Abstract
Introduction:
Hypertrophy of adenoids is a common condition in childhood, resulting in obstructive symptoms such as sleep apnea, snoring, and rhinosinusitis. Adenotonsillectomy is recommended to improve prognosis and quality of life. This case-control study compared facial angles and lip position related to dentofacial and mouth growth in symptomatic children with adenoid hypertrophy and asymptomatic control groups.
Materials and Methods:
The study included children aged 5 to 7 who presented with obstructive symptoms and confirmed severe adenoid hypertrophy in lateral neck radiography. Standard lateral photography was taken. The Nasofacial and Nasomental angles, and upper and lower lip positions and their distance behind the Ricketts line, were measured and compared with the normal control group.
Results:
This study included 54 children with severe adenoid hypertrophy and 66 normal children. Facial angles were not significantly different between the two groups, but the mean horizontal position of the upper and lower lip in children with adenoid hypertrophy was significantly lower than in the control group (P value = 0.05). The lips were too close to the Ricketts line compared with the control group.
Conclusions:
This research demonstrates that children with severe adenoid hypertrophy have more dentofacial disorders than others. Adenotonsillectomy surgery is necessary for children with obstructive symptoms caused by tonsil enlargement, and if symptoms like snoring persist post-surgery, complementary orthodontic treatments should be considered.
Key Words: Adenoid Hypertrophy, Snoring, Adenotonsillectomy, Sleep Apnea, Facial deformity, Facial angle
Introduction
Hypertrophy of adenoids is a common finding, especially in childhood, and according to various studies, it is seen in 11 to 27 percent of children (1,2), which can be accompanied by various symptoms such as Sleep Apnea, snoring, rhinosinusitis, nocturnal enuresis, and others, all of which cause the quality of life of children and their families to decrease compared to the general population (1,3). Therefore, treatment is important in improving the prognosis and quality of life (4). Adenotonsillectomy is the simultaneous removal of palatine and pharyngeal tonsils, one of the most common surgeries performed by ear, nose, and throat specialists. Adenoid hypertrophy, due to obstruction of the respiratory tract from the nose and continuous airflow from the open mouth, leads to deformation of the palate and maxilla, especially in children in the growth stages.
This condition creates the appearance of the adenoid face, a child with an increased arch of the palate, a protruding upper jaw, and a small chin (5).
These facial changes can have a stable course and remain in children even after treatment, which creates concerns for parents (5,6). Given the changes that tonsil enlargement and mouth breathing create in dentofacial growth (7), we decided to compare the facial angles that are especially related to dentofacial and mouth growth in children with adenoid hypertrophy with an asymptomatic group in this study, considering the significant role of adenoid hypertrophy and adenotonsillectomy surgery in dentofacial growth.
Materials and Methods
This case-control study was conducted on all children aged 5 to 7 years old who presented with snoring, sleep apnea, and mouth breathing symptoms and were referred to the ear, nose, and throat clinic of 5 Azar Hospital, which confirmed adenoid hypertrophy in lateral neck radiography and had at least one year of complaints from adenoid hypertrophy problems. In the adenoid view radiography, all patients had a severe obstruction, and more than 75 percent of the nasopharynx was obstructed by severe adenoid hypertrophy, thus being considered as the case group is extra in 5 to 7-year-old (Figure 1).
Fig 1.

Lateral neck radiography shows adenoid and more than 75 percent obstruction in the nasopharynx
Children in the control group were also selected from among all 5 to 7-year-old children hospitalized in the surgery department of the hospital who were candidates for abdominal or hernia surgery and had no history of snoring, sleep apnea, and mouth breathing; they were also being examined by the same otolaryngologist and excluded from the study if they had any symptoms of high-grade palatine tonsil hypertrophy in pharynx exam or if their parents were not reliable about sleep history. Due to ethical issues, we did not perform radiography in the control group of children.
The Sony Cyber-shot DSC HX1 camera performed standard facial photography of all patients in the profile view with professional-grade wide-angle G-lens. The distances and angles of the lateral photo related to teeth, maxilla, and mandible were measured by the ImageMeter Pro software 3.8.0, and their changes were calculated between the two groups. The parameters in this study included the nasofacial and the nasomental angles and the lips’ horizontal position. The nasofacial angle is formed by the intersection of the vertical line from the glabella to the tip of the chin and the line that connects the nasion to the tip of the nose. The nasomental angle is the angle between the line that connects the nasion to the tip of the nose and the line that connects the tip of the nose to the most prominent soft tissue of the chin. The lips should be just behind this line, and the position of the upper lip should be slightly forward relative to the lower lip (Figure 2) (5,8).
Fig 2.
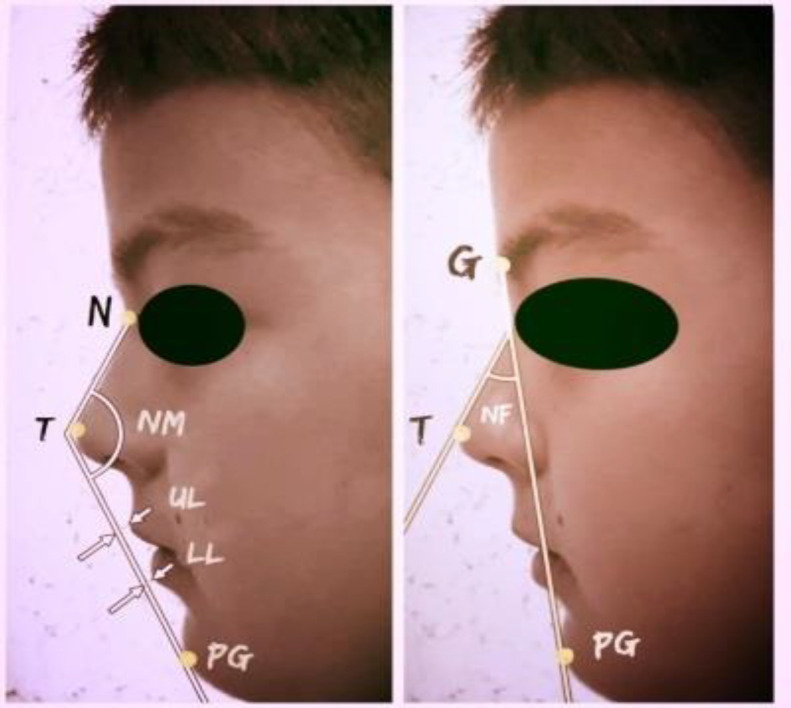
G (Glabella), T (Tip), NF (nasofacial angle), PG (Pogonion), N (Nasion), NM (Nasomental angle), UL (position of upper lip behind the Ricketts line), LL (position of lower lip behind the Ricketts line)
The normal amount of these measurements was considered 43 ± 5 degrees for the nasofacial angle and 120 ± 5 degrees for the nasomental angle, and for the position of the lips, the upper lip 4 mm and the lower lip 2 mm behind the line that connects the tip of the nose to the tip of the chin (Ricketts line) was considered normal (9). Patients with any genetic disorder that resulted in facial deformity, congenital syndromes, jaw disorders, or a history of severe trauma were excluded from the study.
Data analysis
Data were analyzed using SPSS16 software. The normality of the quantitative variables was measured by the Shapiro-Wilk test. An independent t-test was used to compare the mean of normal quantitative variables between the two groups, and for non-normal variables, the Mann-Whitney test was used. The chi-square test was also used to compare the frequency of variables between the two groups. The significance level was 0.05.
Results
In this study, 54 children aged 5 to 7 years with adenoid hypertrophy who were referred to the ear, nose, and throat clinic were entered into the study as the patient group, and 66 children hospitalized in the surgery department of the hospital who were candidates for abdominal or hernia surgery were entered into the study as the control group. All children with adenoid hypertrophy had suffered at least one to two years from the onset of their symptoms. The patient and control groups were matched in terms of age and gender. In the adenoid hypertrophy group, 63% of the children were boys, compared to 51.5% in the control group, so the gender frequency between the two groups did not have a significant statistical difference (Table 1).
Table 1.
The mean age and frequency of gender of children between the two patient and control groups
| Significance | Control | Patient | variable |
|---|---|---|---|
| Age | 5.81 | 6.31 | 0.22* |
| Boy | 34(63) | 34(51.5 | 0.37 |
| Girl | 20(37 | 32(48.5 | 0.37 |
*Mann Whitney u.
Table 2 compares the mean nasofacial and nasomental angles and the upper and lower lip horizontal position between the two groups. The mean nasofacial and nasomental angles showed no significant difference between the two groups. However, the mean horizontal position of the upper and lower lip in the children with adenoid hypertrophy was significantly lower than in the control group.
Table 2.
Comparison of NF and NM angles and horizontal lip position between the two case and control groups.
| variable | group | mean | significance |
|---|---|---|---|
| NFA | patient | 0.59* | |
| control | |||
| NMA | patient | 0.27** | |
| control | |||
| ULD | patient | 0.41 | 0.001* |
| control | 2.09 | ||
| LLD | patient | 0.001* | |
| control |
NFA: Nasofacial Angle, NMA: Nasomental Angle, ULD: Upper Lip Distance, LLD: Lower Lip Distance, angle degree, mm: millimeter, sd: Standard deviation. *Mann Whitney u **independent t-test
Discussion
Tonsils have a special immune defense function. They send immunologically marked lymphocytes and immunoglobulins to the immune system against bacterial organisms. Since the tonsils are located in a narrow region of the respiratory and digestive systems in the oropharynx and nasopharynx, their increase in volume, known as adenotonsillar hypertrophy, leads to narrowing the diameter of this vital pathway and disrupting the respiratory system, necessitating their removal (10).
Adenotonsillectomy is a surgical process in which the palatine tonsils are completely removed along with their capsule, and the adenoid is removed from the posterior wall of the nasopharynx (11). One of the most important indications for this surgery is obstructive causes, which include snoring, chronic mouth breathing, and obstructive sleep apnea. These obstructive issues are caused by tonsil enlargement, especially pharyngeal tonsils or adenoids, and nasopharyngeal obstruction (12,13).
Craniofacial morphology is a risk factor for sleep apnea in children, and a small maxilla or mandible predisposes the child to snoring or sleep apnea (14). On the other hand, this lymphoid tissue, seen in the upper part of the airway in children, leads to degrees of airway obstruction. Although their size and degrees of obstruction decrease over time, the obstruction caused by this tissue leads to changes in the craniofacial structure in children (15,16). Adenoid hypertrophy causes a downward position of the tongue and mandible and an extended head position, which can result in a retrognathic mandible. Moreover, nasal obstruction due to adenoid hypertrophy leads to mouth opening and lack of negative pressure in the nasal cavity, and it prevents the descent of the palatal vault due to internal pressure of the muscles on the maxillary arches. The result of all these changes is the creation of a long face and arched palate. Consequently, the growth of the maxilla is limited in the transverse section and even more so in the vertical section, leading to a high-arched palate (17-20).
All these changes following upper airway obstruction contribute to malocclusion. The incidence of malocclusion in patients with adenotonsillar hypertrophy due to airway stenosis has been reported to be higher than in the normal population (21-23). Additionally, malocclusion was higher in patients with enlargement of both adenoid and palatine tonsils compared to those with adenoid hypertrophy alone (24,25). However, some studies using radiographic methods with cephalometric analysis have rejected this hypothesis, showing that the change in the diameter of the nasopharyngeal airway does not significantly affect the anteroposterior position of the maxilla and mandible and the amount of malocclusion in patients with large adenoids was not higher (26,27).
In our study, all children in the case group had severe adenoid hypertrophy and obstruction of more than 75 percent of the nasopharynx, with or without palatine tonsil enlargement. The case and control groups were matched in age, and since the adenoid reaches its maximum size at six years old (27), all children in the study were aged 5 to 7 years to evaluate them during the peak period of adenoid enlargement issues. Regarding gender, preschool children do not differ in the size of the facial angles measured (9), and the two groups were also matched in gender. Given the disagreement in various studies about the relationship between malocclusion and adenoid enlargement, we decided to evaluate the situation of the upper and lower jaw based on the analysis of facial angles rather than radiographic cephalometry. The facial angles in the photographic lateral profile view, including nasofacial and nasomental angles, showed changes in the adenoid hypertrophy group compared to the control group. Although these changes were not statistically significant as expected, the nasofacial angle in the adenoid hypertrophy group was higher (28). The nasomental angle, crucial in evaluating the maxilla and mandible, was reduced in case groups. These two angles are important in assessing patients with malocclusion, especially in patients with malocclusion class 2, which showed similar changes to our study (28,29).
One of the most important landmarks in evaluating the jaw situation is the position of the lips in the lateral profile view and their distance from the Ricketts line. The Ricketts line connects the tip of the nose to the anterior part of the soft tissue of the chin in the lateral profile view, and the lips should be slightly behind this line. In adults, this distance is 3 to 4 mm for the upper lip and 2 mm for the lower lip (29). Although no study has specifically evaluated this distance in children, the control group in our study, who had no symptoms of upper airway obstruction or maxilla and mandible deformity, showed an upper lip distance of 2.09 ± 1.97 mm and a lower lip distance of 1.30 ± 1.51 mm from the Ricketts line. However, this distance was reduced in the adenoid hypertrophy group (0.41 ± 1.62 for the upper lip and 0.04 ± 1.28 for the lower lip), and this reduction was statistically significant compared to the control group. Notably, no specific reports based on facial angles from lateral photography in children with adenoid hypertrophy exist, as studies have mostly focused on radiography and cephalometry analysis. Nevertheless, the above findings are expected in patients with malocclusion class 2, characterized by protruded upper incisors and retracted mandible, which are more common in children with adenoid hypertrophy (30,31). The common finding in our study was the very close distance of this line with the upper and lower lips (Figure 3).
Fig 3.
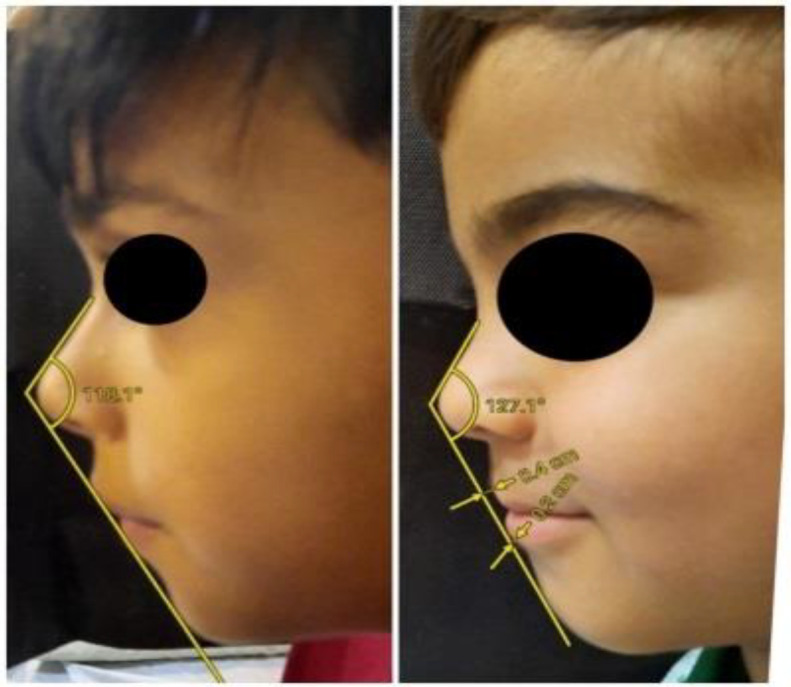
The position of the upper and lower lips
The image on the right shows a child with a normal airway without adenotonsillar hypertrophy. The position of the lips, maxilla, mandible, and chin relative to the Ricketts line is within the normal range. However, in the picture on the left, which shows a child with severe adenoid hypertrophy, the nasomental angle is smaller than others, and the lips are too close to the line, resulting from excessive vertical growth of the maxilla and retrognathic mandible.
Adenotonsillectomy surgery alleviates many symptoms in children with adenotonsillar hypertrophy, including snoring, mouth breathing, sleep apnea, and daytime insomnia, significantly impacting their quality of life (32). However, symptoms such as mouth breathing and snoring may persist post-surgery, possibly due to changes in dentofacial growth caused by upper airway obstruction (33). The changes such as V-shaped narrowing in the maxillary arch and adenoid faces like macroglossia, open mouth posture, anterior and lower tongue position, the retrognathic position of the mandible, the prominent position of maxillary anterior teeth, and retracted position of mandibular anterior teeth may remain after treatment. Early diagnosis and treatment of children with increased upper airway resistance are essential, considering that 80 to 90 percent of craniofacial growth is completed by the age of 12. In cases where changes in the mandible and maxilla occur following adenotonsillar enlargement, adenotonsillectomy surgery alone may be insufficient to improve these changes, and orthodontic treatments may be required to address the dentofacial issues (33,34). Contrary to most studies, Lena et al. found significant improvement in the sizes and angles of the dentofacial features in the lateral cephalogram of children one year after adenotonsillectomy surgery (35).
Belo Horizonte and colleagues also observed that children who underwent surgery had better intercanine and intermolar growth in the maxilla over time than those awaiting surgery for obstructive symptoms, including mouth breathing. Also, the palatal arch in symptomatic children without surgery was deeper (20).
One effective orthodontic treatment for improving symptoms of OSA in children is rapid maxillary expansion (RME) surgery, which improves the enlarged palatal arch and apnea-hypopnea index (AHI). Devices such as the mandibular advancement device (MAD) also mechanically advance the mandible, preventing tongue collapse and airway obstruction during sleep. These treatments are recommended to be considered after adenotonsillectomy surgery and in cases of severe sleep apnea unresponsive to initial treatments (36, 37).
However, we have some limitations regarding the sample size of both groups and the need for more sufficient studies based on facial photography. On the other hand, it would be better and more accurate if children’s facial angles were compared in both the case and control groups at a specific age with more angles, even in frontal view. In addition, we can compare children’s facial angles after surgery and determine the effect of surgery on their facial analysis.
Conclusions
Adenoid hypertrophy, which causes upper airway and nasopharynx obstruction, affects changes in the dentofacial system. These changes may create malocclusion and may remain even after surgery. Adenotonsillectomy is crucial for preventing these changes in children with severe adenoid hypertrophy. After surgery, children who experience changes in the mandible and maxilla may need complementary orthodontic treatments.
Acknowledgements
We thank M. Savar for assistance with the experiments and M. Taziki for valuable discussion.
Ethics
This study was approved by Golestan University of Medical Science and has an Ethic Committee License. All children’s parents were informed about the purpose of the research, and their consent for cooperation was obtained. No individual was forced to participate in the study. Therefore, standard facial photography was performed, which had no harmful effect on the health of the children under study.
Financial disclosure statement:
This research received no specific grant from public, commercial, or not-for-profit sector funding agencies …
Declaration of competing interest:
None
References
- 1.Aydin S, Sanli A, Celebi O, Taşdemir Ö, Paksoy M, Eken M, et al. Prevalence of adenoid hypertrophy and nocturnal enuresis in primary school children in Istanbul, Turkey. Int J Pediatr Otorhinolaryngol. 2008 May;72(5):665. doi: 10.1016/j.ijporl.2008.01.028. [DOI] [PubMed] [Google Scholar]
- 2.Kara CO, Ergin H, Koçak G, Kiliç İ, Yurdakul M. Prevalence of tonsillar hypertrophy and associated oropharyngeal symptoms in primary school children in Denizli, Turkey. Int J Pediatr Otorhinolaryngol 2002Nov. 66(2):175–179. doi: 10.1016/s0165-5876(02)00247-1. [DOI] [PubMed] [Google Scholar]
- 3.Tuncer Ü, Aydogan B, Soylu L, Simsek M, Akcali C, Kucukcan A. Chronic rhinosinusitis and adenoid hypertrophy in children. Am J Otolaryngol. 2004 Jan;25(1):5–10. doi: 10.1016/j.amjoto.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Havas T, Lowinger D. Obstructive adenoid tissue: an indication for powered-shaver adenoidectomy. Arch Otolaryngol Head Neck Surg . 2002 Jul;128(7):789–91. doi: 10.1001/archotol.128.7.789. [DOI] [PubMed] [Google Scholar]
- 5.Koca CF, Erdem T, Bayindir T. The effect of adenoid hypertrophy on maxillofacial development: an objective photographic analysis. J Otolaryngol Head Neck Surg. 2016 Sep;45(1) doi: 10.1186/s40463-016-0161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niedzielski A, Chmielik LP, Mielnik-Niedzielska G, Kasprzyk A, Boguslawska J. Adenoid hypertrophy in children: a narrative review of pathogenesis and clinical relevance. BMJ Paediatr Open 2023Apr. 7(1):e001710. doi: 10.1136/bmjpo-2022-001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin L, Zhao T, Qin D, Hua F, He H. The impact of mouth breathing on dentofacial development: A concise review. Front Public Health. 2022 Sep;: 929165. doi: 10.3389/fpubh.2022.929165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasinato R, Mocellin M, Arantes MC, Coelho MS, Dall'Igna DP, Soccol AT. Pre and Post Operative Facial Angles in Patients Submitted to Rhinoplasty. Int Arch Otorhinolaryngol. 2008 Jul;12(3):393–396. [Google Scholar]
- 9.Gautam B, Sreedharan S, Seetha SM. Photographic Profile Analysis in Preschool Children of Thiruvananthapuram, Kerala. Int J Clin Pediatr Dent. 2019 Mar;12(2):111–115. doi: 10.5005/jp-journals-10005-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alzahrani HA, Alkhaldi RO, Alsufyani DH, Alghamdi SA, Althobity TA, Fageeh YA. Adenoid Hypertrophy and Orthodontic Complications: An Assessment of Parental Knowledge in Saudi Arabia. Cureus. 2023 Jul;15(7) doi: 10.7759/cureus.41692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Luca Canto G, Pachêco-Pereira C, Aydinoz S, Bhattacharjee R, Tan HL, Kheirandish-Gozal L, et al. Adenotonsillectomy Complications: A Meta-analysis. Pediatrics. 2015 Oct;136(4):702–718. doi: 10.1542/peds.2015-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Randall DA. Current Indications for Tonsillectomy and Adenoidectomy. J Am Board Fam Med. 2020 Nov-Dec;33(6):1025–1030. doi: 10.3122/jabfm.2020.06.200038. [DOI] [PubMed] [Google Scholar]
- 13.Nosetti L, Zucconi M, De Bernardi di Valserra F, Simoncini D, Beretta G, Guacci P, et al. Exploring the Intricate Links between Adenotonsillar Hypertrophy, Mouth Breathing, and Craniofacial Development in Children with Sleep-Disordered Breathing: Unraveling the Vicious Cycle. Children (Basel) 2023 Aug;10:8. doi: 10.3390/children10081426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bariani RCB, Bigliazzi R, Badreddine FR, Yamamoto LH, Tufik S, Moreira GA, et al. A clinical trial on 3D CT scan and polysomnographyc changes after rapid maxillary expansion in children with snoring. Braz J Otorhinolaryngol. 2022 Nov-Dec;88(suppl 5):S162–S170. doi: 10.1016/j.bjorl.2022.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang X, Gong X, Gao X. Age-related hypertrophy of adenoid and tonsil with its relationship with craniofacial morphology. BMC Pediatr . 2023 Apr;23(1):163. doi: 10.1186/s12887-023-03979-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berjis N, Sonbolastan M, Jabbarifar E, Farokh K. Evaluation the Effects of Adenoidal Hypertrophy on Occlusion and Indexes of Face and Jaw in 6 - 12 Years Old Children. Shiraz E-Med J. 2006;6(3-4):e32896. [Google Scholar]
- 17.Zucconi M, Caprioglio A, Calori G, Ferini-Strambi L, Oldani A, Castronovo C, et al. Craniofacial modifications in children with habitual snoring and obstructive sleep apnoea: a case-control study. Eur Respir J. 1999 Feb;13(2):411–7. doi: 10.1183/09031936.99.13241199. [DOI] [PubMed] [Google Scholar]
- 18.Baroni M, Ballanti F, Franchi L, Cozza P. Craniofacial features of subjects with adenoid, tonsillar, or adenotonsillar hypertrophy. Prog Orthod. 2011;12(1):38–44. doi: 10.1016/j.pio.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Pawłowska-Seredyńska K, Umławska W, Resler K, Morawska-Kochman M, Pazdro-Zastawny K, Krecicki T. Craniofacial Proportions in Children with Adenoid or Adenotonsillar Hypertrophy Are Related to Disease Duration and Nasopharyngeal Obstruction. Int J Pediatr Otorhinolaryngol. 2020;132:109911. doi: 10.1016/j.ijporl.2020.109911. [DOI] [PubMed] [Google Scholar]
- 20.Petraccone Caixeta AC, Andrade I Jr, Bahia Junqueira Pereira T, Franco LP, Gonçalves Becker HM, Souki BQ. Dental arch dimensional changes after adenotonsillectomy in prepubertal children. Am J Orthod Dentofacial Orthop. 2014;145(4):461–8. doi: 10.1016/j.ajodo.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Mergen DC, Jacobs RM. The Size of Nasopharynx Associated with Normal Occlusion and Class II Malocclusion. Angle Orthodontist . 2009 Jul;40(4):342–6. doi: 10.1043/0003-3219(1970)040<0342:TSONAW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Mlynarek A, Tewfik MA, Hagr A, Manoukian JJ, Schloss MD, Tewfik TL, et al. Lateral neck radiography versus direct video rhinoscopy in assessing adenoid size. J Otolaryngol. 2004 Dec;33(6):360–5. doi: 10.2310/7070.2004.03074. [DOI] [PubMed] [Google Scholar]
- 23.Neuppnnann Feres MF, Hermann JS, Sallum AC, Pignatari SSN. Endoscopic Evaluation of Adenoids: Reproducibility Analysis of Current Methods. Clin Exp Otorhinolaryngol. 2013 Mar;6(1):36–40. doi: 10.3342/ceo.2013.6.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Freitas MR, Virmond Alcazar NMP, Janson G, de Freitas KMS, Henriques JFC. Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns. Am J Orthod Dentofacial Orthop . 2006 Dec;130(6):742–5. doi: 10.1016/j.ajodo.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 25.Nunes WR Jr, Di Francesco RC. Variation of Patterns of Malocclusion by Site of Pharyngeal Obstruction in Children. Arch Otolaryngol Head Neck Surg. 2010 Nov;136(11):1116–20. doi: 10.1001/archoto.2010.187. [DOI] [PubMed] [Google Scholar]
- 26.Feres MFN, Muniz TS, de Andrade SH, Lemos Mde M, Pignatari SSN. Craniofacial skeletal pattern: is it really correlated with the degree of adenoid obstruction? Dental Press J Orthod. 2015 Jul-Aug;20(4):68–75. doi: 10.1590/2176-9451.20.4.068-075.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jana M, Gupta AK. Novel Use of Ultrasound in Evaluation of Adenoid Hypertrophy in Children. Indian J Pediatr. 2020 Nov;87(11):885–886. doi: 10.1007/s12098-020-03487-6. [DOI] [PubMed] [Google Scholar]
- 28.Rathi S, Gilani R, Kamble R, Vishnani R. Analysis of Nasal Morphology in Skeletal Class I and Skeletal Class II Malocclusion: An Observational Study. Cureus. 2022;14(9):e29584. doi: 10.7759/cureus.29584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perović T. The Influence of Class II Division 2 Malocclusions on the Harmony of the Human Face Profile. Med Sci Monit. 2017 Nov;23: 5589–5598. doi: 10.12659/MSM.905453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McIntyre GT, Millett DT. Lip shape and position in Class II division 2 malocclusion. Angle Orthod. 2006 Sep;76(5):739–44. doi: 10.1043/0003-3219(2006)076[0739:LSAPIC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Osiatuma VI, Otuyemi OD, Kolawole KA, Ogunbanjo BO, Amusa YB. Occlusal characteristics of children with hypertrophied adenoids in Nigeria. Int Orthod. 2015 Mar;13(1):26–42. doi: 10.1016/j.ortho.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 32.Orji FT, Ezeanolue BC. Outcome of Adenotonsillectomy for Sleep and Breathing Difficulties in Nigerian Children with Obstructive Adenotonsillar Enlargement. Indian J Otolaryngol Head Neck Surg. 2012 Jun;64(2):131–6. doi: 10.1007/s12070-012-0517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.İnönü-Sakallı N, Sakalli C, Tosun Ö, Akşit-Bıçak D. Comparative Evaluation of the Effects of Adenotonsillar Hypertrophy on Oral Health in Children. Biomed Res Int. 2021 Apr2;2021:5550267. doi: 10.1155/2021/5550267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bucci R, Rongo R, Zunino B, Michelotti A, Bucci P, Alessandri-Bonetti G, et al. Effect of orthopedic and functional orthodontic treatment in children with obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2023 Feb;67:101730. doi: 10.1016/j.smrv.2022.101730. [DOI] [PubMed] [Google Scholar]
- 35.Zettergren-Wijk L, Forsberg CM, Linder-Aronson S. Changes in dentofacial morphology after adeno-/tonsillectomy in young children with obstructive sleep apnoea--a 5-year follow-up study. Eur J Orthod. 2006 Aug;28(4):319–26. doi: 10.1093/ejo/cji119. [DOI] [PubMed] [Google Scholar]
- 36.Xie B, Zhang L, Lu Y. The role of rapid maxillary expansion in pediatric obstructive sleep apnea: Efficacy, mechanism and multidisciplinary collaboration. Sleep Med Rev. 2023 Feb;67:101733. doi: 10.1016/j.smrv.2022.101733. [DOI] [PubMed] [Google Scholar]
- 37.Li Y, Lu Y, Li X, Zhao L, Guo J, Yu L, et al. Efficacy of orthodontic treatment versus adenotonsillectomy in children with moderate obstructive sleep apnoea and mandibular retrognathia: study design and protocol for a non-inferiority randomised controlled trial. BMJ Open. 2022 Apr;12(4):e055964. doi: 10.1136/bmjopen-2021-055964. [DOI] [PMC free article] [PubMed] [Google Scholar]


