Operating rooms (ORs) throughout the country have been challenged by increased turnover rates and recurrent training of new staff in the post-coronavirus disease 2019 era.1 To maintain harmony during this time, collaboration and clear communication between surgical team members is a key factor. Noise pollution, a widely established stressor, now poses an ever-bigger barrier to optimizing the OR. In addition to inhibiting communication, this environmental strain has been associated with increased rates of burnout among staff and reduced wound healing rates in patients.2,3 While noise pollution is closely monitored on certain hospital floors and within intensive care units, ORs remain largely unregulated.3,4 We sought to quantify the level of noise pollution in plastic surgery ORs and assess its effects on surgical team members and communication.
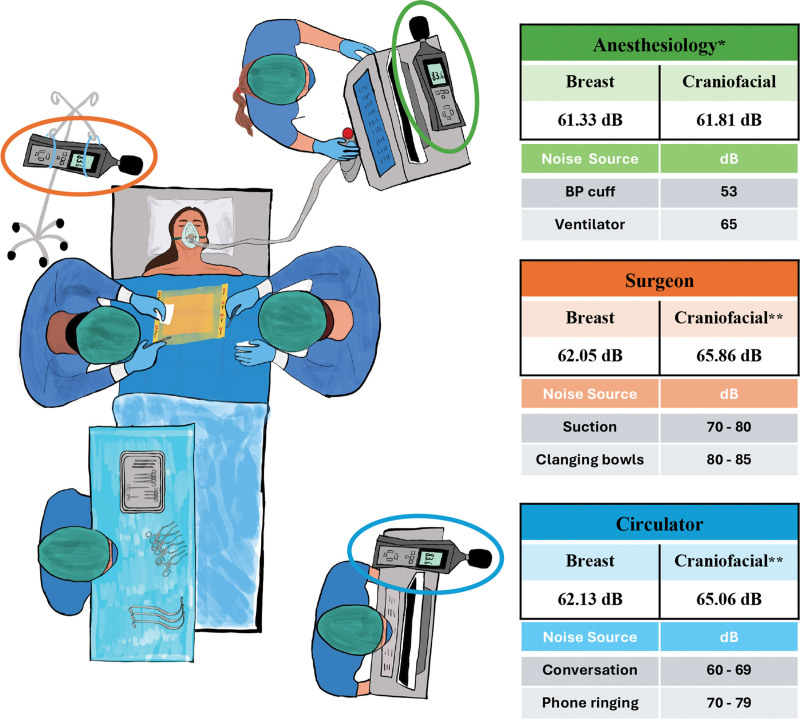
We quantified noise pollution using sound level meters placed near the anesthesiologist, surgeon, and circulating nurse (Fig. 1). Data were collected during craniofacial and breast surgery cases from patient entry to exit. Noise level was recorded in decibels (dB). A survey assessed faculty and staff experience with noise in the OR.
Fig. 1.
Average dB recorded from sound level meters placed at three locations within breast surgery and craniofacial ORs. dB readings of common sounds at each location are also provided. Statistical comparisons were made using Student t tests at a significance level of P < 0.05. *Anesthesiology sound level meters recorded significantly quieter dB than those surrounding the surgeon and circulator (P = 0.013 and P = 0.045, respectively). **Craniofacial cases were overall significantly louder than breast cases due to significant increases in noise around the surgeon and circulator (P = 0.002 and P = 0.018, respectively). BP, blood pressure.
Thirty plastic surgery cases were monitored (16 breast, 14 craniofacial). The average noise level was 62.89 dB, which is about 3 dB above normal conversation. This does not foster an ideal surgical environment and makes it difficult to clearly hear instructions critical to patient safety. Of our 45 survey respondents, 65% reported common miscommunication in the OR and 46% needed to repeat themselves during most operations.
The standardized location of noise level meters allowed us to determine the factors contributing to noise pollution. The area surrounding the anesthesiologist was significantly quieter than the areas surrounding the surgeon or circulator. In many ORs, anesthesia is partitioned off with a combination of machinery and drapes that reflect and absorb soundwaves.5 In contrast, the surgeon is placed in the middle of the room with no barriers. The surgery itself produces most of the noise in the OR. Suction, metal instruments, and drills all add to the constant and inherent noise pollution. Though, in several cases, the circulator’s station recorded the loudest sounds. This was often due to phone calls, closing and opening of doors, and talking amongst staff and surveyors. Music in the OR can blanket these surrounding noises; however, the value of this effect is largely dependent on surgeon preference.
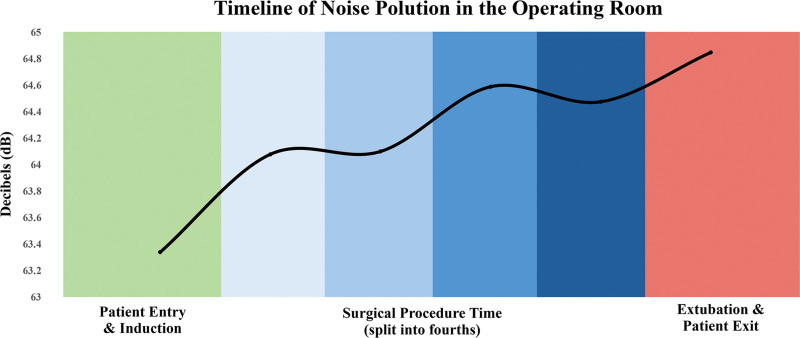
Interestingly, we found that noise in the OR intensified throughout plastic surgery procedures (Fig. 2). From patient entry to exit, there was a logarithmic increase of 1.51 dB. This equates to a 25% rise in perceived loudness. Progressive noise pollution is concerning for laxity of attention and may cause further distress to the patient during extubation.
Fig. 2.
Timeline of average noise level in the operating room from patient entry to exit. Noise, measured on a logarithmic dB scale, trends upward from 63.34 dB to 64.85 dB (R2 = 0.87). Perceived loudness increases by 25% throughout the course of the procedure.
Noise pollution in plastic surgery should no longer be ignored. The rising noise level negatively impacts communication and cohesiveness of the OR. We have begun correlating noise levels to producers of noise and the incidence of miscommunication in each case. Previous studies have shown that the best combatant of noise pollution is education of its effects on team members and patients.4
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ETHICAL APPROVAL
QI project 3797 was approved by the Quality Improvement Board at the University of Pittsburgh Medical Center.
Footnotes
Presented at the Northeastern Society of Plastic Surgeons, September 2023, Washington, D.C., and at Plastic Surgery The Meeting, October 2023, Austin, Texas.
REFERENCES
- 1.Kempen EV, Casas M, Pershagen G, et al. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15:379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wysocki AB. The effect of intermittent noise exposure on wound healing. Adv Wound Care. 1969;9:35–39. [PubMed] [Google Scholar]
- 3.Topf M, Dillion E. Noise-induced stress as a predictor of burnout in critical care nurses. Heart Lung. 1988;17:567–574. [PubMed] [Google Scholar]
- 4.Kahn DM, Cook TE, Carlisle CC, et al. Identification and modification of environmental noise in an ICU setting. Chest. 1998;114:535–540. [DOI] [PubMed] [Google Scholar]
- 5.McNeer RR, Bennett CL, Horn DB, et al. Factors affecting acoustics and speech intelligibility in the operating room: size matters. Anesth Analg. 2017;124:1978–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]