Abstract
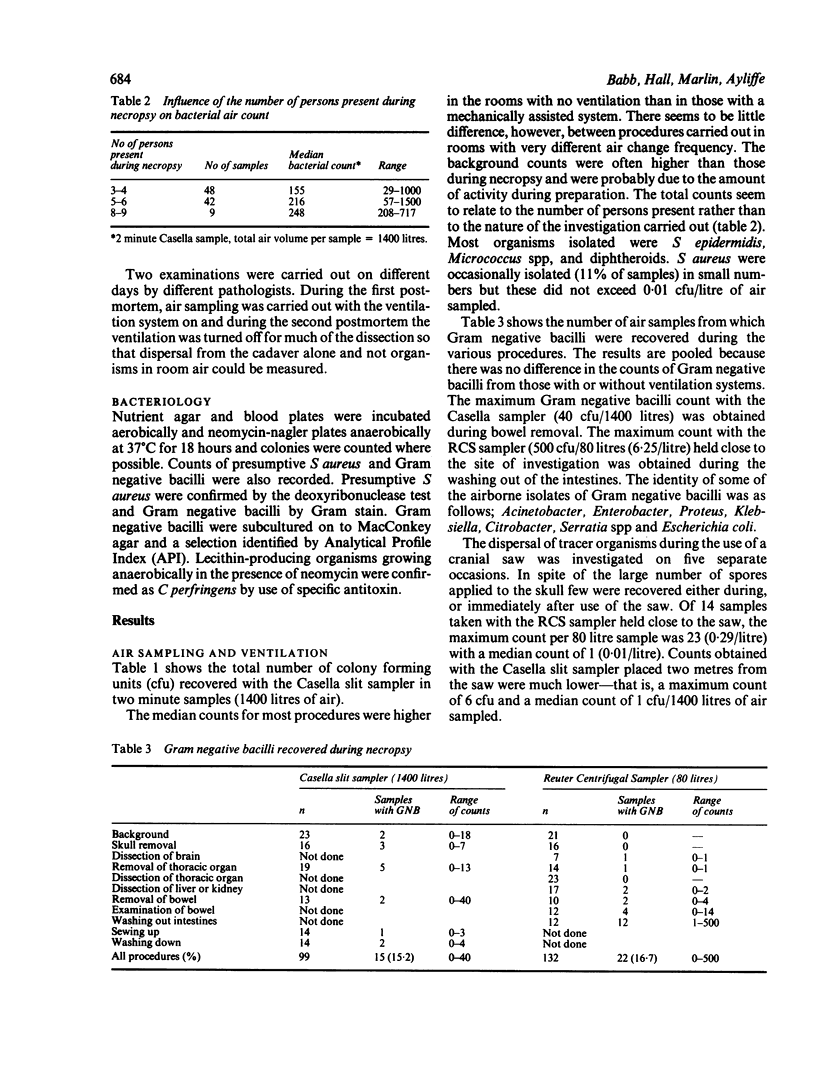
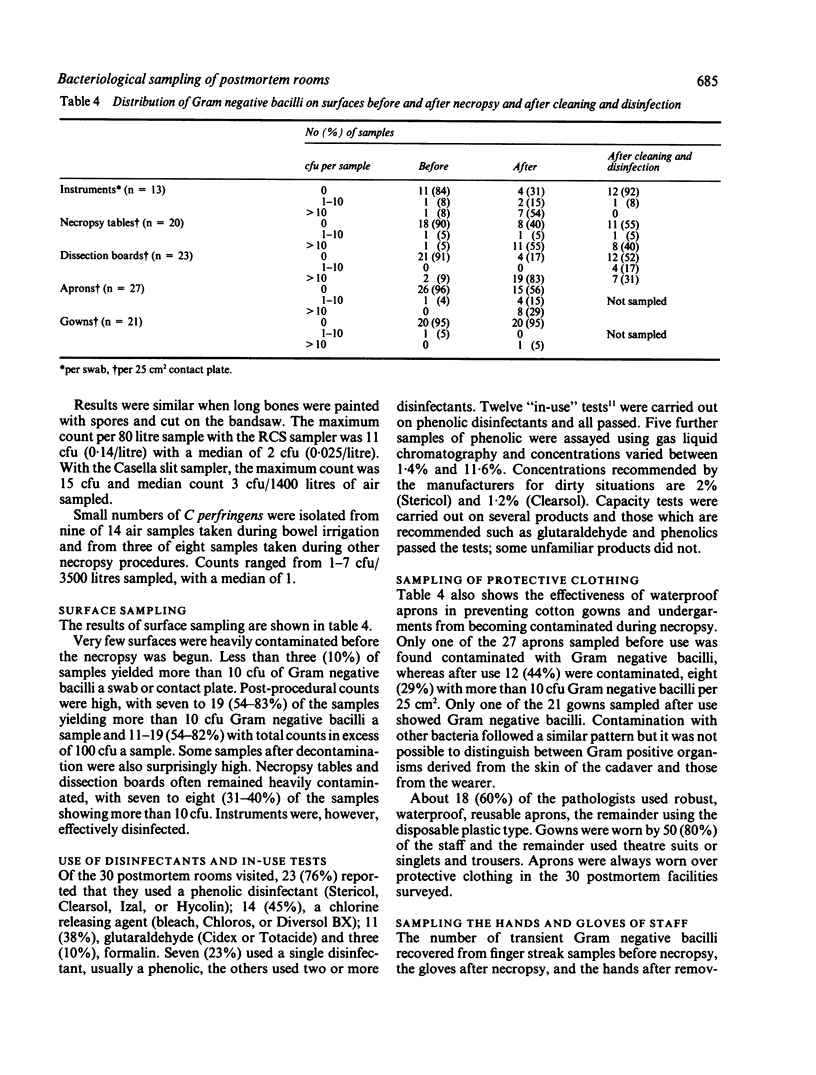
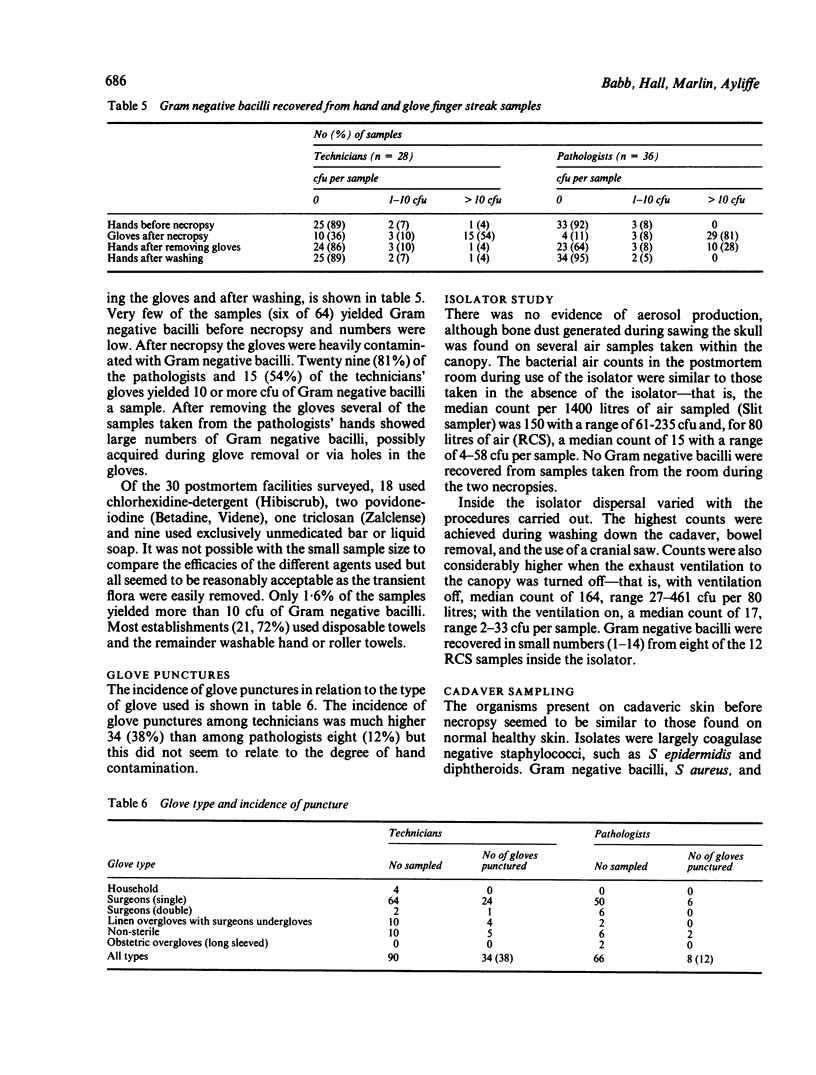
Thirty hospital and coroners' postmortem rooms in the West Midlands were visited over two years. The design, environmental facilities, and hygienic practices were investigated and air exchange rates were measured. Microbiological samples were taken from the environment and from gloves, hands, and protective clothing of staff. Glove punctures were also recorded and a plastic isolator evaluated. Bacterial counts in the air were low and related more to the number of people in the room than to the air exchange rate. There was little evidence of the production of aerosol containing bacteria, although splashing occurred while intestines were being washed out. Surfaces often remained contaminated with Gram negative bacilli after cleaning but numbers were considerably reduced on drying. Decontamination of instruments was satisfactory. A wide range of disinfectants and concentrations was used, but none showed evidence of contamination. Gloves were heavily contaminated after use, and occasionally the hands of the wearer after removal of the gloves. Washing the hands effectively removed residual transient organisms, irrespective of the agent used. The incidence of glove punctures was higher among technicians (38%) than pathologists (12%). The plastic isolator reduced smells and limited environmental contamination but visibility and acceptability were poor. The results of the study suggest that there is little evidence of risk of infection to staff, providing basic hygienic precautions are taken, but consideration should be given to the prevention of glove punctures.
Full text
PDF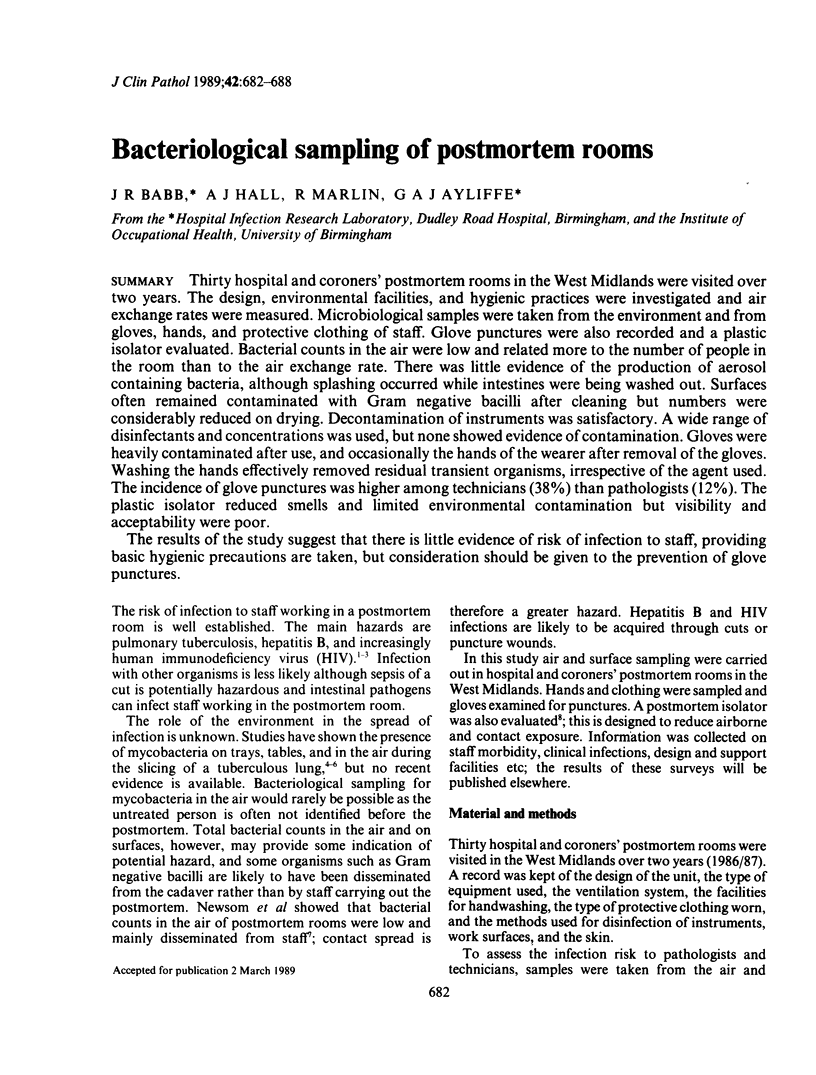


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ayliffe G. A., Bridges K., Lilly H. A., Lowbury E. J., Varney J., Wilkins M. D. Comparison of two methods for assessing the removal of total organisms and pathogens from the skin. J Hyg (Lond) 1975 Oct;75(2):259–274. doi: 10.1017/s002217240004729x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist N. R., Emslie J. A. Infections in British clinical laboratories, 1984-5. J Clin Pathol. 1987 Aug;40(8):826–829. doi: 10.1136/jcp.40.8.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist N. R., Emslie J. Infections in British clinical laboratories, 1982-3. J Clin Pathol. 1985 Jul;38(7):721–725. doi: 10.1136/jcp.38.7.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington J. M., Shannon H. S. Incidence of tuberculosis, hepatitis, brucellosis, and shigellosis in British medical laboratory workers. Br Med J. 1976 Mar 27;1(6012):759–762. doi: 10.1136/bmj.1.6012.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan W. P., Jr, Dahl M., Albert H. L. Contact dermatitis from glutaraldehyde. Arch Dermatol. 1972 Jan;105(1):94–95. [PubMed] [Google Scholar]
- LOWBURY E. J., LILLY H. A. A selective plate medium for Cl. welchii. J Pathol Bacteriol. 1955 Jul;70(1):105–109. doi: 10.1002/path.1700700110. [DOI] [PubMed] [Google Scholar]
- Newsom S. W., Rowlands C., Matthews J., Elliot C. J. Aerosols in the mortuary. J Clin Pathol. 1983 Feb;36(2):127–132. doi: 10.1136/jcp.36.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- REID D. D. Incidence of tuberculosis among workers in medical laboratories. Br Med J. 1957 Jul 6;2(5035):10–14. doi: 10.1136/bmj.2.5035.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trexler P. C., Gilmour A. M. Use of flexible plastic film isolators in performing potentially hazardous necropsies. J Clin Pathol. 1983 May;36(5):527–529. doi: 10.1136/jcp.36.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]


