Abstract
Background:
Patients with heart failure have a high rate of health literacy deficiency, and their hospital readmission is a great burden. Whether health literacy affects hospital readmission remains controversial.
Objective:
To investigate the impact of health literacy on hospital readmission among heart failure patients.
Method:
Relevant keywords were used to search for Chinese and English literature from Web of Science, PubMed, Cochrane Library, China National Knowledge Infrastructure, VIP Database for Chinese Technical Periodicals, Digital Journal of Wanfang Data, and Chinese BioMedical Literature Database. Newcastle-Ottawa Scale was used to assess the quality of the studies. Statistical analysis was performed using Stata 15.0, the fixed effect model was used to calculate the pooled effect estimate, and Begg’s and Egger’s tests were applied to assess the presence of publication bias.
Results:
Nine studies, involving 4093 heart failure patients, were included in this study. The overall rate of inadequate health literacy was 40.3%. Among these articles, 6 were included in the meta-analysis to calculate the pooled effect. The results indicated that, when compared with patients with adequate health literacy, those with inadequate health literacy had a relative risk of hospital readmission of 1.01, which increased to 1.14 after adjusting for follow-up time, the result was not significant (P = .09).
Conclusions:
About 2 out of 5 heart failure patients had inadequate health literacy, and there was no statistical association between health literacy and hospital readmission among these patients. This finding should be carefully considered and confirmed in further studies.
Keywords: heart failure, health literacy, hospital readmission, meta-analysis
1. Introduction
1.1. Heart failure
Heart failure (HF) is a cardiovascular disorder characterized by the inability of the heart to supply sufficient blood and oxygen. As the global population continues to age rapidly, HF has emerged as the leading cause of increased morbidity and mortality worldwide.[1] Lancet reported approximately 64.3 million individuals suffering from HF globally.[2] According to the Report on Cardiovascular Health and Disease in China 2021, there were approximately 8.9 million HF patients in China. In the United States, HF affected approximately 6.5 million adults, leading to substantial mortality rates and financial burden on the healthcare system.[3] Patients with HF frequently experience multiple hospitalizations, resulting in increased medical costs and diminished quality of life.[4] One study estimated that the 30-day and 1-year all-cause hospital readmission rates in China were 0.19 and 0.53, respectively.[5] In the United States, the rate of 30-day hospital readmission was 20%, with 50% of HF-related hospital readmission occurring within 13 days after discharge.[6]
1.2. Health literacy
Health literacy has been defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”[7] The level of health literacy in patients with HF affected their quality of life,[8] and studies have demonstrated a correlation between health literacy and prognosis among HF patients.[9] Furthermore, it has been confirmed that the health outcomes of patients with HF are closely associated with their health literacy levels.[10,11]
1.3. Research justification
As a chronic condition, patients with HF often experience readmissions to hospitals, with an average hospital readmission rate of 21% in the United States.[12] Exploring the factors influencing hospital readmission in patients with HF and implementing effective countermeasures are of great significance. Studies have identified that the New York Heart Association grading, comorbidities, and infections are factors that influence hospital readmission in HF patients.[13,14] In addition, several scholars have investigated the relationship between health literacy and hospital readmission in patients with HF, but the results have been inconsistent.[15–17] To the best of our knowledge, no meta-analysis has examined the impact of health literacy on hospital readmission among patients with HF.
2. Methods
2.1. Search strategy
Ethical approval was waived because this study was a meta-analysis. The protocol has been registered in the PROSPERO registry (CRD42023463912). Relevant studies were identified through the Web of Science Core Collection, PubMed, Cochrane Library, China National Knowledge Infrastructure, VIP Database for Chinese Technical Periodicals, Digital Journal of Wanfang Data, and Chinese BioMedical Literature Database (the last 4 are Chinese databases), and the retrieval time was from the establishment of the databases to January 2024. The search terms used were “health literacy” or “healthy literacy” and “hospital readmission” or “patient readmission,” and the detailed search strategy is reported in Table 1.
Table 1.
Search methods for identification of studies.
| Database | Search terms | Results |
|---|---|---|
| Web of Science | #1: TOPIC: (health literacy) OR TOPIC: (healthy literacy) | |
| #2: TOPIC: (hospital readmission) OR TOPIC: (patient readmission) | ||
| #3: #1 AND #2 | 296 | |
| PubMed | #1: ((health literacy [all field]) OR (healthy literacy [all field])) | |
| #2: ((hospital readmission [MeSH Terms]) OR (patient readmission [MeSH Terms])) | ||
| #3: #1 AND #2 | 144 | |
| Cochrane Library | #1: ((health literacy [Title abstract keyword]) OR (healthy literacy [Title abstract keyword])) | |
| #2: ((hospital readmission [Title abstract keyword]) OR (patient readmission [Title abstract keyword])) | ||
| #3: #1 AND #2 | 84 | |
| CNKI | #1: topic: health literacy | |
| #2: topic: patient readmission | ||
| #3: #1 AND #2 | 22 | |
| VIP | #1: Arbitrary field: health literacy | |
| #2: Arbitrary field: patient readmission | ||
| #3: #1 AND #2 | 10 | |
| WanFang Data | #1: all field: health literacy | |
| #2: all field: patient readmission | ||
| #3: #1 AND #2 | 14 | |
| CBM | #1: All fields: health literacy | |
| #2: All fields: patient readmission | ||
| #3: #1 AND #2 | 7 | |
| Total | 577 |
CBM = stands for Chinese BioMedical Literature Database, CNKI = China National Knowledge Infrastructure, OR = odds ratio, VIP = VIP Database for Chinese Technical Periodicals, WanFang Data = Digital Journal of Wanfang Data.
2.2. Inclusion and exclusion criteria
Studies were included in the analysis if they fulfilled the following criteria: the study participants consisted of patients with HF and the study assessed both patient health literacy and hospital readmission. Studies were excluded if they met any of the following conditions: the study did not involve HF patients; health literacy and hospital readmission were not assessed; the study was published in languages other than English or Chinese; the publication type was an editorial, conference abstract, letter, book news, or review article; and no abstract was available for the study.
2.3. Data collection
Initially, two reviewers (Lei Xiao and Cong Cheng) independently screened articles based on their titles and abstracts. Following this, the full text of the selected articles was thoroughly examined, resulting in further filtration of the remaining articles. In cases where disagreements occurred during the screening process, a consensus was reached through discussion. Relevant data for each study included in the systematic review were extracted using a standardized form. The extracted information included the first author’s name, year of publication, study design, follow-up time, methods used to evaluate health literacy, and hospital readmission numbers categorized according to different levels of health literacy.
2.4. Independent variable and outcome measurements
Various measurement instruments have been utilized to assess health literacy, including the Short-Test of Functional Health Literacy in Adults (S-TOFHLA),[18] the Brief Health Literacy Screen (BHLS),[19] the Newest Vital Sign (NVS),[20] the HF-specific Health Literacy Scale,[21] and the Health Literacy Scale for Chronic Patients.[22] Most studies categorized their patient cohorts into 2 groups: those with adequate health literacy and those with inadequate health literacy. In cases where the patient cohort was divided into adequate, marginal, and inadequate categories, we combined the marginal and inadequate health literacy groups and considered them as 1 category of inadequate health literacy. When health literacy was evaluated using the S-TOFHLA in combination with another measurement tool, the results from the S-TOFHLA were prioritized in the analysis.[10] The outcome measure of interest in this study was all-cause readmission in patients with HF. If a study had multiple follow-up time, the longest follow-up time was selected for inclusion in the analysis.
2.5. Quality assessment
The quality of the original studies included in the meta-analysis was evaluated using the Newcastle-Ottawa Scale (NOS). NOS assesses cohort studies based on 3 aspects: selection of the study population, comparability, and exposure or outcome assessment. NOS uses the semi-quantification principle of the star system to assess literature quality, with a full score of 9 stars. A score of 7 to 9 is considered high-quality research, 4 to 6 is moderate-quality research, and less than 4 is considered low-quality research.
2.6. Statistical analysis
Literature screening was conducted using Endnote X9. The degree of inconsistency was quantified using the I2 statistic. I2 values of 0, 25, 50, and 75% were considered indicative of no, low, moderate, and high heterogeneity, respectively. In this analysis, a fixed effects model was chosen a priori because of the similarity of research types included in the study (all the studies were cohort studies). A subgroup analysis was performed based on the follow-up time of the included studies. To evaluate publication bias, Begg’s and Egger’s tests were employed. All statistical analyses were conducted using Stata version 15.0, and a 2-tailed P-value of less than .05 was considered statistically significant.
3. Results
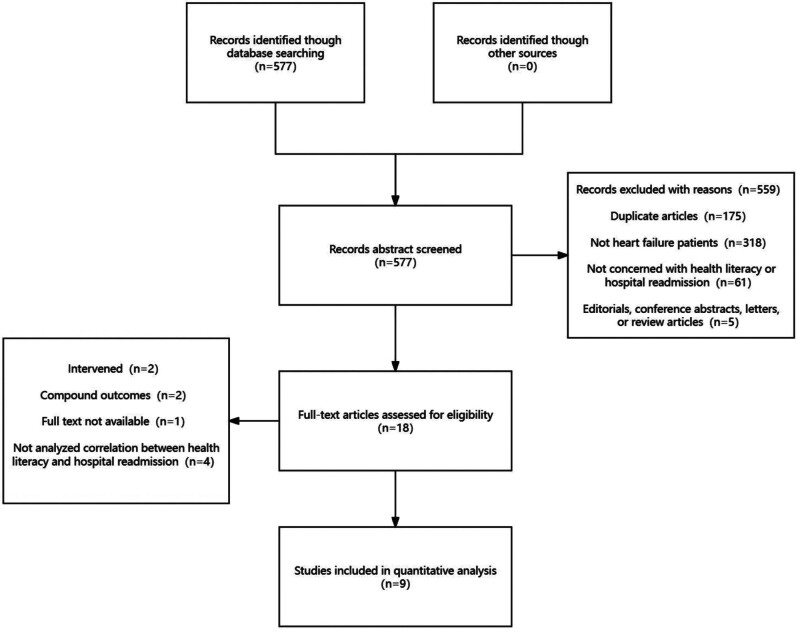
Of the 577 articles identified during the search process, 18 were deemed relevant after reviewing their titles and abstracts. The remaining 559 articles were excluded for various reasons, such as not focusing on patients with HF, not assessing health literacy and readmissions, lacking complete abstracts, or not being of the desired literature type. Following a thorough examination of the full texts, 9 articles were selected and included in the systematic review, of which 6 were included in the meta-analysis. The article screening process is illustrated in Figure 1.
Figure 1.
Flow diagram of the literature search and study selection.
3.1. Characteristics of included studies
Nine articles, involving a combined population of 4093 patients with HF were included in the systematic review. The prevalence of inadequate health literacy was found to be 40.3% (one article did not provide a specific classification of health literacy[23]). Among these 9 articles, S-TOFHLA was used as the assessment tool for health literacy in 3 studies, while BHLS was used in 3 studies. The sample sizes of the included studies varied, ranging from approximately 100 to > 1000 participants. Approximately half of the included studies had a follow-up time of 1 month. Of the 9 articles, 6 demonstrated statistically significant associations between inadequate health literacy and hospital readmission. The selected studies were relatively recent, with publication dates from 2015 onwards, except for 1 study from 2011. In terms of the study population, the majority (5/9) of the studies focused on American patients. The average quality assessment score for the included articles was 7.44, and all studies included were of moderate to high quality. Table 2 shows the detailed characteristics of the articles included in this systematic review. Table 3 shows the quality assessment results.
Table 2.
Characteristics of the articles included in the systematic review.
| Study | Health literacy evaluation tool | Sample size (n) | Age (M ± SD) | Follow-up time | Statistical significance |
|---|---|---|---|---|---|
| Cheryl R Dennison (2011)[24] | S-TOHFLA | 95 | 59 ± 14 | 30 days | No |
| Sarah R Cox (2016)[25] | BHLS | 264 | 66.64 ± 14.26 | 30 days | No |
| Youn-Jung Son (2020)[26] | BHLS | 286 | 75.44 ± 6.51 | 1 year | Yes |
| Monica Isabelle Lopes Oscalices (2019)[27] | NVS | 100 | 63.3 ± 15.2 | 60 days | Yes |
| Candace D McNaughton (2015)[28] | BHLS | 1379 | 63.1 ± 14.8 | 90 days | No |
| Debra K Moser (2015)[29] | S-TOHFLA | 575 | 73.9 ± 10.7 68.0 ± 10.9 63.0 ± 12.6* |
More than 2 years | Yes |
| Madeline R Sterling (2018)[30] | S-TOHFLA | 825 | 63(43, 81)† | 30 days | Yes |
| Chunhua Ma (2020)[23] | The HF-specific Health Literacy Scale | 271 | 71.16 ± 10.49 | 1 year | Yes |
| Xuedong Li (2022)[31] | Health Literacy Scale for Chronic Patients | 231 | 74.89 ± 11.08 | 30 days | Yes |
S-TOFHLA = Short-Test of Functional Health Literacy in Adults, BHLS = Brief Health Literacy Screen, NVS = Newest Vital Sign.
Reported as median (IDR).
Reported as three Health Literacy Group, namely Inadequate, Marginal, and Adequate.
Table 3.
Results of quality assessment.
| Study | Population | Comparability | Outcome | Total |
|---|---|---|---|---|
| Cheryl R Dennison (2011)[24] | 4 | 0 | 2 | 6 |
| Sarah R Cox (2016)[25] | 4 | 0 | 2 | 6 |
| Youn-Jung Son (2020)[26] | 4 | 2 | 3 | 9 |
| Monica Isabelle Lopes Oscalices (2019)[27] | 4 | 0 | 2 | 6 |
| Candace D McNaughton (2015)[28] | 4 | 2 | 3 | 9 |
| Debra K Moser (2015)[29] | 4 | 2 | 2 | 8 |
| Madeline R Sterling (2018)[30] | 4 | 2 | 3 | 9 |
| Chunhua Ma (2020)[23] | 4 | 1 | 2 | 7 |
| Xuedong Li (2022)[31] | 4 | 1 | 2 | 7 |
3.2. Health literacy and hospital readmission
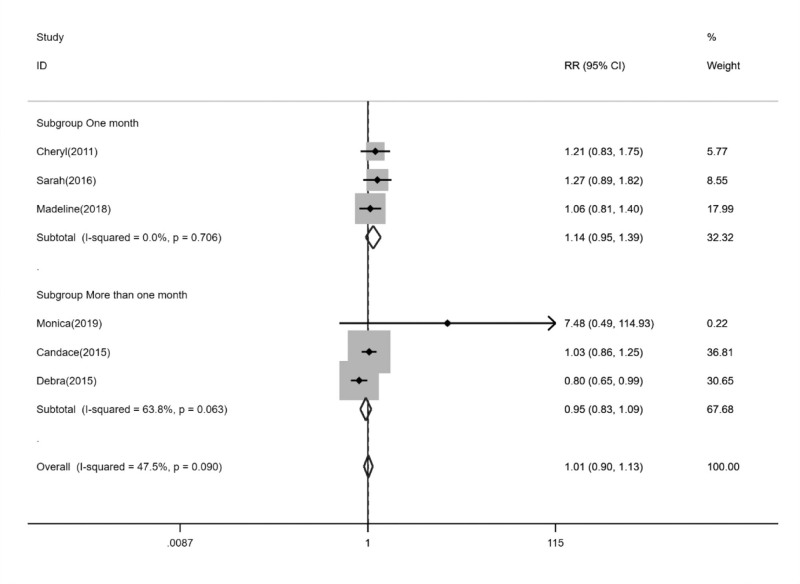
Of the 9 articles included in the systematic review, 6 were incorporated in the meta-analysis. The remaining 3 articles did not provide primary data.[23,26,31] The heterogeneity test revealed a low level of heterogeneity in the correlation between health literacy and hospital readmission (I2 = 47.5%; P = .09). Based on the combined results of the 6 cohort studies, there was no significant increase in the risk of hospital readmission for patients with HF who had inadequate health literacy compared with those with adequate health literacy (relative risk [RR] = 1.01; 95% confidence interval = 0.90–1.13). Subgroup analysis based on different follow-up time demonstrated that health literacy did not significantly impact hospital readmission for HF patients, regardless of whether the follow-up time was 1 month or longer. However, within the subgroup with a 1-month follow-up, HF patients with inadequate health literacy exhibited a 14% increased risk of hospital readmission compared with those with adequate health literacy, although this difference was not statistically significant (RR = 1.14; 95% confidence interval = 0.95–1.39). Furthermore, the heterogeneity observed can be attributed to differences in follow-up time. Within the subgroup in which all follow-up time was 1 month, no heterogeneity was found (I2 = 0.0%; P = .71), whereas the subgroup with follow-up time longer than 1 month displayed a moderate level of heterogeneity (I2 = 63.8%; P = .06). Figure 2 shows a forest plot.
Figure 2.
Forest plot of health literacy and hospital readmission.
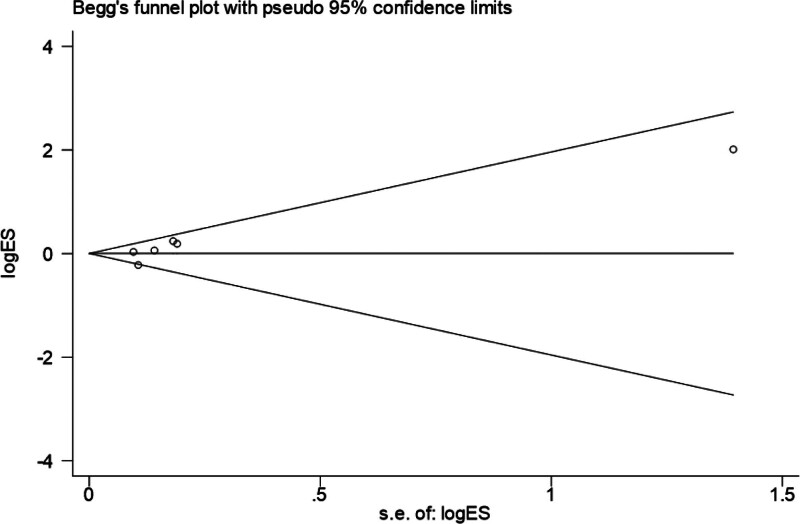
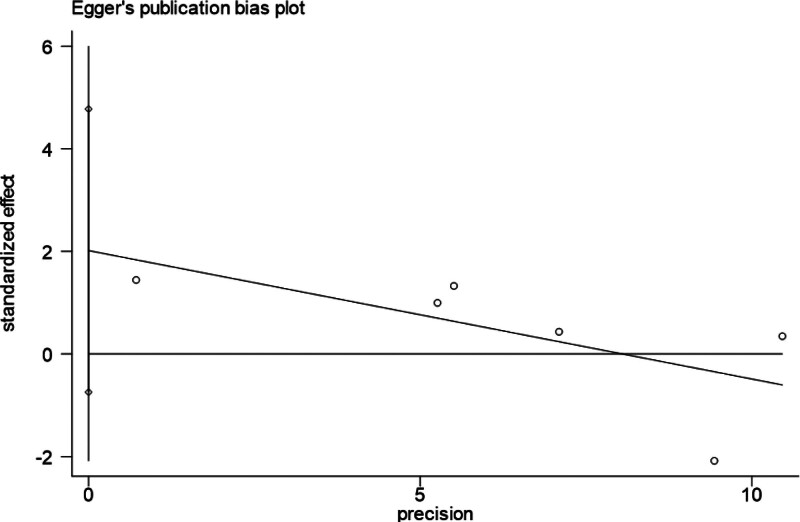
3.3. Publication bias
The results of Begg’s test suggested that there was no significant publication bias observed in the included studies (P = .06). Similarly, the results of Egger’s test indicated no significant publication bias (P = .11). Visual evidence supporting these findings is presented in Figures 3 and 4.
Figure 3.
Results of Begg’s test.
Figure 4.
Results of Egger’s test.
4. Discussion
In our systematic review, 40.3% of patients with HF were found to have inadequate health literacy. This finding aligns with a previous systematic review that reported an average of 39% of patients having low health literacy.[32] Similarly, another systematic review focusing on patients with cardiovascular disease demonstrated that approximately one-third of patients with cardiovascular disease exhibited inadequate health literacy.[33] However, in a separate systematic review specifically targeting HF patients, it was discovered that nearly a quarter of those with HF had inadequate health literacy.[10] Differences in health literacy adequacy in patients with HF varied according to the studies included in the study.[34] Furthermore, when considering the general population, 1 study indicated that 23% had inadequate or marginal health literacy.[35] It is important to note that this discrepancy may be attributed to the fact that our study specifically focused on individuals with HF, who were generally older.
In our meta-analysis, we compared the relative risk of hospital readmission for HF patients with inadequate health literacy to those with adequate health literacy. The relative risk was 1.01, indicating that inadequate health literacy did not have a statistically significant effect on hospital readmission among patients with HF. Subgroup analyses controlling for the same follow-up time showed a slightly elevated relative risk of 1.14 and the difference was not statistically significant. However, it is necessary to consider the results of the articles that were excluded from the meta-analysis. One such article reported a significant association between health literacy and hospital readmission, particularly in older women with limited health literacy (odds ratio: 10.17), as compared with older men with limited health literacy (odds ratio: 5.27).[26] Additionally, the other 2 excluded articles demonstrated a statistical association.[23,31] These studies employed similar methodologies using structural equation models to test the effect of health literacy on hospital readmission, revealing direct effects of −0.21 and −0.30, respectively. It is worth noting that these 3 articles showed statistical significance in elderly patients with HF. Elderly patients with HF are more likely to have inadequate health literacy and be readmitted to the hospital.
Among similar studies, some have taken a composite outcome approach by considering both death and hospital readmission.[11,15] By contrast, our study focused solely on hospital readmission as an outcome measure. This decision was based on the understanding that it was clear that health literacy was associated with mortality.[35] A previous meta-analysis involving 6491 patients with HF demonstrated a strong association between inadequate health literacy and mortality.[10] Another reason for our study’s emphasis on hospital readmission is the growing concern over high readmission rates among patients with HF due to the increasing incidence of this condition. Examining the factors influencing readmission in HF patients is of significant practical importance. Although 6 of the 9 articles included in our systematic review reported statistical associations, our meta-analysis yielded inconsistent results. This discrepancy may be attributed to the relatively small sample sizes of individual studies, resulting in an uneven distribution of weights in our meta-analysis.
In our study, we conducted a subgroup analysis based on the follow-up time, which provided valuable information and helped explain some of the observed heterogeneity. No heterogeneity was found in the 1-month follow-up studies. In all studies on hospital readmission rates of clinical diseases, research on HF has been the most extensive, especially concerning its 30-day readmission rate.[36] In recent years, an increasing number of studies have advocated the adoption of a 30-day time window to assess readmissions in HF patients.[37,38] The choice of follow-up time is a crucial factor when studying disease readmissions as it can significantly influence research outcomes. Establishing a universally recognized standard follow-up schedule would be advantageous for diseases such as HF, with higher readmission rates.
4.1. Study strengths and limitations
Given the limited number of articles included in our analysis, the consideration and analysis of different follow-up times on readmission may have been suboptimal. We were only able to conduct a simple subgroup analysis by dividing the follow-up time into 1 month and more than 1 month as the follow-up time of 3 articles was 1 month while the other 3 were 60 days, 90 days, and more than 2 years. Additionally, we did not account for potential variations in the results due to the different types of HF or the age of the study population. However, it is important to highlight several strengths of this study. To the best of our knowledge, this is the first systematic review to quantify the association between health literacy and hospital readmissions. All the studies included in our analysis utilized validated literacy assessment instruments, which ensured the reliability of the independent variable. This adds credibility to the findings and enhances the robustness of the outcomes.
5. Conclusion
Approximately two-fifths of patients with HF have insufficient health literacy, indicating that significant proportion of patients with HF face challenges in understanding and utilizing healthcare information. However, our study did not find a statistically significant association between health literacy and hospital readmission in these patients. It is important to interpret this finding cautiously and validate it through additional research.
Acknowledgments
We would like to thank all authors of the studies included in this systematic review and meta-analysis.
Author contributions
Conceptualization: Yuan Yang.
Data curation: Lei Xiao, Cong Cheng.
Formal analysis: Lei Xiao.
Writing—original draft: Lei Xiao.
Methodology: Fan Zhang.
Writing—review & editing: Ningling Yang, Qi Huang.
Abbreviations:
- BHLS
- brief health literacy screen
- CBM
- Chinese BioMedical Literature Database
- CNKI
- China National Knowledge Infrastructure
- CVD
- cardiovascular disease
- HF
- heart failure
- NOS
- Newcastle-Ottawa Scale
- NVS
- newest vital sign
- NYHA
- New York Heart Association
- S-TOFHLA
- Short-Test of Functional Health Literacy in Adults
- VIP
- VIP Database for Chinese Technical Periodicals
- WanFang Data
- digital journal of Wanfang data.
This study was funded by the Natural Science Foundation of Chongqing (No. CSTB2022NSCQ-MSX0080).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
How to cite this article: Xiao L, Zhang F, Cheng C, Yang N, Huang Q, Yang Y. Effect of health literacy on hospital readmission among patients with heart failure: A protocol for systematic review and meta-analysis. Medicine 2024;103:38(e39644).
Contributor Information
Lei Xiao, Email: 2022110594@stu.cqmu.edu.cn.
Fan Zhang, Email: zhangfan@cqmu.edu.cn.
Cong Cheng, Email: 2021110595@stu.cqmu.edu.cn.
Ningling Yang, Email: 2022120851@stu.cqmu.edu.cn.
Qi Huang, Email: 2022120797@stu.cqmu.edu.cn.
References
- [1].Metra M, Teerlink JR. Heart failure. Lancet. 2017;390:1981–95. [DOI] [PubMed] [Google Scholar]
- [2].Roberts NLS, Mountjoy-Venning WC, Anjomshoa M, Banoub JAM, Yasin YJ; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study (vol 392, pg 1789, 2018). Lancet. 2019;393:E44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11:e004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Allen LA, Gheorghiade M, Reid KJ, et al. Identifying patients hospitalized with heart failure at risk for unfavorable future quality of life. Circ Cardiovasc Qual Outcomes. 2011;4:389–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lan T, Liao YH, Zhang J, et al. Mortality and readmission rates after heart failure: a systematic review and meta-analysis. Ther Clin Risk Manag. 2021;17:1307–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pham PN, Xiao H, Sarayani A, Chen M, Brown JD. Risk factors associated with 7- versus 30-day readmission among patients with heart failure using the nationwide readmission database. Med Care. 2019;57:1–7. [DOI] [PubMed] [Google Scholar]
- [7].Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press; 2004. [PubMed] [Google Scholar]
- [8].Lima MA, Duque AP, Rodrigues Junior LF, Lima VC, Trotte LA, Guimaraes TC. Health literacy and quality of life in hospitalized heart failure patients: a cross-sectional study. Am J Cardiovasc Dis. 2020;10:490–8. [PMC free article] [PubMed] [Google Scholar]
- [9].Gomez R, Andrey JL, Puerto JL, et al. Health literacy and prognosis of heart failure: a prospective propensity-matched study in the community. Eur J Cardiovasc Nurs. 2023;22:282–90. [DOI] [PubMed] [Google Scholar]
- [10].Fabbri M, Murad MH, Wennberg AM, et al. Health literacy and outcomes among patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2020;8:451–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wu JR, Moser DK, DeWalt DA, Rayens MK, Dracup K. Health literacy mediates the relationship between age and health outcomes in patients with heart failure. Circ Heart Fail. 2016;9:e002250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Rizzuto N, Charles G, Knobf MT. Decreasing 30-day readmission rates in patients with heart failure. Crit Care Nurse. 2022;42:13–9. [DOI] [PubMed] [Google Scholar]
- [13].Niu XN, Wen H, Sun N, Zhao R, Wang T, Li Y. Exploring risk factors of short-term readmission in heart failure patients: a cohort study. Front Endocrinol (Lausanne). 2022;13:1024759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wang N, Farrell M, Hales S, et al. Prevalence and seasonal variation of precipitants of heart failure hospitalization and risk of readmission. Int J Cardiol. 2020;316:152–60. [DOI] [PubMed] [Google Scholar]
- [15].McNaughton CD, Collins SP, Kripalani S, et al. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail. 2013;6:40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wu JR, Holmes GM, DeWalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28:1174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Fabbri M, Yost K, Finney Rutten LJ, et al. Health literacy and outcomes in patients with heart failure: a prospective community study. Mayo Clin Proc. 2018;93:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- [19].Sand-Jecklin K, Coyle S. Efficiently assessing patient health literacy: the BHLS instrument. Clin Nurs Res. 2014;23:581–600. [DOI] [PubMed] [Google Scholar]
- [20].Rodrigues R, de Andrade SM, González AD, Birolim MM, Mesas AE. Cross-cultural adaptation and validation of the Newest Vital Sign (NVS) health literacy instrument in general population and highly educated samples of Brazilian adults. Public Health Nutr. 2017;20:1907–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Matsuoka S, Tsuchihashi-Makaya M, Kayane T, et al. Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Educ Couns. 2016;99:1026–32. [DOI] [PubMed] [Google Scholar]
- [22].Sun H, Peng H, Fu H. Dimensional structure of health literacy scale for patients with chronic disease. J Environ Occup Med. 2013;30:171–5. [Google Scholar]
- [23].Ma C, Zhou W. Predictors of rehospitalization for community-dwelling older adults with chronic heart failure: a structural equation model. J Adv Nurs. 2020;76:1334–44. [DOI] [PubMed] [Google Scholar]
- [24].Dennison CR, McEntee ML, Samuel L, et al. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26:359–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Cox SR, Liebl MG, McComb MN, et al. Association between health literacy and 30-day healthcare use after hospital discharge in the heart failure population. Res Social Adm Pharm. 2017;13:754–8. [DOI] [PubMed] [Google Scholar]
- [26].Son YJ, Won MH. Gender differences in the impact of health literacy on hospital readmission among older heart failure patients: a prospective cohort study. J Adv Nurs. 2020;76:1345–54. [DOI] [PubMed] [Google Scholar]
- [27].Oscalices MIL, Okuno MFP, Lopes M, Batista REA, Campanharo CRV. Health literacy and adherence to treatment of patients with heart failure. Rev Esc Enferm USP. 2019;53:e03447. [DOI] [PubMed] [Google Scholar]
- [28].McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4:e001799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21:612–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Sterling MR, Safford MM, Goggins K, et al. Numeracy, health literacy, cognition, and 30-day readmissions among patients with heart failure. J Hosp Med. 2018;13:145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Li X, Zhang X, Jiang S, Yang W, Li Y, Zang X. The impact of health literacy on health behavior and outcomes of patients with chronic heart failure. J Nurs Sci. 2022;37:74–77 + 91. [Google Scholar]
- [32].Cajita MI, Cajita TR, Han HR. Health literacy and heart failure: a systematic review. J Cardiovasc Nurs. 2016;31:121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP. Impact of health literacy in patients with cardiovascular diseases: a systematic review and meta-analysis. Patient Educ Couns. 2022;105:1793–800. [DOI] [PubMed] [Google Scholar]
- [34].Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Fan ZY, Yang Y, Zhang F. Association between health literacy and mortality: a systematic review and meta-analysis. Arch Public Health. 2021;79:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22:1342–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Mahajan SM, Heidenreich P, Abbott B, Newton A, Ward D. Predictive models for identifying risk of readmission after index hospitalization for heart failure: a systematic review. Eur J Cardiovasc Nurs. 2018;17:675–89. [DOI] [PubMed] [Google Scholar]
- [38].Shin S, Austin PC, Ross HJ, et al. Machine learning vs. conventional statistical models for predicting heart failure readmission and mortality. ESC Heart Fail. 2021;8:106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]