Abstract
Introduction
This study aimed to compare the clinical efficacy of sexual stimulation with that of placebo in the treatment of distal ureteral stones.
Methods
We searched PubMed, Web of Science, Cochrane Library, and Google Scholar from January 1, 2000 to December 31, 2022 for studies comparing the efficacy of sexual stimulus with that of placebo for the treatment of distal ureteral stones. RevMan 5.3 software was used to pool the data. The study protocol was registered on PROSPERO (Registration Number: CRD42023432408).
Results
A total of six randomized controlled trials comprising 535 cases of distal ureteral stones were included in this study. Among these, 273 cases were associated with sexual intercourse or masturbation 3–4 times a week, while 262 cases only received symptomatic treatment. The pooled results showed that the 2-week [risk ratios (RR) = 1.77, 95 % confidence interval (CI): 1.34, 2.33] and 4-week [RR = 1.48, 95 % CI: 1.29, 1.69] ureteral stone expulsion rates of the sexually stimulated group were significantly higher than those of the placebo group (ps < 0.01). Additionally, sexual stimulation was associated with a shorter ureteral stone expulsion time [weighted mean differences (WMD) = −3.74, 95 % CI: −6.27, −1.22, p < 0.01] and a decreased prevalence of renal colic attacks [WMD = −0.61, 95 % CI: −1.01, −0.22, p < 0.01] compared with those of the placebo group.
Conclusion
Appropriate sexual stimulation can enhance the spontaneous expulsion of distal ureteral stones in patients presenting with tolerable pain.
Keywords: Sexual intercourse, Masturbation, Distal ureteral stone, Meta-analysis, Randomized controlled trials
1. Introduction
Urolithiasis is one of the most prevalent urological diseases, affecting 5–10 % of the global population and associated with a 50 % lifetime recurrence rate [1]. According to the latest statistics, the annual medical expenditure for urolithiasis in the U.S. is up to 5.3 billion U.S. dollars, exhibiting an increasing trend over the years and placing a heavy burden on the patient population and society [2].
It has been established that 14 % of the cases with urolithiasis involve ureteral stones, and the expulsion of stones is largely dependent on the size and location of the calculi [3]. A meta-analysis reported that the spontaneous expulsion rates for proximal, middle and distal ureteral stones were 12 %, 22 %, 45 %, respectively, while calculi with a size of <4 mm, 4–6 mm and >6 mm had expulsion rates of 55 %, 35 % and 8 %, respectively [4]. Clinically, it is hard to predict the expulsion time, and the expulsion is generally accompanied by unbearable pain; in long-term cases, infections and renal dysfunction may be observed. Accordingly, it is essential to promote the expulsion of stones and concurrently decrease related symptoms. As recommended by the American Urological Association and European Association of Urology, medical expulsive therapy (MET) should be scheduled for patients carrying newly diagnosed ureteral stones with a size of <10 mm and having well-controlled symptoms [1,5]. Medical treatment consists of α-adrenoreceptor antagonists, calcium channel blockers, phosphodiesterase inhibitors and corticosteroids. Among these, α-adrenoreceptor antagonists are the most prescribed given their ability to reduce smooth muscle tone and peristaltic frequency of the ureter [5].
Importantly, at our hospital, we tend to use more minimally invasive or even non-invasive methods to promote stone removal. A recent randomized controlled trial (RCT) conducted by Doluogl et al. [6] first reported that sexual intercourse 3–4 times a week could significantly promote the expulsion of distal ureteral stones <6 mm in size and reduce analgesic use. They discovered that sexual activity produces high levels of nitric oxide (NO) that stimulates the non-adrenergic non-cholinergic (nitrogenous) nerves at the distal ureter, reducing ureteral tonus and peristalsis [6]. It not only promotes the passage of stones, but also reduces the use of analgesics. In support of this hypothesis, a series of studies have shown the effectiveness and safety of sexual stimulation in the expulsion of ureteral stones. We undertook a meta-analysis to provide a comprehensive evaluation of the role of sexual stimulation in the expulsion of distal ureteral stones.
2. Materials and methods
2.1. Search strategy and literature selection
This meta-analysis was performed according to the Preferred Reporting Items for Systemic Reviews and Meta-analysis (PRISMA) statement [7]. PubMed, Web of Science, Cochrane Library, and Google Scholar databases were systematically searched from January 1, 2000 to December 31, 2022, to retrieve all randomized controlled trials (RCTs) comparing the efficacy of sexual stimulus and placebo for the treatment of distal ureteral stones. There was no language restriction. Search terms included: “sexual stimulation”, “sexual stimulus”, “sexual stimuli”, “sexual intercourse”, “masturbation”, “ureteral stones”, “ureteral calculi”, “ureteric stones”, “distal ureteral stones.” Our study protocol was registered on PROSPERO (Registration Number: CRD42023432408).
The criteria for including studies in this meta-analysis were as follows: 1) RCT studies; 2) The study participants were patients diagnosed with distal ureteral stones and aged >18 years, with no restrictions on sex, nation and race/ethnicity; 3) In the experimental group, patients were advised to engage in sexual intercourse or masturbation at least three times per week; in the placebo group, participants were instructed not to engage in sexual intercourse or masturbation during the study; 4) All the patients were advised to drink 1.5–2.0 L of water daily, and informed that they would receive symptomatic treatment on demand that would be non-steroidal anti-inflammatory drugs to be taken orally or as an intramuscular injection when attacked by renal colic; 5) At least one of the following outcome measures was included in the study: stone expulsion rate, stone expulsion time, analgesic use.
The criteria for excluding studies from this meta-analysis were as follows: 1) Non-RCT studies; 2) Duplicate studies; 3) Data not available or extractable from the study; 3) Studies comprising patients with erectile dysfunction, renal insufficiency, urinary infection, fever, high grade hydronephrosis, solitary kidney, history of ureteral surgery or previous endoscopic procedures, ureteric strictures, stones ≥15 mm in size, stone located in the mid- or proximal ureter.
2.2. Data extraction and quality assessment
Two researchers independently performed the literature search and assessed the eligibility of each study according to the inclusion/exclusion criteria by reading the titles and abstracts. Any points of disagreement were resolved by discussion with a third researcher. The following contents were extracted: 1) General data, including the first author, publication time, nation, literature type; 2) Patient characteristics, including sex, age, grouping information, interventions, stone size, observation time; 3) Outcome measures, including stone expulsion rate, stone expulsion time, analgesic use. An assessment of research quality was carried out using the modified Jadad scale. According to the criteria for this assessment, studies with a Jadad score of >4 points were considered of high quality, where the maximus Jadad score is 7 points.
2.3. Statistical analysis
Statistical analysis was performed by Revman 5.3 software (Cochrane Collaboration, Oxford, United Kingdom). Dichotomous variables were expressed as Risk Ratios (RR) with a 95 % confidence interval (CI), and continuous categories were expressed as weighted mean differences (WMD). A P-value <0.05 was deemed statistically significant. Heterogeneity was assessed using the χ2 and I2 statistics. A random-effects model was used upon significant heterogeneity (I2 ≥ 50 %, p ≤ 0.1); otherwise, a fixed-effects model was used. A Forest plot was generated to visualize the results.
3. Results
3.1. Search results and study characteristics
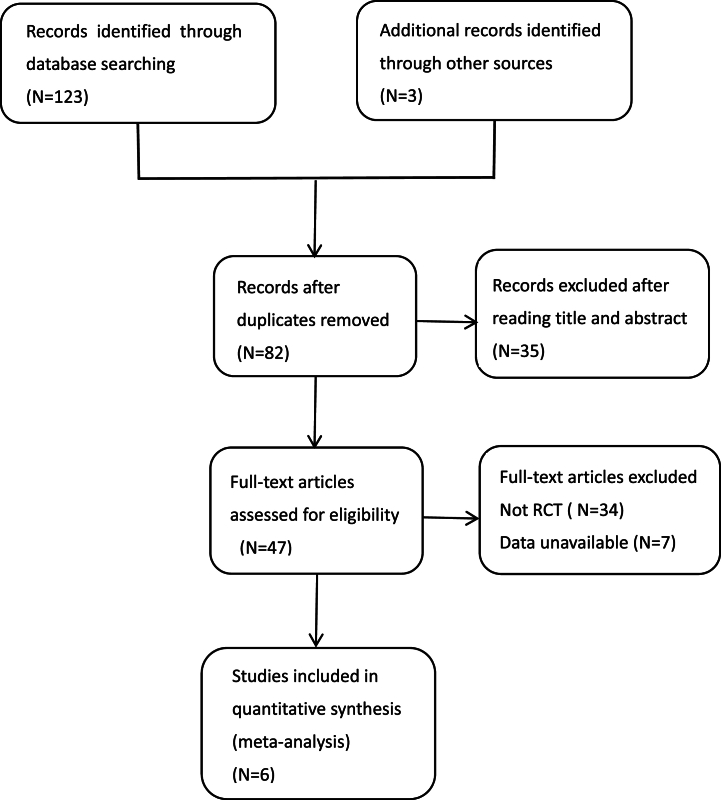
A flow diagram of the literature screening process is displayed in Fig. 1. A total of six high-quality RCTs were included in this study. The basic information and quality assessment of the included studies are detailed in Table 1. Four of the included studies allocated patients into three groups: experimental group, MET group, and placebo group [6,[8], [9], [10]]; the remaining two RCTs did not involve an MET group [11,12]. Accordingly, our meta-analysis only compared the experimental group to the placebo group. A total of 535 patients were included in the present meta-analysis, where 273 (51.0 %) patients formed the experimental group and had sexual intercourse or masturbated 3–4 times a week, and 262 (49.0 %) participants of the placebo group only received symptomatic treatment. The study participants were predominantly men (n = 465, 86.9 %), and the average follow-up time was approximately 2–4 weeks.
Fig. 1.
Literature screening process of our meta-analysis.
Table 1.
Characteristics and quality assessment of included studies.
| Study | Country | Therapy in the experimental group | Therapy in the placebo group | Therapy in the MET group | Sample size: experiment/placebo/MET | Age: Mean ± SD, years |
Stone size: Mean ± SD, mm | Duration of treatment | Included population | Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|
| Doluoglu 2015 [6] | Turkey | Sexual intercourse at least 3 times per week | symptomatic treatment | received 0.4 mg tamsulosin daily | 31/23/21 | 34.9 ± 10.6/34 ± 10.4/39.3 ± 8.1 | 4.7 ± 0.8/4.9 ± 0.8/5 ± 1 | 4 weeks | Married males diagnosed with distal ureteral stones 6 mm in size. | 6 |
| Abdel-Kader 2017 [11] | Egypt | Sexual intercourse 3–4 times per week | symptomatic treatment | NA | 28/28/NA | 36.5 ± 10.7/37.3 ± 12.5/NA | 7.03 ± 1.59/6.69 ± 1.33/NA | 4 weeks | Married males diagnosed with distal ureteral stones 5–10 mm in size. | 5 |
| Bayraktar 2017 [10] | Turkey | Sexual intercourse at least 3 times per week | symptomatic treatment | received 0.4 mg tamsulosin daily | 66/64/60 | 38.6 ± 14.1/36.92 ± 12.4/34.4 ± 13.5/ | 7.01 ± 1.4/7.1 ± 1.3/7.09 ± 1.4 | 4 weeks | Married males diagnosed with distal ureteral stones 5–10 mm in size. | 6 |
| Li 2020 [9] | China | Sexual intercourse at least 3 times per week | symptomatic treatment | received 0.4 mg tamsulosin daily | 70/68/71 | 35.1 ± 8.3/34.1 ± 8.4/35.3 ± 8.1 | 11.1 ± 2.4/11.9 ± 2.3/10.6 ± 1.9 | 2 weeks | Married males diagnosed with distal ureteral stones 7–15 mm in size that underwent SWL within 24 hours. | 5 |
| Turgut 2021-1 [12] | Turkey | Sexual intercourse 3–4 times per week | symptomatic treatment | NA | 35/35/NA | 36.4 ± 10.8/37.1 ± 12.4/NA | 7.01 ± 1.6/6.67 ± 1.4/NA | 4 weeks | Married females diagnosed with distal ureteral stones <10 mm in size. | 6 |
| Turgut 2021-2 [8] | Turkey | Masturbation at least 3–4 times per week | symptomatic treatment | received 0.4 mg tamsulosin daily | 43/44/41 | 37 ± 5/38.4 ± 6.8/37.6 ± 4.6 | 6.93 ± 1.1/6.87 ± 1.1/7.1 ± 0.9 | 4 weeks | Adult males diagnosed with distal ureteral stones 5–10 mm in size. | 6 |
Symptomatic treatment: usage of non-steroidal anti-inflammatory drugs when attacked by renal colic. NA: Not available.
All the patients were advised to drink 1 0.5–2.0 L of water daily, and they would receive symptomatic treatment on demand.
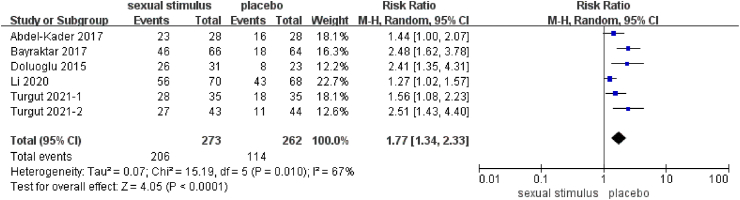
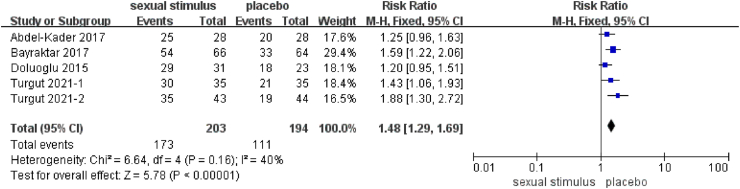
3.2. Stone expulsion rate
The stone expulsion rate was reported in all RCT studies (n = 6) included in this meta-analysis. The pooled results showed that sexual stimulation yielded a significantly higher 2-week ureteral stone expulsion rate than the placebo group [RR = 1.77, 95 % CI: 1.34, 2.33, I2 = 67 %, p < 0.01] (Fig. 2). Five studies reported the 4-week stone expulsion rate; similar to the 2-week data, these studies reported a significantly higher stone expulsion rate for the sexual stimulation group compared to the placebo group [RR = 1.48, 95 % CI: 1.29, 1.69, I2 = 67 %, p < 0.01] (Fig. 3).
Fig. 2.
Forest plot of 2-week ureteral stone expulsion rate.
Fig. 3.
Forest plot of 4-week ureteral stone expulsion rate.
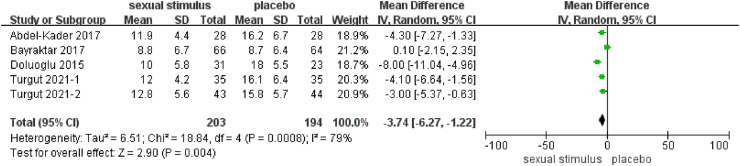
3.3. Stone expulsion time
Five RCT studies included in this meta-analysis reported the stone expulsion time. The pooled results showed that sexual stimulation significantly reduced the time for stone expulsion compared to the placebo group [WMD = −3.74, 95 % CI: −6.27, −1.22, I2 = 79 %, p < 0.01] (Fig. 4).
Fig. 4.
Forest plot of the stone expulsion time.
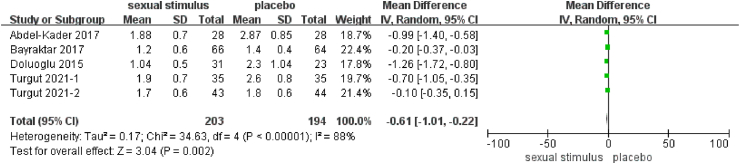
3.4. Analgesic use
It is widely established that usage of non-steroidal anti-inflammatory medications is required upon the onset of renal colic. All RCT studies included in this meta-analysis reported data on analgesic use, and the pooled results revealed that sexual stimulation was associated with a significant decrease in analgesic use [WMD = −0.61, 95 % CI: −1.01, −0.22, I2 = 88 %, p < 0.01] (Fig. 5).
Fig. 5.
Forest plot of analgesic use.
4. Discussion
The past decade has witnessed significant medical progress as multiple invasive/non-invasive approaches have been developed for the management of ureteral stone expulsion, including conservative therapy, MET, external shock wave lithotripsy (ESWL), ureterorenoscopic lithotripsy, percutaneous nephrolithotomy, and laparoscopic ureterolithotomy [13]. Among these, MET remains the mainstay of treatment for distal ureteral stones <10 mm in size [5,14]. It is widely believed that MET can increase the stone passage rate by 65 % [14]. Many factors, including the stone location, size, number, type, ureteral spasm, mucosal inflammation and edema, and the ureteral anatomy, have been established to influence the expulsion of ureteral stones [15]. Importantly, routine MET for ureteral stones can decrease edema and induce relaxation of the ureteral smooth muscle layer, thereby allowing stone passage [14,15].
α-adrenoreceptor antagonists remain the most commonly used MET drugs in clinical practice. However, they are associated with common side effects, including dizziness, headache, orthostatic hypotension, syncope, and abnormal ejaculation [16]. It has been shown that the incidence of side effects varies according to the different types of α-adrenoreceptor antagonists prescribed. Tamsulosin is the most used clinically, with a side effect prevalence of 20 % [17]. Therefore, many patients discontinue treatment due to various side effects. Doluogl et al. [6] first reported the effect of sexual stimulation in the treatment of distal ureteral stones that is more efficient, less expensive, has fewer side effects, and provides a novel therapeutic option to treat ureteral calculi.
In the present study, we sought to reveal whether sexual stimulation (3–4 times a week of sexual intercourse or masturbation) could promote the passage of distal ureteral stones. Similar to the mechanism of phosphodiesterase 5 inhibitors (PDE5i), sexual stimulation promotes ureteral stone expulsion through the NO/cyclic guanosine monophosphate (cGMP) pathway to relax ureteral smooth muscle. It is known that ureteral peristalsis is a myogenic process mediated by neurogenic factors. Biologically, the smooth muscle activity in the distal ureter and the ureterovesical junction is regulated by a combination of noradrenergic, cholinergic, and non-adrenergic non-cholinergic nerves [18]. NO is a well-recognized non-adrenergic non-cholinergic inhibitory neurotransmitter that acts as an important gaseous regulator in different visceral organs and is important for smooth muscle relaxation. An increasing body of evidence suggests that the distal ureter is rich in nitrergic nerve fibers that are responsible for the synthesis of NO that regulates the key transmitters involved in ureteral peristalsis, resistance to urinary flow, and regional blood flow [[19], [20], [21]].
Similarly, NO plays an important role in triggering and maintaining human sexual activity [22]. It has been established that NO is the main neurotransmitter responsible for penile erection and clitoral congestion [23,24]. Interestingly, the level of circulating NO increases following sexual stimulation until orgasm [20]. High NO concentrations are known to exert a positive effect on ureteral smooth muscle relaxation, altering the activities in the Ca2+ and K+ channels in smooth muscle cells by activating soluble guanylyl cyclase and elevating the level of cyclic guanosine monophosphate in cells [25,26]. Over the years, selective PDE5is have been widely used to treat erectile dysfunction in men. Multiple PDE5is, such as Sildenafil, Vardenafil and Tadalafil, have been demonstrated to promote the expulsion of ureteral stones by increasing blood NO concentrations [27]. Hedlund et al. [20] found that sublingual administration of NO donors, such as isosorbide dinitrate, could reduce the ureteral smooth muscle tone. It was also found that NO could suppress the release of norepinephrine from the neuromuscular junctions [25]. These findings corroborate that either externally ingested or self-generated NO can reduce the peristaltic frequency, basal tone and decrease the incidence of spasms, providing a theoretical foothold for developing new methods to enhance the expulsion of ureteral stones.
In our meta-analysis, we found that the 2-week and 4-week expulsion rates in the experimental group were significantly higher than in the placebo group, and experimental group needed less ureteral stone expulsion time. Sexual activity induces the release of a significant quantity of NO from nerve endings that can act on the distal ureter to decrease tension in the ureteral wall, improve urine flow, elevate pressure above the stone, inhibit ureteral peristalsis, reducing distal stone resistance, and ultimately creating a potent pressure gradient that facilitates stone expulsion [11]. In addition to improving ureteral factors, NO has the potential to enhance renal blood flow and glomerular filtration rate, thereby increasing urine volume and facilitating the passage of stones [28]. Recently, Jayant et al. [29] conducted an RCT to compare the clinical effect of tamsulosin versus tamsulosin plus tadalafil in ureteral stone expulsion. They found that adding tadalafil yielded a higher rate of ureteral stone excretion (83.6 % vs 65.5 %, p = 0.031) and less expulsion time (14.9 ± 4.4 vs 16.7 ± 4.8 days, p = 0.003). In this regard, a meta-analysis by Bai et al. [30] showed that treatment with tadalafil alone or with tamsulosin in patients with distal ureteral stones resulted in a higher stone expulsion rate and shorter stone passage time, consistent with our findings. Interestingly, Li et al. [9] reported that sexual intercourse at least 3 times a week in patients receiving ESWL could significantly reduce the formation of steinstrasse and enhance stone expulsion.
Presently, nonsteroidal anti-inflammatory drugs are frequently employed for pain management in cases of acute ureteral obstruction. We also documented a decreased prevalence of renal colic attacks and analgesic use in patients that underwent sexual stimulation. Theoretically, faster stone clearance could potentially decrease the necessity for analgesic use. Elevating endogenous NO levels has been shown to markedly decrease the incidence of renal colic in patients with ureteral stones. Li et al. [9] demonstrated that patients in the sexual stimulation group exhibited lower visual analog scale pain scores in comparison to those in the placebo group, indicating improved pain experience among the former. This may be one of the reasons that sexual stimulation can reduce the need for analgesia.
Of the six RCT studies we included in the present meta-analysis, four studies included an MET group [6,[8], [9], [10]]. We analyzed the data for the experimental and MET groups; however, no statistically significant difference was found in outcomes such as stone expulsion rate, stone expulsion time, and analgesic use between the two groups. Other data had high heterogeneity, so we did not include the sexual stimulation group versus MET analysis in our study. However, Doluoglu et al. [6] demonstrated that sexual stimulation resulted in higher 2-week expulsion rate and shorter expulsion time compared to MET. We found that patients in their study had the smallest stones suggesting that sexual stimulation was most effective for stones under 6 mm in size. They included the youngest patients who had more frequent, longer, and higher-quality sexual activity, and this may also have influenced the results. In the other three RCTs, no significant difference in stone expulsion rate or time between the two groups was evident [[8], [9], [10]]. First, a factor of concern was the possibility that the patients may not effectively adhere to the prescribed intervention. Second, different types of stones have varying compositions and shapes, affecting their ability to be expulsed. For example, smooth stones like calcium oxalate are easier to pass, while rough stones like calcium phosphate are more difficult [31]. Third, sex factors may be important: men have higher sexual desire than women in scientific studies for sexualities, while men who are more dominant in sexual activities are more likely to reach orgasm [12]. Lastly, nation and race or ethnicity factors combine with varying diets and climates, resulting in different types of ureteral stones, as well as differing sexual cultures [32]. These factors may explain the differing results from various previous studies.
All studies included in our meta-analysis were from randomized, double-blind, placebo-controlled trials. We found that all these RCTs were of high quality, according to the modified Jadad scale. Our study has some limitations. First, our study included a relatively small number of studies that originated from specific locations (e.g., Turkey, Egypt), restricting the applicability of the results to a wider population. We hope that more researchers will conduct this valuable research in future. We will add studies from various geographic regions to strengthen our study in the future. Second, it remains unclear whether the patients in both intervention and placebo groups strictly followed the specified measures, and we are unaware as to whether the enrolled patients reached orgasm. To improve accuracy, one may consider increasing patient follow-up frequency to minimize the impact of patient compliance and recall errors on the results. Third, we did not consider factors like stone composition, sex, race, ethnicity, and other parameters that impact stone expulsion. To minimize their influence on the results, these factors can be used for subgroup analysis. Further, the effect of other involuntary types of erection, such as sleep-related erections, on the study results could not be controlled or excluded.
5. Conclusion
We conclude that sexual stimulation can efficiently promote the expulsion of distal ureteral stones, reduce the expulsion time, and concurrently decrease the need for analgesics.
Statement of ethics
Review and/or approval by an ethics committee was not needed for this study because this study is based exclusively on published literature.
Funding sources
This manuscript did not receive any funding.
Data availability statement
Data included in article/supp. material/referenced in article.
CRediT authorship contribution statement
Cheng-Xia Peng: Writing – review & editing, Writing – original draft, Methodology. Ming-Hui Zhou: Writing – review & editing, Writing – original draft. Dan-Ping Zhao: Data curation. Guang-Hao Wu: Formal analysis. Li Xu: Software. Chao Feng: Resources.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Moe O.W., Pearle M.S., Sakhaee K. Pharmacotherapy of urolithiasis: evidence from clinical trials. Kidney Int. 2011;79(4):385–392. doi: 10.1038/ki.2010.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corbo J., Wang J. Kidney and ureteral stones. Emerg. Med. Clin. 2019;37(4):637–648. doi: 10.1016/j.emc.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Schlomer B.J. Urologic treatment of nephrolithiasis. Curr. Opin. Pediatr. 2020;32(2):288–294. doi: 10.1097/MOP.0000000000000849. [DOI] [PubMed] [Google Scholar]
- 4.Özsoy M., Liatsikos E., Scheffbuch N., Kallidonis P. Comparison of silodosin to tamsulosin for medical expulsive treatment of ureteral stones: a systematic review and meta-analysis. Urolithiasis. 2016;44(6):491–497. doi: 10.1007/s00240-016-0872-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skolarikos A. Medical treatment of urinary stones. Curr. Opin. Urol. 2018;28(5):403–407. doi: 10.1097/MOU.0000000000000523. [DOI] [PubMed] [Google Scholar]
- 6.Doluoglu O.G., Demirbas A., Kilinc M.F., Karakan T., Kabar M., Bozkurt S., et al. Can sexual intercourse Be an alternative therapy for distal ureteral stones? A prospective, randomized, controlled study. Urology. 2015;86(1):19–24. doi: 10.1016/j.urology.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turgut H., Sarıer M. Evaluation of the efficacy of masturbation on distal ureteral stones: a prospective, randomized, controlled study. Int. Urol. Nephrol. 2021;53(4):655–660. doi: 10.1007/s11255-020-02672-y. [DOI] [PubMed] [Google Scholar]
- 9.Li W., Mao Y., Lu C., Gu Y., Gu X., Hua B., et al. Role of sexual intercourse after shockwave lithotripsy for distal ureteral stones: a randomized controlled trial. Urol. J. 2020;17(2):134–138. doi: 10.22037/uj.v0i0.5400. [DOI] [PubMed] [Google Scholar]
- 10.Bayraktar Z., Albayrak S. Sexual intercourse as a new option in the medical expulsive therapy of distal ureteral stones in males: a prospective, randomized, controlled study. Int. Urol. Nephrol. 2017;49(11):1941–1946. doi: 10.1007/s11255-017-1677-9. [DOI] [PubMed] [Google Scholar]
- 11.Abdel-Kader M.S. Evaluation of the efficacy of sexual intercourse in expulsion of distal ureteric stones. Int. Urol. Nephrol. 2017;49(1):27–30. doi: 10.1007/s11255-016-1448-z. [DOI] [PubMed] [Google Scholar]
- 12.Turgut H. Evaluation of the efficacy of sexual intercourse on distal ureteral stones in women: a prospective, randomized, controlled study. Int. Urol. Nephrol. 2021;53(3):409–413. doi: 10.1007/s11255-020-02661-1. [DOI] [PubMed] [Google Scholar]
- 13.Ogreden E., Demirelli E., Aksu M., Tok D.S., Oğuz U. Early ureteroscopic lithotripsy in acute renal colic caused by ureteral calculi. Int. Urol. Nephrol. 2020;52(1):15–19. doi: 10.1007/s11255-019-02298-9. [DOI] [PubMed] [Google Scholar]
- 14.De Coninck V., Antonelli J., Chew B., Patterson J.M., Skolarikos A., Bultitude M. Medical expulsive therapy for urinary stones: future trends and knowledge gaps. Eur. Urol. 2019;76(5):658–666. doi: 10.1016/j.eururo.2019.07.053. [DOI] [PubMed] [Google Scholar]
- 15.Wang R.C., Addo N., Chi T., Moore C., Mallin M., Shiboski S., et al. Medical expulsive therapy use in emergency department patients diagnosed with ureteral stones. Am. J. Emerg. Med. 2017;35(8):1069–1074. doi: 10.1016/j.ajem.2017.02.040. [DOI] [PubMed] [Google Scholar]
- 16.Conway J.C., Friedman B.W. Medical expulsive therapy (alpha blockers) for urologic stone disease. Acad. Emerg. Med. 2020;27(9):923–924. doi: 10.1111/acem.13935. [DOI] [PubMed] [Google Scholar]
- 17.Campschroer T., Zhu X., Vernooij R.W., Lock M.T. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst. Rev. 2018;4(4) doi: 10.1002/14651858.CD008509.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersson K.E., Persson K. The L-arginine/nitric oxide pathway and non-adrenergic, non-cholinergic relaxation of the lower urinary tract. Gen. Pharmacol. 1993;24(4):833–839. doi: 10.1016/0306-3623(93)90156-r. [DOI] [PubMed] [Google Scholar]
- 19.Mastrangelo D., Baertschi A.J., Roatti A., Amherdt M., Iselin C.E. Nitric oxide production within rat urothelial cells. J Urol. 170. 2003;(4 Pt 1):1409–1414. doi: 10.1097/01.ju.0000083492.80217.20. [DOI] [PubMed] [Google Scholar]
- 20.Hedlund P. Nitric oxide/cGMP-mediated effects in the outflow region of the lower urinary tract--is there a basis for pharmacological targeting of cGMP? World J. Urol. 2005;23(6):362–367. doi: 10.1007/s00345-005-0019-1. [DOI] [PubMed] [Google Scholar]
- 21.Fernandes V.S., Hernández M. The role of nitric oxide and hydrogen sulfide in urinary tract function. Basic Clin. Pharmacol. Toxicol. 2016;119:34–41. doi: 10.1111/bcpt.12565. [DOI] [PubMed] [Google Scholar]
- 22.Krassioukov A., Elliott S. Neural control and physiology of sexual function: effect of spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2017;23(1):1–10. doi: 10.1310/sci2301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prieto D. Physiological regulation of penile arteries and veins. Int. J. Impot. Res. 2008;20(1):17–29. doi: 10.1038/sj.ijir.3901581. [DOI] [PubMed] [Google Scholar]
- 24.Meyer-Bahlburg H.F., Dolezal C. The female sexual function index: a methodological critique and suggestions for improvement. J. Sex Marital Ther. 2007;33(3):217–224. doi: 10.1080/00926230701267852. [DOI] [PubMed] [Google Scholar]
- 25.Prieto D., Rivera L., Benedito S., Recio P., Villalba N., Hernández M., et al. Ca2+-activated K+ (KCa) channels are involved in the relaxations elicited by sildenafil in penile resistance arteries. Eur. J. Pharmacol. 2006;531(1–3):232–237. doi: 10.1016/j.ejphar.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 26.Prieto D., Rivera L., Recio P., Rubio J.L., Hernández M., García-Sacristán A. Role of nitric oxide in the relaxation elicited by sildenafil in penile resistance arteries. J. Urol. 2006;175(3 Pt 1):1164–1170. doi: 10.1016/S0022-5347(05)00320-4. [DOI] [PubMed] [Google Scholar]
- 27.Çelik S., Akdeniz F., Afsar Y.M., Bozkurt O., Gursoy B.M., Hacihasanoglu M.L., et al. Tadalafil versus alpha blockers (alfuzosin, doxazosin, tamsulosin and silodosin) as medical expulsive therapy for < 10 mm distal and proximal ureteral stones. Arch. Ital. Urol. Androl. 2018;90(2):117–122. doi: 10.4081/aiua.2018.2.117. [DOI] [PubMed] [Google Scholar]
- 28.Bądzyńska B., Vaneckova I., Sadowski J., Hojná S., Kompanowska-Jezierska E. Effects of systemic and renal intramedullary endothelin-1 receptor blockade on tissue NO and intrarenal hemodynamics in normotensive and hypertensive rats. Eur. J. Pharmacol. 2021;910 doi: 10.1016/j.ejphar.2021.174445. [DOI] [PubMed] [Google Scholar]
- 29.Jayant K., Agrawal R., Agrawal S. Tamsulosin versus tamsulosin plus tadalafil as medical expulsive therapy for lower ureteric stones: a randomized controlled trial. Int. J. Urol. 2014;21(10):1012–1015. doi: 10.1111/iju.12496. [DOI] [PubMed] [Google Scholar]
- 30.Bai Y., Yang Y., Wang X., Tang Y., Han P., Wang J. Tadalafil facilitates the distal ureteral stone expulsion: a meta-analysis. J. Endourol. 2017;31(6):557–563. doi: 10.1089/end.2016.0837. [DOI] [PubMed] [Google Scholar]
- 31.Wu W., Zhang J., Yi R., Li X., Wan W., Yu X. A simple predictive model with internal validation for assessment of stone-left after ureteroscopic lithotripsy in upper ureteral stones. Transl. Androl. Urol. 2022;11(6):786–793. doi: 10.21037/tau-22-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Randall J.H., Whiles B.B., Carrera R.V., Ito W.E., Thompson J.A., Duchene D.A., et al. On the rocks: can urologists identify stone composition based on endoscopic images alone? A worldwide survey of urologists. World J. Urol. 2023;41(2):575–579. doi: 10.1007/s00345-022-04269-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supp. material/referenced in article.