Abstract
This preliminary investigation compares peripheral blood cell counts including red blood cells (RBCs), white blood cells (WBCs), neutrophils, peripheral blood lymphocytes (PBLs), CD4+, CD8+ and CD16+ lymphocytes, CD4+/CD8+ ratio, hematocrit, humoral parameters including serum interferon-γ and interleukin-6, salivary secretory immunoglobulin A (IgA). Psychological measures including the State–Trait Anxiety Inventory (STAI) questionnaire and the Self-rating Depression Scale (SDS) between recipients (n = 11) of carrier oil massage and aromatherapy massage, which includes sweet almond oil, lavender oil, cypress oil and sweet marjoram oil. Though both STAI and SDS showed a significant reduction (P < 0.01) after treatment with aromatherapy and carrier massage, no difference between the aromatherapy and control massage was observed for STAI and SDS. Aromatherapy, in contrast to control massage, did not significantly reduce RBC count or hematocrit. However, aromatherapy massage showed a significant (P > 0.05) increase in PBLs, possibly due to an increase in CD8+ and CD16+ lymphocytes, which had significantly increased post-treatment (P < 0.01). Consequently, the CD4+/CD8+ ratio decreased significantly (P < 0.01). The paucity of such differences after carrier oil massage suggests that aromatherapy massage could be beneficial in disease states that require augmentation of CD8+ lymphocytes. While this study identifies the immunological benefits of aromatherapy massage, there is a need to validate the findings prospectively in a larger cohort of patients.
Keywords: anxiety, aromatherapy, immune function, massage
Introduction
Aromatherapy is the use of essential oils, the pure volatile portion of aromatic plant products normally extracted by distillation, for therapeutic or medical purposes. Essential oils encompass >60 kinds of herbal oils (1) that are used to ease aches, pains and injuries (2–4). Aromatherapy also acts on the central nervous system, relieving depression and anxiety, reducing stress, relaxing, sedating or stimulating, and restoring both physical and emotional well-being (5–7).
Several basic research studies and clinical trials examining the effectiveness of the therapy have been published recently. The antimicrobial properties of aromatherapy have been studied most actively. The in vitro results of the effects of essential oils on methicillin-resistant Staphylococcus aureus (MRSA) (8,9), Helicobacter pylori (10), Candida albicans infection (11), and so forth have been reported. Phase I clinical trials have been done on inhibition of oral plaque formation (12), MRSA infection (13) and interdigital tinea pedis (14). Furthermore, clinical trials of aromatherapy on pruritus in patients undergoing hemodialysis (15) and on agitated behavior in dementia patients have also been reported (16,17).
Another popular application of aromatherapy is to reduce anxiety, promote relaxation and increase well-being of patients in palliative care or intensive care units, patients undergoing abortion or hemodialysis, and so forth (7,18–22). Cooke and Ernst reviewed six randomized clinical trials to study the results of aromatherapy massage, concluding that aromatherapy appeared to have at least a transient ability to reduce anxiety, but there was no evidence of lasting benefit (23). There have been reports on the influence of massage on the immune functions of human immune deficiency (HIV)-positive patients (9,24,25). Based on these studies, we hypothesize that aromatherapy massage may influence the cellular and humoral compartments of the immune function in both normal and pathological states.
In this investigation, our objective was to examine and compare the cellular immune parameters such as white blood cells (WBCs), peripheral blood lymphocytes (PBLs), neutrophils, CD4+, CD8+ and CD16+ lymphocytes, CD4+/CD8+ ratio, humoral parameters including serum interferon-γ (IFN-γ) and interleukin-6 (IL-6), including salivary secretory immunoglobulin A (s-IgA) and psychological parameters including the State–Trait Anxiety Inventory (STAI) and Self-rating Depression Scale (SDS) of healthy recipients who received conventional sweet almond oil massage and those who received aromatherapy massage, which combined lavender oil, cypress oil and sweet marjoram oil in sweet almond oil.
Methods
Subjects
This study was performed between August and December 2002. We recruited 11 volunteers (Table 1) from employees and students of Kyoto Prefectural University of Medicine and their relatives for our study. This study was conducted after obtaining approval from the Ethics Committee of Kyoto Prefectural University of Medicine. We gave detailed explanations of the project to each subject and all subjects signed informed consent forms prior to participating. Prior to participation, all subjects were asked if they had any medical treatment or daily medication and confirmed that they were healthy and did not take any daily medication. Then, we performed a 15 min closed skin patch test with blended oil used in this study on the forearms of subjects to confirm that they did not have an acute reaction to the oil.
Table 1.
Subject characteristics
| Number | 11 |
| Gender | 9 males, 2 females |
| Age range (years) | 28–37 |
| Median age (years) | 32 |
Essential Oils
Sweet almond oil (Prunus dulcis) was purchased from Meadows (Canterbury, UK). Tea tree oil (Melaleuca alternifolia) (Lot No. LF2090298), lavender oil (Lavandula angustifolia) (Lot No. LF2190418), cypress oil (Cupressus sempervirens) (Lot No. LF2090220) and sweet marjoram oil (Origanum majorana) (Lot No. LF2060129) were purchased from Laboratoire Sanoflore (Gigore-et-Lozeron, France). Tea tree oil was used for a foot bath and the other three oils were used for aromatherapy massage. We chose these oils for their relaxing effect on healthy subjects and for the balance of the fragrance. Lavender oil is one of the most famous essential oils and its sedative quality is often used for managing stress (1,6). Sweet marjoram oil and cypress oil are also known to reduce anxiety and fatigue (1). Table 2 shows an analysis report with the major chemical composition for the lots of essential oils used in this study.
Table 2.
Major chemical constituents of the essential oils used in our study
| Lavender oil | |
| Linalool | 36.31% |
| Linalyl acetate | 34.05% |
| Cis-β-ocimene | 3.50% |
| Trans-β-ocimene | 2.32% |
| Lavendulyl acetate | 2.12% |
| Cypress oil | |
| α-Pinene | 61.85% |
| σ-Carene | 15.2% |
| Terpinene | 2.36% |
| Mycene | 2.27% |
| Limonene | 2.17% |
| Sweet marjoram oil | |
| Terpinen-4-ol | 21.26% |
| γ-Terpinene | 13.46% |
| Trans-thujanol | 11.43% |
| Linalyl acetate | 4.28% |
| Terpinolene | 4.18% |
| Cis-thujanol | 2.83% |
| β-Caryophyllene | 2.54% |
| Tea tree oil | |
| Terpinen-4-ol | 37.90% |
| γ-Terpinene | 21.50% |
| α-Terpinene | 10.20% |
| Terpinolene | 3.60% |
| 1.8 Cineole | 3.30% |
| Paracimene | 2.80% |
| α-Pinene | 2.70% |
| α-Terpineol | 2.70% |
Psychological Tests
We evaluated the psychological response using the STAI and SDS.
Procedure
First, subjects filled out the psychological test forms. Blood was drawn and saliva was collected. The physiological response upon brief psychological stress was monitored. Subjects were seated in a reclining seat and allowed to rest for 2 min. Then they performed a serial subtraction task for 2 min, and rested again for 2 min while we monitored their palmer Galvanic skin response (GSR), finger skin temperature and finger plethysmogram amplitude using a biofeedback system (Multitrace Biofeedback, Thort Technology, USA). After that, they took a footbath at 42°C for 5 min with one drop of tea tree oil and received a 30 min aromatherapy massage or control massage. Then, the physiological response upon brief psychological stress was monitored and they filled out STAI and SDS forms again. Their blood was drawn and saliva was collected again. All subjects received both an aromatherapy massage and a carrier oil control massage at an interval of at least 2 weeks. The first five subjects received the aromatherapy massage before the carrier oil massage. The other six subjects received the carrier oil massage first.
Massage Procedure
Each subject received the same standardized massage of the back, shoulders, arms, hands, lower legs and feet with or without essential oils for ∼30 min by the same skilled therapist. For the aromatherapy massage, 10–15 ml of sweet almond oil containing 0.15 ml of lavender oil, 0.1 ml of sweet marjoram oil and 0.05 ml of cypress oil was used. For the control massage, only sweet almond oil was used.
Methods for Immune Measurements
Blood cell counts including numbers and proportions of leukocytes were examined at the Central Laboratory Unit of Kyoto Prefectural University of Medicine. A 2 ml aliquot of the heparinized blood samples was used to determine the levels of various lymphocyte subsets. Mononuclear cells were isolated by Ficoll-Paque™ PLUS (Amersham Biosciences AB, Sweden) gradient centrifugation. Lymphocyte subsets were identified by fluorescence activated cell sorting (FACS) analysis (FACS Caliber, Becton, Dickinson and Company, Franklin Lakes, NJ) using fluorecein isothiocyanate (FITC)–CD16, phycoerythrin (PE)–CD8 and FITC–CD4 antibodies (Becton, Dickinson and Company). Serum samples were stored at −80°C until serum IFN-γ and IL-6 concentrations were analyzed with enzyme-linked immunosorbent assay (ELISA) kits (Pierce Biotechnology, Rockford, IL). Serum cortisol level was measured with chemiluminescence immunosorbent assays (CLIAs; BML, Inc., Tokyo, Japan).
Saliva samples were collected before and after the massage using saliva collection test tubes (Salivette®, Sarstedt, Nümbrecht, Germany). The saliva was stored at −80°C in a freezer until the s-IgA concentration was assayed using a EIA s-IgA test (Medical & Biological Laboratories Co., Ltd, Nagoya, Japan) following the manufacturer's instructions.
Statistical Analysis
Since blood cell counts may change due to hemodilution or hemoconcentration caused by massage, the cell counts measured after the massage were calibrated as if hematocrit values after the massage were the same as those before the massage.
The differences in data between pre- and post-massage sessions were examined using a paired t-test, and the results of aromatherapy and control massage were mutually examined using the two-way analysis of variance (ANOVA). All statistical analyses were conducted using SPSS software (Base 10.0J). A P-value < 0.05 was considered statistically significant.
Results
Psychological Response to Treatment
Psychological responses to treatment were assessed as changes in anxiety and depression according to the STAI and SDS results. State anxiety scores from the STAI were significantly reduced after both aromatherapy massage and control massage compared with the baseline obtained before the massage. The mean state anxiety score dropped from 41.2 to 34.1 (P = 0.0084) after aromatherapy massage and from 42.0 to 34.0 (P = 0.0064) after control massage (Table 3).
Table 3.
Psychological measures
| STAI (trait-anxiety) | STAI (state-anxiety) | SDS | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | ||||
| Aromatherapy massage | |||||||||
| Mean | 41.4 | 39.4 | 41.2 | 34.1 | 37 | 37.6 | |||
| P-value | 0.21 | 0.0084 | 0.52 | ||||||
| Carrier oil massage | |||||||||
| Mean | 43 | 41 | 42 | 34 | 36 | 37 | |||
| P-value | 0.22 | 0.0064 | 0.3 | ||||||
The SDS score did not change before and after either aromatherapy massage or control massage (P = 0.52 and P = 0.30, Table 3).
Hematological Measures
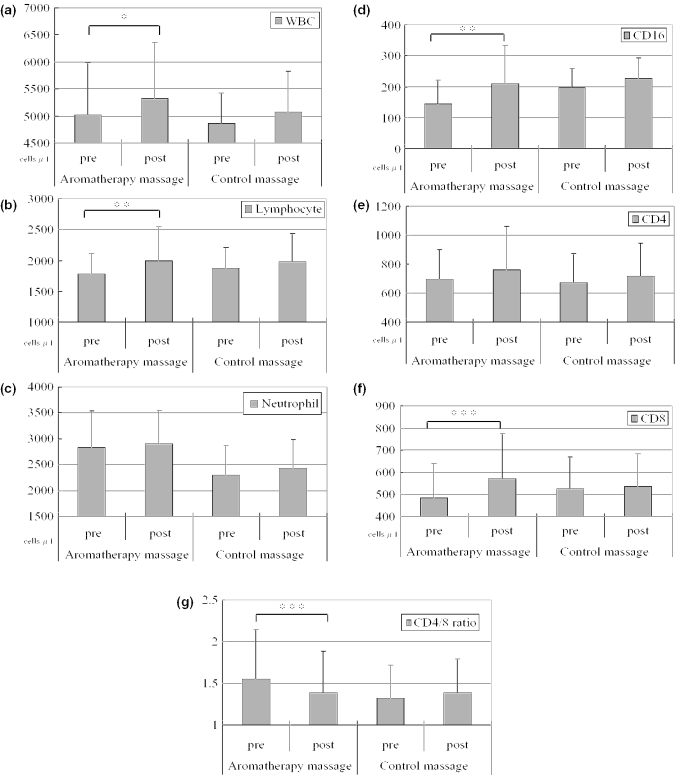
Hematocrit and red blood cell (RBC) counts were significantly decreased following control massage therapy (P = 0.0057), but not after aromatherapy massage (P = 0.37) (Table 4). The numbers of lymphocytes, CD8+ cells and CD16+ cells significantly increased after the aromatherapy massage (P < 0.05, P < 0.01 and P < 0.05, respectively), but not after the control massage (P = 0.17, P = 0.70 and P = 0.17, respectively) (Table 5 and Figure 1).
Table 4.
Changes in RBCs and hematocrit after massage
| Pre-massage mean | Post-massage mean | P-value | |
|---|---|---|---|
| Aromatherapy massage | |||
| RBC (cells/ml) | 5.01 × 106 | 5.06 × 106 | 0.59 |
| Hct (%) | 42 | 41.7 | 0.37 |
| Control massage | |||
| RBC (cells/ml) | 4.74 × 106 | 4.69 × 106 | 0.058 |
| Hct (%) | 42.75 | 42.05 | 0.0057 |
Hct = hematocrit.
Table 5.
Changes in immunological measures after aromatherapy massage and control massage
| Blood cell count (cells per μl) | Aromatherapy massage | Control massage | ||||
|---|---|---|---|---|---|---|
| Pre-, mean (SD) | Post-, mean (SD) | P-value | Pre-, mean (SD) | Post-, mean (SD) | P-value | |
| WBCs | 5020 (959) | 5322 (1036) | 0.057 | 4866 (556) | 5072 (753) | 0.12 |
| Lymphocytes | 1772 (344) | 1988 (556) | 0.035 | 1872 (330) | 1983 (449) | 0.17 |
| Neutrophils | 2835 (706) | 2907 (639) | 0.509 | 2302 (563) | 2426 (554) | 0.11 |
| CD16 | 143 (79) | 209 (126) | 0.021 | 197 (61) | 226 (67) | 0.26 |
| CD4 | 696 (205) | 759 (303) | 0.191 | 670 (204) | 718 (227) | 0.7 |
| CD8 | 483 (160) | 572 (201) | 0.008 | 527 (141) | 538 (146) | 0.17 |
| CD4/8 ratio | 1.55 (0.6) | 1.39 (0.5) | 0.01 | 1.32 (0.4) | 1.39 (0.4) | 0.14 |
Post-test values were calibrated for the hematocrit.
Figure 1.
Changes in immunological measures after aromatherapy massage and control massage. Bars represent numbers of (a) WBCs, (b) PBLs, (c) neutrophils, (d) CD16+ cells, (e) CD4+ cells, and (f) CD8+ cells and (g) CD4+/CD8+ ratio before and after aromatherapy massage or control massage. (n = 11) * P = 0.05, compared them before and after treatment, **P < 0.05, compared them before and after treatment, *** P < 0.05, compared them before and after treatment. Error bars show standard deviation.
In the next stage, we examined the influence of aromatherapy and massage on hematocrit, and lymphocyte, CD8+ and CD16+ cell counts using two-way ANOVA. The main effects of aromatherapy were not significant for hematocrit, and lymphocyte, CD8+ cell and CD16+ cell counts (P = 0.45, P = 0.90, P = 0.18 and P = 0.12, respectively). The main effects of massage were significant for hematocrit, and lymphocyte and CD16+ cell counts (P = 0.038, P = 0.042 and P = 0.028, respectively), and of borderline significance for CD8+ cell counts (P = 0.055). A positive interaction between aromatherapy and massage was significantly detected for CD8+ cell counts (P = 0.023), i.e. the increase in CD8+ cell counts after aromatherapy massage was significantly larger than the change in the cell counts after control massage. The interactions for hematocrit, and lymphocyte and CD16+ cell counts were not significant (P = 0.37, P = 0.24 and P = 0.14, respectively).
Examinations of serum IL-6, IFn-γ and saliva s-IgA showed that concentrations of IFN-γ were below the detectable limit (10 pg/ml) in all samples. No significant changes were found in concentrations of serum IL-6 and saliva s-IgA when values obtained before both types of massage were compared with those after massage (data not shown).
Additionally, we examined serum cortisol levels before and after aromatherapy and control massage. Serum cortisol levels were significantly decreased after the aromatherapy massage (P < 0.05), but not after the control massage (P = 0.36, Table 6). We further analyzed the data with two-way ANOVA and discovered that although massage had a significant influence (P = 0.038), aromatherapy itself and the interaction between aromatherapy and massage did not significantly influence (P = 0.73 and P = 0.20) serum cortisol levels.
Table 6.
Changes in plasma cortisol levels after aromatherapy massage and control massage
| Aromatherapy massage | Control massage | ||||
|---|---|---|---|---|---|
| Pre-, mean (SD) | Post-, mean (SD) | P-value | Pre-, mean (SD) | Post-, mean (SD) | P-value |
| 10.5 (3.5) | 7.6 (2.4) | 0.02 | 9.5 (3.0) | 9.1 (4.2) | 0.36 |
Physiological Response upon Brief Psychological Stress
GSR, finger skin temperature and finger plethysmogram amplitude as physiological responses were monitored upon brief psychological stress before and after the session. Although there were variations among individuals, most subjects showed an increase in GSR, and a decrease in finger skin temperature and finger plethysmogram amplitude during psychological stress. We did not find any statistical difference, however, in the rate of change in the three variables when we compared them before and after massage (data not shown).
Discussion
This preliminary investigation revealed that both aromatherapy and control massage were beneficial for inducing relaxation by decreasing state anxiety levels. Even though trait anxiety scores did not change, state anxiety scores were lowered significantly, This is because the ‘state anxiety’ score represents a temporary condition that changes every moment, while the ‘trait anxiety’ score represents a more general and long-standing quality of anxiety. However, we did not observe any difference between aromatherapy and control massage.
As in the present study, STAI has also failed to detect any difference in psychological results between aromatherapy massage and control massage in other studies. To compare the extent of relaxation after massage and aromatherapy massage in future studies, it might be useful to apply other measurements such as the Rotterdam Symptom Checklist (RSCL), which has demonstrated differences in the psychological and physiological functions of the two types of massage (22). Furthermore, we did not observe any change of SDS scores before and after massage. This might mean that unlike a state of anxiety, depression does not change instantly. It would be interesting to perform massage several times and examine its long-term effect on depression.
In this preliminary study, a significant decrease in hematocrit was observed after the control massage. In our previous study, massage therapy caused a similar hemodilution (26). This phenomenon may happen because of a relative parasympathetic nervous system dominant state. On the other hand, the lack of statistically significant hemodilution after aromatherapy massage may have been due to the diuretic effect of essential oils, especially cypress (1). This difference in hemodilution between aromatherapy massage and control massage was not statistically significant by ANOVA.
With regard to immune measures, a significant increase in numbers of total, CD8+ and CD16+ lymphocytes was observed after aromatherapy massage, but not after control massage. In particular, the increase in CD8+ cell counts after aromatherapy massage was significantly larger than the change in the cell counts after control massage.
A meta-analytic review on psychological interventions and the immune system revealed a significant increase in total lymphocyte numbers with stress management intervention (27). The same review, however, reported that there were no significant changes in natural killer (NK) cells and lymphocyte numbers after the use of relaxation techniques including biofeedback-assisted relaxation, progressive muscle relaxation and relaxation response. In the case of HIV-positive patients, Ironson et al. reported that twenty 45 min massages in 1 month or twice a week for 12 weeks significantly increased NK cell numbers and cytotoxicity (9,24).
There is no consistent view about how relaxation influences lymphocyte counts and NK cell numbers, and it is difficult to interpret changes in lymphocyte counts observed in the present study. One possibility is that a difference in the extent of relaxation between aromatherapy massage and control massage results in this divergence. In the present study, the serum cortisol level was reduced significantly after aromatherapy massage, but not after control massage. Although the difference in cortisol levels between aromatherapy massage and control massage was not statistically significant by ANOVA, this result partly supports the above hypothesis in terms of stress hormone reduction. Another possibility is the pharmacological benefit of essential oils. Indeed, almost all of the essential oils used are known to stimulate the function of WBCs (28).
In our preliminary study, both aromatherapy massage and control massage decreased state anxiety significantly, and only aromatherapy massage (P < 0.05) increased PBLs, possibly due to an increase in CD8+ and CD16+ lymphocytes. These results suggest that aromatherapy massage is a valuable relaxation technique for reducing anxiety and stress, and beneficial to the immune system. Since this study was done on a small number of patients and examined over a short period, it is important to validate the results in a phase I or II trial with a larger cohort of patients over a longer period of time.
Acknowledgments
The authors would like to thank Ms Natsuko Ikeda for performing excellent massage, Hyperplants, Co., Ltd for providing oils and a biofeedback system for the study, and Dr Naohisa Fujita and staff of the Central Laboratory Unit of Kyoto Prefectural University of Medicine for hematological measurements.
References
- 1.Price S, Price L. Aromatherapy for Health Professionals. 2nd edn. London: Churchill Livingston; 1999. [Google Scholar]
- 2.Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database Syst Rev. 2003:CD003521. doi: 10.1002/14651858.CD003521. [DOI] [PubMed] [Google Scholar]
- 3.Gedney JJ, Glover TL, Fillingim RB. Sensory and affective pain discrimination after inhalation of essential oils. Psychosom Med. 2004;66:599–606. doi: 10.1097/01.psy.0000132875.01986.47. [DOI] [PubMed] [Google Scholar]
- 4.Leach MJ. A critical review of natural therapies in wound management. Ostomy Wound Manage. 2004;50:36–40. 42,44–6 passim. [PubMed] [Google Scholar]
- 5.Buckle J. Clinical Aromatherapy in Nursing. London: Edward Arnold Ltd; 1997. [Google Scholar]
- 6.Motomura N, Sakurai A, Yotsuya Y. Reduction of mental stress with lavender odorant. Percept Mot Skills. 2001;93:713–8. doi: 10.2466/pms.2001.93.3.713. [DOI] [PubMed] [Google Scholar]
- 7.Edge J. A pilot study addressing the effect of aromatherapy massage on mood, anxiety and relaxation in adult mental health. Complement Ther Nurs Midwifery. 2003;9:90–7. doi: 10.1016/S1353-6117(02)00104-X. [DOI] [PubMed] [Google Scholar]
- 8.Hada T, Furuse S, Matsumoto Y, et al. Comparison of the effects in vitro of tea tree oil and plaunotol on methicillin-susceptible and methicillin-resistant strains of Staphylococcus aureus. Microbios. 2001;106:133–41. [PubMed] [Google Scholar]
- 9.Ironson G, Field T. Massage therapy is associated with enhancement of the immune system's cytotoxic capacity. Int J Neurosci. 1996;84:205–17. doi: 10.3109/00207459608987266. [DOI] [PubMed] [Google Scholar]
- 10.Ohno T, Kita M, Yamaoka Y, et al. Antimicrobial activity of essential oils against Helicobacter pylori. Helicobacter. 2003;8:207–215. doi: 10.1046/j.1523-5378.2003.00146.x. [DOI] [PubMed] [Google Scholar]
- 11.Abe S, Sato Y, Inoue S, et al. [Anti-Candida albicans activity of essential oils including Lemongrass (Cymbopogon citratus) oil and its component, citral] Nippon Ishinkin Gakkai Zasshi. 2003;44:285–91. doi: 10.3314/jjmm.44.285. [DOI] [PubMed] [Google Scholar]
- 12.Fine DH, Furgang D, Barnett ML, et al. Effect of an essential oil-containing antiseptic mouthrinse on plaque and salivary Streptococcus mutans levels. J Clin Periodontol. 2000;27:157–61. doi: 10.1034/j.1600-051x.2000.027003157.x. [DOI] [PubMed] [Google Scholar]
- 13.Caelli M, Porteous J, Carson CF, Heller R, Riley TV. Tea tree oil as an alternative topical decolonization agent for methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2000;46:236–7. doi: 10.1053/jhin.2000.0830. [DOI] [PubMed] [Google Scholar]
- 14.Satchell AC, Saurajen A, Bell C, Barnetson RS. Treatment of interdigital tinea pedis with 25% and 50% tea tree oil solution: a randomized, placebo-controlled, blinded study. Australas J Dermatol. 2002;43:175–8. doi: 10.1046/j.1440-0960.2002.00590.x. [DOI] [PubMed] [Google Scholar]
- 15.Ro YJ, Ha HC, Kim CG, Yeom HA. The effects of aromatherapy on pruritus in patients undergoing hemodialysis. Dermatol Nurs. 2002;14:231–4. 237–8, 256; quiz 239. [PubMed] [Google Scholar]
- 16.Rowe J. Sensory stimulation in dementia. Bright light may not illuminate. Br Med J. 2003;326:661. [PubMed] [Google Scholar]
- 17.Snow LA, Hovanec L, Brandt J. A controlled trial of aromatherapy for agitation in nursing home patients with dementia. J Altern Complement Med. 2004;10:431–7. doi: 10.1089/1075553041323696. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson S, Aldridge J, Salmon I, Cain E, Wilson B. An evaluation of aromatherapy massage in palliative care. Palliat Med. 1999;13:409–17. doi: 10.1191/026921699678148345. [DOI] [PubMed] [Google Scholar]
- 19.Hadfield N. The role of aromatherapy massage in reducing anxiety in patients with malignant brain tumours. Int J Palliat Nurs. 2001;7:279–85. doi: 10.12968/ijpn.2001.7.6.9025. [DOI] [PubMed] [Google Scholar]
- 20.Charles CH, Sharma NC, Galustians HJ, Qaqish J, McGuire JA, Vincent JW. Comparative efficacy of an antiseptic mouthrinse and an antiplaque/antigingivitis dentifrice. A six-month clinical trial. J Am Dent Assoc. 2001;132:670–5. doi: 10.14219/jada.archive.2001.0245. [DOI] [PubMed] [Google Scholar]
- 21.Wiebe E. A randomized trial of aromatherapy to reduce anxiety before abortion. Eff Clin Pract. 2000;3:166–9. [PubMed] [Google Scholar]
- 22.Soden K, Vincent K, Craske S, Lucas C, Ashley S. A randomized controlled trial of aromatherapy massage in a hospice setting. Palliat Med. 2004;18:87–92. doi: 10.1191/0269216304pm874oa. [DOI] [PubMed] [Google Scholar]
- 23.Cooke B, Ernst E. Aromatherapy: a systematic review. Br J Gen Pract. 2000;50:493–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Diego MA, Field T, Hernandez-Reif M, Shaw K, Friedman L, Ironson G. HIV adolescents show improved immune function following massage therapy. Int J Neurosci. 2001;106:35–45. doi: 10.3109/00207450109149736. [DOI] [PubMed] [Google Scholar]
- 25.Birk TJ, McGrady A, MacArthur RD, Khuder S. The effects of massage therapy alone and in combination with other complementary therapies on immune system measures and quality of life in human immunodeficiency virus. J Altern Complement Med. 2000;6:405–14. doi: 10.1089/acm.2000.6.405. [DOI] [PubMed] [Google Scholar]
- 26.Kuriyama H, Watanabe S, Tadai T, Fukui K, Shirahata I, Imanishi J. The effect of massage therapy on the immune, hematological and psycological state of adult subject. Jpn J Altern Complement Med. 2005;2:59–65. [Google Scholar]
- 27.Miller GE, Cohen S. Psychological interventions and the immune system: a meta-analytic review and critique. Health Psychol. 2001;20:47–63. doi: 10.1037//0278-6133.20.1.47. [DOI] [PubMed] [Google Scholar]
- 28.Rose JE. The Aromatherapy Book: Application & Inhalations. Berkeley: North Atlantic Books; 1992. [Google Scholar]