Abstract
Extranodal intraductal papilloma of the unilateral axillary supernumerary breast is a rare and unusual medical condition. This condition involves the development of a benign tumor, known as a papilloma, in the ducts of supernumerary breast tissue found in the axilla. We report a rare case of extranodal papilloma of an extranodal intraductal papilloma of a unilateral axillary supernumerary breast in a 70-year-old woman, who presented with a right axillary mass. The diagnosis was suspected on imaging and confirmed on anatomical examination. Surgical treatment with good post-treatment outcome.
Keywords: Extranodal intraductal papilloma, Supernumerary breast, Imaging, Ultrasonography
Introduction
Intraductal papilloma is a common benign tumor of the milk ducts. It consists of a proliferation of epithelial and myoepithelial cells supported by fibrovascular nuclei, producing a characteristic arborescent architecture in the lumen of the duct [1].
Polymastia, or supernumerary breast or ectopic breast tissue, is a congenital condition corresponding to abnormally localized persistent mammary glandular tissue, usually along the milky line that extends from the armpit to the groin crease [2,3].
Intraductal papilloma arising within ectopic breast tissue is relatively a rare pathology. To our knowledge there have been only a few cases reports in the literature [4].
Patient and observation
A 70-year-old woman, without particular pathological history, presented with a right axillary mass that had been progressively growing for 4 years. Clinical examination revealed a right axillary supernumerary breast with areola and nipple (Fig. 1). Physical examination showed a mobile mass within the supernumerary breast.
Fig. 1.
Front view photograph of patient's right axillary region, showing axillary supernumerary breast.
A mammogram was performed. There were no calcifications or architectural distortion. Also, there were no abnormalities in the 2 thoracic breasts.
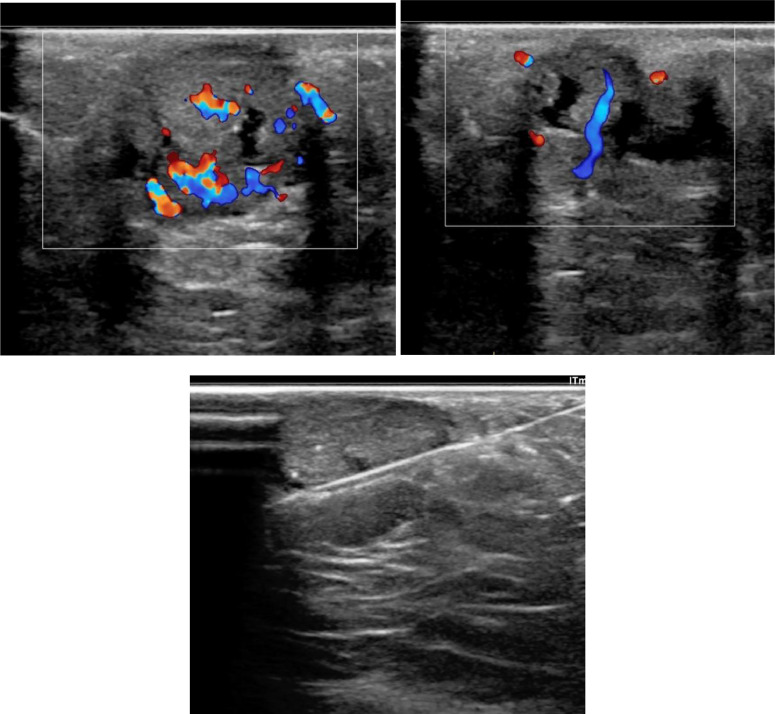
Ultrasound was performed and showed a circumscribed hypoechoic solid and cystic mass of 40 mm, the solid portion showed a Doppler signal with a vascular pedicle (Fig. 2A and B).
Fig. 2.
Breast ultrasound showed a well-circumscribed hypoechoic solid and cystic mass of 40mm, the solid portion showed a Doppler signal with a vascular pedicle (A, B). Ultrasound-guided core-needle biopsy of the lesion (C).
An ultrasound-guided core-needle biopsy of the lesion was performed (Fig. 2C).
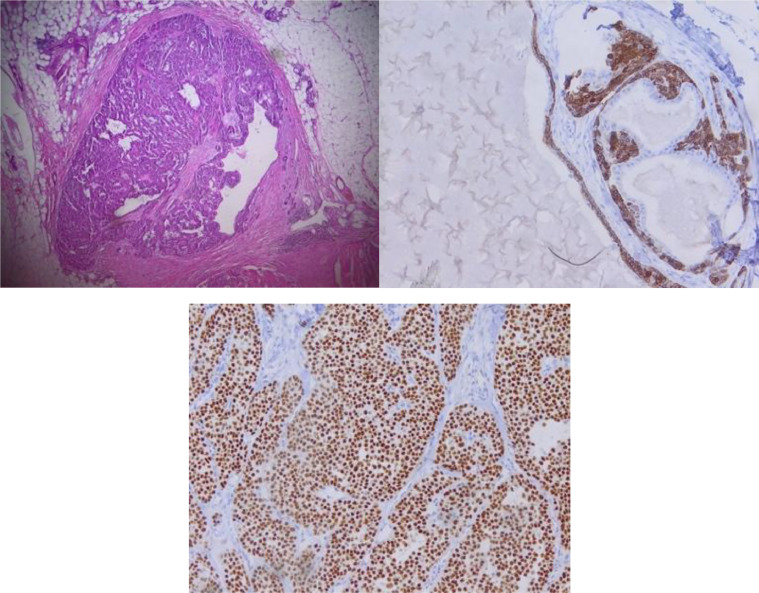
Histological study (Fig. 3) showed a circumscribed intraductal lesion made of papillary structure with fibrovascular cores lined by an outer layer of epithelial cells showing low-grade atypia, and an inner layer of myoepithelial cells. p63 and CK5/6 immunoreactivity both at the peripheral wall and along the fibrovascular cores highlighted myoepithelial cells, and CK5/6 positivity along the cores showed usual ductal hyperplasia
Fig. 3.
Histopatogical evaluation of the lesion revealed a circumscribed intraductal lesion made of papillary structure with fibrovascular cores lined by an outer layer of epithelial cells showing low-grade atypia, and an inner layer of myoepithelial cells. p63 and CK5/6 immunoreactivity both at the peripheral wall and along the fibrovascular cores highlighted myopepithelial cells, and CK5/6 positivity along the cores showed usual ductal hyperplasia.
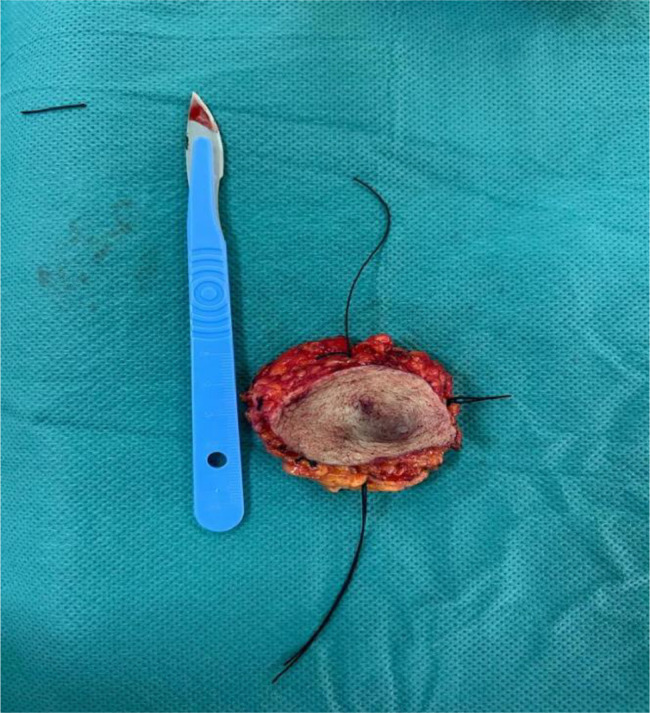
The patient subsequently underwent surgery on the supernumerary breast (Fig. 4).
Fig. 4.
Front view photograph of the supernumerary mastectomy operating room.
Discussion
Breast tissue develops along milk lines from the axillary to the pectoral thoracic region, and any premature cessation of migration will form what is known as ectopic breast tissue [2,5].
Ectopic breast tissue occurs in 2%-6% of females and 1%-3% of males. Preferentially located in the thorax or abdomen in 67% of cases, with 20% in the axilla, and other locations also reported in the literature [5].
To the best of our knowledge, intraductal papilloma (IDP) of ectopic breast tissue is rarely reported in the literature, and its development in ectopic breast tissue not included at the nodal level, is exceptional and has been reported in 3 cases in the literature with pathology history histological details [[5], [6], [7], [8]].
A solitary intraductal papilloma is usually observed on mammography as a rounded or ovoid, well-circumscribed retro areolar mass that may be associated with ductal dilatation. Smaller lesions may be occult on mammography [9].
On mammogram, IDP is difficult to detect, with a PPV of only 25% [10].
Multiple papillomas are usually peripheral in location and can be bilateral. Calcifications are uncommon and include both coarse dense calcifications and microcalcifications [9].
Ultrasound finding of a papilloma consists on a solid mural nodule within a dilated duct. Other features include an intracystic mass or a well-circumscribed hypoechoic solid mass. Ductal dilatation may be the only finding in a small papilloma. Doppler signal can depict a vascular pedicle within the mural nodule [9].
MRI is a valuable tool in detecting breast lesions and that it has a higher sensitivity and specificity in detecting papilloma than both US and mammography [10].
The management of intraductal papillomas is varied, surgical excision is generally recommended. Patients with a tumor measuring less than 1.5 cm can be potentially candidate for vacuum-assisted excision, but only if the tumor does not extend into the branching ducts [11].
Conclusion
Intraductal papilloma is a frequent pathology in women, but its localization in extranodal of supernumerary axillary unilateral breast tissue is extremely rare. Imaging is very useful in the assessment of this condition and on diagnosis confirmation by core-needle biopsy for histological examination.
Patient consent
Written and informed consent for publication of the case was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Daoud Bentaleb, Email: daoud.bentaleb@gmail.com.
Imane Miara, Email: miara.imane@gmail.com.
Ibtissam Erraad, Email: erraadibtissam18@gmail.com.
Dalale Laoudiyi, Email: laoudiyi.dal@gmail.com.
Younes Bencherifi, Email: bencherifiyounes@gmail.com.
Manal Abatourab, Email: manal.abat@gmail.com.
Asmae Mazti, Email: maztiasmae@gmail.com.
Kamilia Chbani, Email: kamiliachbani@gmail.com.
Siham Salam, Email: salamsiham@yahoo.fr.
References
- 1.Cottom H, Rengabashyam B, Turton PE, Shaaban AM. Intraductal papilloma in an axillary lymph node of a patient with human immunodeficiency virus: a case report and review of the literature. J Med Case Rep. 2014;8:162. doi: 10.1186/1752-1947-8-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andaloussi Serraj MS, Mahdaoui S, Kawtari S, Bouffetal H, Samouh N. A rare case of unilateral axillary supernumerary breast. Radiol Case Rep. 2021;16:2804–2807. doi: 10.1016/j.radcr.2021.06.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kajava Y. The proportions of supernumerary nipples in the Finnish population. Duodecim. 1915;31:143–170. [Google Scholar]
- 4.Davrayev M, Teng T, Asarian A, Genato R, Xiao P. Intraductal papilloma arising in ectopic breast tissue within the axillary region. J Surg Case Rep. 2023;2023(6):rjad302. doi: 10.1093/jscr/rjad302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad A, Al-Boukai MD. Bilateral intraductal papillomas arising in ectopic axillary breast tissue synchronously with right breast intraductal carcinoma. Saudi Med J. 2010;31(3):321–324. [PubMed] [Google Scholar]
- 6.Bae SJ, Yang GE. Rdiologic and pathologic of axillary intraductal papilloma arising in accessory breat tissue: a case report and literature review. Curr Med Imaging. 2022;18(issue 14):1526–1528. doi: 10.2174/1573405618666220511193557. [DOI] [PubMed] [Google Scholar]
- 7.Davrayev M, Teng T, Asarian A, Genato R, Philip Xiao., 3 Intraductal papilloma arising in ectopic breast tissue within the axillary region. J Surg Case Rep. 2023;6:1–2. doi: 10.1093/jscr/rjad302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaffer S, Lin R, Bleiweiss IJ, Nagi C. Intraductal carcinoma arising in intraductal papilloma in an axillary lymph node: review of the literature and proposed theories of evolution. Arch Pathol Lab Med. 2008;132:1940–1942. doi: 10.5858/132.12.1940. [DOI] [PubMed] [Google Scholar]
- 9.Jagmohan P, Pool FJ, Putti TC, Wong J. Papillary lesions of the breast: imaging findings and diagnostic challenges. Diagn Interv Radiol. 2013;19:471–478. doi: 10.5152/dir.2013.13041. [DOI] [PubMed] [Google Scholar]
- 10.Wang W, Ding J, Yang W, Li Y, Zhou L, Zhang S, et al. MRI characteristics of intraductal papilloma. Acta Radiol Online First. 2015;26(3):276–283. doi: 10.1177/0284185114526590. [DOI] [PubMed] [Google Scholar]
- 11.Zhu Q-L, Zhang J, Lai X-J, Wang H-Y, Xiao M-S, Jiang Y-X. Characterisation of breast papillary neoplasm on automated breast ultrasound. Br J Radiol. 2013;86 doi: 10.1259/bjr.20130215. [DOI] [PMC free article] [PubMed] [Google Scholar]