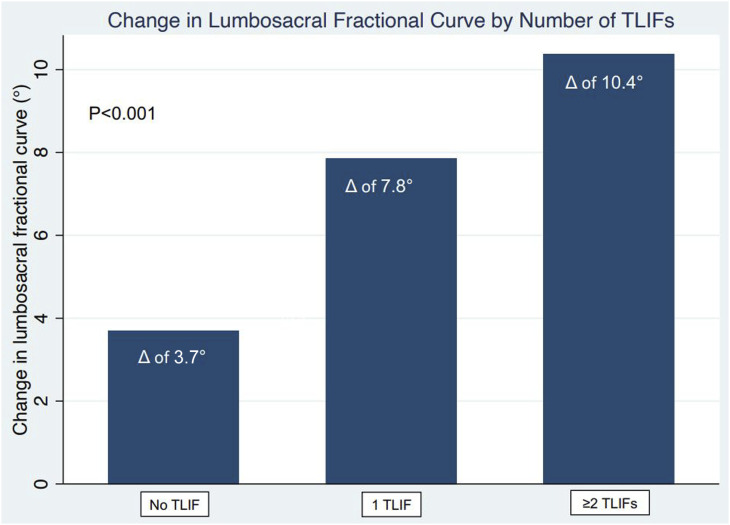
The mean LSF curve was 12.1° ± 9.9° (.2-62.3). A LSF curve >5° was seen in 71.6% of all patients and 81.1% of patients with preoperative CM (P = .012). Though the largest LSF curves were seen in the CM (14.6 ± 11.9°) and CCSM (13.1 ± 8.3°) groups, the LSF curve was not statistically different between all groups (Figure 1(a)). A significantly higher LSF curve was seen in Type C patients (15.6°), compared to Type A (11.1°) and B (12.7°) patients (P = .037) (Figure 1(b)). With respect to operative variables, a higher LSF curve was seen in patients with fusion to the sacrum and instrumentation to the pelvis (P = .009) (Figure 2(a)). In addition, a higher LSF curve was associated with a more TLIFs (P = .031) (Figure 2(b)). Postoperatively, more TLIFs were associated with greater amount of LSF curve correction (Figure 3).
Figure 1.
Preoperative alignment patterns based on mean lumbosacral fractional curve by (A) alignment group and (B) Qiu type.
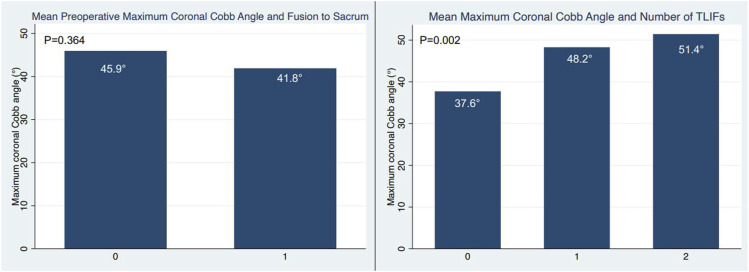
Figure 2.
Operative technique based on to mean lumbosacral fractional curve by (A) instrumentation to pelvis (B) number of TLIFs.
Figure 3.
Mean change in lumbosacral fractional curve by number of TLIFs performed.
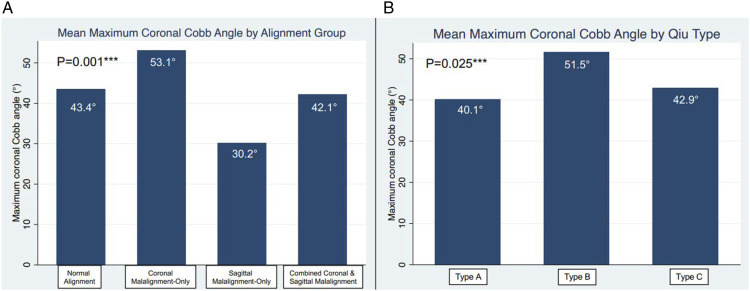
Maximum Coronal Cobb Angle
Mean max Cobb angle was 43.0 ± 26.5° (.0-134.3). The largest max Cobb angles were seen in the CM (53.1 ± 23.0°) and CCSM (42.1 ± 30.3°) groups, and in contrast to the LSF curve, the max Cobb angles were significantly different between all groups (Figure 4(a)). According to Qiu classification, a significantly higher max Cobb angle was seen in Type B patients, compared to Type A and C patients (Figure 4(b)), which is different than the LSF curve trend where Type C curves had the largest LSF curve. With respect to operative variables, max Cobb angles were similar in patients fused and not fused to the sacrum (P = .364) (Figure 5(a)). In addition, a higher LSF curve was associated with a higher number of TLIFs (P = .002) (Figure 5(b)).
Figure 4.
Preoperative alignment patterns based on mean maximum coronal Cobb angle by (A) alignment group and (B) Qiu type.
Figure 5.
Operative technique based on to mean maximum coronal Cobb angle by (A) instrumentation to pelvis (B) number of TLIFs.
Directionality
A total of 82.7% of patients had the LSF curve opposite the max cobb angle. Interestingly, 22 (9.1%) patients had a LSF curve that was larger than the max Cobb angle. Of these 22 patients, the majority were Type A (59.1%) compared to Type B (36.4%) and Type C (4.6%).
Comparison of Lumbosacral Fractional Curve vs Maximum Coronal Cobb Angle Correction
The amount of LSF curve and max Cobb angle correction is summarized by Qiu Type in Figure 6. The LSF curve appeared to be corrected most in Type C patients compared to Type A and B (P = .023). However, the amount of correction of the max Cobb angle was statistically similar across groups (P = .602). Taken together, different amounts of LSF curve correction occurred based on Qiu type (Type C the most), whereas as max Cobb angle correction was consistent across all Qiu types.
Figure 6.
Correction of LSF curve and maximum coronal Cobb angle according to Qiu type.
The max Cobb angle also achieved more correction than the LSF curve, judged by % of each preop angle that was improved from preop (54.5% Cobb vs 46.5% LSF, P = .025) in patients with max cobb>20° and LSF curve >5°.
Radiographic, Clinical, and Patient-Reported Outcomes
The impact of LSF curve (preoperative, postoperative, and percent correction) on the 3 primary outcomes is seen in Table 2. Interestingly, multivariate analysis revealed that a higher preoperative and postoperative LSF curve was associated with a decreased odd of readmission, while amount of LSF curve correction was not correlated.
Table 2.
Impact of Preoperative, Postoperative, and Total Correction of Lumbosacral Fractional Curve on Radiographic Outcomes, Clinical Outcomes, and Patient-Reported Outcomes.
| Outcome | Univariate | Multivariate (Controlling for Age, CVA, SVA, PO, Total Instrumented levels) | |||
|---|---|---|---|---|---|
| /OR (95% CI) | P-value | /OR (95% CI) | P-value | ||
| 1. Radiographic | |||||
|
Postop CM
Logistic regression |
Preop LSF curve | 1.016 (.984, 1.049) | .341 | 1.022 (.986, 1.059) | .232 |
| Postop LSF curve | 1.054 (.988, 1.125) | .112 | 1.047 (.973, 1.127) | .217 | |
| LSF curve correction | .665 (.287, 1.541) | .341 | .835 (.335, 2.085) | .700 | |
|
Postop CVA*
Linear regression |
Preop LSF curve | .00816 (-.0117, .0280) | .418 | .0074 (-.0118, .0266) | .447 |
| Postop LSF curve | .0482 (.0071, .0893) | .0218 | .0367 (-.0028, .0761) | .0682 | |
| LSF curve correction | -.328 (-.9065, .2514) | .293 | -.1765 (-.7215, .3686) | .348 | |
| 2. Clinical | |||||
|
Complication
Logistic regression |
Preop LSF curve | 1.011 (.978, 1.045) | .509 | 1.007 (.972, 1.043) | .693 |
| Postop LSF curve | 1.040 (.971, 1.113) | .261 | 1.005 (.933, 1.083) | .899 | |
| LSF curve correction | .957 (.369, 2.479) | .9277 | .881 (.306, 2.539) | .815 | |
|
Readmission
Logistic regression |
Preop LSF curve | .966 (.925, 1.008) | .113 | .945 (.898, .994) | .0273 |
| Postop LSF curve | .879 (.792, .975) | .0148 | .845 (.743, .961) | .0106 | |
| LSF curve correction | 1.224 (.402, 3.728) | .722 | .908 (.253, 3.263) | .883 | |
|
Reoperation
Logistic regression |
Preop LSF curve | .962 (.919, 1.007) | .0936 | .941 (.892, .992) | .0234 |
| Postop LSF curve | .871 (.779, .973) | .015 | .799 (.690, .926) | .0029 | |
| LSF curve correction | 1.46 (.433, 4.924) | .542 | 1.185 (.294, 4.769) | .811 | |
| 3. Patient-reported outcomes | |||||
|
ODI*
Linear regression |
Preop LSF curve | -.1271 (-.3810, .1267) | .325 | -.2053 (-.4302, .0196) | .0734 |
| Postop LSF curve | -.0538 (-.6080, .5005) | .849 | -.0401 (-.5293, .4473) | .869 | |
| LSF curve correction | -1.3755 (-8.1842, 5.4331) | .690 | -3.8477 (-9.9227, 2.2274) | .213 | |
|
MCID
Logistic regression |
Preop LSF curve | .967 (.936, .998) | .0377 | .968 (.936, 1.001) | .0561 |
| Postop LSF curve | .969 (.904, 1.038) | .373 | .963 (.896, 1.036) | .311 | |
| LSF curve correction | .416 (.133, 1.296) | .130 | .423 (.124, 1.439) | .168 | |
The impact of the max Cobb angle (preoperative, postoperative, and percent correction) on the 3 primary outcomes is seen in Table 3. The only significant relationship was that a larger preoperative max Cobb angle was associated with a decreased ODI, a somewhat counterintuitive finding. In addition, a higher amount of max Cobb angle correction was associated with a decreased ODI.
Table 3.
Impact of Preoperative, Postoperative, and Total Correction of MAXIMUM CORONAL COBB ANGLE on Radiographic Outcomes, Clinical Outcomes, and Patient-Reported Outcomes.
| Outcome | Univariate | Multivariate (Controlling for Age, CVA, SVA, PO, Total Instrumented levels) | |||
|---|---|---|---|---|---|
| /OR (95% CI) | P-value | /OR (95% CI) | P-value | ||
| 1. Radiographic | |||||
|
Postop CM
Logistic regression |
Preop max cobb | 1.007 (.995, 1.019) | .281 | 1.009 (.994, 1.025) | .245 |
| Postop max cobb | 1.022 (.997, 1.048) | .088 | 1.016 (.985, 1.047) | .314 | |
| Max cobb correction | 1.117 (.201, 6.206) | .899 | 2.464 (.381, 15.956) | .344 | |
|
Postop CVA*
Linear regression |
Preop max cobb | .0040 (-.0033, .0113) | .279 | .0022 (-.0057, .010) | .589 |
| Postop max cobb | .0179 (.0026, .0333) | .0221 | .0080 (-.0080, .239) | .326 | |
| Max cobb correction | -.2804 (-1.2919, .7312) | .585 | -.0657 (-1.047, .9158) | .895 | |
| 2. Clinical | |||||
|
Complication
Logistic regression |
Preop max cobb | 1.016 (1.004, 1.029) | .011 | 1.009 (.994, 1.024) | .224 |
| Postop max cobb | 1.035 (1.009, 1.061) | .0085 | 1.025 (.996, 1.055) | .092 | |
| Max cobb correction | .302 (.060, 1.505) | .144 | .240 (.040, 1.438) | .118 | |
|
Readmission
Logistic regression |
Preop max cobb | .982 (.967, .996) | .013 | .986 (.969, 1.004) | .123 |
| Postop max cobb | .970 (.939, 1.002) | .068 | .992 (.958, 1.027) | .655 | |
| Max cobb correction | 1.541 (.204, 11.64) | .675 | .614 (.070, 5.416) | .661 | |
|
Reoperation
Logistic regression |
Preop max cobb | .983 (.968, .998) | .025 | .983 (.966, 1.001) | .067 |
| Postop max cobb | .971 (.938, 1.004) | .089 | .987 (.952, 1.023) | .474 | |
| Max cobb correction | 1.476 (.182, 11.968) | .715 | .533 (.056, 5.050) | .584 | |
| 3. Patient-reported outcomes | |||||
|
ODI*
Linear regression |
Preop max cobb | -.2420 (-.3329, -.1510) | <.0001 | -.2133 (-.3023, -.1242) | <.0001 |
| Postop max cobb | -.2831 (-.487, -.0793) | .0067 | -.1736 (-.3700, .0228) | .083 | |
| Max cobb correction | -10.641 (-23.259, 1.9771) | .098 | -11.928 (-23.182, -.6751) | .038 | |
|
MCID
Logistic regression |
Preop max cobb | .992 (.979, 1.004) | .190 | .992 (.978, 1.007) | .315 |
| Postop max cobb | .999 (.972, 1.027) | .929 | 1.000 (.971, 1.031) | .978 | |
| Max cobb correction | .500 (.080, 3.141) | .459 | .540 (.077, 3.767) | .534 | |
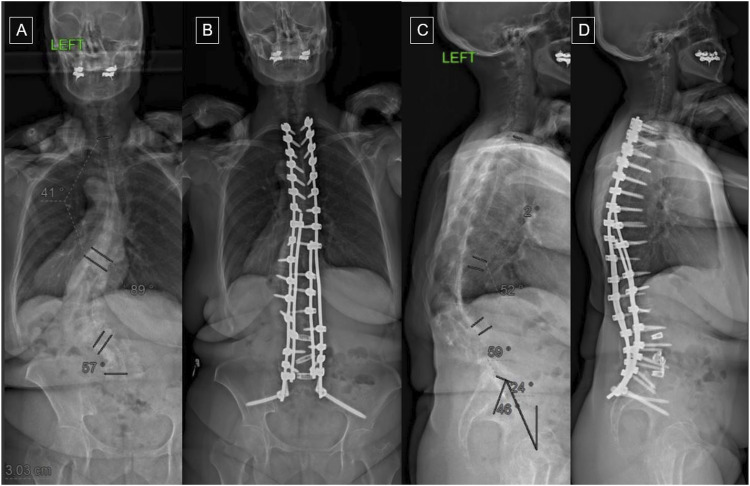
A case example of AdIS is illustrated in Figure 7, demonstrating a major correction of an 89° TL/L Cobb angle and 57° LSF curve following posterior spinal fusion (PSF) with multilevel posterior column osteotomies (PCO) for TL/L curve correction and three-level transforaminal interbody fusion (TLIF) for LSF curve correction.
Figure 7.
Case example of a female patient with progressive adult idiopathic scoliosis (AdIS) presenting with coronal and sagittal malalignment. Major correction of a large LSF curve of 57° and maximum coronal Cobb angle are demonstrated at 2-years postoperatively, following posterior spinal fusion (PSF) with multilevel posterior column osteotomies (PCO) for thoracolumbar curve correction and three-level transforaminal interbody fusion (TLIF) for LSF curve correction. A: preoperative posteroanterior (PA) view, B: postoperative PA view, C: preoperative lateral view, D: postoperative lateral view.
Discussion
In the current ASD population, though the max Cobb angle was higher in patients with CM, similar size LSF curves were seen in all alignment types, signifying that a notable LSF curve can be present in any alignment pattern. A LSF curve >5° was seen in 71.6% of all ASD patients and 81.1% of ASD patients with preoperative CM. The majority of patients (82.7%) had a LSF curve that was opposite the max Cobb angle, and in 22 (9.1%) patients, the LSF was larger than any of the max Cobb angles. In Qiu Type B patients, the max Cobb angle was significantly higher than Type A/C, whereas in Qiu Type C patients, the LSF curve was significantly higher than Type A/BA higher LSF curve often led to 1 or more TLIFs, and more TLIFs were associated with more LSF curve correction. Further supporting the importance of the LSF curve in Qiu Type C patients, while all Qiu types underwent similar magnitudes of coronal Cobb angle corrections, Type C patients had a significantly larger amount of LSF curve correction than Type A/B. Lastly, the LSF curve was a slightly stronger driver of postoperative CM than max Cobb angle.
In terms of alignment, the LSF curve was similar amongst all alignment patterns regardless of a neutral, sagittal, or coronal malalignment. Even in patients with neutral alignment or SM only, the LSF curve can still be high despite normal coronal alignment. Furthermore, the LSF curve was highest in Type C patients, whereas max Cobb angle was highest in Type B patients. Correspondingly, Type C patients underwent a significantly larger LSF curve correction than Type A or B. In a recent study of 24 ASD patients undergoing minimally invasive ASD correction (MIS) by Walker et al, 10 the authors reported similar LSF curves between Type B and C patients, which is in contrast to our results where the highest LSF curve prevalence was in Qiu Type C patients. Moreover, while we showed a significant improvement in the LSF curve across all Qiu types, with Type C being the highest, Walker et al 10 showed that Type C patients were the only group to not improve their LSF curve. These results may be attributed to a smaller sample size of an exclusively degenerative population undergoing a minimally invasive approach, compared to our open surgery series. An additional study by Theologis et al 9 showed similar results to Walker et al, 10 where Type C patients also had persistently greater postoperative LSF curves. Overall, our results and the literature likely confirm that the LSF curve is most important in Qiu Type C patients.
A higher LSF curve led to more fusions to the sacrum and more TLIFs, and more TLIFs led to more LSF curve correction. Amara et al 14 showed that patients undergoing more levels of interbody fusion had greater LSF curve correction (7.4° vs 12.3° vs 12.1° for 1, 2, and 3 levels; P = .009), and importantly a combination of anterior interbody fusions (ALIF) and TLIFs were used. In a study of 124 patients, Theologis et al 9 concluded that the correction of the LSF curve with TLIFs was better than no interbody in conjunction with these findings. Moreover, compared to the 2 aforementioned studies, significant correction was seen in Type C patients with only TLIFs, which appears to be the most difficult type of curves to correct.
Fewer associations were seen between LSF curves and correction of max Cobb angles. However, 1 counterintuitive finding was the preoperative and postoperative LSF curve which were associated with a decreased odds of reoperation and readmission. Potentially this could be due to a greater correction of a larger LSF curve, though amount of LSF curve correction was associated with neither outcome. With respect to max Cobb angle, a higher amount of max Cobb correction was associated with a decreased ODI.
While the max Cobb angle has been extensively studied in ASD surgery, the LSF curve has received less attention. In this study, we showed that differentiating LSF curve and major Cobb angle is crucial, as a high LSF curve was seen in the majority of patients with ASD, especially those with CM. We also found that the LSF curve was a stronger predictor of postoperative CM compared to max Cobb angle. These results may assist surgeons in the preoperative planning by optimizing the LSF curve to improve the postoperative coronal malalignment. Furthermore, these results reinforce the need for surgeons to pay close attention the LSF curve, even though our eyes often gravitate to the largest curve, which is the max Cobb angle. By paying close attention to the LSF curve, surgeons can pay close attention to the optimal placement of L5/S1 or L4/5 interbodies to correct the LSF curve and the choice of lower instrumented vertebra (lumbar vs sacrum/pelvis). These strategies are most important in Qiu type C curves, which have been shown to have the highest rates of postoperative CM. 9
This study has several limitations. First, these results represent retrospectively collected data. Second, since the data was received from a single institution including patients treated by 2 separate spine surgeons, selection and treatment biases remain and may have not been accounted for. Another potentially perceived limitation is not reporting the reason behind readmissions and reoperations, which might not be directly related to the degree of malalignment. Other shortcoming of our analysis was not including the surgical approach used. Reporting these techniques can uncover potential surgical confounding factors that may influence patients’ outcomes.664
Conclusion
In 243 patients undergoing ASD surgery, a LSF curve >5° was seen in 81.1% of ASD patients with preoperative CM. The LSF curve opposed the max Cobb angle in 83.0% of cases and was a slightly stronger driver of postoperative CM than max Cobb angle, potentially due to it being corrected less and/or not included in the surgery than the max cobb angle. A higher LSF curve often led to 1 or more TLIFs, and more TLIFs were associated with more LSF curve correction. Qiu Type C patients had a significantly larger amount of LSF curve correction than Type A/B. These results underscore the importance of differentiating the LSF curve from the max coronal Cobb angle in ASD surgery.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Statements and Declarations: Dr. Lehman’s disclosure: Paid consultant for a company or supplier: Medtronic; other support: contracted research with the Department of Defense. Dr Lenke’s disclosure: Royalties from a company or supplier: Medtronic; Paid consultant for a company or supplier: Medtronic, Acuity Surgical; Medical/Orthopaedic publications editorial/governing board: Deputy Editor of Spine Deformity; Reviewer for Spine, The Spine Journal, European Spine Journal, JBJS, Global Spine Journal; Other support: International Spine Study Group, Harms Study Group, AO Spine Deformity Knowledge Forum. No other perceived conflict of interests by any of the listed authors.
ORCID iDs
Hani Chanbour https://orcid.org/0000-0003-2409-8623
Fthimnir M Hassan https://orcid.org/0000-0003-3928-8972
Yong Shen https://orcid.org/0000-0002-4866-838X
Mena G Kerolus https://orcid.org/0000-0002-0902-6528
Nathan J Lee https://orcid.org/0000-0001-9572-5968
Eric Leung https://orcid.org/0000-0001-8722-8056
References
- 1.Bao H, Yan P, Qiu Y, Liu Z, Zhu F. Coronal imbalance in degenerative lumbar scoliosis: Prevalence and influence on surgical decision-making for spinal osteotomy. Bone Joint Lett J. 2016;98-B:1227-1233. doi: 10.1302/0301-620X.98B9.37273 [DOI] [PubMed] [Google Scholar]
- 2.Tanaka N, Ebata S, Oda K, Oba H, Haro H, Ohba T. Predictors and clinical importance of postoperative coronal malalignment after surgery to correct adult spinal deformity. Clin Spine Surg. 2020;33:E337-E341. doi: 10.1097/BSD.0000000000000947 [DOI] [PubMed] [Google Scholar]
- 3.Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2- to 5-year follow-up study. J Spinal Disord Tech. 2015;28:341-347. doi: 10.1097/BSD.0b013e3182aab2ff [DOI] [PubMed] [Google Scholar]
- 4.Lewis SJ, Keshen SG, Kato S, Dear TE, Gazendam AM. Risk factors for postoperative coronal balance in adult spinal deformity surgery. Global Spine J. 2018;8:690-697. doi: 10.1177/2192568218764904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bao H, Liu Z, Zhang Y, et al. Sequential correction technique to avoid postoperative global coronal decompensation in rigid adult spinal deformity: A technical note and preliminary results. Eur Spine J. 2019;28:2179-2186. doi: 10.1007/s00586-019-06043-9 [DOI] [PubMed] [Google Scholar]
- 6.Plais N Bao H Lafage R, et al.International Spine Study Group . The clinical impact of global coronal malalignment is underestimated in adult patients with thoracolumbar scoliosis. Spine Deform. 2020;8:105-113. doi: 10.1007/s43390-020-00046-z [DOI] [PubMed] [Google Scholar]
- 7.Obeid I, Berjano P, Lamartina C, Chopin D, Boissiere L, Bourghli A. Classification of coronal imbalance in adult scoliosis and spine deformity: A treatment-oriented guideline. Eur Spine J. 2019;28:94-113. doi: 10.1007/s00586-018-5826-3 [DOI] [PubMed] [Google Scholar]
- 8.Geddes B, Glassman SD, Mkorombindo T, Gardner JQ, Carreon LY. Improvement of coronal alignment in fractional low lumbar curves with the use of anterior interbody devices. Spine Deform. 2021;9:1443-1447. doi: 10.1007/s43390-021-00328-0 [DOI] [PubMed] [Google Scholar]
- 9.Theologis AA, Lertudomphonwanit T, Lenke LG, Bridwell KH, Gupta MC. The role of the fractional lumbosacral curve in persistent coronal malalignment following adult thoracolumbar deformity surgery: A radiographic analysis. Spine Deform. 2021;9:721-731. doi: 10.1007/s43390-020-00228-9 [DOI] [PubMed] [Google Scholar]
- 10.Walker CT, Godzik J, Angel S, Giraldo JP, Turner JD, Uribe JS. (2021) Coronal balance with circumferential minimally invasive spinal deformity surgery for the treatment of degenerative scoliosis: Are we leaning in the right direction? J Neurosurg Spine:34, 879-887. doi: 10.3171/2020.8.SPINE201147 [DOI] [PubMed] [Google Scholar]
- 11.Yilgor C Sogunmez N Boissiere L, et al.European Spine Study Group ESSG . Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 2017;99:1661-1672. doi: 10.2106/JBJS.16.01594 [DOI] [PubMed] [Google Scholar]
- 12.Baum GR, Ha AS, Cerpa M, et al. (2021) Does the global alignment and proportion score overestimate mechanical complications after adult spinal deformity correction? J Neurosurg Spine:34, 96-102. doi: 10.3171/2020.6.SPINE20538 [DOI] [PubMed] [Google Scholar]
- 13.Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine. 2012;16:547-564. doi: 10.3171/2012.2.SPINE11320. [DOI] [PubMed] [Google Scholar]
- 14.Amara D, Mummaneni PV, Burch S, et al. The impact of increasing interbody fusion levels at the fractional curve on lordosis, curve correction, and complications in adult patients with scoliosis. J Neurosurg Spine. 2021;34:430-439. doi: 10.3171/2020.6.SPINE20256 [DOI] [PubMed] [Google Scholar]
- 15.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271-273. [PubMed] [Google Scholar]
- 16.Fairbank JC, Pynsent PB. The oswestry disability index. Spine. 2000;25:2940-2952. ; discussion 2952. doi: 10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 17.Crawford CH, 3rd, Glassman SD, Bridwell KH, Berven SH, Carreon LY. (2015) The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine 1976) 40:377-381. doi: 10.1097/BRS.0000000000000761 [DOI] [PubMed] [Google Scholar]
- 18.Kelly MP, Lurie JD, Yanik EL, et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am. 2019;101:338-352. doi: 10.2106/JBJS.18.00483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu S Diebo BG Henry JK, et al.International Spine Study Group ISSG . The benefit of nonoperative treatment for adult spinal deformity: identifying predictors for reaching a minimal clinically important difference. Spine J. 2016;16:210-218. doi: 10.1016/j.spinee.2015.10.043 [DOI] [PubMed] [Google Scholar]
- 20.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. (2008) Minimum clinically important difference in lumbar spine surgery patients: A choice of methods using the oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J 8:968-974. doi: 10.1016/j.spinee.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 21.Yuksel S Ayhan S Nabiyev V, et al.European Spine Study Group ESSG . Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J. 2019;19:71-78. doi: 10.1016/j.spinee.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 22.Jann B. (2014) Plotting regression coefficients and other estimates. STATA J 14(4): 708, 737. [Google Scholar]