Abstract
Background
Treating obesity may be a pathway to prevent and control hypertension. In the SURMOUNT-1 trial in people with obesity or overweight with weight-related complications, 72-week tirzepatide treatment led to clinically meaningful body weight and blood pressure reduction. Post hoc analyses were conducted to further explore the effects of tirzepatide on the pattern of blood pressure reduction and whether the effects were consistent across various subgroups.
Methods
The mixed effect for repeated measure model was used to compare changes in overall blood pressure, across demographic and clinical subgroups, baseline blood pressure subgroups and hypertension categories between SURMOUNT-1 participants randomised to treatment with tirzepatide and placebo. The association between weight changes and blood pressure and adverse events associated with low blood pressure were also evaluated by mediation analysis.
Results
Tirzepatide treatment was associated with a rapid decline in systolic and diastolic blood pressure over the first 24 weeks, followed by blood pressure stabilisation until the end of the observation period, resulting in a significant net reduction by 72 weeks of 6.8 mm Hg systolic and 4.2 mm Hg diastolic blood pressure versus placebo. Participants randomly assigned to any tirzepatide group were more likely than those assigned to placebo to have normal blood pressure at week 72 (58.0% vs 35.2%, respectively). The effects were broadly consistent across baseline blood pressure subgroups, shifting the blood pressure distribution curve to lower blood pressure levels. The mediation analysis indicated that weight loss explained 68% of the systolic and 71% of the diastolic blood pressure reduction. Low blood pressure adverse events were infrequent, but the rate was higher in the tirzepatide group.
Conclusions
In these post hoc analyses, in participants with obesity or overweight, tirzepatide was associated with reduced blood pressure consistently across participant groups primarily via weight loss, with relatively few blood pressure-related adverse events.
Trial registration number
Keywords: Hypertension
WHAT IS ALREADY KNOWN ON THIS TOPIC
Tirzepatide reduced blood pressure in people living with obesity or overweight in the SURMOUNT-1 trial. The ambulatory blood pressure monitoring sub-study additionally reported consistent daytime and night-time systolic blood pressure effects across clinically relevant subgroups after 36 weeks of treatment.
WHAT THIS STUDY ADDS
The present post hoc analyses demonstrated that 72-week treatment with tirzepatide was associated with consistent reductions in blood pressure, shifting the blood pressure distribution curve to the left, frequently leading to normalisation of blood pressure values in participants with elevated blood pressure and stage 1 and stage 2 hypertension at baseline, with relatively few blood pressure-related adverse events. The effects were largely mediated by weight change.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Pharmacological treatment of obesity with tirzepatide may be a novel strategy to help prevent or control hypertension and its complications.
Introduction
Hypertension persists as a leading contributor to global disability and premature death. The Global Burden of Disease Study has estimated that high systolic blood pressure (SBP) is the leading global risk factor for death and disability.1 An analysis of more than 1.5 million individuals from eight geographic regions identified SBP as contributing the highest population-attributable fraction of all cardiovascular disease risk factors.2 While global prevalence of hypertension is rising,3 the proportion of people in the USA with controlled blood pressure (BP) is declining,4 with evidence of increasing hypertension-associated mortality.5
Weight gain increases BP6; therefore, treating obesity may be a pathway to prevent and control hypertension. Marked weight loss, such as that associated with bariatric surgery7 or very low-calorie diets,8 can substantially reduce BP.9 A recent meta-analysis showed that incretin-based anti-obesity medications may also have favourable effects on BP.10
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for the treatment of type 2 diabetes and obesity. In the SURMOUNT-1 trial, tirzepatide showed reductions in body weight and office BP in people living with obesity or overweight.11 The 24-hour pattern of BP changes with tirzepatide was further characterised in a subset (n=600) of SURMOUNT-1 participants, using ambulatory blood pressure monitoring (ABPM).12 In this post hoc analysis of SURMOUNT-1, we characterised the pattern and consistency of BP reductions across tirzepatide doses and subgroups of participants with various baseline BP, demographic and clinical characteristics, as well as the frequency of BP-related adverse events, during 72-week observation. Additionally, we evaluated what proportion of BP reduction was mediated by weight reduction. Through this study, we sought insight into the potential utility of tirzepatide for hypertension prevention and treatment.
Methods
Study design and participants
SURMOUNT-1 was a phase 3 randomised, double-blind, placebo-controlled trial in which adults with a body mass index (BMI) ≥30 kg/m2 or ≥27 kg/m2 and at least one weight-related complication, excluding diabetes, were assigned to once weekly, subcutaneous tirzepatide (5 mg, 10 mg or 15 mg) or placebo for 72 weeks as an adjunct to lifestyle intervention. Subjects were excluded if they had an SBP ≥160 mm Hg or diastolic blood pressure (DBP) ≥100 mm Hg at screening. The trial protocol (online supplemental file 1) and results have been published previously.11 We did not involve patients or the public in the design, conduct, reporting or dissemination plans for this post hoc analysis.
heartjnl-2024-324170supp001.pdf (1.8MB, pdf)
BP was measured at every office visit with an automated BP machine after the participant sat quietly for 5 min. Three measurements were taken at least 1 min apart using the same arm. The average value was used for analysis. Participants continued their baseline antihypertensive medications, and investigators were allowed to adjust them during the trial, per their clinical judgement.
Changes from baseline in SBP and DBP were prespecified key secondary and secondary endpoints of SURMOUNT-1, respectively. Post hoc endpoints included changes in BP by age, sex, BMI, BP categories and use of antihypertensive medications.
Blood pressure categories
Participants were categorised by BP according to definitions described in the 2017 multi-society Guideline for High Blood Pressure in Adults13: normal (SBP<120 mm Hg and DBP<80 mm Hg), elevated (SBP 120–129 mm Hg and DBP<80 mm Hg), stage 1 hypertension (SBP 130–139 mm Hg or DBP 80–89 mm Hg), stage 2 hypertension (SBP≥140 mm Hg or DBP≥90 mm Hg).
Statistical analysis
Randomised participants who took at least one dose of the study drug were included in the modified intent-to-treat population (mITT). Participants were analysed according to the treatment they were randomly assigned, regardless of the treatment received. All analyses were conducted based on the efficacy analysis set, which included data obtained during the treatment period from mITT, excluding data after discontinuation of the study drug. Safety was assessed using the safety analysis set, which included data obtained during the treatment and safety follow-up periods from mITT, regardless of adherence to the study drug.
A mixed model for repeated measures (MMRM) model was used to analyse the effect of tirzepatide on SBP and DBP over time. For the MMRM, independent variables of the analysis model are treatment group, visit, treatment-by-visit interaction, pre-diabetes status at randomisation, sex and region (USA/outside the USA) as a fixed effect and baseline BP (SBP/DBP) as a covariate. For interaction p values within BP subgroups (baseline sex, age, hypertension category, use of antihypertensive medication, SBP cut-off of 120 mm Hg, 130 mm Hg and 140 mm Hg, or DBP cut-off of 80 mm Hg and 90 mm Hg), a full model including the covariates mentioned above with additional covariates such as subgroup-by-visit interaction, treatment-by-subgroup interaction and treatment-visit-subgroup interaction were included as fixed effects in the MMRM model. An unstructured covariance was used in the MMRM to model the relationship of within-participant errors, with a plan to evaluate other variance-covariance structures if the models failed to converge. Missing data were addressed by the MMRM model and no explicit imputation methods for missing data were employed.
Mediation analysis was used to assess what proportion of the estimated treatment difference (ETD) in BP with tirzepatide versus placebo was attributable to an indirect effect mediated by weight loss or to a direct effect. The model for estimation of weight loss-dependent and weight loss-independent effects on SBP and DBP at week 72 included interaction between treatment and weight change, with their baseline variables (SBP or DBP), sex, region and pre-diabetes status at randomisation as a covariate in the model, and effects were reported using 5000 bootstrap iterations to accommodate the uncertainty of the estimates.
Two-sided p values of <0.05 were considered statistically significant. All the analyses were done using SAS (V.9.4) and RStudio (V.2023.03.0).
Results
Participants
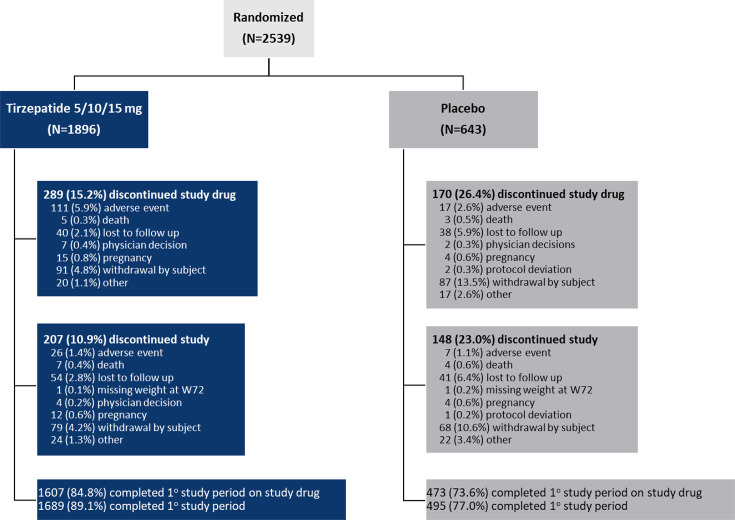
A total of 2539 participants from SURMOUNT-1 who had BP measurements at baseline and at least one postbaseline measurement were included in the analyses. Overall, 86% of participants completed the trial, with the participant disposition described in figure 1. Baseline clinical and demographic characteristics were similar across treatment groups (table 1). In 32.3% of participants, hypertension was reported at baseline as assessed through a review of medical history, and 29.9% of the participants used antihypertensive medications at baseline. The mean SBP and DBP were 123.3 mm Hg and 79.5 mm Hg at baseline, respectively.
Figure 1.
Flowchart of participants in the SURMOUNT-1 trial. Participant disposition from randomisation to primary endpoint. N (randomised population), all participants who were randomly assigned to a treatment group; W72, week 72.
Table 1.
Demographic and clinical characteristics of participants at baseline*
| Characteristic | Tirzepatide 5/10/15 mg (N=1896) |
Placebo (N=643) |
Overall (N=2539) |
| Age, years | 45.0±12.4 | 44.4±12.5 | 44.9±12.5 |
| Female sex, n (%) | 1278 (67.4) | 436 (67.8) | 1714 (67.5) |
| Race or ethnic group, n (%)† | |||
| American Indian or Alaska Native | 173 (9.1) | 58 (9.0) | 231 (9.1) |
| Asian | 205 (10.8) | 71 (11.0) | 276 (10.9) |
| Black or African American | 146 (7.7) | 55 (8.6) | 201 (7.9) |
| White | 1342 (70.8) | 450 (70.0) | 1792 (70.6) |
| Other | 30 (1.6) | 9 (1.4) | 39 (1.5) |
| Hispanic or Latino, n (%) | 904 (47.7) | 310 (48.2) | 1214 (47.8) |
| Duration of obesity, years | 14.5±10.9 | 14.0±10.7 | 14.4±10.8 |
| Body weight, kg | 104.8±22.4 | 104.8±21.4 | 104.8±22.1 |
| BMI, kg/m2 | 37.9±6.8 | 38.2±6.9 | 38.0±6.8 |
| BMI category, n (%) | |||
| <30 | 116 (6.1) | 24 (3.7) | 140 (5.5) |
| ≥30 to <35 | 649 (34.2) | 227 (35.3) | 876 (34.5) |
| ≥35 to <40 | 540 (28.5) | 180 (28.0) | 720 (28.4) |
| ≥40 | 591 (31.2) | 212 (33.0) | 803 (31.6) |
| Blood pressure, mm Hg | |||
| Systolic | 123.5±12.7 | 122.9±12.8 | 123.3±12.7 |
| Diastolic | 79.5±8.2 | 79.6±8.0 | 79.5±8.2 |
| Pulse, beats per minute | 72.2±9.7 | 72.9±9.3 | 72.4±9.6 |
| Lipid levels, mg/dL‡ | |||
| Total cholesterol | 188.4 (20.3) | 187.5 (20.6) | 188.2 (20.4) |
| HDL cholesterol | 47.6 (26.1) | 46.6 (27.0) | 47.3 (26.3) |
| LDL cholesterol | 110.1 (30.1) | 109.4 (30.7) | 109.9 (30.2) |
| Triglycerides | 127.5 (50.0) | 130.8 (49.2) | 128.3 (49.8) |
| eGFR, mL/min/1.73 m2¶ | 98.0±17.9 | 98.1±18.3 | 98.1±18.0 |
| Pre-diabetes, n (%) | 762 (40.2) | 270 (42.0) | 1032 (40.6) |
| Hypertension, n (%)§ | 620 (32.7) | 199 (30.9) | 819 (32.3) |
| Use of antihypertensive medication, n (%)§ | 578 (30.5) | 181 (28.1) | 759 (29.9) |
| Use of ACE inhibitors | 147 (7.8) | 57 (8.9) | 204 (8.0) |
| Use of ARBs | 289 (15.2) | 89 (13.8) | 378 (14.9) |
| Use of calcium channel blockers | 25 (1.3) | 4 (0.6) | 29 (1.1) |
| Use of diuretics | 39 (2.1) | 11 (1.7) | 50 (2.0) |
*Plus-minus values are mean±SD except where noted.
†Race or ethnic group was reported by participants.
‡Data are geometric mean (coefficient of variation, %).
§Assessed through a review of medical history.
¶eGFR denotes the estimated glomerular filtration rate calculated with the use of the serum creatinine-based Chronic Kidney Disease Epidemiology Collaboration equation.
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; BMI, body mass index; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; N, number of randomised patients; n, number.
Change in blood pressure
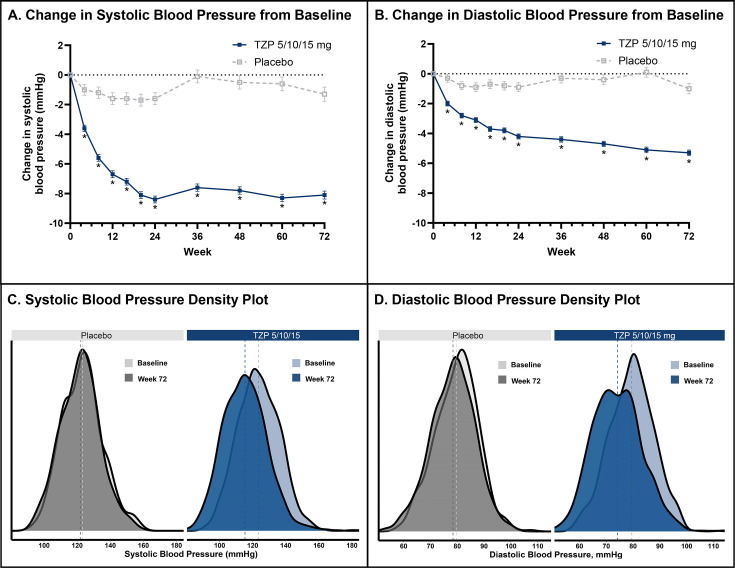
Tirzepatide treatment was associated with a rapid decline in SBP and DBP until about week 24. At week 24, all doses of tirzepatide had significantly greater SBP reductions than placebo (−7.8 for 5 mg, −8.3 for 10 mg and −8.5 for 15 mg vs −1.6 mm Hg, p<0.001 for all dose comparisons to placebo) and significantly greater DBP reductions than placebo (−4.4 for 5 mg, −4.0 for 10 mg and −3.9 for 15 mg vs −0.9 mm Hg, p<0.001 for all dose comparisons to placebo) from baseline. A plateau in the effect was observed, particularly for SBP. At week 72, all doses maintained the BP reductions observed at week 24, with change from baseline in SBP significantly greater than placebo (−7.0 for 5 mg, −8.2 for 10 mg and −7.6 for 15 mg vs −1.2 mm Hg, p<0.001 for all dose comparisons to placebo) and DBP significantly greater than placebo (−5.2 for 5 mg, −5.5 for 10 mg and −4.6 for 15 mg vs −1.0 mm Hg, p<0.001 for all dose comparisons to placebo). When doses were pooled, tirzepatide-treated participants had significantly greater SBP reductions than placebo (−8.1 mm Hg vs −1.3 mm Hg, ETD of −6.8 mm Hg (95% CI, −7.9 to −5.7), p<0.001) and significantly greater DBP reductions than placebo (−5.3 mm Hg vs −1.0 mm Hg, ETD of −4.2 mm Hg (95% CI, −5.0 to −3.5), p<0.001) from baseline to week 72 (figure 2A,B). Density plots demonstrate where the trial population BP readings are concentrated at baseline and week 72. SBP distribution shifted to the left in tirzepatide-treated participants at week 72, representing a decrease in mean SBP from 123.4 mm Hg to 115.3 mm Hg from baseline (figure 2C). The placebo group was relatively unchanged (122.8 mm Hg to 122.1 mm Hg). At week 72, DBP distribution also shifted to the left in tirzepatide-treated participants, representing a decrease in DBP from 79.5 mm Hg to 74.2 mm Hg from baseline (figure 2D). The placebo group was changed from 79.5 mm Hg to 78.5 mm Hg.
Figure 2.
Changes in blood pressure over 72 weeks: tirzepatide 5/10/15 mg compared with placebo. *p<0.001 tirzepatide vs placebo. Least-squares means are presented. Data were derived from a mixed model for repeated measures. (A) The change in systolic blood pressure from baseline to week 72. (B) The change in diastolic blood pressure from baseline to week 72. (C) The systolic blood pressure density plot at baseline and week 72 for placebo and tirzepatide treatment. (D) The diastolic blood pressure density plot at baseline and week 72 for placebo and tirzepatide treatment. TZP, tirzepatide 5/10/15 mg.
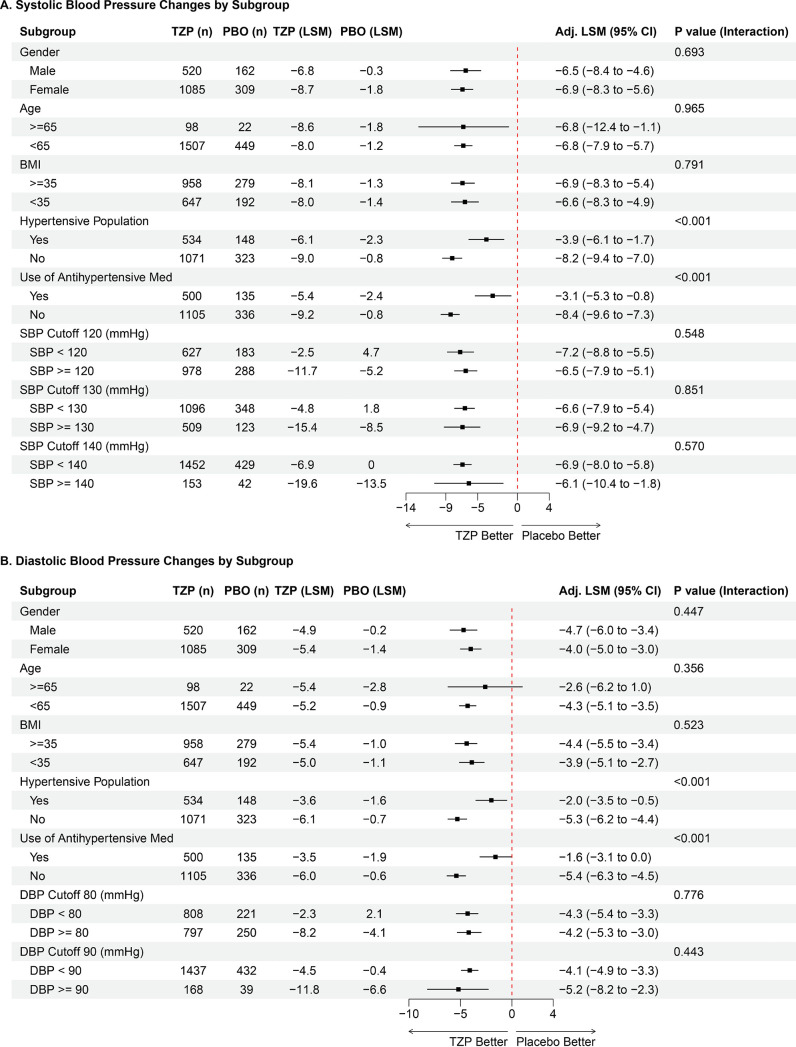
In subgroups defined by sex, age, baseline BMI and BP, there were consistent SBP and DBP reductions at 72 weeks with tirzepatide (figure 3A,B). However, SBP and DBP reductions with tirzepatide were significantly larger in participants without diagnosed hypertension or those not receiving antihypertensive medications (pinteraction<0.001 for each; figure 3A,B).
Figure 3.
Blood pressure changes from baseline to week 72 by subgroup. Data are blood pressure changes from baseline to week 72 for each subgroup represented as least square means change from baseline. Adjusted least square means represent the difference in change from baseline for tirzepatide compared with placebo. Panel A shows the SBP changes by subgroup. Panel B shows the diastolic blood pressure changes by subgroup. Adj, adjusted; BMI, body mass index; DBP, diastolic blood pressure; LSM, least square means; Med, medication; n, number of participants, PBO, placebo; SBP, systolic blood pressure; TZP, tirzepatide 5/10/15 mg.
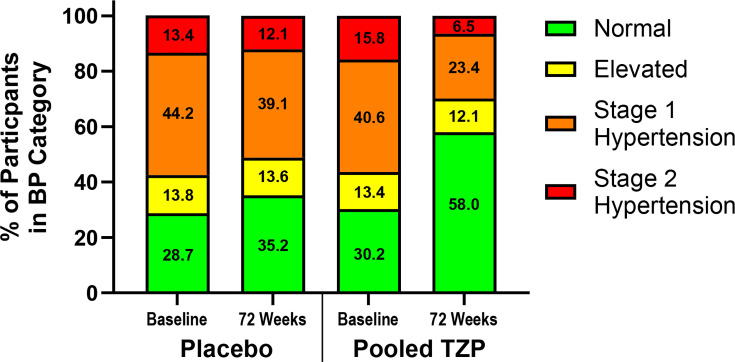
Blood pressure categories
At baseline, a similar proportion of tirzepatide and placebo participants had normal BP (30.2% and 28.7%, respectively), elevated BP and stage 1 and stage 2 hypertension (figure 4). At 72 weeks, more tirzepatide participants achieved normal BP than placebo participants (58.0% vs 35.2%, respectively) (figure 4). A greater reduction from baseline in the proportion of tirzepatide participants having stage 1 or stage 2 hypertension at week 72 was observed compared with placebo (figure 4).
Figure 4.
Percentage of participants by blood pressure categories at baseline and 72 weeks. The number inside the bar represents the percentage of participants in each category at baseline and week 72. TZP, tirzepatide 5/10/15 mg.
Association of changes in blood pressure and body weight
Tirzepatide led to greater per cent body weight reduction compared with placebo from baseline to week 72 (−15.0% to −20.9% across dosage ranges vs −3.1% with placebo).11 For the direct effect between tirzepatide and placebo at week 72, the ETD (95% CI) in the mean SBP change from baseline was −2.14 mm Hg (−3.5 mm Hg to –0.84 mm Hg) and the mean DBP change from baseline was −1.18 mm Hg (−2.12 mm Hg to –0.26 mm Hg). The estimated indirect effect between tirzepatide and placebo in the mean SBP was −4.47 (–5.32 to–3.58) and the mean DBP was −2.90 (–3.47 to –2.30). Weight loss was estimated to explain 67.6% of SBP reduction and 71.0% of DBP reduction. There was a significant but moderate correlation between the change in body weight and SBP (r=0.24, p<0.001) and DBP (r=0.24, p<0.001) in the tirzepatide group at week 72.
Safety
Mean pulse change from baseline was 0.6, 2.3 and 2.6 for tirzepatide 5 mg, 10 mg and 15 mg, respectively, and 0.1 for placebo.11 BP-related treatment-emergent adverse events (TEAEs) were reported by 6.8% of tirzepatide participants and 3.3% of placebo participants (table 2). The most frequently reported BP-related adverse event was dizziness, which occurred more frequently in tirzepatide-treated participants. Severe or serious TEAEs occurred among four participants (0.2%) in the pooled tirzepatide group and included hypotension (n=1), syncope (n=1), presyncope (n=1) and loss of consciousness (n=1). There were no participants with serious TEAEs in the placebo group. There were no reports of severe orthostatic hypotension in any group.
Table 2.
Blood pressure-related adverse events
| Variable | Tirzepatide 5/10/15 mg (N=1896) | Placebo (N=643) |
| Participants with ≥1 blood pressure-related adverse event during treatment period | 128 (6.8%) | 21 (3.3%) |
| Dizziness | 87 (4.6%) | 15 (2.3%) |
| Hypotension | 19 (1.0%) | 0 (0%) |
| Syncope | 9 (0.5%) | 5 (0.8%) |
| Orthostatic hypotension | 11 (0.6%) | 0 (0%) |
| Presyncope | 9 (0.5%) | 0 (0%) |
| Blood pressure decreased | 2 (0.1%) | 0 (0%) |
| Loss of consciousness | 1 (0.1%) | 1 (0.2%) |
Data are number of subjects with variable (%).
Discussion
In the SURMOUNT-1 trial, in addition to substantial body weight reduction, tirzepatide demonstrated robust and sustained BP lowering in people with overweight or obesity over 72 weeks of treatment. Tirzepatide lowered SBP and DBP over the first 24 weeks, followed by maintenance through 72 weeks. By the end of the study, tirzepatide led to a 6.8 mm Hg lower mean SBP than placebo and a 4.2 mm Hg lower DBP. BP reductions were similar with all investigated doses of tirzepatide and showed the same pattern over time. The effects were consistent across demographic and clinical subgroups, including various baseline SBP and DBP categories. However, BP reduction was greater in participants without hypertension or those not taking antihypertensive medications at baseline. Greater reductions in antihypertensive medications in some tirzepatide recipients may contribute to this observed interaction, but we cannot exclude other explanations. Tirzepatide was associated with a much greater proportion of participants with normal BP.
A high-level meta-analysis showed that semaglutide was associated with a 4.8 mm Hg reduction in SBP, but there were no details about the timing, safety, subgroups or hypertension categories.10 The primary SURMOUNT-1 publication reported office BP reduction with tirzepatide, but only limited analyses were performed.11 The ABPM sub-study further characterised the effects of tirzepatide on BP over 24 hours, as well as reported that SBP reductions were consistent across clinically relevant subgroups; however, the results were on a smaller patient cohort (n=600), and BP measurements were only measured at baseline and one other time point after 36 weeks of treatment.12 Importantly, the ABPM sub-study reported that tirzepatide treatment led to consistent SBP reductions for daytime and night-time BP, as nocturnal hypertension has been shown to increase the risk of organ damage.14 The results of the present post hoc analyses were consistent with the findings in both reports. Further, they examined the effects on both SBP and DBP in additional clinically relevant subgroups, the effect on hypertension categories, the pattern of change over 72 weeks of treatment, the association between weight reduction and BP and, importantly for care, details on the safety profile relevant to BP reductions. These findings are noteworthy because they further elucidate the effects of tirzepatide on BP and its potential role in preventing and controlling hypertension since the effect consistently reduced SBP and DBP in participants reporting hypertension or being treated with antihypertensive medications, as well as in those with SBP and/or DBP above the normal range at baseline.
The placebo-adjusted net reduction in SBP of 6.8 mm Hg and DBP of 4.2 mm Hg represents a clinically relevant change and is notable given mean BPs at baseline were within ‘normal’ range, as reduction of SBP has been shown to reduce the risk of major cardiovascular events regardless of baseline BP values.15 Also, we observed reductions in BP across a range of baseline BP values with similar placebo-corrected changes in SBP and DBP across BP cut-offs ranging from ≥140 mm Hg to ≥120 mm Hg for SPB and ≥90 mm Hg to ≥80 mm Hg for DBP (figure 3A,B). Tirzepatide was associated with a substantial beneficial influence on BP categories. At baseline, about 16% had stage 2 hypertension, 41% had stage 1 hypertension and about 30% had normal BP. By the end of the trial, most of those taking tirzepatide had normal BP, and only 7% had stage 2 hypertension, while there were only slight changes in such proportions in the placebo group (figure 4).
In a recently published meta-analysis, a 5 mm Hg reduction of SBP reduced the risk of major cardiovascular events by about 10%, irrespective of previous diagnoses of cardiovascular disease and irrespective of baseline BP values being normal or high-normal.15 While direct comparisons cannot be made, the observed overall effect in this analysis is on par with, or exceeds, the treatment effects of many antihypertensive medications and procedures.16 This highlights the potential of tirzepatide as a therapeutic tool for managing hypertension in people living with obesity.
The mediation analysis suggested that most of the BP reduction in the trial could be driven by weight loss. However, the correlation between a reduction in BP and weight loss was not strong. A possible explanation could be a difference in the magnitude of weight loss in relation to BP reduction and the timing of these reductions. Unlike weight loss, the effect on BP was similar across dosing regimens, which showed a more pronounced reduction with higher dosages. This dose–effect divergence between these outcomes may suggest a compensatory mechanism that regulates BP after an initial reduction. Further work is needed to better understand the mechanisms.
Importantly, these reductions were associated with only small increases in side effects attributable to low BP levels, even for participants whose baseline BP was in the normotensive category. This finding suggests that tirzepatide may be beneficial even for those at the lower end of the BP spectrum. Given emerging evidence of continuous relationships between SBP and long-term cardiovascular disease outcomes, even with SBP below the ‘normal range’, it is plausible that additional long-term cardiovascular disease benefits of incretin therapies may emerge among those with normal baseline BP.15 It is well established that GLP-1 receptor agonists increase heart rate modestly, yet they have shown cardiovascular benefits.17–20 The increase in heart rate in SURMOUNT-1 was comparable to selective GLP-1 receptor agonists used for chronic weight management.
Finally, the BP effects were more pronounced among those not on antihypertensive medications. The study did not collect robust information on medication changes, and BP medication dosage and number may have been reduced in response to declining BP with tirzepatide. The group not on antihypertensive medications thus may provide the clearest and least confounded indication of the effect of tirzepatide on BP, and notably in this group, mean reductions in SBP and DBP (−8.40 mm Hg and −5.40 mm Hg, respectively) were somewhat greater than the overall average (figure 3A,B).
The potential clinical implications of these findings are notable. The use of tirzepatide in people living with obesity was associated with substantial and sustained reductions in BP levels, which may reduce the risk of hypertension-related end-organ complications. Moreover, such effects could eliminate or meaningfully delay some individuals’ need for antihypertensive medications. Targeting hypertension by this method might also lower diabetes risks and improve lipids and quality of life, given the associated weight loss. The study also shows that the BP reductions with tirzepatide were associated with relatively few BP-related events and tended to flatten out after 6 months of treatment.
The study has several limitations. The trial tested a single incretin-based medication, and it is not possible to determine if these effects can be generalised, especially because tirzepatide, unlike selective GLP-1 receptor agonists approved for weight management, combines both GIP and GLP-1 receptor agonism. In addition, SURMOUNT-1 lacked robust information on medication changes, limiting our ability to investigate the effect of those medication changes on BP changes. In addition, this trial did not include many individuals with hypertension (32.3% had a history of hypertension reported at baseline) and excluded individuals with SBP≥160 mm Hg or DBP>100 mm Hg. Finally, the study was not designed to investigate the long-term cardiometabolic benefits of tirzepatide. The ongoing SURMOUNT-MMO (NCT05556512) and SURPASS-CVOT (NCT04255433) trials are designed to provide insights into the effects of tirzepatide on clinical outcomes.
In these post hoc analyses, tirzepatide was associated with a sustained and clinically relevant reduction in BP comparable to effects from standard antihypertensive medications. BP lowering was consistent across a range of baseline BP levels and most subgroups with a safety profile typical of incretin-based therapies approved for chronic weight management. Pharmacological treatment of obesity with tirzepatide holds promise as a potential strategy to help control or prevent hypertension and its complications in this population.
Footnotes
@hmkyale
Presented at: Presented in part at the 2023 American Heart Association meeting (11–13 November 2023).
Contributors: AS, NNA and MCB contributed to the study design, and AS provided medical oversight during the trial. PS was responsible for the statistical analyses. AS and BL are the guarantors of this work and, as such, take responsibility for the integrity of the data and the accuracy of the data analysis. All authors participated in the interpretation of the data and critical review of the manuscript, had full access to the data and approved this manuscript to be submitted for publication.
Funding: This study was sponsored by Eli Lilly and Company.
Competing interests: In the past 3 years, HMK received options for Element Science and Identifeye and payments from F-Prime for advisory roles. He is a co-founder of and holds equity in Hugo Health, Refactor Health, and ENSIGHT-AI. He is associated with research contracts through Yale University from Janssen, Kenvue, Novartis, and Pfizer. JAdL has received honoraria for participation in data safety monitoring committees from Eli Lilly and Company, Novo Nordisk, Amgen, Regeneron, AstraZeneca and Merck. NS has consulted for Abbott Laboratories, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Hanmi Pharmaceuticals, Janssen, MSD, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, Sanofi and received grant support paid to his university from AstraZeneca, Boehringer Ingelheim, Novartis, and Roche Diagnostics. BL, PS, CJM, NNA, MCB and AS are employees and shareholders of Eli Lilly and Company.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Lilly provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval was obtained from Comité de Ética en Investigacion Clinica (1587/56/2019), Comité de Ética Centro de Osteopatías Médicas (I8F-MC-GPHK), Comité de Ética en Investigación del Centro de Investigaciones Metabólicas (225), Comité de Ética en Investigación Instituto de Investigaciones Clínicas (I8F-MC-GPHK), Comite de Ética en Investigación del Instituto Clinico Metabolico (I8F-MC-GPHK), Comite de Ética en Investigación DIM Clinica Privada (0846820), Comitê de Ética em Pesquisa do Hospital Pró-Cardíaco - ESHO Empresa de Serviços Hospitalares (5.199.437), Comitê de Ética em Pesquisa do Instituto de Saúde e Bem estar da Mulher (ISBEM) (5.367.428), Comitê de Ética em Pesquisa da Faculdade de Medicina do ABC / Fundação do ABC (5.351.852), Comitê de Ética em Pesquisa do Instituto de Saúde e Bem estar da Mulher (ISBEM) (5.317.171), Comitê de Ética em Pesquisa Investiga - Institutos de Pesquisa (5.385.206), Comitê de Ética em Pesquisa do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo – HCFMUSP (5.336.771), Comitê de Ética em Pesquisa - CIAS - Unimed Vitória (5.414.781), Comitê de Ética em Pesquisa Investiga - Institutos de Pesquisa (5.358.073), Research Ethics Committee-The Fourth Hospital of Harbin Medical University (临伦审第(2020-001)号), Research Ethics Committee- West China Hospital of Sichuan University (2019年临床试验(西药)审(251)号), Research Ethics Committee-Beijing Tsinghua Changgung Hospital (20001-1-01), Research Ethics Committee-The First Affiliated Hospital of Xi'an Medical University (XYYFY2020LSYL-004), Research Ethics Committee- Jinan Central Hospital (伦理临审2020-023-02号), Research Ethics Committee- Ningbo First Hospital (2020-D003), Research Ethics Committee- The Second Affiliated Hospital of Nanjing Medical University ([2020]-YW-004-LP-01), Institutional Ethics Committee (ECR/94/Inst./AP/2013/RR-19), Institutional Ethics Committee (IEC/2020/SPO/02), ILS Hospital Ethics Committee (ECR/130/Inst/WB/2013/RR-19), Institutional Ethics Committee (CT_2020_Feb_VD_611), Institutional Ethics Committee (ECR/382/Inst/MH/2013/RR-19), Gastroplus Ethics Committee (Protocol Number: I8F-MC-GPHK), Japan Conference of Clinical Research IRB (3-337), Tokyo-Eki Center-Building Clinic IRB (688001-20191115), Medical Corporation Heishinkai OPHAC Hospital IRB (511CLI), Medicine, Medical Corporation Kyosokai AMC Shinjuku Clinic IRB (ll08002AC01), Comité de Ética en Investigación del Centro Especializado en Diabetes, Obesidad y Prevención de Enfermedades Cardiovasculares, SC (CONBIOETICA-09-CEI-026-20170929), Comité de Ética en Investigación Unidad Clínica de Bioequivalencia S. de R.L de C.V. (CONBIOETICA-14-CEI-002-20160718), Comité de Ética en Investigación “Hospital Universitario Dr Jose Eleuterio Gonzalez (I8F-MC-GPHK), Comité de Ética en Investigación del Instituto Mexicano de Trasplantes, SC (HIMT-INV-112-2022), Comité de Ética en Investigación Unidad de Investigación en Salud en Chihuahua, SC (CONBIOETICA-08-CEI-002-20170526), Comité de Ética en Investigación Río Mayo (MRM980313GD2), Comité de Ética en Investigación de Clínica Bajío CLINBA, SC (CONBIOETICA-11-CEI-003-20160708), Comité de Ética en Investigación del Hospital General de Culiacán Dr Bernardo J. Gastelum (CONBIOETICA-25-CEI-001-20160708), Comité de Ética en Investigación Accelerium S. R.L de C.V. (I8F-MC-GPHK), Research Ethics Committee – National Taiwan University Hospital (02-23123456-63998), Research Ethics Committee – China Medical University Hospital (CMUH108-REC2-155), Institutional Review Board – Chi Mei Medical Center (10902-008), Institutional Review Board – Chung Shan Medical University Hospital (I8F-MC-GPHK), Institutional Review Board – National Cheng Kung University Hospital (AB-CR-109-002) and Advara (Pro00039638).
References
- 1. GBD 2017 Risk Factor Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1923–94. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Magnussen C, Ojeda FM, Leong DP, et al. Global effect of modifiable risk factors on cardiovascular disease and mortality. N Engl J Med 2023;389:1273–85. 10.1056/NEJMoa2206916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–50. 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA 2020;324:1190–200. 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nambiar L, LeWinter MM, VanBuren PC, et al. Decade-long temporal trends in U.S. hypertension-related cardiovascular mortality. J Am Coll Cardiol 2020;75:2644–6. 10.1016/j.jacc.2020.03.009 [DOI] [PubMed] [Google Scholar]
- 6. Hall JE, do Carmo JM, da Silva AA, et al. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res 2015;116:991–1006. 10.1161/CIRCRESAHA.116.305697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schiavon CA, Bersch-Ferreira AC, Santucci EV, et al. Effects of bariatric surgery in obese patients with hypertension: the GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension). Circulation 2018;137:1132–42. 10.1161/CIRCULATIONAHA.117.032130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leslie WS, Ali E, Harris L, et al. Antihypertensive medication needs and blood pressure control with weight loss in the diabetes remission clinical trial (DiRECT). Diabetologia 2021;64:1927–38. 10.1007/s00125-021-05471-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall ME, Cohen JB, Ard JD, et al. Weight-loss strategies for prevention and treatment of hypertension: a scientific statement from the American Heart Association. Hypertension 2021;78:e38–50. 10.1161/HYP.0000000000000202 [DOI] [PubMed] [Google Scholar]
- 10. Kennedy C, Hayes P, Salama S, et al. The effect of semaglutide on blood pressure in patients without diabetes: a systematic review and meta-analysis. J Clin Med 2023;12:772. 10.3390/jcm12030772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med 2022;387:205–16. 10.1056/NEJMoa2206038 [DOI] [PubMed] [Google Scholar]
- 12. de Lemos JA, Linetzky B, le Roux CW, et al. Tirzepatide reduces 24-hour ambulatory blood pressure in adults with body mass index >/=27 kg/M(2): SURMOUNT-1 ambulatory blood pressure monitoring substudy. Hypertension 2024;81:e41–3. 10.1161/HYPERTENSIONAHA.123.22022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 2018;71:e13–115. 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 14. Costello HM, Gumz ML. Circadian rhythm, clock genes, and hypertension: recent advances in hypertension. Hypertension 2021;78:1185–96. 10.1161/HYPERTENSIONAHA.121.14519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rahimi K, Bidel Z, Nazarzadeh M. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021;397:1625–36. 10.1016/S0140-6736(21)00590-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Canoy D, Copland E, Nazarzadeh M, et al. Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials. Heart 2022;108:1281–9. 10.1136/heartjnl-2021-320171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet 2019;394:121–30. 10.1016/S0140-6736(19)31149-3 [DOI] [PubMed] [Google Scholar]
- 18. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–22. 10.1056/NEJMoa1603827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834–44. 10.1056/NEJMoa1607141 [DOI] [PubMed] [Google Scholar]
- 20. Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med 2023;389:2221–32. 10.1056/NEJMoa2307563 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
heartjnl-2024-324170supp001.pdf (1.8MB, pdf)
Data Availability Statement
Data are available upon reasonable request. Lilly provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.