ABSTRACT
Background
Disorders of the cervical spine are some of the costliest musculoskeletal conditions to manage globally. Joint mobilization and manipulation have been shown to be an effective treatment for neck pain. However, the generalizability and clinical translation depends on the nature of the trial designs that inform its use. The extent to which randomized control trials (RCTs) assessing manual therapy treatments for cervical spine disorders fall on the efficacy (explanatory) -effectiveness (pragmatic) spectrum often informs how the findings are translated into clinical practice.
Objective
The aim of this systematic review was to determine where RCTs of manual therapy for neck disorders fall on the efficacy-effectiveness spectrum.
Methods
A search of three electronic databases including PubMed, CINAHL, and CENTRAL were completed for trials published from inception to May 2023. RCTs in which joint mobilization or manipulation were used to treat cervical spine disorders were assessed on the effectiveness-efficacy spectrum using the Rating of Included Trials on the Efficacy-Effectiveness Spectrum (RITES) tool and risk of bias using the Revised Cochrane Risk of Bias tool.
Results
A total of 174 trials met eligibility. RITES domain two trial setting (71.3% vs 16.1%), domain three flexibility of intervention(s) (62.1% vs 23%), and domain four clinical relevance of experimental and comparison intervention(s) (51.7% vs 29.3%) all favored efficacy over effectiveness. Domain one participant characteristic(s) had a slightly greater emphasis on effectiveness compared to efficacy (36.8% vs 44.8%). Most studies (96%) had at least some risk of bias.
Conclusion
Over half of the RCTs assessing the treatment effect of joint mobilization and manipulation for neck pain favor efficacy (explanatory) over effectiveness (pragmatic) designs. Future RCTs on this topic should consider a greater emphasis on pragmatic trial design components in order to better reflect real-world translation to clinical practice.
KEYWORDS: Systematic review, neck pain, manual therapy, pragmatic design, RITES tool
Introduction
Neck pain is one of the most common and costly musculoskeletal disorders globally, alongside low back pain (LBP), resulting in one of the highest healthcare expenditures for musculoskeletal disorders in the United States [1–5]. Although no single intervention has been shown to be superior for neck pain, manual therapy including joint mobilization and manipulation has been shown to improve neck pain [6–12]. However, the applicability of manual therapy interventions used in clinical trials can vary based on overall study design, making it challenging to determine what will work best in routine clinical practice. This variability can create confusion and challenges when attempting to replicate manual therapy interventions in clinical settings. Many randomized controlled trials (RCTs) require specific inclusion/exclusion criteria, such as female-only patients with a narrow age range [13], and use treatment approaches that may appear less relevant for real-world care settings, such as a single session joint manipulation or mobilization [14], which could be considered a sub-clinical dose in many settings [15,16]. This defined criteria can create challenges with knowledge translation when attempting to generalize findings to a broader patient population [17,18].
Clinical trial designs vary in their goals to include explanatory (e.g. efficacy) and pragmatic (e.g. effectiveness) designs. Explanatory trials emphasizing efficacy aim to explore the benefits of an intervention under ideal and highly controlled situations [9–11]. For example, Vieira-Pellenz et al. [19] focused on the explanatory factors by comparing the short-term effects of lumbar manipulation to sham manipulation. The study included a homogenous male patient population, the intervention was performed by one clinician, it implemented a single session with an immediate follow-up assessment, and there was no flexibility in the intervention delivery [19]. Although this design typically minimizes threats to internal validity, the generalizability is not ideal. In contrast, an effectiveness approach would favor external validity [20–23]. The outcomes of these interventions are examined under circumstances that more closely approximate clinical practice, including less standardized treatment protocols applied to more heterogeneous patient populations, and by a larger number of clinicians more representative of routine clinical care [20,24]. In one study, Hoving et al. [25] compared the effectiveness of manual therapy, physical therapy, and continued care by the general practitioner for patients with mechanical neck pain. This study had a heterogeneous patient population, included a long term follow-up of one year, implemented individualized and flexible interventions that allowed for tailored clinical decision making, and used multiple treating clinicians [25]. The reality is that trials in general with these designs are not commonly published, reported to be less than 2% of total RCTs based on MEDLINE searches of title and abstracts in 2010 [23]. Most studies fall somewhere on the spectrum of effectiveness (pragmatic) versus efficacy (explanatory) due to the design of the study [21]. Study designs that are more pragmatic in nature may be more useful for clinicians in that they lend themselves to applicability in a real-world setting while also guiding clinical care and changing clinical practice [26]. Clinical trials often emphasize either internal or external validity in their design; however, many factors such as the patient population, the clinician’s background, the location of treatment, and the intervention strategy all may play a role in determining where on the efficacy-effectiveness spectrum the study design falls and how it can be generalized to clinical practice [9–14].
There is currently a limited understanding of where trial designs lie on the efficacy-effectiveness spectrum for any form of neck pain [21,27,28]. A recent scoping review investigated the reporting of manual therapy interventions in clinical trials for neck pain, but only assessed intervention delivery and not the overall level of efficacy or effectiveness of the study designs [29]. Another systematic review investigated the impact that pragmatic or explanatory interventions had on neck and LBP when comparing joint mobilization versus manipulation; however, this study again only examined the intervention component and did not assess study design aspects such as trial settings, expertise and background of clinicians, and participant characteristics [16]. A more recent systematic review assessed trial designs for manual therapy and LBP as it relates to efficacy and effectiveness [15], but is currently the only study assessing this for any musculoskeletal condition. Given the lack of assessment of pragmatism in trials for patients with neck pain and the relevance for clinical decision making, the primary objective of this systematic review was to assess manual therapy trials for neck pain using the Rating of Included Trials on the Efficacy-Effectiveness Spectrum (RITES) tool to determine where these trial designs fall on the efficacy-effectiveness spectrum. A secondary objective was to determine if patterns of trial design domains (efficacy vs effectiveness) were more likely to be associated with a treatment effect.
Methods
This systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [30] and registered a priori (PROSPERO registration number CRD42023425928).
Search strategy
A search strategy of three databases included PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and CENTRAL (Cochrane Central Register of Controlled Trials) for studies published from inception to May 2023. The search used All Map Terms to Subject Headings, Medical Subject Headings (MeSH) terms, keywords related to neck pain, joint mobilization/manipulation, and the search term including RCTs. Our search strategy included electronic searching of databases for RCTs for individuals who received joint mobilization or manipulation used to treat neck pain and cervical related disorders (e.g. cervicogenic dizziness, cervical radiculopathy, and cervicogenic headaches). The first search used MeSH terms and keywords related to the cervical spine and neck pain in PubMed. The second search used MeSH terms and keywords related to manipulation and mobilization, and the third search used a combination of MeSH terms and keywords for RCTs. The three main search strategies were combined with the Boolean operator AND and OR to identify specific studies relevant to our research question with details provided in Appendix A. Search strategies were modified and adapted based on the requirements of each specific database.
Study selection criteria
We defined manual therapy, for the purpose of this review, as joint mobilization or manipulation in order to control heterogeneity due to the broad range of approaches that can fall under the label of manual therapy [31]. Any RCT where joint mobilization or manipulation was used to treat cervical pain was included in the review. Joint mobilization was defined as a skilled manual therapy intervention applied to a joint at varying speeds and amplitudes using accessory motion in the spine for therapeutic purposes [32]. Joint manipulation was defined as a high-velocity, low-amplitude technique performed at the pathological limit of the joint [32]. Adjunct interventions (e.g. acupuncture, massage, soft tissue mobilization, instrument-assisted soft tissue, mechanically-assisted manipulation), exercise therapy, and other interventions such as modalities, education, or advice were included as long as joint mobilization and manipulation were used and assessing the treatment effect of manual therapy was the primary objective of the research. This also included any placebo or true control group as the comparison arm of the study.
Additionally, we included studies if they: (1) were written in English, and (2) studied adults aged 18+ . We excluded trials if: (1) they focused on non-musculoskeletal related disorders (e.g. migraines and tension-type headaches) in the absence of neck pain or on post-surgical care related to neck pain, (2) the study did not focus on assessing treatment effect for neck disorders, (3) they were not peer reviewed, (4) manual therapy was not the primary focus of the study, (5) there was not enough information in the study to determine inclusion, (6) the full-text was unavailable (e.g. not available in English, protocol or abstract only), (7) subjects were treated for disorders other than the neck, (8) the study was a secondary analysis from an original study, (9) if the sample also included non-adult participants or, (10) the manual therapy assessed did not specifically include joint mobilization/manipulation.
Data management
Covidence software (Veritas Health Innovation Ltg, Melbourne, Australia) was used for all data management [33]. Title, abstracts, and full-texts were uploaded to Covidence where duplicates were removed. Two independent reviewers (KC, MS) performed the title and abstract screening in Covidence to determine eligibility for full-text reviews. Following title and abstract screening, the same two reviewers individually screened the full-text of the included studies for final eligibility. All discrepancies were reconciled by the two reviewers.
Data extraction
Details of the studies including title, year of publication, country of origin, primary author, total sample size, sample size per treatment group, and patient demographics with mean (standard deviation) or proportion were collected within Covidence from each included study. Definitions of manual therapy as defined within the trial, types of neck pain/disorders, and the follow-up time points of the trial were also collected. Information needed for the assessment of the RITES tool and risk of bias was also extracted for each included trial.
Assessment of trial design efficacy-effectiveness spectrum
The RITES tool was used to assess where each trial fell on the efficacy-effectiveness spectrum. This tool is currently underused in assessing the spectrum of trials investigating manual therapy for musculoskeletal conditions [13]. The RITES tool was developed based on categories within the Pragmatic Explanatory Continuum Indicator Summary (PRECIS) tool [34], used to help design trials, and is scored on a 5-point Likert scale within four domains that include participant characteristics, trial setting, flexibility of interventions, and clinical relevance of experimental and comparison interventions [21]. Scoring is completed as one to two being more explanatory, three showing a balance between explanatory and pragmatic, four to five being more pragmatic, and not applicable (N/A) where information was not available [21]. The RITES tool is used to determine the level of efficacy and effectiveness in each study, which was the primary objective of the review [15]. In-depth descriptors for efficacy and effectiveness adapted from Wieland et al. [21] and Maddox et al. [15] are provided in Table 1.
Table 1.
Ratings of included trials on the efficacy-effectiveness spectrum tool domains and descriptors.
|
Emphasis on Efficacy |
Emphasis on Effectiveness |
|
|
Domain |
Description |
Description |
| Participant characteristics | Participants different than those seen in usual care Restrictive inclusion and exclusion criteria Recruitment process different than what is seen in usual care Homogenous patient population |
Similar patients to those likely to receive intervention in usual care Heterogeneous patient population Recruitment consistent with usual care Diverse with parameters that reflect adherence |
| Trial setting | Single center Specialized/academic setting Additional training or certifications Only one individual providing intervention |
Multiple settings Conducted within clinical settings Variety of experience and certifications More than one individual providing intervention |
| Flexibility of intervention(s) | Less flexible with a strict protocol Other co-interventions discouraged |
Interventions performed based on examination findings Minimal-to-no controls over other interventions Advice and education provided with intervention |
| Clinical relevance of experimental and comparison intervention(s) |
Interventions not typical of usual care Immediate follow-up designs Contains a placebo/control group Ineffective interventions performed |
Intervention considered best practice Study duration and follow-up typical of usual care Treatment groups optimal for each group |
Based on a 5-point Likert scale, each domain rated as follows: 1 = strong emphasis on efficacy, 2 = rather strong emphasis on efficacy, 3 = balanced emphasis on both efficacy and effectiveness, 4 = rather strong emphasis on effectiveness, 5 = strong emphasis on effectiveness, or N/A = information not available. Table adapted from Wieland et al. [21] and Maddox et al. [15]
Risk of bias
Risk of bias for each trial was analyzed by two reviewers (KC, MS) using the Cochrane Collaboration of Risk-of-Bias Tool for Randomized Trials (RoB 2) [35]. The RoB 2 tool assesses bias in five domains including randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [35]. A score of low, high, or some concerns was assigned for each domain [36].
Data synthesis and analysis
To ensure consistency in the data extraction process, the two independent reviewers (KC, MS) planned to extract data independently for iterations of 20 studies until a minimum agreement of 80% was reached. The level of agreement was initially 84.4% within the first 20 studies for data items extracted. An additional nine studies were reviewed for additional consistency with data extraction, RITES scores, and risk of bias scores. The remaining studies were divided, and data was then extracted independently by the two reviewers. After the four domains of the RITES tool were scored for each trial, results were reported descriptively by domain. For each RITES domain, the proportion of all trials that focused more on efficacy (explanatory) compared to effectiveness (pragmatic) was determined, as well as those that were balanced between efficacy and effectiveness.
Each reviewer completed the RoB 2 for all studies individually where a consensus was made on each item afterward. After RoB judgments were determined for each trial, count and percentage data were calculated based on the number of trials having low, high, or some concerns for risk of bias.
A logistic regression was used to model the relationship between each of the four efficacy-effectiveness spectrum domains in RITES score (one through five) and the study treatment effect (positive versus null trial). For the model, a score of one or two was considered a study with higher efficacy, a score of three was a neutral study, and a score of four or five was a study with higher effectiveness. Each of the four domains was assessed in a separate model. All statistical analyses were performed using IBM SPSS Statistics (Version 28; Chicago, IL) [37].
Results
The initial search identified 4063 studies. A total of 1266 duplicates were removed resulting in 2797 studies for title and abstract screening. After title and abstract screening, 2412 studies were excluded followed by another 211 after full-text review resulting in a final total of 174 [7,8,13,14,25,38–206]. Figure 1 provides reasons for exclusion during full-text screening. There was moderate agreement between reviewers for title and abstract screening (k = .52) and substantial agreement for full-text review (k = .66).
Figure 1.

Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram.
A total of 117 (67.2%) studies in this review investigated nonspecific neck pain. Additionally, we identified 15 (8.6%) studies specific to cervical radiculopathy, 19 (10.9%) to cervicogenic headaches, 8 (4.6%) to cervicogenic dizziness with neck pain, 4 (2.3%) to whiplash associated disorder, and 11 (6.6%) as other including neck strain, cervical osteoarthritis/spondylosis, etc. Spain (20.1%, n = 35), United States (16.7%, n = 29), and Australia (7.5%, n = 13) were the top three countries publishing manual therapy trials for neck pain. Regarding follow-up within each trial, 20.7% (n = 36) of trials assessed outcomes immediately post treatment, 30.9% (n = 54) assessed them within one month, 20.7% (n = 36) assessed them after one month and up to three months, 8.6% (n = 15) assessed them from three to six months, and 11.6% (n = 20) assessed them beyond six months. A total of 7.5% (n = 13) of trials did not specify length of follow-up.
RITES scores
A significant proportion of studies had an emphasis on efficacy (scores of one or two) over effectiveness (scores of four or five) for the four domains of the RITES tool (Figure 2). Participant characteristics (RITES domain one) was the only domain with a slightly greater emphasis on effectiveness compared to efficacy. Individual RITES scores can be found in Figure 4.
Figure 2.
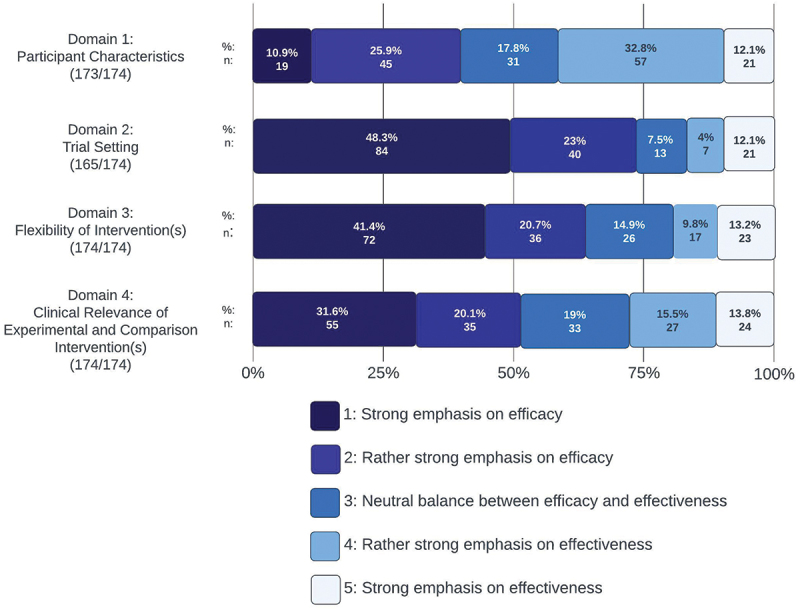
RITES scoring of included trails (by percentage and count). Abbreviation: RITES, ratings of included trials on the efficacy-effectiveness spectrum.
Figure 4.

RITES scores for trails included in systematic review.
Participant characteristics (RITES domain one)
For this domain, we identified 19 trials (10.9%) with strong efficacy, 45 (25.9%) with rather strong efficacy, 31 (17.8%) were balanced between the two, 57 (32.8%) with rather strong effectiveness, and 21 (12.1%) with a strong emphasis on effectiveness. A total of 64 (36.8%) trials had strong or rather strong emphasis on efficacy, whereas 78 (44.8%) had strong or rather strong emphasis on effectiveness. One study (0.6%) out of the 174 was judged as N/A as there was not enough information within the study to make a determination about this domain.
Trial setting (RITES domain two)
For this domain, we identified 84 trials (48.3%) with strong efficacy, 40 (23%) with rather strong efficacy, 13 (7.5%) were balanced between efficacy and effectiveness, 7 (4%) with rather strong effectiveness, and 21 (12.1%) with an emphasis on strong effectiveness. A total of 124 (71.3%) had strong or rather strong emphasis on efficacy, whereas 28 (16.1%) had strong or rather strong emphasis on effectiveness. Nine studies (5.2%) out of the 174 were judged as N/A as there was not enough information within the study to make a determination about this domain.
Flexibility of interventions (RITES domain three)
We identified 72 trials (41.4%) with strong efficacy, 36 (20.7%) with rather strong efficacy, 26 (14.9%) were balanced, 17 (9.8%) with rather strong effectiveness, and 23 (13.2%) with strong effectiveness. A total of 108 (62.1%) had strong or rather strong emphasis on efficacy, whereas 40 (23%) had strong or rather strong emphasis on effectiveness. No studies in this domain were judged as N/A.
Clinical relevance of experimental and comparison intervention(s) (RITES domain four)
For this domain, we identified a total of 55 (31.6%) trials with strong efficacy, 35 (20.1%) with rather strong efficacy, 33 (19%) were balanced, 27 (15.5%) with rather strong effectiveness, and 24 (13.8%) with strong effectiveness. A total of 90 (51.7%) had strong or rather strong emphasis on efficacy, whereas 51 (29.3%) had strong or rather strong emphasis on effectiveness. No studies in this domain were judged as N/A.
Assessment of RITES scores on outcomes of trial
Most RITES trial domains that favored effectiveness were more likely to be null trials, for trial setting (OR = 0.38, 95% CI 0.17–0.88; p = .02), flexibility of interventions (OR = 0.36, 95% CI 0.17–0.77; p = .01), and clinical relevance of experimental and comparison interventions (OR = 0.39, 95% CI 0.18–0.78; p = .01). The only domain where there was no significant difference in trial outcome was the domain of participants (OR = 1.46, 95% CI 0.74–2.89; p = .28).
Risk of bias (RoB 2)
The majority of trials had at least some risk or high risk of bias (Figure 3). The most common reasons were concerns identified with the patient using patient-reported outcomes (e.g. Neck Disability Index) as the primary outcome, handling of missing data, and not registering the trial a priori. A total of 136 (78.2%) trials were judged as having some concerns of bias, 31 (17.8%) demonstrated an overall high risk of bias, and only 7 (4%) demonstrated a low risk of bias. See Appendix B for individual risk of bias scores for each trial. All risk of bias figures and appendixes were created using an online risk of bias visualization tool called ROBVIS [207].
Figure 3.

Aggregate risk of bias summary across all studies in this review.
Discussion
This review, to our knowledge, is the first to specifically evaluate the designs of clinical trials assessing manual therapy treatment for neck pain on the efficacy-effectiveness spectrum. Three out of the four RITES domains favored efficacy over effectiveness for the RCTs included within this review. Within the domain of participant characteristics, clinical trials marginally favored effectiveness over efficacy, while the remaining three domains, including trial setting, flexibility of intervention(s), and clinical relevance of experimental and comparison intervention(s), favored efficacy, consistent with our hypothesis that the majority of RCTs would have less pragmatic designs. These findings are consistent with studies assessing this same question in trials for low back pain [15].
For the trial setting domain, some examples of explanatory characteristics included the RCT being conducted within university settings, having only one treatment provider or using specialized provider(s) with advanced post-professional training, and including only one clinical setting. In one study, a fully registered trained osteopathic practitioner with ten years of clinical and academic experience provided the treatment conducted within a university setting [173]. Common reasons trials were explanatory in the domain of flexibility of intervention(s) include examples of strict criteria of intervention(s) set forth within the methods (e.g. performing three sets of one-minute lateral glide), no ability to modify location or intervention(s) based on patient findings, and participants being prohibited on other co-interventions such as medication and exercise. Saavedra-Hernandez et al. [169] used an intervention group where a mid-cervical spine manipulation technique was directed at C3 in supine and a C7-T1 manipulation technique was performed in prone for each patient regardless of presentation. For the domain of clinical relevance of experimental and comparison intervention(s), the most common examples of how RCTs favored explanatory designs were due to not performing a clinically relevant or current best practice treatment and the study duration being shorter than the minimum length of treatment in usual care (e.g. immediate follow-up, one treatment session). For example, Yung et al. [195] had a short-term follow-up of two days following intervention using only non-thrust mobilizations without other adjunct treatment or education provided.
The discussion of efficacy (explanatory) and effectiveness (pragmatic) designs in clinical trials is not a new topic, with literature dating as far back as the late 1960s [208]. Maddox et al. [15] was the first to assess the effectiveness versus efficacy nature of studies for joint mobilization and manipulation in the treatment of generalized LBP, finding over half the trial designs favoring efficacy consistent with this study’s findings. We included trials of different health professionals beyond physical therapists treating neck pain with manual therapy for greater generalizability as we hypothesized a lower number of studies of neck trials compared to LBP [15]. No other studies have assessed the efficacy-effectiveness spectrum of manual therapy trials for other body regions beyond the lumbar spine.
Our findings suggest more manual therapy trial designs with effectiveness (pragmatic) approaches are needed to to better assist with knowledge translation into real-world clinical settings. However, development of trial designs with this in mind can be challenging. One way to assist with development of pragmatic trials prospectively is the Pragmatic-Explanatory Continuum Indicator Summary (PRECIS-2) tool. This tool can assist researchers in prospectively designing RCTs with a pragmatic emphasis [34]. The PRECIS-2 tool contains nine domains to consider when designing a specific study including eligibility, recruitment, setting, organization, delivery and adherence to interventions, follow-up, primary analysis, and primary outcome [21,34]. Using these nine domains, researchers can be more explicit with their trial design development to best fit their primary outcome focusing on a effectiveness (pragmatic) approach [34].
We found that if a trial design had a greater focus on effectiveness in the RITES domains of trial setting, flexibility of intervention(s), or clinical relevance of experimental and comparison intervention(s), it had decreased odds of showing a treatment effect. However, we recommend caution when interpreting these findings. Many of the studies within this systematic review had great variability in what was included in each comparison group. Comparison groups for studies considered to favor effectiveness often included manipulation and/or mobilization for treatment of neck pain, as well as other clinically relevant treatment interventions. For example, Karas et al. [108] compared flexion-biased versus extension-biased thoracic manipulation with pragmatic exercise prescription by each PT finding no differences between groups. Further research is necessary before any definitive conclusions are made.
There are some limitations in this review. Several common cervical disorders were poorly represented (e.g. whiplash associated disorder, cervicogenic dizziness, and cervical radiculopathy), which was due to few trials assessing the effect of manual therapy for these conditions. Second, while limiting the manual therapy interventions to only joint mobilization and manipulation techniques, some techniques that may not traditionally be known in some settings as joint mobilization and manipulation, including Chuna manual therapy, bone setting, Mulligan mobilization, instrument-assisted manual manipulation (e.g. Activator), and naprapathic manual therapy, were included. These treatment interventions all met the criteria established to define manual therapy techniques as those consisting of joint mobilization and manipulation [31,32]. Lastly, no meta-analysis was conducted as that was not the intent of this review, and therefore treatment effects of manual therapy for neck pain could not be determined.
Conclusion
Over half (55.5%) of the clinical trials assessing joint mobilization and manipulation for neck pain favored efficacy (explanatory) over effectiveness (pragmatic) trial designs. Trials designed to have a greater focus on effectiveness (pragmatic) were less likely to find a treatment effect. Additional trials are needed with a greater focus on effectiveness designs to better facilitate generalizability and knowledge translation. Researchers should also considers including the use of multiple centers to conduct trials, implementation beyond university settings, using a variety of treating clinicians with various experience and specialties, properly explaining the influence of sample heterogeneity on the conclusions that can be made when presenting results of the trial, not restricting groups from other real world co-treatments they may be receiving, allowing clinicians to deliver interventions similar to how they would be delivered in real world settings, and extending time of follow-up beyond the immediate or short-term. Although we found that three of four domains that favored effectiveness over efficacy had decreased odds of showing a treatment effect, the results should be interpreted cautiously. Trials are designed to ask unique questions. The nature of those questions could be explored in more depth when designing trials, with tools like the PRECIS-2 checklist [34], based on the desired intent and impact of the study question.
Supplementary Material
Acknowledgements
The authorship team would like to thank Cindy Reinl, Bellin Health Systems Librarian, Bellin College, Green Bay, WI, USA for her work with developing the electronic search strategy for this review.
Biographies
Kyle Cottone PT, DPT, OCS, FAAOMPT is an assistant professor and core faculty in the Bradley University DPT program in Peoria, IL. He is a Board-Certified Orthopaedic Clinical Specialist through the American Physical Therapy Association and Fellow of the American Academy of Orthopaedic Manual Physical Therapy.
Matthew Schumacher PT, DPT, OCS, FAAOMPT is an assistant professor and core faculty in the University of Mary Physical Therapy program in Bismarck, ND. He is a Board-Certified Orthopaedic Clinical Specialist through the American Physical Therapy Association and Fellow of the American Academy of Orthopaedic Manual Physical Therapy.
Jodi Young is the Director of Research in the Bellin College DSc in Physical Therapy Program. She is a Fellow of the American Academy of Orthopaedic Manual Physical Therapy. She completed her PhD through the University of Newcastle in Australia researching physical therapy dosing in patients with lower extremity injuries.
Dan Rhon is a clinician and active health services researcher. He has a Masters and Doctor of Science in Physical Therapy from Baylor University, a Doctorate of Physical Therapy from Temple University and a PhD from the University of Newcastle. He completed a clinical fellowship at Brooke Army Medical Center (Orthopaedic Manual Physical Therapy) and a postdoctoral research fellowship at the University of Utah.
Funding Statement
The authors report there is no funding associated with the work featured in the article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions statement
KC and MS all developed the final study protocol, designed, and analyzed the data, and wrote the initial draft of the manuscript. DR and JY conceived the study idea, assisted with interpretation of results, provided feedback for drafts of the manuscript, and helped supervise the project process. All authors approved of the final version.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10669817.2024.2327127
References
- [1].Fejer R, Kyvik KO, Hartvigsen J.. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. doi: 10.1007/s00586-004-0864-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vingård E. Chapter 5.6: Major public health problems — musculoskeletal disorders. Scand J Public Health Suppl. 2006;67:104–112. doi: 10.1080/14034950600677113 [DOI] [PubMed] [Google Scholar]
- [3].Kazeminasab S, Nejadghaderi SA, Amiri P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. doi: 10.1186/s12891-021-04957-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323(9):863–884. doi: 10.1001/jama.2020.0734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cloward RB. Cervical diskography. A contribution to the etiology and mechanism of neck, shoulder and arm pain. Ann Surg. 1959;150(6):1052–1064. doi: 10.1097/00000658-195912000-00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1–A83. doi: 10.2519/jospt.2017.0302 [DOI] [PubMed] [Google Scholar]
- [7].Walker MJ, Boyles RE, Young BA, et al. The effectiveness of manual physical therapy and exercise for mechanical neck pain: a randomized clinical trial. Spine. 2008;33(22):2371–2378. doi: 10.1097/BRS.0b013e318183391e [DOI] [PubMed] [Google Scholar]
- [8].Bronfort G, Evans R, Anderson AV, et al. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Ann Intern Med. 2012;156(1 Pt 1):1–10. doi: 10.7326/0003-4819-156-1-201201030-00002 [DOI] [PubMed] [Google Scholar]
- [9].Puentedura EJ, Cleland JA, Landers MR, et al. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. J Orthop Sports Phys Ther. 2012;42(7):577–592. doi: 10.2519/jospt.2012.4243 [DOI] [PubMed] [Google Scholar]
- [10].Hidalgo B, Hall T, Bossert J, et al. The efficacy of manual therapy and exercise for treating non-specific neck pain: a systematic review. J Back Musculoskelet Rehabil. 2017;30(6):1149–1169. doi: 10.3233/BMR-169615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hoving JL, Koes BW, de Vet HCW, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136(10):713–722. doi: 10.7326/0003-4819-136-10-200205210-00006 [DOI] [PubMed] [Google Scholar]
- [12].Boyles R, Toy P, Mellon JJ, et al. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19(3):135–142. doi: 10.1179/2042618611Y.0000000011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mansilla-Ferragut P, Fernández-de-Las PeñPeñAs C, Alburquerque-Sendín F, et al. Immediate effects of atlanto-occipital joint manipulation on active mouth opening and pressure pain sensitivity in women with mechanical neck pain. J Manip Physiol Ther. 2009;32(2):101–106. doi: 10.1016/j.jmpt.2008.12.003 [DOI] [PubMed] [Google Scholar]
- [14].Arias-Álvarez G, Bustos MM, Hidalgo-García C, et al. Are there differences between a real C0-C1 mobilization and a sham technique in function and pressure pain threshold in patients with chronic neck pain and upper cervical restriction? a randomised controlled clinical trial. J Back Musculoskelet Rehabil. 2023;36(1):61–70. doi: 10.3233/BMR-220008 [DOI] [PubMed] [Google Scholar]
- [15].Maddox CD, Subialka JA, Young JL, et al. Over half of clinical trials of mobilization and manipulation for patients with low back pain may have limited real-world applicability: a systematic review of 132 clinical trials. J Orthop Sports Phys Ther. 2022;52(8):532–545. doi: 10.2519/jospt.2022.10962 [DOI] [PubMed] [Google Scholar]
- [16].Roenz D, Broccolo J, Brust S, et al. The impact of pragmatic vs. prescriptive study designs on the outcomes of low back and neck pain when using mobilization or manipulation techniques: a systematic review and meta-analysis. J Man Manip Ther. 2018;26(3):123–135. doi: 10.1080/10669817.2017.1398923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].MacDermid JC, Graham ID. Knowledge translation: putting the “practice” in evidence-based practice. Hand Clin. 2009;25(1):125–143. viii. doi: 10.1016/j.hcl.2008.10.003. [DOI] [PubMed] [Google Scholar]
- [18].Zidarov D, Thomas A, Poissant L. Knowledge translation in physical therapy: from theory to practice. Disabil Rehabil. 2013;35(18):1571–1577. doi: 10.3109/09638288.2012.748841 [DOI] [PubMed] [Google Scholar]
- [19].Vieira-Pellenz F, Oliva-Pascual-Vaca A, Rodriguez-Blanco C, et al. Short-term effect of spinal manipulation on pain perception, spinal mobility, and full height recovery in male subjects with degenerative disk disease: a randomized controlled trial. Arch Phys Med Rehabil. 2014;95(9):1613–1619. doi: 10.1016/j.apmr.2014.05.002 [DOI] [PubMed] [Google Scholar]
- [20].Cleland JA, Noteboom JT, Whitman JM, et al. A primer on selected aspects of evidence-based practice relating to questions of treatment. part 1: asking questions, finding evidence, and determining validity. J Orthop Sports Phys Ther. 2008;38(8):476–484. doi: 10.2519/jospt.2008.2722 [DOI] [PubMed] [Google Scholar]
- [21].Wieland LS, Berman BM, Altman DG, et al. Rating of included trials on the efficacy-effectiveness spectrum: development of a new tool for systematic reviews. J Clin Epidemiol. 2017;84:95–104. doi: 10.1016/j.jclinepi.2017.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Delitto A. Pragmatic clinical trials: implementation opportunity, or just another fad? Phys Ther. 2016;96(2):137–138. doi: 10.2522/ptj.2016.96.2.137 [DOI] [PubMed] [Google Scholar]
- [23].Chalkidou K, Tunis S, Whicher D, et al. The role for pragmatic randomized controlled trials (pRcts) in comparative effectiveness research. Clin Trials. 2012;9(4):436–446. doi: 10.1177/1740774512450097 [DOI] [PubMed] [Google Scholar]
- [24].Noteboom JT, Allison SC, Cleland JA, et al. A primer on selected aspects of evidence-based practice to questions of treatment. part 2: interpreting results, application to clinical practice, and self-evaluation. J Orthop Sports Phys Ther. 2008;38(8):485–501. doi: 10.2519/jospt.2008.2725 [DOI] [PubMed] [Google Scholar]
- [25].Hoving JL, de Vet HCW, Koes BW, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long-term results from a pragmatic randomized clinical trial. Clin J Pain. 2006;22(4):370–377. doi: 10.1097/01.ajp.0000180185.79382.3f [DOI] [PubMed] [Google Scholar]
- [26].Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials. 2009;10(1):37. doi: 10.1186/1745-6215-10-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Dal-Ré R, Janiaud P, Ioannidis JPA. Real-world evidence: how pragmatic are randomized controlled trials labeled as pragmatic? BMC Med. 2018;16(1):49. doi: 10.1186/s12916-018-1038-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Taljaard M, McDonald S, Nicholls SG, et al. A search filter to identify pragmatic trials in medline was highly specific but lacked sensitivity. J Clin Epidemiol. 2020;124:75–84. doi: 10.1016/j.jclinepi.2020.05.003 [DOI] [PubMed] [Google Scholar]
- [29].Leech JB, Owen WE, Young JL, et al. Incomplete reporting of manual therapy interventions and a lack of clinician and setting diversity in clinical trials for neck pain limits replication and real-world translation. A scoping review. J Man Manip Ther. 2022 Sep 1; 1–10. doi: 10.1080/10669817.2022.2113295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wenger LE, Barrett DR, Rhon DI, et al. Evaluating and characterizing the scope of care for interventions labeled as manual therapy in low back pain trials: a scoping review. Phys Ther. 2023 Dec 29; doi: 10.1093/ptj/pzad178 [DOI] [PubMed] [Google Scholar]
- [32].Kisner C, Allen Colby L, Borstad J. Therapeutic exercise: foundations and techniques. Philadelphia, PA: F.A. Davis Company; 2017. [Google Scholar]
- [33].Babineau J. Product review: covidence (systematic review software). J Can Health Libr Assoc. 2014;35(2):68. doi: 10.5596/c14-016 [DOI] [Google Scholar]
- [34].Loudon K, Treweek S, Sullivan F, et al. The precis-2 tool: designing trials that are fit for purpose. BMJ. 2015;350(may08 1):h2147. doi: 10.1136/bmj.h2147 [DOI] [PubMed] [Google Scholar]
- [35].Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; oct18 2343:d5928–d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- [37].Masuadi E, Mohamud M, Almutairi M, et al. Trends in the usage of statistical software and their associated study designs in health sciences research: a bibliometric analysis. Cureus. 2021;13(1):e12639. doi: 10.7759/cureus.12639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Abd El-Azeim A, Grase M. Efficacy of Mulligan on electromyography activation of cervical muscles in mechanical neck pain: randomized experimental trial. Physiother Q. 2023;31(4):7–14. doi: 10.5114/pq.2023.117224. [DOI] [Google Scholar]
- [39].Afzal R, Ghous M, Shakil Ur Rehman S, et al. Comparison between manual traction, manual opening technique and combination in patients with cervical radiculopathy: randomized control trial. J Pak Med Assoc. 2019;69(9):1237–1241. https://www.ncbi.nlm.nih.gov/pubmed/31511705 [PubMed] [Google Scholar]
- [40].Akgüller T, Coşkun R, Analay Akbaba Y. Comparison of the effects of cervical thrust manipulation and exercise in mechanical neck pain: a randomized controlled trial. Physiother Theory Pract. 2023; Jan 131–15. doi: 10.1080/09593985.2022.2164475. [DOI] [PubMed] [Google Scholar]
- [41].Akhter S, Khan M, Ali SS, et al. Role of manual therapy with exercise regime versus exercise regime alone in the management of non-specific chronic neck pain. Pak J Pharm Sci. 2014;27(6):2125–2128. https://www.ncbi.nlm.nih.gov/pubmed/25410083 [PubMed] [Google Scholar]
- [42].Alansari SM, Youssef EF, Shanb AA. Efficacy of manual therapy on psychological status and pain in patients with neck pain. A randomized clinical trial. Saudi Med J. 2021;42(1):82–90. doi: 10.15537/smj.2021.1.25589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Allison GT, Nagy BM, Hall T. A randomized clinical trial of manual therapy for cervico-brachial pain syndrome - a pilot study. Man Ther. 2002;7(2):95–102. doi: 10.1054/math.2002.0453 [DOI] [PubMed] [Google Scholar]
- [44].Alshami AM, Bamhair DA. Effect of manual therapy with exercise in patients with chronic cervical radiculopathy: a randomized clinical trial. Trials. 2021;22(1):716. doi: 10.1186/s13063-021-05690-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Aquino RL, Caires PM, Furtado FC, et al. Applying joint mobilization at different cervical vertebral levels does not influence immediate pain reduction in patients with chronic neck pain: a randomized clinical trial. J Man Manip Ther. 2009;17(2):95–100. doi: 10.1179/106698109790824686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Argali Deniz M, Köse E, Ercan M, et al. Comparison of physical therapy and mulligan mobilization technique in the treatment of cervicogenic headache. Türk Fizyoterapi ve Rehabilitasyon Dergisi. 2022;33(2):13–22. doi: 10.21653/tjpr.764779 [DOI] [Google Scholar]
- [47].Arsh A, Darain H, Iqbal M, et al. Effectiveness of manual therapy to the cervical spine with and without manual therapy to the upper thoracic spine in the management of non-specific neck pain; a randomized controlled trial. J Pak Med Assoc. 2020;70(3):399–403. doi: 10.5455/JPMA.300523 [DOI] [PubMed] [Google Scholar]
- [48].Ashfaq M, Babur MN, Malick WH, et al. Comparative effectiveness of proprioceptive neuromuscular facilitation and passive vertebral mobilization for neck disability in patients with mechanical neck pain: a randomized controlled trial. J Bodyw Mov Ther. 2022;31:16–21. doi: 10.1016/j.jbmt.2022.02.009 [DOI] [PubMed] [Google Scholar]
- [49].Bakken AG, Eklund A, Warnqvist A, et al. The effect of two weeks of spinal manipulative therapy and home stretching exercises on pain and disability in patients with persistent or recurrent neck pain; a randomized controlled trial. BMC Musculoskelet Disord. 2021;22(1):903. doi: 10.1186/s12891-021-04772-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Bautista-Aguirre F, Oliva-Pascual-Vaca Á, Heredia-Rizo AM, et al. Effect of cervical vs. thoracic spinal manipulation on peripheral neural features and grip strength in subjects with chronic mechanical neck pain: a randomized controlled trial. Eur J Phys Rehabil Med. 2017;53(3):333–341. doi: 10.23736/S1973-9087.17.04431-8 [DOI] [PubMed] [Google Scholar]
- [51].Bernal-Utrera C, Gonzalez-Gerez JJ, Anarte-Lazo E, et al. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: a randomized controlled trial. Trials. 2020;21(1):682. doi: 10.1186/s13063-020-04610-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Blickenstaff B, Perman J, Rojan A, et al. The immediate effects of kinesio taping versus thoracic manipulation in subjects with mechanical neck pain: a pilot study. Orthop Phys Ther Prac. 2017;29(2):92–97. https://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,ip,uid&db=cul&AN=122803092&site=ehost-live&scope=site [Google Scholar]
- [53].Bracht MA, Coan ACB, Yahya A, et al. Effects of cervical manipulation on pain, grip force control, and upper extremity muscle activity: a randomized controlled trial. J Man Manip Ther. 2018;26(2):78–88. doi: 10.1080/10669817.2017.1393177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bronfort G, Aker PD, Evans R, et al. A randomized controlled clinical trial of rehabilitative exercise and chiropractic spinal manipulation for chronic neck pain. Spine. 2001;267(7):788–799. 10.1097/00007632-200104010-00020 [DOI] [PubMed] [Google Scholar]
- [55].Brück K, Jacobi K, Schmidt T. Fascial treatment versus manual therapy (HVLA) in patients with chronic neck pain: a randomized controlled trial. J Back Musculoskelet Rehabil. 2021;34(6):997–1006. doi: 10.3233/BMR-191731 [DOI] [PubMed] [Google Scholar]
- [56].Buyukturan O, Buyukturan B, Sas S, et al. The effect of mulligan mobilization technique in older adults with neck pain: a randomized controlled, double-blind study. Pain Res Manag. 2018;2018:1–7. doi: 10.1155/2018/2856375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Kim BJ, Park AL, Hwang MS, et al. Comparative effectiveness and safety of concomitant treatment with chuna manual therapy and usual care for whiplash injuries: a multicenter randomized controlled trial. IJERPH. 2022;19(17):1–12. doi: 10.3390/ijerph191710678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Calvo-Lobo C, Unda-Solano F, López-López D, et al. Is pharmacologic treatment better than neural mobilization for cervicobrachial pain? a randomized clinical trial. Int J Med Sci. 2018;15(5):456–465. doi: 10.7150/ijms.23525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Campa-Moran I, Rey-Gudin E, Fernandez-Carnero J, et al. Comparison of dry needling versus orthopedic manual therapy in patients with myofascial chronic neck pain: a single-blind, randomized pilot study. Pain Res Treat. 2015;2015(101566863):327307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Carrasco-Uribarren A, Rodríguez-Sanz J, López-de-Celis C, et al. An upper cervical spine treatment protocol for cervicogenic dizziness: a randomized controlled trial. Physiother Theory Pract. 2022;38(13):2640–2649. doi: 10.1080/09593985.2021.1972500 [DOI] [PubMed] [Google Scholar]
- [61].Carrasco-Uribarren A, Rodriguez-Sanz J, López-de-Celis C, et al. Short-term effects of the traction-manipulation protocol in dizziness intensity and disability in cervicogenic dizziness: a randomized controlled trial. Disabil Rehabil. 2022;44(14):3601–3609. doi: 10.1080/09638288.2021.1872719 [DOI] [PubMed] [Google Scholar]
- [62].Carrasco-Uribarren A, Pardos-Aguilella P, Pérez-Guillén S, et al. Combination of two manipulative techniques for the treatment of cervicogenic dizziness: a randomized controlled trial. Life. 2022;12(7):1023. doi: 10.3390/life12071023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Casanova-Méndez A, Oliva-Pascual-Vaca A, Rodriguez-Blanco C, et al. Comparative short-term effects of two thoracic spinal manipulation techniques in subjects with chronic mechanical neck pain: a randomized controlled trial. Man Ther. 2014;19(4):331–337. doi: 10.1016/j.math.2014.03.002 [DOI] [PubMed] [Google Scholar]
- [64].Celenay ST, Akbayrak T, Kaya DO. A comparison of the effects of stabilization exercises plus manual therapy to those of stabilization exercises alone in patients with nonspecific mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2016;46(2):44–55. doi: 10.2519/jospt.2016.5979 [DOI] [PubMed] [Google Scholar]
- [65].Chaibi A, Benth JS, Tuchin PJ, et al. Chiropractic spinal manipulative therapy for migraine: a three-armed, single-blinded, placebo, randomized controlled trial. Eur J Neurol. 2017;241(1):143–153. doi: 10.1111/ene.13166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Cholewicki J, JM P Jr, Reeves NP, et al. The effects of osteopathic manipulative treatment on pain and disability in patients with chronic neck pain: a single-blinded randomized controlled trial. PM R. 2022;14(12):1417–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Cleland JA, Childs JD, McRae M, et al. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10(2):127–135. doi: 10.1016/j.math.2004.08.005 [DOI] [PubMed] [Google Scholar]
- [68].Cleland JA, Mintken PE, Carpenter K, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90(9):1239–1250. doi: 10.2522/ptj.20100123 [DOI] [PubMed] [Google Scholar]
- [69].Copurgensli C, Gur G, Tunay VB. A comparison of the effects of mulligan’s mobilization and Kinesio taping on pain, range of motion, muscle strength, and neck disability in patients with cervical spondylosis: a randomized controlled study. J Back Musculoskelet Rehabil. 2017;30(1):51–62. doi: 10.3233/BMR-160713 [DOI] [PubMed] [Google Scholar]
- [70].Corum M, Aydin T, Medin Ceylan C, et al. The comparative effects of spinal manipulation, myofascial release and exercise in tension-type headache patients with neck pain: a randomized controlled trial. Complement Ther Clin Pract. 2021;43 doi: 10.1016/j.ctcp.2021.101319 [DOI] [PubMed] [Google Scholar]
- [71].Kim DH, Kim SY. Comparison of immediate effects of sling-based manual therapy on specific spine levels in subjects with neck pain and forward head posture: a randomized clinical trial. Disabil Rehabil. 2020;42(19):2735–2742. doi: 10.1080/09638288.2019.1571638 [DOI] [PubMed] [Google Scholar]
- [72].Maduro de Camargo V, Alburquerque-Sendín F, Bérzin F, et al. Immediate effects on electromyographic activity and pressure pain thresholds after a cervical manipulation in mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2011;34(4):211–220. doi: 10.1016/j.jmpt.2011.02.002 [DOI] [PubMed] [Google Scholar]
- [73].De Hertogh W, Vaes P, Devroey D, et al. Preliminary results, methodological considerations and recruitment difficulties of a randomised clinical trial comparing two treatment regimens for patients with headache and neck pain. BMC Musculoskelet Disord. 2009;10(1):115. doi: 10.1186/1471-2474-10-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Domingues L, Pimentel-Santos FM, Cruz EB, et al. Is a combined programme of manual therapy and exercise more effective than usual care in patients with non-specific chronic neck pain? a randomized controlled trial. Clin Rehabil. 2019;33(12):1908–1918. doi: 10.1177/0269215519876675 [DOI] [PubMed] [Google Scholar]
- [75].Dunning JR, Cleland JA, Waldrop MA, et al. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2012;42(1):5–18. doi: 10.2519/jospt.2012.3894 [DOI] [PubMed] [Google Scholar]
- [76].Dunning JR, Butts R, Mourad F, et al. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC Musculoskelet Disord. 2016;17(1):64. doi: 10.1186/s12891-016-0912-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Duymaz T, Yagci N. Effectiveness of the mulligan mobilization technique in mechanical neck pain. Clin Anal Med. 2018;94(4):304–309. doi: 10.4328/JCAM.5715 [DOI] [Google Scholar]
- [78].Dziedzic K, Hill J, Lewis M, et al. Effectiveness of manual therapy or pulsed shortwave diathermy in addition to advice and exercise for neck disorders: a pragmatic randomized controlled trial in physical therapy clinics. Arthritis Rheum. 2005;532(2):214–222. doi: 10.1002/art.21087 [DOI] [PubMed] [Google Scholar]
- [79].Erdem EU, Ünver B, Akbas E, et al. Immediate effects of thoracic manipulation on cervical joint position sense in individuals with mechanical neck pain: a randomized controlled trial. BMR. 2021;34(5):735–743. doi: 10.3233/BMR-191798 [DOI] [PubMed] [Google Scholar]
- [80].Evans R, Bronfort G, Schulz C, et al. Supervised exercise with and without spinal manipulation performs similarly and better than home exercise for chronic neck pain: a randomized controlled trial. Spine. 2012;37(11):903–914. doi: 10.1097/BRS.0b013e31823b3bdf [DOI] [PubMed] [Google Scholar]
- [81].Farooq MN, Mohseni-Bandpei MA, Gilani SA, et al. The effects of neck mobilization in patients with chronic neck pain: a randomized controlled trial. J Bodyw Mov Ther. 2018;22(1):24–31. doi: 10.1016/j.jbmt.2017.03.007 [DOI] [PubMed] [Google Scholar]
- [82].Fathollahnejad K, Letafatkar A, Hadadnezhad M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: a six-week intervention with a one-month follow-up study. BMC Musculoskelet Disord. 2019;20(1):86. doi: 10.1186/s12891-019-2438-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Fernandez-de-Las-Pen C, Fernandez-Carnero J, Palomeque DC, et al. Manipulative treatment vs. conventional physiotherapy treatment in whiplash injury: a randomized controlled trial. J Whiplash Related Disord. 2004;32(2):73–90. doi: 10.3109/J180v03n02_06 [DOI] [Google Scholar]
- [84].Fernandez-de-Las-Pen C, Fernandez-Carnero J, Fernandez AP, et al. Dorsal manipulation in whiplash injury treatment: a randomized controlled trial. J Whiplash Related Disord. 2004;32(2):55–72. doi: 10.3109/J180v03n02_05 [DOI] [Google Scholar]
- [85].Galindez-Ibarbengoetxea X, Setuain I, Ramírez-Velez R, et al. Short-term effects of manipulative treatment versus a therapeutic home exercise protocol for chronic cervical pain: a randomized clinical trial. J Back Musculoskelet Rehabil. 2018;31(1):133–145. doi: 10.3233/BMR-169723 [DOI] [PubMed] [Google Scholar]
- [86].Galindez-Ibarbengoetxea X, Setuain I, Ramírez-Velez R, et al. Immediate effects of osteopathic treatment versus therapeutic exercise on patients with chronic cervical pain. Altern Ther Health Med. 2018;24(3):24–32. [PubMed] [Google Scholar]
- [87].García-Pérez-Juana D, Fernández-de-Las- PeñPeñAs C, Arias-Buría JL, et al. Changes in cervicocephalic kinesthetic sensibility, widespread pressure pain sensitivity, and neck pain after cervical thrust manipulation in patients with chronic mechanical neck pain: a randomized clinical trial. J Manip Physiol Ther. 2018;41(7):551–560. doi: 10.1016/j.jmpt.2018.02.004 [DOI] [PubMed] [Google Scholar]
- [88].Gemmell H, Miller P. Relative effectiveness and adverse effects of cervical manipulation, mobilisation and the activator instrument in patients with sub-acute non-specific neck pain: results from a stopped randomised trial. Chiropr Osteopat. 2010;18:14p–14p. doi: 10.1186/1746-1340-18-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Giles LG, Müller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipulative Physiol Ther. 1999;226(6):376–381. doi: 10.1016/S0161-4754(99)70082-5 [DOI] [PubMed] [Google Scholar]
- [90].Gómez F, Escribá P, Oliva-Pascual-Vaca J, et al. Immediate and short-term effects of upper cervical high-velocity, low-amplitude manipulation on standing postural control and cervical mobility in chronic nonspecific neck pain: a randomized controlled trial. J Clin Med Res. 2020;9(8). doi: 10.3390/jcm9082580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].González-Rueda V, Hidalgo-García C, Rodríguez-Sanz J, et al. Does upper cervical manual therapy provide additional benefit in disability and mobility over a physiotherapy primary care program for chronic cervicalgia? a randomized controlled trial. Int J Environ Res Public Health. 2020;17(22):8334. doi: 10.3390/ijerph17228334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].González-Rueda V, López-de-Celis C, Bueno-Gracia E, et al. Short- and mid-term effects of adding upper cervical manual therapy to a conventional physical therapy program in patients with chronic mechanical neck pain. randomized controlled clinical trial. Clin Rehabil. 2021;35(3):378–389. [DOI] [PubMed] [Google Scholar]
- [93].Gorrell LM, Beath K, Engel RM. Manual and instrument applied cervical manipulation for mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2016;395(5):319–329. doi: 10.1016/j.jmpt.2016.03.003 [DOI] [PubMed] [Google Scholar]
- [94].Griswold D, Learman K, Kolber MJ, et al. Pragmatically applied cervical and thoracic nonthrust manipulation versus thrust manipulation for patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2018;48(3):137–145. doi: 10.2519/jospt.2018.7738 [DOI] [PubMed] [Google Scholar]
- [95].Griswold D, Learman K, O’Halloran B, et al. A preliminary study comparing the use of cervical/upper thoracic mobilization and manipulation for individuals with mechanical neck pain. J Man Manip Ther. 2015;23(2):75–83. doi: 10.1179/2042618614Y.0000000095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Groeneweg R, van Assen L, Kropman H, et al. Manual therapy compared with physical therapy in patients with non-specific neck pain: a randomized controlled trial. Chiropr Man Therap. 2017;25(1):12. doi: 10.1186/s12998-017-0141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Groisman S, Malysz T, de Souza da Silva L, et al. Osteopathic manipulative treatment combined with exercise improves pain and disability in individuals with non-specific chronic neck pain: a pragmatic randomized controlled trial. J Bodyw Mov Ther. 2020;24(2):189–195. doi: 10.1016/j.jbmt.2019.11.002 [DOI] [PubMed] [Google Scholar]
- [98].Haas M, Bronfort G, Evans R, et al. Dose-response and efficacy of spinal manipulation for care of cervicogenic headache: a dual-center randomized controlled trial. Spine J. 2018;18(10):1741–1754. doi: 10.1016/j.spinee.2018.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Haas M, Groupp E, Aickin M, et al. Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manipulative Physiol Ther. 2004;27(9):547–553. doi: 10.1016/j.jmpt.2004.10.007 [DOI] [PubMed] [Google Scholar]
- [100].Häkkinen A, Salo P, Tarvainen U, et al. Effect of manual therapy and stretching on neck muscle strength and mobility in chronic neck pain. J Rehabil Med. 2007;39(7):575–579. doi: 10.2340/16501977-0094 [DOI] [PubMed] [Google Scholar]
- [101].Hassan F, Osama M, Ghafoor A, et al. Effects of oscillatory mobilization as compared to sustained stretch mobilization in the management of cervical radiculopathy: a randomized controlled trial. J Back Musculoskelet Rehabil. 2020;33(1):153–158. doi: 10.3233/BMR-170914 [DOI] [PubMed] [Google Scholar]
- [102].Hemmilä HM Bone setting for prolonged neck pain: a randomized clinical trial. J Manipulative Physiol Ther. 2005;287(7):508–515. doi: 10.1016/j.jmpt.2005.07.008 [DOI] [PubMed] [Google Scholar]
- [103].Hurwitz EL, Morgenstern H, Harber P, et al. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the ucla neck-pain study. Am J Public Health. 2002;9210(10):1634–1641. doi: 10.2105/AJPH.92.10.1634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Jafari M, Bahrpeyma F, Togha M, et al. Effects of upper cervical spine manual therapy on central sensitization and disability in subjects with migraine and neck pain. Muscles, Ligaments & Tendons J. 2023;13(1):177–185. doi: 10.32098/mltj.01.2023.21 [DOI] [Google Scholar]
- [105].Jordan A, Bendix T, Nielsen H, et al. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain. A prospective, single-blinded, randomized clinical trial. Spine. 1998;233(3):311–318. doi: 10.1097/00007632-199802010-00005 [DOI] [PubMed] [Google Scholar]
- [106].Kanlayanaphotporn R, Chiradejnant A, Vachalathiti R. Immediate effects of the central posteroanterior mobilization technique on pain and range of motion in patients with mechanical neck pain. Disabil Rehabil. 2010;32(8):622–628. doi: 10.3109/09638280903204716 [DOI] [PubMed] [Google Scholar]
- [107].Karas S, Olson Hunt MJ. A randomized clinical trial to compare the immediate effects of seated thoracic manipulation and targeted supine thoracic manipulation on cervical spine flexion range of motion and pain. J Man Manip Ther. 2014;22(2):108–114. doi: 10.1179/2042618613Y.0000000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Karas S, Hunt MJO, Temes B, et al. The effect of direction specific thoracic spine manipulation on the cervical spine: a randomized controlled trial. J Man Manip Ther. 2018;26(1):3–10. doi: 10.1080/10669817.2016.1260674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Kashif M, Manzoor N, Safdar R, et al. Effectiveness of sustained natural apophyseal glides in females with cervicogenic headache: a randomized controlled trial. J Back Musculoskelet Rehabil. 2022;35(3):597–603. doi: 10.3233/BMR-210018 [DOI] [PubMed] [Google Scholar]
- [110].Kaur A, Mali K, Mitra M. To compare the immediate effects of active cranio cervical flexion exercise versus passive mobilization of upper cervical spine on pain, range of motion and cranio cervical flexion test in patients with chronic neck pain. Indian J Physiother Occup. 2018;12(3):22–27. doi: 10.5958/0973-5674.2018.00050.3 [DOI] [Google Scholar]
- [111].Kelly DD, Murphy BA, Backhouse DP. Use of a mental rotation reaction-time paradigm to measure the effects of upper cervical adjustments on cortical processing: a pilot study. J Manipulative Physiol Ther. 2000;23(4):246–251. doi: 10.1067/mmt.2000.106099 [DOI] [PubMed] [Google Scholar]
- [112].Kendall JC, French SD, Hartvigsen J, et al. Chiropractic treatment including instrument-assisted manipulation for non-specific dizziness and neck pain in community-dwelling older people: a feasibility randomised sham-controlled trial. Chiropr Man Therap. 2018;26(1):14. doi: 10.1186/s12998-018-0183-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Khatwani P, Yadav J, Kalra S. The effect of cervical lateral glide and manual cervical traction combined with neural mobilization on patients with cervical radiculopathy. Indian J Physiother Occup. 2015;9(4):152–158. doi: 10.5958/0973-5674.2015.00163.X [DOI] [Google Scholar]
- [114].Kim SY, An CM, Cha YS, et al. Effects of sling-based manual therapy on cervicothoracic junction in patients with neck pain and forward head posture: a randomized clinical trial. J Bodyw Mov Ther. 2021;27:447–454. doi: 10.1016/j.jbmt.2021.03.007 [DOI] [PubMed] [Google Scholar]
- [115].Krauss J, Creighton D, Ely JD, et al. The immediate effects of upper thoracic translatoric spinal manipulation on cervical pain and range of motion: a randomized clinical trial. J Orthop Sports Phys Ther. 2008;391(1):A18–A18. doi: 10.1179/106698108790818530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Lagoutaris C, Sullivan J, Hancock M, et al. Approaches to cervical spine mobilization for neck pain: a pilot randomized controlled trial. Chiropr Man Therap. 2020;28(1):61. doi: 10.1186/s12998-020-00348-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Langevin P, Roy J-S, Desmeules F, et al. Cervical radiculopathy: A randomized clinical trial evaluating the short-term effect of two manual therapy and exercise protocols. Physiother. 2015;101:eS820–eS821. doi: 10.1016/j.physio.2015.03.3709 [DOI] [PubMed] [Google Scholar]
- [118].Langevin P, Desmeules F, Lamothe M, et al. Comparison of two manual therapy and exercise protocols for cervical radiculopathy: a randomized clinical trial evaluating short-term effects. J Orthop Sports Phys Ther. 2015;45(1):4–17. doi: 10.2519/jospt.2015.5211 [DOI] [PubMed] [Google Scholar]
- [119].Lau MH. To investigate the immediate and long term effects of thoracic manipulation (TM) in patients with chronic mechanical neck pain: a randomized controlled trial. 2011. [DOI] [PubMed]
- [120].Leaver AM, Maher CG, Herbert RD, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Arch Phys Med Rehabil. 2010;91(9):1313–1318. doi: 10.1016/j.apmr.2010.06.006 [DOI] [PubMed] [Google Scholar]
- [121].Lee KW, Kim WH. Effect of thoracic manipulation and deep craniocervical flexor training on pain, mobility, strength, and disability of the neck of patients with chronic nonspecific neck pain: a randomized clinical trial. J Phys Therapy Sci. 2016;281(1):175–180. doi: 10.1589/jpts.28.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Lerner-Lentz A, O’Halloran B, Donaldson M, et al. Pragmatic application of manipulation versus mobilization to the upper segments of the cervical spine plus exercise for treatment of cervicogenic headache: a randomized clinical trial. J Man Manip Ther. 2021;29(5):267–275. doi: 10.1080/10669817.2020.1834322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Lin JH, Shen T, Chung RCK, et al. The effectiveness of long’s manipulation on patients with chronic mechanical neck pain: a randomized controlled trial. Man Ther. 2013;18(4):308–315. doi: 10.1016/j.math.2012.11.005 [DOI] [PubMed] [Google Scholar]
- [124].Lluch E, Schomacher J, Gizzi L, et al. Immediate effects of active cranio-cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio-cervical flexion test. Man Ther. 2014;191(1):25–31. doi: 10.1016/j.math.2013.05.011 [DOI] [PubMed] [Google Scholar]
- [125].Lohman EB, Pacheco GR, Gharibvand L, et al. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2019;27(4):186–196. doi: 10.1080/10669817.2018.1553696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Lopez-Lopez A, Alonso Perez JL, González Gutierez JL, et al. Mobilization versus manipulations versus sustain apophyseal natural glide techniques and interaction with psychological factors for patients with chronic neck pain: randomized controlled trial. Eur J Phys Rehabil Med. 2015;51(2):121–132. [PubMed] [Google Scholar]
- [127].Malo-Urriés M, Tricás-Moreno JM, Estébanez-de-Miguel E, et al. Immediate effects of upper cervical translatoric mobilization on cervical mobility and pressure pain threshold in patients with cervicogenic headache: a randomized controlled trial. J Manipulative Physiol Ther. 2017;40(9):649–658. doi: 10.1016/j.jmpt.2017.07.007 [DOI] [PubMed] [Google Scholar]
- [128].Marks M, Schottker-Koniger T, Probst A. Efficacy of cervical spine mobilization versus peripheral nerve slider techniques in cervicobrachial pain syndrome- a randomized clinical trial. J Phys Therapy Sci. 2011;41(1):9–17. [Google Scholar]
- [129].Martel J, Dugas C, Dubois JD, et al. A randomised controlled trial of preventive spinal manipulation with and without a home exercise program for patients with chronic neck pain. BMC Musculoskelet Disord. 2011;12(1):41. doi: 10.1186/1471-2474-12-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Martínez-Segura R, Fernández-de-Las- PeñPeñAs C, Ruiz-Sáez M, et al. Immediate effects on neck pain and active range of motion after a single cervical high-velocity low-amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2006;297(7):511–517. doi: 10.1016/j.jmpt.2006.06.022 [DOI] [PubMed] [Google Scholar]
- [131].Martínez-Segura R, de-la-Llave-Rincón AI, Ortega-Santiago R, et al. Immediate changes in widespread pressure pain sensitivity, neck pain, and cervical range of motion after cervical or thoracic thrust manipulation in patients with bilateral chronic mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2012;42(9):806–814. doi: 10.2519/jospt.2012.4151 [DOI] [PubMed] [Google Scholar]
- [132].Masaracchio M, Cleland J, Hellman M, et al. Short-term combined effects of thoracic spine thrust manipulation and cervical spine nonthrust manipulation in individuals with mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43(3):118–127. doi: 10.2519/jospt.2013.4221 [DOI] [PubMed] [Google Scholar]
- [133].McDevitt AW, Cleland JA, Rhon DI, et al. Thoracic spine thrust manipulation for individuals with cervicogenic headache: a crossover randomized clinical trial. J Man Manip Ther. 2022;30(2):78–95. doi: 10.1080/10669817.2021.1947663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. JAOA J American Osteopathic Ass. 2005;105(2):57–68. [PubMed] [Google Scholar]
- [135].Micarelli A, Viziano A, Granito I, et al. Postural and clinical outcomes of sustained natural apophyseal glides treatment in cervicogenic dizziness patients: a randomised controlled trial. Clin Rehabil. 2021;35(11):1566–1576. doi: 10.1177/02692155211012413 [DOI] [PubMed] [Google Scholar]
- [136].Ferreira Miranda I, Facchini D, Manfio EF. Influence of the cervical spine manipulation in the neck disability index in patients with chronic neck pain: a preliminary study. Man Ther Posturology Rehabil J. 2015;13:1–5. doi: 10.17784/mtprehabJournal.2015.13.283 [DOI] [Google Scholar]
- [137].Nambi G, Alghadier M, Ebrahim EE, et al. Comparative effects of Mulligan’s mobilization, spinal manipulation, and conventional massage therapy in cervicogenic headache—A prospective, randomized, controlled trial. Healthcare. 2022;11(1). doi: 10.3390/healthcare11010107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Nee RJ, Vicenzino B, Jull GA, et al. Neural tissue management provides immediate clinically relevant benefits without harmful effects for patients with nerve-related neck and arm pain: a randomised trial. J Physiother. 2012;58(1):23–31. doi: 10.1016/S1836-9553(12)70069-3 [DOI] [PubMed] [Google Scholar]
- [139].Nilsson N. A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1995;18(7):435–440. [PubMed] [Google Scholar]
- [140].Nilsson N, Yang K. A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1996;19(4):282–282. [PubMed] [Google Scholar]
- [141].Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1997;20(5):326–330. [PubMed] [Google Scholar]
- [142].Ouseley BR, Parkin-Smith GF. Possible effects of chiropractic spinal manipulation and mobilization in the treatment of chronic tension-type headache: a pilot study. J European Of Chiropract. 2002;50(1):3–13. [Google Scholar]
- [143].Paanalahti K, Wertli MM, Held U, et al. Spinal pain-good sleep matters: a secondary analysis of a randomized controlled trial. Eur Spine J. 2016;25(3):760–765. [DOI] [PubMed] [Google Scholar]
- [144].Palmgren PJ, Sandstrom PJ, Lundqvist FJ, et al. Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. J Manipulative Physiol Ther. 2006;29(2):100–106. doi: 10.1016/j.jmpt.2005.12.002 [DOI] [PubMed] [Google Scholar]
- [145].Peña-Salinas M, Oliva-Pascual-Vaca J, Heredia-Rizo AM, et al. No immediate changes on neural and muscular mechanosensitivity after first rib manipulation in subjects with cervical whiplash: a randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30(4):921–928. doi: 10.3233/BMR-160645 [DOI] [PubMed] [Google Scholar]
- [146].Perveen S, Zahra SR, Mahmood T, et al. Effects of low amplitude high velocity thurst manipulation as compare to grade III Maitland mobilization of thoracic spine on mechanical neck pain and disability. J Liaq Uni Med Health Sci. 2020;19(4):252–256. [Google Scholar]
- [147].Pillastrini P, de Lima E, Sá Resende F, et al. Effectiveness of global postural re-education in patients with chronic nonspecific neck pain: randomized controlled trial. Phys Ther. 2016;96(9):1408–1416. doi: 10.2522/ptj.20150501 [DOI] [PubMed] [Google Scholar]
- [148].Pires PF, Packer AC, Dibai-Filho AV, et al. Immediate and short-term effects of upper thoracic manipulation on myoelectric activity of sternocleidomastoid muscles in young women with chronic neck pain: a randomized blind clinical trial. J Manipulative Physiol Ther. 2015;388(8):555–563. doi: 10.1016/j.jmpt.2015.06.016 [DOI] [PubMed] [Google Scholar]
- [149].Pool JJ, Ostelo RW, Knol DL, et al. Is a behavioral graded activity program more effective than manual therapy in patients with subacute neck pain? results of a randomized clinical trial. Spine. 2010;3510(10):1017–1024. doi: 10.1097/BRS.0b013e3181c212ee [DOI] [PubMed] [Google Scholar]
- [150].Prabhakar R, Ramteke GJ. Cervical spine mobilization versus tens in the management of cervical radiculopathy: a comparative experimental randomized controlled trial. Indian J Physiother Occup. 2011;52(2):128–133. [Google Scholar]
- [151].Harihara Prakash R, Mehta J, Patel D. Effect of thrust versus non-thrust mobilization directed at the thoracic spine in patients with mechanical neck pain: a randomized control trial. Natl J Physiol Pharm Pharmacol. 2020;1010(10):878–883. doi: 10.5455/njppp.2020.10.05129202004072020 [DOI] [Google Scholar]
- [152].Puentedura EJ, Landers MR, Cleland JA, et al. Thoracic spine thrust manipulation versus cervical spine thrust manipulation in patients with acute neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(4):208–220. doi: 10.2519/jospt2011.3640 [DOI] [PubMed] [Google Scholar]
- [153].Puntumetakul R, Suvarnnato T, Werasirirat P, et al. Acute effects of single and multiple level thoracic manipulations on chronic mechanical neck pain: a randomized controlled trial. Neuropsychiatr Dis Treat. 2015;11:137–144. doi: 10.2147/NDT.S69579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Ranganath PNU, Dowle P, Chandrasekhar P. Effectiveness of mwm, neurodynamics and conventional therapy versus neurodynamics and conventional therapy in unilateral cervical radiculopathy: a randomized control trial. Indian J Physiother Occup. 2018;12(3):101–106. doi: 10.5958/0973-5674.2018.00066.7 [DOI] [Google Scholar]
- [155].Rani M, Kaur J. Effectiveness of spinal mobilization and postural correction exercises in the management of cervicogenic headache: a randomized controlled trial. Physiother Theory Pract. 2022;(9015520):1–15. doi: 10.1080/09593985.2022.2037032 [DOI] [PubMed] [Google Scholar]
- [156].Rani M, Kaur J. Effectiveness of different physiotherapy interventions in the management of cervicogenic headache: a pilot randomized controlled trial. J Man Manip Ther. 2022;302(2):96–104. doi: 10.1080/10669817.2021.1962687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Razzaq A, Sajjad AG, Yasin S, et al. Comparison of cyriax manipulation with traditional physical therapy for the management of cervical discogenic problems. A randomized control trial. J Pak Med Assoc. 2020;70(8):1329–1333. doi: 10.5455/JPMA.13250 [DOI] [PubMed] [Google Scholar]
- [158].Reid SA, Rivett DA, Katekar MG, et al. Sustained natural apophyseal glides (snags) are an effective treatment for cervicogenic dizziness. Man Ther. 2008;13(4):357–366. doi: 10.1016/j.math.2007.03.006 [DOI] [PubMed] [Google Scholar]
- [159].Reid SA, Callister R, Katekar MG, et al. Effects of cervical spine manual therapy on range of motion, head repositioning, and balance in participants with cervicogenic dizziness: a randomized controlled trial. Arch Phys Med Rehabil. 2014;95(9):1603–1612. doi: 10.1016/j.apmr.2014.04.009 [DOI] [PubMed] [Google Scholar]
- [160].Reid SA, Rivett DA, Katekar MG, et al. Comparison of mulligan sustained natural apophyseal glides and Maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Phys Ther. 2014;94(4):466–476. doi: 10.2522/ptj.20120483 [DOI] [PubMed] [Google Scholar]
- [161].Arjona Retamal JJ, Fernández Seijo A, Torres Cintas JD, et al. Effects of instrumental, manipulative and soft tissue approaches for the suboccipital region in subjects with chronic mechanical neck pain. A randomized controlled trial. Int J Environ Res Public Health. 2021;18(16). doi: 10.3390/ijerph18168636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Rezkallah SS, Abdullah GA. Comparison between sustained natural apophyseal glides (snags) and myofascial release techniques combined with exercises in non specific neck pain. Physiother Prac Res. 2018;39(2):135–145. doi: 10.3233/PPR-180116 [DOI] [Google Scholar]
- [163].Rodriguez-Sanz J, Malo-Urries M, Lucha-Lopez MO, et al. Comparison of an exercise program with and without manual therapy for patients with chronic neck pain and upper cervical rotation restriction. randomized controlled trial. PeerJ. 2021;9(101603425):e12546. doi: 10.7717/peerj.12546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Rodriguez-Sanz D, Calvo-Lobo C, Unda-Solano F, et al. Cervical lateral glide neural mobilization is effective in treating cervicobrachial pain: a randomized waiting list controlled clinical trial. Pain Med. 2017;18(12):2492–2503. doi: 10.1093/pm/pnx011 [DOI] [PubMed] [Google Scholar]
- [165].Rodríguez-Sanz J, Malo-Urriés M, Corral-de-Toro J, et al. Short- and medium-term effects of manual therapy on the upper cervical spine combined with exercise vs isolated exercise in patients with cervicogenic headache. A randomized controlled trial. Int J Osteopath Med. 2022;43:5–15. doi: 10.1016/j.ijosm.2022.04.006 [DOI] [Google Scholar]
- [166].Rodríguez-Sanz J, Malo-Urriés M, Lucha-López MO, et al. Effects of the manual therapy approach of segments C0-1 and C2-3 in the flexion-rotation test in patients with chronic neck pain: a randomized controlled trial. Int J Environ Res Public Health. 2021;18(2):753. doi: 10.3390/ijerph18020753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Rodríguez-Sanz J, Malo-Urriés M, Lucha-López MO, et al. Is cervical stabilization exercise immediately effective in patients with chronic neck pain and upper cervical spine dysfunction? randomized controlled trial. Life. 2022;12(5):714. doi: 10.3390/life12050714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Romero Del Rey R, Saavedra Hernández M, Rodríguez Blanco C, et al. Short-term effects of spinal thrust joint manipulation on postural sway in patients with chronic mechanical neck pain: a randomized controlled trial. Disabil Rehabil. 2022;44(8):1227–1233. doi: 10.1080/09638288.2020.1798517 [DOI] [PubMed] [Google Scholar]
- [169].Saavedra-Hernández M, Castro-Sánchez AM, Arroyo-Morales M, et al. Short-term effects of kinesio taping versus cervical thrust manipulation in patients with mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2012;42(8):724–730. doi: 10.2519/jospt.2012.4086 [DOI] [PubMed] [Google Scholar]
- [170].Saavedra-Hernández M, Arroyo-Morales M, Cantarero-Villanueva I, et al. Short-term effects of spinal thrust joint manipulation in patients with chronic neck pain: a randomized clinical trial. Clin Rehabil. 2013;27(6):504–512. doi: 10.1177/0269215512464501 [DOI] [PubMed] [Google Scholar]
- [171].Saayman L, Hay C, Abrahamse H. Chiropractic manipulative therapy and low-level laser therapy in the management of cervical facet dysfunction: a randomized controlled study. J Manipulative Physiol Ther. 2011;343(3):153–163. doi: 10.1016/j.jmpt.2011.02.010 [DOI] [PubMed] [Google Scholar]
- [172].Salom-Moreno J, Ortega-Santiago R, Cleland JA, et al. Immediate changes in neck pain intensity and widespread pressure pain sensitivity in patients with bilateral chronic mechanical neck pain: a randomized controlled trial of thoracic thrust manipulation vs non-thrust mobilization. J Manipulative Physiol Ther. 2014;375(5):312–319. doi: 10.1016/j.jmpt.2014.03.003 [DOI] [PubMed] [Google Scholar]
- [173].Santiago RJ, Esteves JE, Baptista JS, et al. Results of a feasibility randomised controlled trial of osteopathy on neck-shoulder pain in computer users. Complement Ther Clin Pract. 2022;46:N.PAG- N.PAG. doi: 10.1016/j.ctcp.2021.101507 [DOI] [PubMed] [Google Scholar]
- [174].Savolainen A, Ahlberg J, Nummila H, et al. Active or passive treatment for neck-shoulder pain in occupational health care? a randomized controlled trial. Occup Med. 2004;546(6):422–424. doi: 10.1093/occmed/kqh070 [DOI] [PubMed] [Google Scholar]
- [175].Schomacher J. The effect of an analgesic mobilization technique when applied at symptomatic or asymptomatic levels of the cervical spine in subjects with neck pain: a randomized controlled trial. J Man Manip Ther. 2009;17(2):101–108. doi: 10.1179/106698109790824758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [176].Schwerla F, Bischoff A, Nurnberger A, et al. Osteopathic treatment of patients with chronic non-specific neck pain: a randomised controlled trial of efficacy. Forsch Komplementmed. 2008;15(3):138–145. doi: 10.1159/000132397 [DOI] [PubMed] [Google Scholar]
- [177].Seo J, Song C, Shin D. A single-center study comparing the effects of thoracic spine manipulation vs mobility exercises in 26 office workers with chronic neck pain: a randomized controlled clinical study. Med Sci Monit. 2022;28:e937316. doi: 10.12659/MSM.937316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Shabbir M, Rafique S, Majeed R, et al. Comparison of sub-occipital myofascial release and cervical mobilization in managing cervicogenic headache. Med Forum Mon. 2021;329(9):110–114. [Google Scholar]
- [179].Shabbir M, Arshad N, Naz A, et al. Clinical outcomes of Maitland mobilization in patients with myofascial chronic neck pain: a randomized controlled trial. Pak J Med Sci Q. 2021;37(4):1172–1178. doi: 10.12669/pjms.37.4.4220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Shafique S, Ahmad S, Shakil-Ur-Rehman S. Effect of mulligan spinal mobilization with arm movement along with neurodynamics and manual traction in cervical radiculopathy patients: a randomized controlled trial. J Pak Med Assoc. 2019;69(11):1601–1604. doi: 10.5455/JPMA.297956. [DOI] [PubMed] [Google Scholar]
- [181].Sharma A, Hameed UA, Grover S. Multimodal therapy in cervicogenic headache - a randomized controlled trial. Indian J Physiother Occup. 2011;5(1):9–13. [Google Scholar]
- [182].Sillevis R, Cleland J, Hellman M, et al. Immediate effects of a thoracic spine thrust manipulation on the autonomic nervous system: a randomized clinical trial. J Man Manip Ther. 2010;18(4):181–190. doi: 10.1179/106698110X12804993427126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Snodgrass SJ, Rivett DA, Sterling M, et al. Dose optimization for spinal treatment effectiveness: a randomized controlled trial investigating the effects of high and low mobilization forces in patients with neck pain. J Orthop Sports Phys Ther. 2014;44(3):141–152. doi: 10.2519/jospt.2014.4778 [DOI] [PubMed] [Google Scholar]
- [184].Sterling M, Pedler A, Chan C, et al. Cervical lateral glide increases nociceptive flexion reflex threshold but not pressure or thermal pain thresholds in chronic whiplash associated disorders: a pilot randomised controlled trial. Man Ther. 2010;152(2):149–153. doi: 10.1016/j.math.2009.09.004 [DOI] [PubMed] [Google Scholar]
- [185].Suvarnnato T, Puntumetakul R, Kaber D, et al. The effects of thoracic manipulation versus mobilization for chronic neck pain: a randomized controlled trial pilot study. J Phys Therapy Sci. 2013;25(7):865–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Tahir R, Ammar Ahmad Sohail M, Ain NU, et al. Comparative effect of upper thoracic spine mobilization with mobility exercises and upper cervical spine mobilization with stabilization exercises in mechanical neck pain: a randomized clinical trial. Anaesth Pain Intensive Care. 2022;26(4):488–495. doi: 10.35975/apic.v26i4.1952 [DOI] [Google Scholar]
- [187].Valera-Calero A, Lluch Girbes E, Gallego-Izquierdo T, et al. Endocrine response after cervical manipulation and mobilization in people with chronic mechanical neck pain: a randomized controlled trial. Eur J Phys Rehabil Med. 2019;55(6):792–805. doi: 10.23736/S1973-9087.19.05475-3 [DOI] [PubMed] [Google Scholar]
- [188].van Dongen JM, Groeneweg R, Rubinstein SM, et al. Cost-effectiveness of manual therapy versus physical therapy in patients with sub-acute and chronic neck pain: a randomized controlled trial. Value Health. 2015;18(7):A669–A670. [DOI] [PubMed] [Google Scholar]
- [189].Wood TG, Collaca CJ, Matthews R. A pilot randomized clinical trial on the relative effect of instrumental (mfma) versus manual (hvla) manipulation in the treatment of cervical spine dysfunction. J Manipulative Physiol Ther. 2001;24(4):260–271. doi: 10.1067/mmt.2001.114365 [DOI] [PubMed] [Google Scholar]
- [190].Yao M, Tang ZY, Cui XJ, et al. Shi-style cervical mobilizations versus massage for cervical vertigo: a multicenter, randomized, controlled clinical trial. J Altern Complement Med. 2020;26(1):58–66. doi: 10.1089/acm.2019.0113 [DOI] [PubMed] [Google Scholar]
- [191].Yıldırım A, Akbaş A, Sürücü GD, et al. Effectiveness of mobilization practices for patients with neck pain due to myofascial pain syndrome: a randomized clinical trial. Turk J Phys Med Rehabil. 2016;62(4):337–345. doi: 10.5606/tftrd.2016.95777 [DOI] [Google Scholar]
- [192].Ylinen J, Kautiainen H, Wirén K, et al. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross-over trial. J Rehabil Med. 2007;39(2):126–132. doi: 10.2340/16501977-0015 [DOI] [PubMed] [Google Scholar]
- [193].Young IA, Pozzi F, Dunning J, et al. Immediate and short-term effects of thoracic spine manipulation in patients with cervical radiculopathy: a randomized controlled trial. J Orthop Sports Phys Ther. 2019;49(5):299–309. doi: 10.2519/jospt.2019.8150 [DOI] [PubMed] [Google Scholar]
- [194].Youssef EF, Shanb ASA. Mobilization versus massage therapy in the treatment of cervicogenic headache: a clinical study. J Back Musculoskelet Rehabil. 2013;26(1):17–24. doi: 10.3233/BMR-2012-0344 [DOI] [PubMed] [Google Scholar]
- [195].Yung E, Oh C, Wong M, et al. Non-thrust cervical manipulations reduce short-term pain and decrease systolic blood pressure during intervention in mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2020;28(2):82–93. doi: 10.1080/10669817.2019.1646985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [196].Yurkiw D, Mior S. Comparison of two chiropractic techniques on pain and lateral flexion in neck pain patients: a pilot study. Chiropractic Tech. 1996;8(4):155–162. [Google Scholar]
- [197].Zaproudina N, Hänninen OO, Airaksinen O. Effectiveness of traditional bone setting in chronic neck pain: randomized clinical trial. J Manipulative Physiol Ther. 2007;306(6):432–437. doi: 10.1016/j.jmpt.2007.05.004 [DOI] [PubMed] [Google Scholar]
- [198].Madson TJ, Cieslak KR, Gay RE. Joint mobilization vs massage for chronic mechanical neck pain: a pilot study to assess recruitment strategies and estimate outcome measure variability. J Manipulative Physiol Ther. 2010;33(9):644–651. doi: 10.1016/j.jmpt.2010.08.008 [DOI] [PubMed] [Google Scholar]
- [199].Maicki T, Bilski J, Szczygieł E, et al. PNF and manual therapy treatment results of patients with cervical spine osteoarthritis. J Back Musculoskelet Rehabil. 2017;30(5):1095–1101. doi: 10.3233/BMR-169718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200].Maiers M, Bronfort G, Evans R, et al. Spinal manipulative therapy and exercise for seniors with chronic neck pain. Spine J. 2014;149(9):1879–1889. [DOI] [PubMed] [Google Scholar]
- [201].Maiers M, Hartvigsen J, Evans R, et al. Short- or long-term treatment of spinal disability in older adults with manipulation and exercise. Arthritis Care Res. 2019;71(11):1516–1524. doi: 10.1002/acr.23798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [202].González-Iglesias J, Fernández-de-Las- PeñPeñAs C, Cleland JA, et al. Inclusion of thoracic spine thrust manipulation into an electro-therapy/thermal program for the management of patients with acute mechanical neck pain: a randomized clinical trial. Man Ther. 2009;143(3):306–313. doi: 10.1016/j.math.2008.04.006 [DOI] [PubMed] [Google Scholar]
- [203].González-Iglesias J, Fernández-de-Las- PeñPeñAs C, Cleland JA, et al. Thoracic spine manipulation for the management of patients with neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;391(1):20–27. doi: 10.2519/jospt.2009.2914 [DOI] [PubMed] [Google Scholar]
- [204].Joshi S, Balthillaya G, Neelapala YVR. Immediate effects of cervicothoracic junction mobilization versus thoracic manipulation on the range of motion and pain in mechanical neck pain with cervicothoracic junction dysfunction: a pilot randomized controlled trial. Chiropr Man Therap. 2020;28(1):38. doi: 10.1186/s12998-020-00327-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Rodríguez-Sanz J, Malo-Urriés M, Corral-de-Toro J, et al. Does the addition of manual therapy approach to a cervical exercise program improve clinical outcomes for patients with chronic neck pain in short- and mid-term? a randomized controlled trial. Int J Environ Res Public Health. 2020;17(18):6601. doi: 10.3390/ijerph17186601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206].Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27(17):1835–1843. doi: 10.1097/00007632-200209010-00004 discussion 1843. [DOI] [PubMed] [Google Scholar]
- [207].McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2020;1–7. doi: 10.1002/jrsm.1411 [DOI] [PubMed] [Google Scholar]
- [208].Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Clin Epidemiol. 2009;62(5):499–505. doi: 10.1016/j.jclinepi.2009.01.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


